f&vd final
1/129
Earn XP
Description and Tags
includes all of the lectures that were on quiz 4 and after, and a couple terms from quiz 3. i have a study set for that material too :)
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
130 Terms
dysphonia
altered quality, pitch, loudness, or increased effort
aphonia
loss of voice
vocal fatigue
client perceives an increase in phonatory effort over time that may be accompanied by decreased phonatory function
globus sensation
feeling like something is in your throat
fixed abduction or adduction
when the vocal cords are stuck and cannot move (abduction = open, adduction = closed)
dyspnea & what are 2 potential/primary causes
feeling out of breath due to interference of airflow due to…
vocal pathology
uncontrolled adduction or abduction obstructing the airway
odynophagia
pain when swallowing
sharp pain
pain at other times besides odynophagia
vocal fold bowing & two causes
inward curvature of vocal fold due to lost muscle bulk caused by aging or nerve damage
vocal fold paresis
weak vocal fold movement
organic voice disorders
due to detectable physical or biochemical changes within cells, tissues, or organs
lesion
damage or abnormal change in tissue
neoplasm
growth of new tissue, either benign or cancerous
two subtypes of organic voice disorders
structural and neurogenic
organic structural voice disorders
something is physically wrong with the vocal mechanism’s laryngeal or velar structure, due either to lesions in tissue or joint tissue
examples of potential causes of organic structural voice disorders
phonotrauma, medical conditions, birth defects, puberty, smoking
organic neurogenic voice disorders
problems with central or peripheral nervous system innervation due to larynx causing trouble with motor movement and muscle tone
examples of potential causes of organic neurogenic voice disorders
neurological diseases, infectious diseases, growths, tumors
velopharyngeal disfunction
insufficient velopharyngeal closure resulting in a leakage of air to the nasal cavity; causes resonance voice disorders
3 causes of VPD
velum deformed due to congenital disorder, doesn’t close due to neurological disorder, or velum is normal but client is not using habitual sufficient velopharyngeal closure
examples of things that cause medical trauma
surgeries, medical procedures, intubation damage, injury, burn, excessive emotional stress
functional voice disorders
vocal mechanism being used inappropriately even though the physical structure is normal
what do voice alterations due to changes in vocal fold vibration cause
changes in quality and pitch
what do voice alterations due to changes in airflow through vocal cords cause cause
changes in quality and loudness
5 categories of organic disorders
growths — neoplasms
lesions
potential or established disease
chronic congenital & acquired
related to development/changes across lifespan
3 types of voice issues — growths
vocal nodules
vocal polyps
vocal cysts
4 types of voice issues — lesions
laryngeal hemorrhage
reinke’s edema
contact ulcers
sulcus vocalis
2 types of voice issues — potential or established diseases
laryngeal leukoplakia
laryngeal cancer
two types of chronic congenital and & acquired voice issues
