BMSC 208 - Midterm 1
5.0(1)
Card Sorting
1/320
Earn XP
Description and Tags
Last updated 4:48 PM on 2/15/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
321 Terms
1
New cards
List the four major functions of the respiratory system
1. Exchange of gases between atmosphere and blood
2. Homeostatic regulation of body pH
3. Protection from inhaled pathogens and irritating substances
4. vocalization
2
New cards
What are the 3 structures involved in ventilation and gas exchange?
1. Conducting system or air ways (nasal cavity, pharynx, larynx, trachea, bronchii, bronchiole)
2. Alveoli
3. Bones and muscles of the thorax (ex. SCM, scalenes, intercostals, diaphragm, abdominal muscles)
3
New cards
What is the upper respiratory system?
* Anything not in thoracic cavity
* Nasal cavity, pharynx, larynx
* Nasal cavity, pharynx, larynx
4
New cards
What is lower respiratory system?
* Anything in the thoracic cavity
* Trachea, bronchii, bronchiole, alveoli
* Trachea, bronchii, bronchiole, alveoli
5
New cards
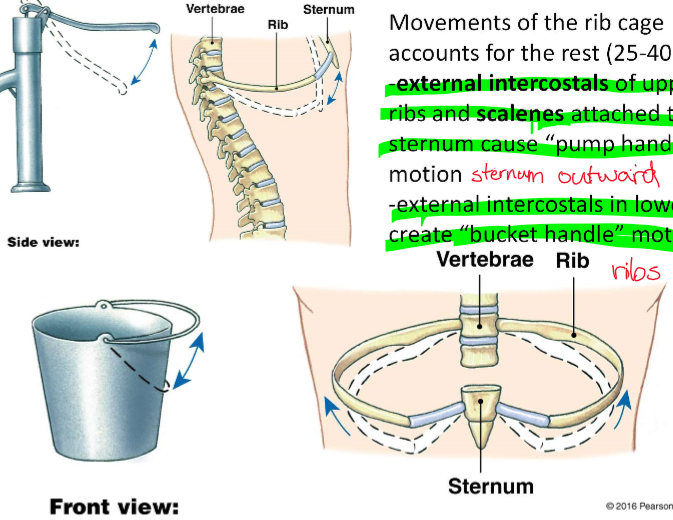
What lung is larger in size?
* Right lung
* Left is smaller due to cardiac notch
* Left is smaller due to cardiac notch
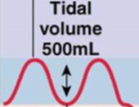
6
New cards
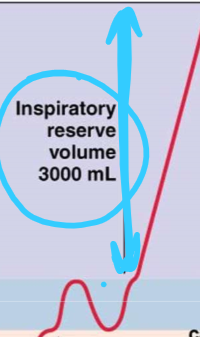
The lungs are surrounded by what structure?
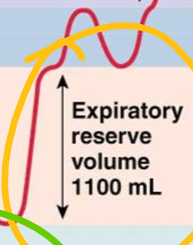
Fluid filled pleural sac
7
New cards
What are the 2 layers of the pleural sac?
1. Visceral pleura – outside surface of lungs
2. Parietal pleura – inside surface of thoracic cavity
8
New cards
2 functions of pleura
1. Creates moist slippery surface (decreases friction)
2. Holds lungs tight to thoracic wall (holds lungs open)
9
New cards
Pathway of air through respiratory system
* Nasal cavity or mouth
* Pharynx
* Larynx
* Trachea
* Bronchus
* Bronchiole
* Alveoli
* Pharynx
* Larynx
* Trachea
* Bronchus
* Bronchiole
* Alveoli
10
New cards
What structure is the voice box/vocal cords?
\- Larynx
11
New cards
What structure is the windpipe?
\- Trachea
12
New cards
Structure of trachea
\- Semi-flexible tube held open with 15-20 cartilage rings
13
New cards
How is the branching of the respiratory system similar to the CV system?
Branching increases down the respiratory system causing an increase in **total** cross-sectional area (even though there is a decrease in single pathway CSA)
14
New cards
Velocity of air flow is _________ proportional to total cross-sectional area
* Inversely
* V=Q/A
* V=Q/A
15
New cards
Velocity _____ as CSA increases?
\- Decreases
16
New cards
Velocity _______ as CSA decreases?
