Week 1 - Foundational Concepts & Frameworks for Promoting the Mental Health of Individuals and Communities; Inclusive of Substance Use Spectrum
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
what is mental health?
enables people to cope with the stresses of life, realize their abilities, learn and work well, and contribute to their community
capacity for us to feel, think, and act in ways that enhance our ability to enjoy life and deal with the challenges we face
more than the absence or presence of illness
what does mental health mean, as described by Keyes?
flourishing -- presence of positive emotions and good functioning in life
subjective sense of well being --> positive functioning in life
flourishing requires 3 types of well being. list them.
psychological well being
emotional well being
social well being
define the following:
-psychological well being
-emotional well being
-social well being
1. positive functioning in personal life
2. positive feelings about life and the absence of negative feelings
3. positive functioning in society and one's community
what is poor mental health / mental illness, as described by Keyes?
languishing -- absence of positive mental health despite not necessarily having a mental illness
emptiness, stagnation, "the end"
**diagnosed clinical conditions that are NOT the opposite of mental health
mental health continuum (Keyes): describe the following...
-mental illness & good MH
-mental illness & poor MH
-no mental illness & good MH
-no mental illness & poor MH

mental health is addressed on 4 levels. what are they?
individual: resilience, control, physical activity, substance use
family: relationships, parenting style, household composition
community: social networks, school, workplace, environment
society: inequalities, politics, discrimination, stigma
the First Nations mental wellness continuum emphasizes that mental wellness is a...
balance of the mental, physical, spiritual, and emotional
mental wellness is enriched as individuals have....
-PURPOSE in their daily lives
-HOPE for their future and those of their families, grounded in a sense of identity
-sense of BELONGING and connectedness within their families, to community, and to culture
-sense of MEANING and an understanding of their lives in history
Indigenist ecological systems model contexts: history
understanding ancestral histories of place, resilience, perseverance, family, community via intergenerational learning
Indigenist ecological systems model contexts: culture
intergenerational learning and transmission of Indigenous knowledge
Indigenist ecological systems model contexts: indigenous youth
relationality and connectedness to ancestors, family, community, spirit, lands
Indigenist ecological systems model contexts: immediate
developing positive strengths-based interactions with caregivers, peers, schools, community
Indigenist ecological systems model contexts: surrounding
promoting positive interactions between 2 or more immediate contexts
Indigenist ecological systems model contexts: distant
promoting positive policy changes and advocacy through societal and human service systems (governance systems, sports teams, healthcare system, media)
what does the substance use spectrum demonstrate?
-substance use is across a spectrum, people vary in stages
-not all substance use is bad (medical, religious, ceremonial)