laryngeal papilloma
laryngeal web
5 types of voice issues related to development/lifespan
laryngeal ankylosis
presbyphonia
puberphonia
laryngomalacia
VPD
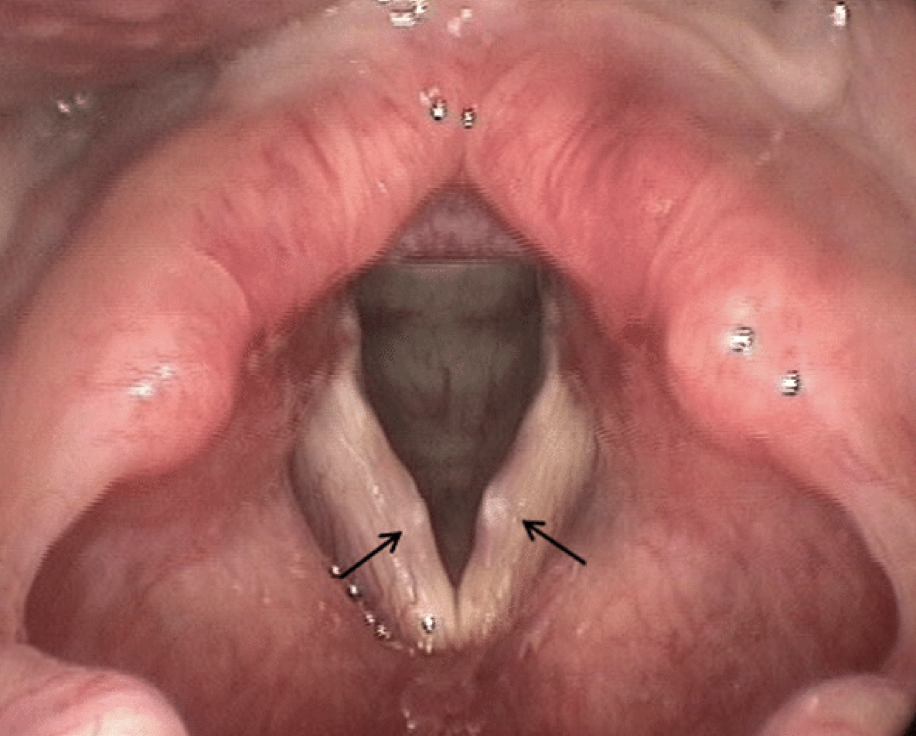
vocal nodules
white soft growth that becomes hard, thick and fibrous like a callous
vocal polyps
blister filled with fluid or blood. can be directly on vocal fold usually at the midpoint (sessile), or attached by a separate piece of tissue (pedunculated)

vocal cysts
blockage in the glandular duct causing retention of mucus or blood

laryngeal hemorrhage
ruptured blood vessels in the submucosal layer of vocal folds (superficial lamina propria). often due to an acute event and increased risk if on blood thinners

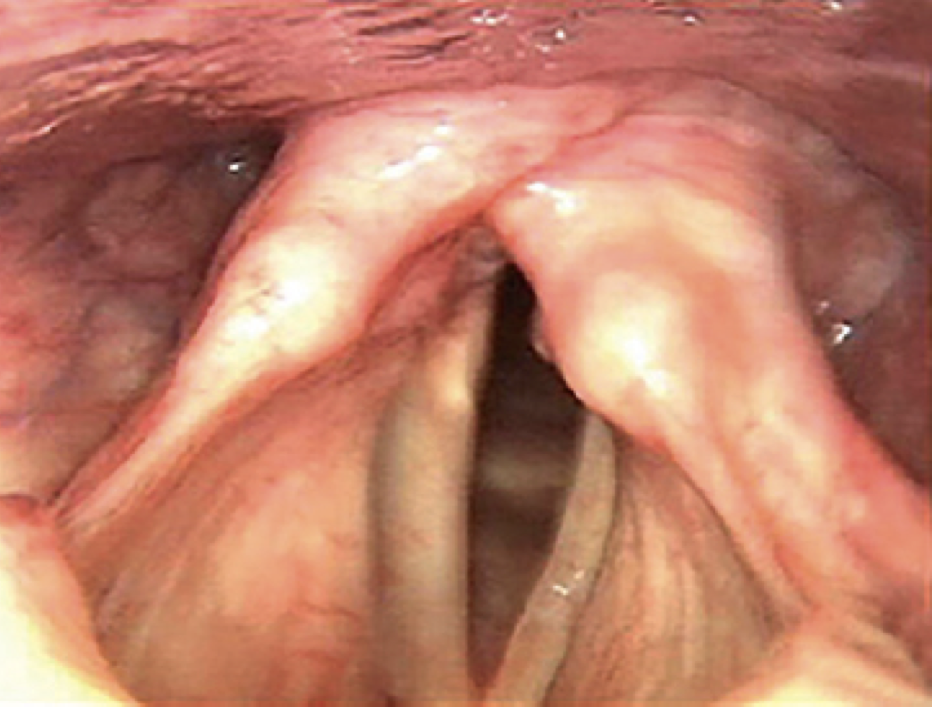
reinke’s edema & alternate names for it
aka polypoid corditis, or if extreme called polypoid degeneration; buildup of fluids or polyps in the superficial lamina propria, which causes edema or swelling of the vocal folds

contact ulcers & what’s associated with it
aka laryngogranuloma; an open sore. leaves a bitter taste in mouth and causes odynophagia or sharp pain during coughing or throat clearing

sulcus vocalis
groove in the development or a narrow cut in the vocal fold
laryngeal leukoplakia
white plaque-like lesions and red patches; can be precancerous

laryngeal cancer
aka carcinoma; it can metastasize

laryngeal papilloma & two ways it can be contracted
benign tumor with wart-like bumps. chronic so it can reoccur
HPV 6 and 11 through skin or STD; congenital through mother’s amniotic fluid or infected area that makes contact during the birth process

laryngeal web & symptoms
sheet of tissue over the vocal folds, that can grow back if removed
stridor, shortness of breath, difficulty swallowing, weak cry in infants, higher pitch
laryngeal ankylosis & 2 typical causes
abnormal stiffening and immobility of the cricoarytenoid jount, that can causes fixed addiction, fixed abduction, dyspnea & odynophagia
typically caused by:
arthritis/joint disease
intubation
presbyphonia
voice issues that occur due to aging changes & anatomical changes. especially loss of muscle mass, muscle strength, and vocal folds becoming thinner, drier and less pliable (vocal atrophy)
puberphonia — organic & causes
remaining prepubescent voice after puberty
congenital laryngeal anomalies, underdevelopment, changes in hormonal development, debilitating disease during puberty
laryngomalacia
malformation of infraglottal tissue, where tissues fall over airway opening, partially blocking it
must resolve without surgery by 18-20 months
three kinds of organic neurogenic disorders, and what can cause them
essential tremor — caused by neurological disease or condition
spasmodic dysphonia — caused by neurological disease, condition, or acute event
unilateral/bilateral vocal fold paresis/paralysis — caused by neurological disease, condition, or acute event
essential tremor & what causes it
shake in the voice. due to involuntary movements of any muscles related to voicing — intrinsic laryngeal, extrinsic laryngeal, pharyngeal, chest wall, abdomen, diaphragm.
disorder is about movement
spasmodic dysphonia & 3 kinds