\- Increases
17
New cards
The major role of the upper airways and bronchi is?
\- Conditioning the air before it reaches the alveoli
18
New cards
What are the 3 ways upper airways and bronchi condition the air before reaching the alveoli?
1. Warming air to body temp
2. Adding water vapor (liquid in alveoli needed for gas exchange)
3. Filtering out foreign material (nasal hairs, shape of nasal airways causes particles to embed in mucus in back of pharynx and slide down to esophagus)
19
New cards
How is air filtered in the trachea and bronchi? i.e. What types of cells line the airways, what do these cells produce, and what is their function?
* Airways are lined with ciliated epithelial cells and goblet cells
* Ciliated epithelial cells produce saline
* Goblet cells produce mucus (overtop the saline) which contain immunoglobulins
* Ciliated epithelial cells push the mucus towards the pharynx (mucocilliary escalator)
* Ciliated epithelial cells produce saline
* Goblet cells produce mucus (overtop the saline) which contain immunoglobulins
* Ciliated epithelial cells push the mucus towards the pharynx (mucocilliary escalator)
20
New cards
Explain why saline is necessary for mucocillary escalator function?
* Cilia move the saline layer which pulls mucus layer upward towards the pharynx
* Without the saline layer, cilia would become embedded in thick mucus and unable to move
* Without the saline layer, cilia would become embedded in thick mucus and unable to move
21
New cards
How is saline produced?
* produced by epithelial cells
* Cl- secreted into lumen by apical CFTR channel (cystic fibrosis transmembrane regulator channel)
* Secretion of Cl- creates electrochemical gradient which draws Na+ into lumen paracellularly (between epithelial cells)
* NaCl movement lumen creates an osmotic/concentration gradient, so water flows into lumen producing saline
* Cl- secreted into lumen by apical CFTR channel (cystic fibrosis transmembrane regulator channel)
* Secretion of Cl- creates electrochemical gradient which draws Na+ into lumen paracellularly (between epithelial cells)
* NaCl movement lumen creates an osmotic/concentration gradient, so water flows into lumen producing saline
22
New cards
What causes cystic fibrosis?
* CFTR channel non-functioning = reduced production of saline
* Without saline layer, cilia trapped in mucus and can no longer move
* Mucus cannot be cleared, bacteria colonize the airways, resulting in recurrent lung infections.
* Without saline layer, cilia trapped in mucus and can no longer move
* Mucus cannot be cleared, bacteria colonize the airways, resulting in recurrent lung infections.
23
New cards
Alveoli are the site of?
\- Gas exchange
24
New cards
Where are alveoli?
\- Clustered at ends of bronchioles
25
New cards
Alveoli are ________ vascularized and have _______ surface area, optimal for gas exchange
* Heavily
* Huge (very short diffusion distance for increased gas exchange)
* Huge (very short diffusion distance for increased gas exchange)
26
New cards
Alveoli are __% surface area
\- 95%
27
New cards
Function of Type 1 alveolar cell
\- Gas exchange
28
New cards
Function of type 2 alveolar cell
\- Synthesizes surfactant
29
New cards
Alveolar macrophage
\- Ingests foreign material
30
New cards
How does air exchange occur by?
\- Bulk flow
31
New cards
Air exchange occurs by bulk flow and follow what 3 principles that also govern bulk flow through the CV system?
1. Flows from high to low pressure
2. Muscular pump creates pressure gradient
3. Resistance is primarily influenced by diameter of tubes (remember that viscosity and length also affect flow, however these are relatively constant in respiratory system)
32
New cards
What is the flow, pressure, resistance relationship?
F= ∆P/R
33
New cards
Pulmonary circulation has _____ flow and _____ pressure
* High
* Low
* Low
34
New cards
Why does pulmonary circulation have high flow?
* Low blood volume and equal CO to systemic circuit
* Cardiac output in pulmonary system = systemic circuit (this means that as much blood flows through the lungs in 1 minute as flows through the rest of the body)
* Low blood volume = greater turnover of blood
* Cardiac output in pulmonary system = systemic circuit (this means that as much blood flows through the lungs in 1 minute as flows through the rest of the body)
* Low blood volume = greater turnover of blood
35
New cards
Why does pulmonary circulation have low pressure?