stages of the substance use spectrum
-non use
-beneficial use
-lower risk use
-higher risk use
-addiction (substance use disorder)
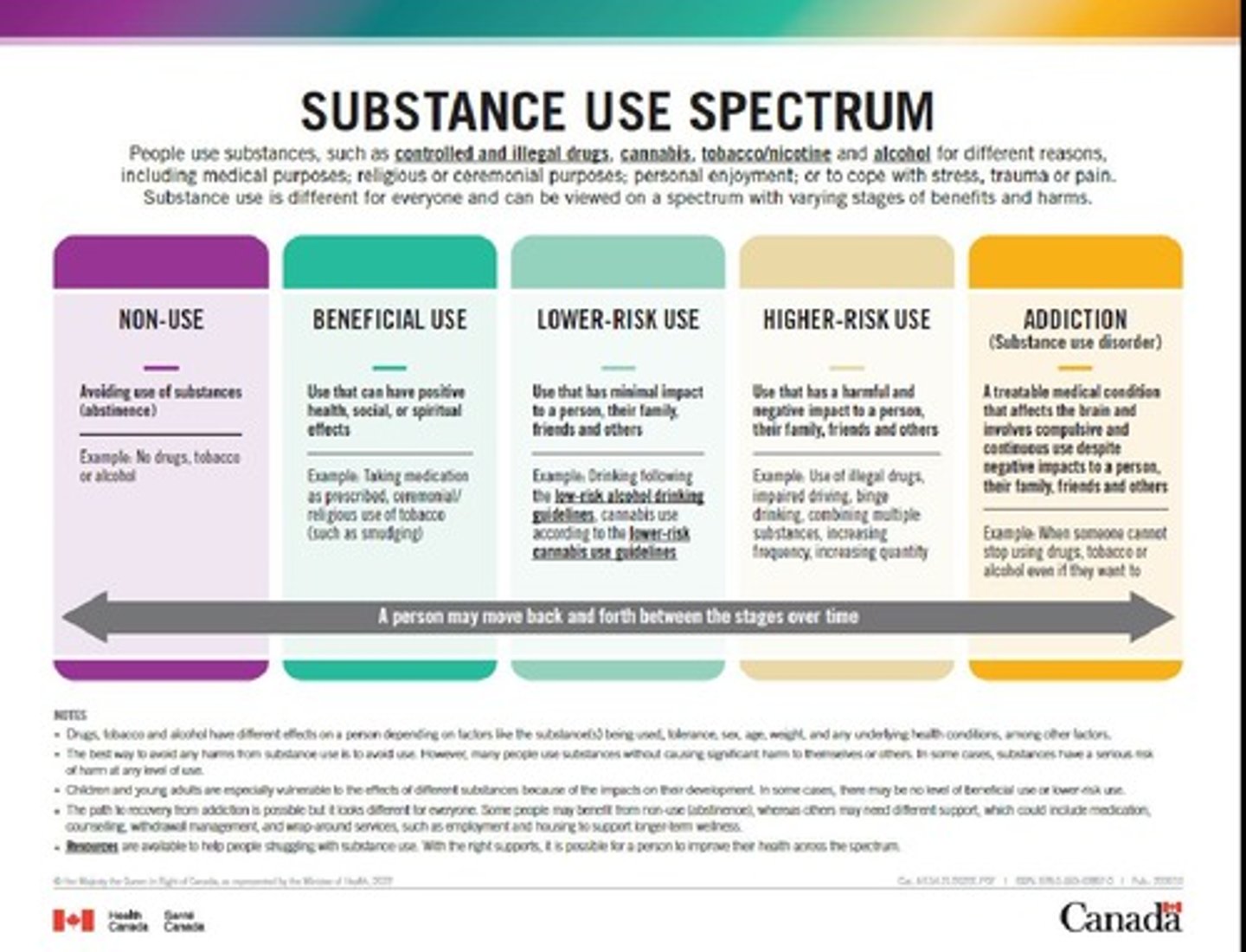
non use
avoiding use of substances (abstinence)
beneficial use
use that has positive health, spiritual, or social impact
lower risk use
use that has minimal impact to a person, their family, friends and others
-eg. drinking or cannabis use following the low risk guidelines
higher risk use
use that has a harmful and negative impact to a person, their family, friends and others
-eg. use of illegal drugs, impaired driving, binge drinking, combining multiple substances, increasing frequency and quantity
addiction
treatable medical condition that affects the brain and involves compulsive and continuous use despite negative impacts
-when someone cannot stop using even if they want to
what is harm reduction defined as?
an approach, set of strategies, policy or program designed to reduce substance-related harm without requiring abstinence
with harm reduction, it aims to work with people who use substances as partners to....
-reduce negative consequences related to substance use
-promote public health, human rights, and social justice
-promotes equity, inclusion, dignity, self-determination
what is trauma?
experience of, and response to, a negative event or events that threaten the person's safety or life
includes responses such as shock, terror, shame, and powerlessness
what is the goal of trauma and violence-informed approaches?
-minimize harm to individuals, not treat the trauma
-aim to increase safety, control, and resilience
4 core principles of a trauma and violence-informed approach
Realize.
Recognize.
Respond.
Reduce Re-traumatization.
3 important reasons to implement trauma and violence-informed approaches
1. increase attention on the impact of violence on people's lives and well-being
2. reduce harm
3. improve system responses for everyone
4 aspects of trauma and violence-informed care
1. understand trauma and violence, and its impact on lives and behaviour
2. create emotionally and physically safe environments
3. fosster opportunities for choice, collaboration
4. use a strengths-based and capacity-building approach
what does "moving away from what is wrong to what has happened?"
instead of thinking "what is wrong with the person?", one should be asking "what has happened to the person?"
enables you to try to understand what the other person has experienced or events which may influence their behaviours
what is stigma?
negative attitude or belief toward someone or something
occurs in forms such as dehumanizing language, stereotypes, and social exclusion
correlation between stigma and mental health conditions
affects how people with mental health or substance use concerns are seen, treated, and how they see themselves.
significantly creates barriers to accessing quality care
cultural competency
knowledge and awareness of cultural and health related beliefs, practices, and cultural values
cultural humility
self-reflection of personal place of power, identity and biases and how that may interface when interacting with people
process of reflection rather than outcome
cultural safety
decolonizing services, systems and policies to mitigate the potential harms, traumas and lack of safety that people experience
places responsibility for creating safety on service providers