aka laryngeal dystonia; spasms or jerking movements due to muscle contractions or abnormal fixed postures. may see tremors in other parts of the body as well as in the voice
abductor
adductor
mixed (both)
the disorder is about movement
vocal cord paresis/paralysis & two types for both
weak or lack of movement of the vocal cords
may see vocal fold bowing, and there’s a unilateral type and a bilateral type. unilateral is more common
two kinds of functional use voice disorders
inappropriate use
psychogenic reasons
two kinds of inappropriate use functional disorders
muscle tension dysphonia
ventricular phonation
two kinds of psychogenic functional disorders
conversion aphonia
puberphonia
muscle tension dysphonia
habitual use of excessive muscle tension or constriction; aka functional dysphonia
ventricular phonation
habitual use of the false or ventricular folds during phonation
conversion aphonia
aphonia due to manifestation of stress, depression, or anxiety due to traumatic experience. aka psychogenic aphonia
this is a disorder of movement
puberphonia — functional & 3 possible causes
result of habitual use of a higher pitch or falsetto register. voice sounds the same as the type due to organic reasons
Possible causes:
resistance to pubertal changes
Difficulty accepting change of voice
voice does not match identity
4 specific voice qualities that often face misperception
glottal fry
upspeak
high pitched/nasal voice
monotone voice
glottal fry — definition and misperceptions
use of a low, gravely, crackly sounding voice
may be perceived as sexy, edgy or with the time; lazy or immature in the business world/a different generation
upspeak — definition and misperceptions
tendency to raise pitch of voice at the end of a sentence regardless of whether or not it’s a question
may be perceived as contemporary, immature, less confident & less intelligent
high pitched or nasal voice — definition and misperceptions
use of a higher pitch or a denasal/hypernasal voice
may be perceived as immature, less authoritative, less “manly”
monotone voice — definition and misperceptions
use of a vocal tone with no change in pitch or inflection
may be perceived as bored/disconnected, lacking enthusiasm, lacking concern
percentage of people affected by voice disorders and percentage that seek treatment
3-9% of the US population; however, less than 1% seek treatment
Populations that experience higher incidence
Female adults
Male children
Elderly adults
Professions who speak for long periods of time
Prevention — what three things to do
provide prevention information to individuals and groups; both those who are at a higher risk of them & those who work with those at risk
refer clients in need of medical or psychological intervention
Remain informed of best practices in vocal health
advocacy — what two things to do
support clients with voice disorders or clients who desire voice modification — give them a voice
remain informed of research in the area of voice — knowledge is power
4 kinds of assessment types
observable and measureable physiological
measureable phsyiological
auditory
self-assessment
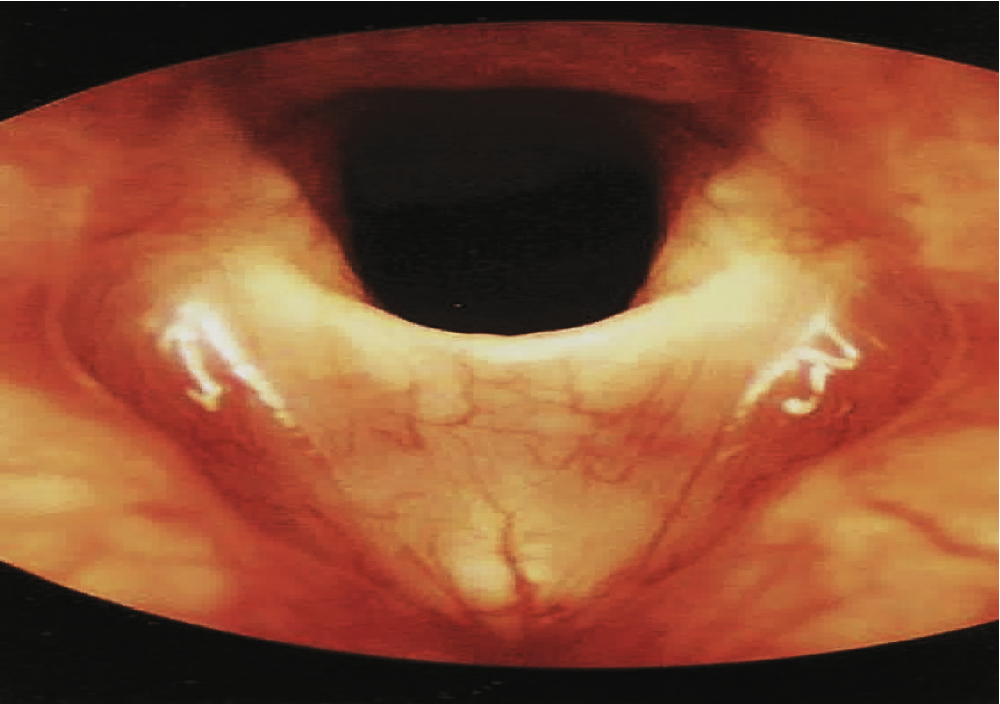
flexible endoscope
long tube with camera and light. bendable so it can go in harder to reach areas of the body such as the nose; less steady, so less clear picture. in real time