Due to low resistance (shorter length circuit, more distensible and larger total cross-sectional area of arterioles
36
New cards
What law describes the pressure-volume relationship of gasses?
* Boyles law
* P1V1=P2V2
* P1V1=P2V2
37
New cards
If the volume of a container decreases, the pressure will?
\- Increase
38
New cards
If the volume of a container increases, the pressure will?
\- decrease
39
New cards
What are the muscles and their functions in quiet inspiration?
* 60-75% of inspiratory volume change is due to diaphragm contracting to move downward/flatten
* 40-25% due to movements of the rib cage
* Pump handle: external intercostals of upper ribs and scalenes attached to sternum pull the sternum outward
* Bucket handle: external internal intercostals of lower ribs pull ribs up and out
* 40-25% due to movements of the rib cage
* Pump handle: external intercostals of upper ribs and scalenes attached to sternum pull the sternum outward
* Bucket handle: external internal intercostals of lower ribs pull ribs up and out
40
New cards
What are the muscles involved in quiet expiration?
* No contraction of muscles, passive process with relaxation of inspiratory muscles
* Diaphragm, external intercostals, and scalene muscle relax
* Diaphragm, external intercostals, and scalene muscle relax
41
New cards
What are the 4 different lung volumes?
1. Tidal volume
2. Inspiratory reserve volume
3. Expiratory reserve volume
4. Residual volume
42
New cards
Do lung volumes overlap?
\- NO
43
New cards
Tidal volume
\- Amount of air that enters/exits the lungs during quiet respiration
44
New cards
Inspiratory reserve volume
Additional air that could still be inspired after quiet inspiration
45
New cards
Expiratory reserve volume
At end of quiet expiration, the volume of remaining air that can be expired
46
New cards
Residual volume
The amount of air that will always remain in the lungs
47
New cards
Two important functions of residual volume
1. Prevents airway collapse, if collapsed would take an unusually large pressure to re-inflate it
2. Allows continuous exchange of gases
48
New cards
Total pulmonary ventilation
* Total ventilation during rest
* Tidal volume x frequency of breaths
* Tidal volume x frequency of breaths
49
New cards
What are the 4 lung capacities?
1. Total lung capacity
2. Functional residual capacity
3. Inspiratory capacity
4. Vital capacity
50
New cards
Total lung capacity
The sum of all 4 lung volumes (IRV, TV, ERV, RV)
51
New cards
Functional residual capacity
* Capacity of air remaining in lungs after quiet expiration
* ERV+RV
* ERV+RV
52
New cards
Inspiratory capacity
* Maximal amount of air that can be inspired after quiet expiration
* IRV+TV
* IRV+TV
53
New cards
Vital capacity
* Maximal achievable air moved with a single breath
* IRV+TV+ERV
* IRV+TV+ERV
54
New cards
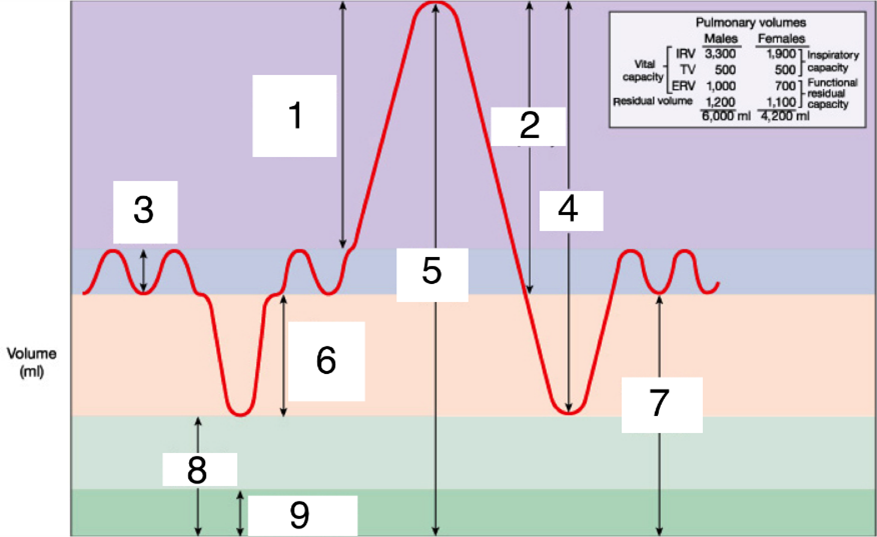
Label
1. inspiratory reserve volume IRV
2. Inspiratory capacity
3. Tidal volume TV
4. Vital capacity
5. Total lung capacity
6. Expiratory reserve volume ERV
7. Functional residual capacity
8. Residual volume
55
New cards
Explain how pressure and lung volumes change during normal breathing and how that affects air flow in the respiratory system.
* Inspiration: alveolar volume increases resulting in decreased pressure below atmospheric pressure, resulting in air flow from the atmosphere into alveoli
* Expiration: alveolar volume decreases resulting in increased pressure above atmospheric pressure, resulting in air flow from the alveoli to the atmosphere
* Expiration: alveolar volume decreases resulting in increased pressure above atmospheric pressure, resulting in air flow from the alveoli to the atmosphere
56
New cards
True or false: the lung is directly attached to the diaphragm and thoracic wall, so breathing occurs from diaphragm pulling lungs downward and ribcage outward
* False
* The lungs are attached to the pleural sac
* The lungs are attached to the pleural sac
57
New cards
What is the intrapleural pressure within the parietal sac
* About -3 mmHg
58
New cards
The lungs have a natural tendency to go inwards or outwards?
* Inwards
* They have a natural recoil
* They have a natural recoil
59
New cards
The chest wall has a natural tendency to go inwards or outwards?
\- Outwards
60
New cards
The natural inward recoil of the lungs and the natural outward recoil of the chest wall creates a?
* Negative intrapleural pressure
* The inspiratory muscles pull the parietal layer of pleura away from visceral layer, increasing the volume of the intrapleural cavity and thus decreasing the intrapleural pressure
* The inspiratory muscles pull the parietal layer of pleura away from visceral layer, increasing the volume of the intrapleural cavity and thus decreasing the intrapleural pressure
61
New cards
True or False, the apex of the lungs are more positive in intrapleural pressure?
\- False, the apex is more negative
62
New cards
Explain how lungs expand in inspiration with the intrapleural cavity
* Inspiratory muscles expand chest cavity which increases the intrapleural volume
* Increase in intrapleural volume decreases to an even more negative value
* Lungs are drawn to more negative intrapleural pressure and thus expand
* Increase in intrapleural volume decreases to an even more negative value
* Lungs are drawn to more negative intrapleural pressure and thus expand
63
New cards
Fill in the blanks. Inspiration: Diaphragm and inspiratory intercostals _________. Thorax ______. Intrapleural pressure becomes _________. Lungs ________. Alveolar pressure becomes _________. Air flows _______.
* Contract
* Expands
* More Sub atmospheric (more negative)
* Expand
* Sub atmospheric (more positive)
* Into alveoli
* Expands
* More Sub atmospheric (more negative)
* Expand
* Sub atmospheric (more positive)
* Into alveoli
64
New cards
Fill in the blanks. Expiration: Diaphragm and inspiratory intercostals ________. Chest wall _______. Intrapleural pressure _______. Lungs ______. Air in alveoli becomes _________. Alveolar pressure becomes _______. Air flows ________.
* Relax
* Recoils inward
* Becomes more positive and moves back toward preinspiration value
* Recoil toward preinspiration size
* Compressed
* Greater than atmospheric pressure
* Out of lungs
* Recoils inward
* Becomes more positive and moves back toward preinspiration value
* Recoil toward preinspiration size
* Compressed
* Greater than atmospheric pressure
* Out of lungs
65
New cards
Traumatic pneumothorax
\- Puncture of parietal or visceral pleura
66
New cards
Spontaneous pneumothorax
\- Lung and visceral pleura rupture
67
New cards
The degree of lung expansion at any time is _______ to the change in pressure
\- Proportional
68
New cards
What is compliance?
* Stretchability
* How much any given change in pressure expands the lungs is dependent on compliance
* How much any given change in pressure expands the lungs is dependent on compliance
69
New cards
What is elastance?