rigid endoscope
steel metal rod which functions much like a periscope (camera). steady clearer picture. in real time
videostroboscopy
controlled high-speed flashes of light timed to the frequency of the patient’s voice. images acquired during these flashes provide a slow-motion like view of vocal fold vibration during sound productions, which increases ability to see function in movement, but not in real time
three kinds of observable measureable assessments
indirect laryngoscopy, flexible fiberoptic laryngoscopy, videostroboscopy
indirect laryngoscopy — what kind of assessment is it, who can perform it what what does it do
Observable measurable
ENT or SLP with specialized training
can observe only — uses a small long-handled mirror and a light placed on the roof of the mouth
flexible fiberoptic laryngoscopy — what kind of assessment is it, who can perform it what what does it do
Observable measurable
ENT or SLP with highly specialized training
observe and record a video of function; video playback is in real-time, and can produce consonants and vowels since the tube is up the nose
videostroboscopy — what kind of assessment is it, who can perform it what what does it do
observable measurable
ENT or SLP with highly specialized training
observe and record a video of a function, can be with a rigid or flexible tube. goes down the throat; so it’s closer to the VF; video shows a slow-motion movement of the VF, which makes it the best determiner of VF function and movement. can only produce vowels
measurable assessments — four paramaters (ARAM) and what specialist can perform then
aerodynamic (respiratory)
resonatory
acoustic (pitch/intensity)
muscular
1-3: ENT or SLP who has the equipment
4: neurologist or MD
measurable aerodynamic — what they measure (4 things) and instruments (3) — VBSA, think s&hs
measures vital capacity, breath support, subglottal air pressure, and airflow;
dry spirometer, pneumotachograph, wet spirometer
measureable resonatory — what is measures and instrument (only 1 for each)
measures nasality through nasometer
measurable acoustic — what it measures (4 things) and instruments (2) — think speech & hearing science stuff
measures fundamental frequency, frequency/pitch instability (jitter), amplitude or intensity instability (shimmer), or percentage of voiced/voiceless
instruments are spectrogram & visipitch
measurable muscular — who can perform it and how is it achieved
neurologist or MD
through a procedure such as an electromyography (EMG) — observes the movements of the laryngeal muscles by recording electrical activity through electrodes on the skin and inserted in the muscle
auditory-perceptual assessment: who performs it, what is its method, and what are its tools
performed by an SLP
method is that SLP listens and makes clinical judgements
tools are checklist-like exams, that organize the information to give normative data, such as the buffalo voice profile III and the consensus auditory perceptual evaluation of voice (CAPE-V)
auditory perceptual assessments: three general parameters
respiration, resonation, and phonation
auditory-perceptual — respiration and resonation — how are they measured?