* The ability to resist being deformed
* Elastic recoil
* Elastic recoil
70
New cards
Pulmonary fibrosis
* Formation of excess fibrous connective tissue in the lungs
* Decreased compliance, increased elastance
* Decreased compliance, increased elastance
71
New cards
Emphysema
* Enzymes secreted by WBCs attack alveoli tissue causing them to merge, lose capillaries, lose surface area
* Increased compliance
* Loss of elastance
* Airway resistance
* Increased compliance
* Loss of elastance
* Airway resistance
72
New cards
An important determinant of compliance and a major determinant of the lungs elastic recoil is the __________ at the air water interface of the airways.
\- Surface tension
73
New cards
What is surface tension
\- Measure of the force acting to pull a liquids molecules together at an air water interface
\- The water molecules on the fluid’s surface are attracted to other water molecules beside and beneath them but are not attracted to gases in the air at the air-fluid interface, therefore, the resultant force is downward
\- The water molecules on the fluid’s surface are attracted to other water molecules beside and beneath them but are not attracted to gases in the air at the air-fluid interface, therefore, the resultant force is downward
74
New cards
What direction is surface tension in alveoli?
* directed toward the center of the bubble and creates pressure in the interior of the bubble
75
New cards
What law is an expression of alveolar surface tension?
* Laplace
* P=2T/r
* P=2T/r
76
New cards
If the radius of an alveoli is small, the pressure is?
\- Greater
77
New cards
Increase radius = ______ alveolar pressure
* Decrease
78
New cards
Increase surface tension = _______ alveolar pressure
\- Increase
79
New cards
Decrease surface tension = _______ alveolar pressure
\- Decrease
80
New cards
_____ pressure is needed to keep a small bubble inflated
\- Increased
81
New cards
______ pressure is needed to keep a large bubble inflated
\- Decreased
82
New cards
What is surfactant?
\- Detergent like molecule
\- Secreted by type II alveolar cells
\- Reduces surface tension by decreasing density of water molecules
\- Secreted by type II alveolar cells
\- Reduces surface tension by decreasing density of water molecules
83
New cards
What are the 2 main functions of surfactant in the respiratory system?
1. Increases compliance
1. a.Decreases the inward pressure, so easier to inflate
2. Ensures alveoli of all size inflate
a. Smaller alveoli have more surfactant, which equalizes the pressure between large and small alveoli
84
New cards
85
New cards
What is infant respiratory distress syndrome?
* Developmental insufficiency of surfactant production and immaturity of lungs
* Prevalence decreases with gestational age
* Prevalence decreases with gestational age
86
New cards
Bronchoconstriction/dilation is commonly under ______ control
\- Paracrine
87
New cards
What is the primary paracrine molecule that affects bronchiolar diameter?
\- Carbon dioxide
88
New cards
Increase CO2 in expired air leads to?
\- Bronchodilation
89
New cards
Decreased CO2 in expired air leads to?
\- Bronchoconstriction
90
New cards
_____ is a paracrine signal molecule that acts as a powerful bronchoconstrictor and is released by ____ cells.
* Histamine
* Mast
* Mast
91
New cards
Circulating ________ binding to __ _______ receptors causes dilation
* Epinephrine
* B2
* Adrenergic
* B2
* Adrenergic
92
New cards
Parasympathetic nerves innervate bronchiole smooth muscle and activate _________ pathway via __ _______ receptor and cause constriction
* PLC-IP3
* M3 muscarinic
* M3 muscarinic
93
New cards
What is total pulmonary ventilation?
* Volume of air moved into and out of lungs each minute (minute ventilation)
* Total pulmonary ventilation = ventilation rate x tidal volume
* It is the effectiveness of breathing (similar to stroke volume)
* Total pulmonary ventilation = ventilation rate x tidal volume
* It is the effectiveness of breathing (similar to stroke volume)
94
New cards
What is alveolar ventilation?
* Alveolar ventilation = ventilation rate x (tidal volume – dead space)
* Amount of fresh air that reaches the alveoli
* Amount of fresh air that reaches the alveoli
95
New cards
What is dead space?
* The conducting airways (trachea and bronchi) that do not exchange gases with the blood
* Some air that enters the respiratory system does not reach the alveoli because part of every breath remains in the conducting airways
* Some air that enters the respiratory system does not reach the alveoli because part of every breath remains in the conducting airways
96
New cards
Why does gas composition or PO2 and PCO2 remain relatively constant during quiet inspiration?