respiration: observe breath support and endurance during phonation measurements
resonation: read passages with and without nasal sounds; compare them and see if there’s a difference
auditory-perceptual — phonation — how is it measured? (4 ways)
maximum phonation time: how long can a vowel be sustained (male 25-35 seconds, females 15-25 seconds)
s/z ratio: how long can /s/ and /z/ be sustained; should be a ratio of 1, and greater than 1.4 = reduced function, which means there’s an air leakage
dynamic range: gradually count from 1-10 with volume ranging from low to high and high to low
singing up and down the scale: determine pitch and pitch range
self assessment — who can perform it, and how
client and SLP
client — fill out answers to questionnaire/survey (e.g. voice handicap index) to determine symptoms, characteristics, habits, and severity of voice issues
SLP — look over the client’s responses and determine the impact their voice is having on their lifed
diagnosis — what can ENT/other professional do vs SLP
ENT: medical diagnosis; specific kind of disorder
SLP: presence of a disorder, and severity of the disorder
prognosis — who can do it and what should be considered for it
any professional; considers components like need for medical intervention, overall health, awareness, willingness to change, family, etc.
four kinds of nonrehabilitative intervention
medical management
hormone therapy
surgery — only for when issue does not respond to medical management or rehabilitation
post-operative care
medical management: definition and when it is used (6 things)
treating the medical condition causing the voice disorder
used for situations such as diseases, infections, reflux, allergies, smoking cessation, neurological conditions
hormone therapy: who receives it
for someone who wants to achieve a more masculine sounding voice. testosterone will cause the larynx to make changes by thickening and lengthening the vocal folds; this cannot be uses for someone who wants to achieve a more feminine voice through estrogen
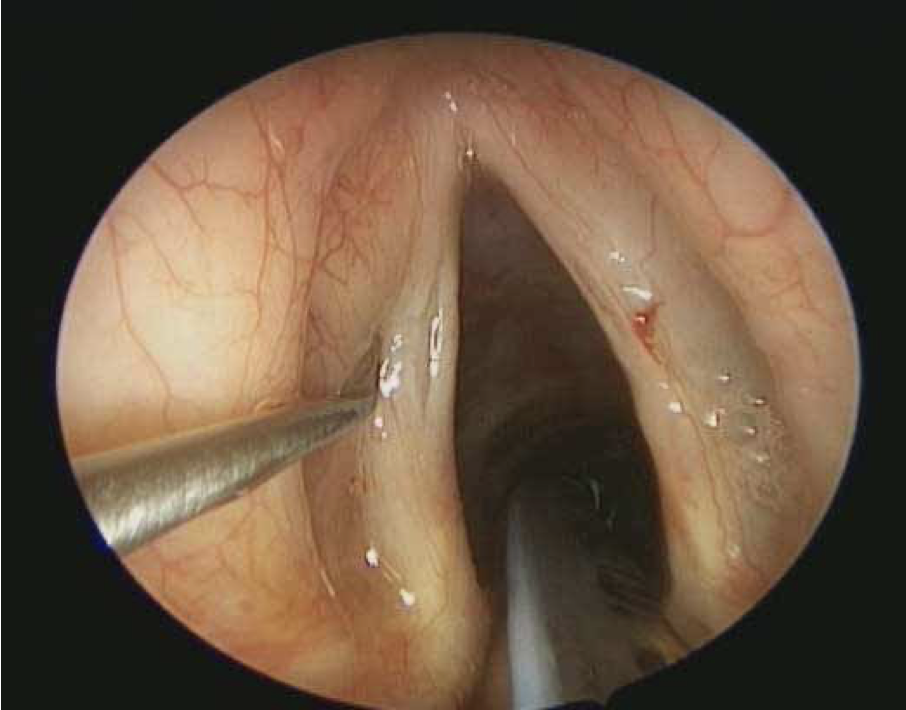
surgery — removal of lesions — purpose and methods (2)
removal of noncancerous, precancerous, or cancerous lesions
methods:
microsurgery, with surgical instruments
laser surgery, with lasers
surgery — removal of the larynx — what is it and why
a laryngectomy; removing the larynx when cancer cannot be treated with surgery or radiation
surgery —medialization — purpose (helps 4 things) and methods (3)
purpose: to help close the glottis for…
atrophy
v.f. bowing
scarring
neurological disease
methods:
arytenoid adduction; rotate cartilage
medialization laryngoplasty (thyroplasty; placing an implant between the thyroid cartilage and VF
injection laryngoplasty; injecting a gel-like substance into one VF to make it closer to the other VF
surgery — lateralization— purposes (2) and methods (3)
Purposes:
to increase lateralization (opening) of the glottis for bilateral vocal fold paralysis and laryngeal ankylosis
To decrease abnormal movement/spasms that cause adduction for spasmodic dysphonia
Methods:
arytenoidectomy — widens the space
vocal fold cordotomy — incision of one or both VF to widen the airway
botox injections — to decrease muscle spasms
surgery — nerve reinnervation — purpose and method
to improve adduction or abduction that is affected by paralysis, paresis, or spasm
regenerates the nerves that innervate the laryngeal muscles where a healthy nerve is moved from a different area of the neck to replace the damaged vocal cord. can take as long as 6-9 months to see improvement
surgery — altering tension and length — purposes and methods (3 - 2 increase, 1 decreases)
changing the length, depth, and tension of the VF by elongating or shortening the laryngeal area, which alters the pitch due to an organic issue or someone who wants voice modification
methods for increasing pitch:
cricothyroid approximation — sutures cricothyroid in a permanent position of contraction to increase tension
anterior glottal web formation — creates a web or scar band at the front of the VF to increase tension
method for decreasing pitch: laryngoplasty; changing shape of thyroid cartilage which decreases tension and stretching of the VF
surgery — reconstruction — purposes (2) and method
Purposes:
surgically correcting tissue loss/malformation
changing larynx for appearance preference (e.g. tracheal shave)
Method: surgery to change shape or size of larynx
post-operative care, definition and 2 things it may include
protocol that client follows after the surgery
may include:
medical regiment
vocal rest; which includes not laughing, crying, etc.
3 kinds of rehabilitative intervention
indirect therapy: modify cognitive, behavioral, psychological, and physical environments where client uses their voice
collaboration: collaborate with relevant professionals
direct therapy: focus on manipulation the voice — respiration, phonation, resonation to modify vocal behaviors and establish healthy voice production
indirect therapy: two kinds
patient education: discussing things like a&p of the voice, their pathology, vocal hygiene, optimal voice use
counseling: addressing things like lifestyle changes, managing best vocal production practices, talking feelings and attitudes, etc.
positive changes that indirect therapy may focus on
preventing phonotrauma/abuse, reducing pathology to promote self-healing, minimizing need for surgery, prevent recurrent pathology
collaboration: who would we collaborate with for…
All
Any organic
Neurogenic
Functional-psychogenic
Trangsgender voice modification
All: ENT
Any organic: pulmonologists, respiratory specialists, endo, genetic counselors, allergists…
Neurogenic: neurologist
Functional-psychogenic: psychologist/psychiatrist/trauma counselor
Trans voice mod: specialty endo, ENT, psychology, surgeon