* Because O2 entering lungs is equal to O2 uptake
* And amount of fresh air that enters the lungs with each breath is only about 10% of total lung volume at end of inspiration
* And amount of fresh air that enters the lungs with each breath is only about 10% of total lung volume at end of inspiration
97
New cards
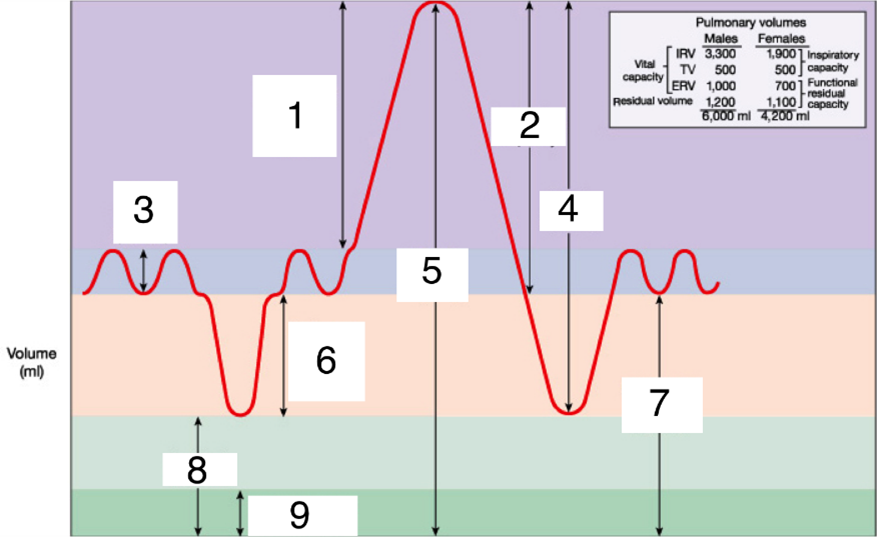
As alveolar ventilation increases (hyperventilation) alveolar PO2 ______ and PCO2 _______
* Increases (more O2 in than diffusion into blood)
* Decreases (removing CO2 more rapidly)
* Decreases (removing CO2 more rapidly)
98
New cards
As alveolar ventilation decreases (hypoventilation) alveolar PO2 _______ and PCO2 ________
* Decreases (less O2 in than diffusion)
* Increases (build of CO2, exhale less)
* Increases (build of CO2, exhale less)
99
New cards
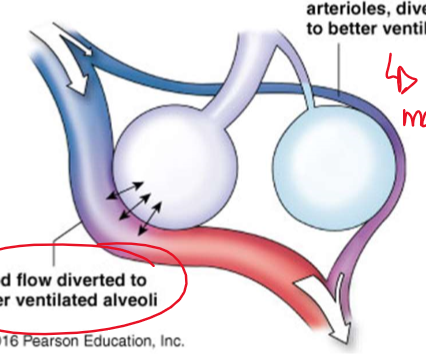
Explain the local control mechanisms by which ventilation and perfusion are matched
* Gravity:
* More negative intrapleural pressure at apex means alveoli are already partially open and filled even at rest, and therefor do not take in much air during ventilation
* Apex gets less perfusion, base gets most
* causes similar regions of lungs to receive matching ventilation and perfusion
* Regulating diameter of arterioles/bronchioles:
* Increased PCO2 = bronchodilation, decreased PCO2 = bronchoconstriction
* decreased PO2 = arterioles constrict
* Constriction of arterioles diverts blood away from under-ventilated region to better ventilated parts of the lung
* More negative intrapleural pressure at apex means alveoli are already partially open and filled even at rest, and therefor do not take in much air during ventilation
* Apex gets less perfusion, base gets most
* causes similar regions of lungs to receive matching ventilation and perfusion
* Regulating diameter of arterioles/bronchioles:
* Increased PCO2 = bronchodilation, decreased PCO2 = bronchoconstriction
* decreased PO2 = arterioles constrict
* Constriction of arterioles diverts blood away from under-ventilated region to better ventilated parts of the lung
100
New cards
What is hypoxia? What is it usually associated with?
* Hypoxia: too little oxygen
* Hypercapnia: excess CO2
* Hypercapnia: excess CO2