2. large animal med- equine stomach/small intestine disease
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
53 Terms
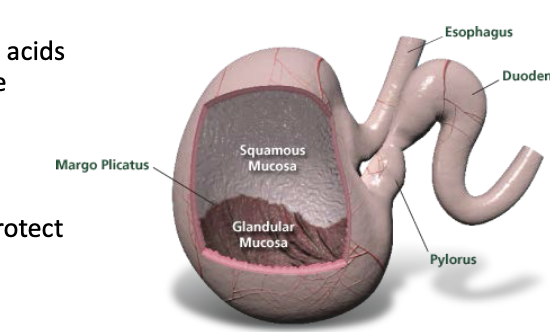
what is the etiology of squamous gastric ulcers?
exposure to gastric acid:
-24 hour acid secretion
-decreased protection on squamous portion
-high grain meal (less forage consumption, VFA)
-increased abdominal pressure (high intensity exercise)
-secondary to delayed gastric outflow

what is the etiology of glandular gastric ulcers?
breakdown of the normal defense mechanisms that protect the lower (glandular) portion of the stomach
what are clinical signs of gastric ulcers in foals?
moderate colic, bruxism

what are clinical signs of gastric ulcers in adult horses?
-low grade, recurrent colic
-bruxism
-decreased appetite
-poor performance
how are gastric ulcers diagnosed?
1. gastroscopy (only definitive way to diagnose)
2. fecal occult blood test
3. SUCCEED equine fecal blood test

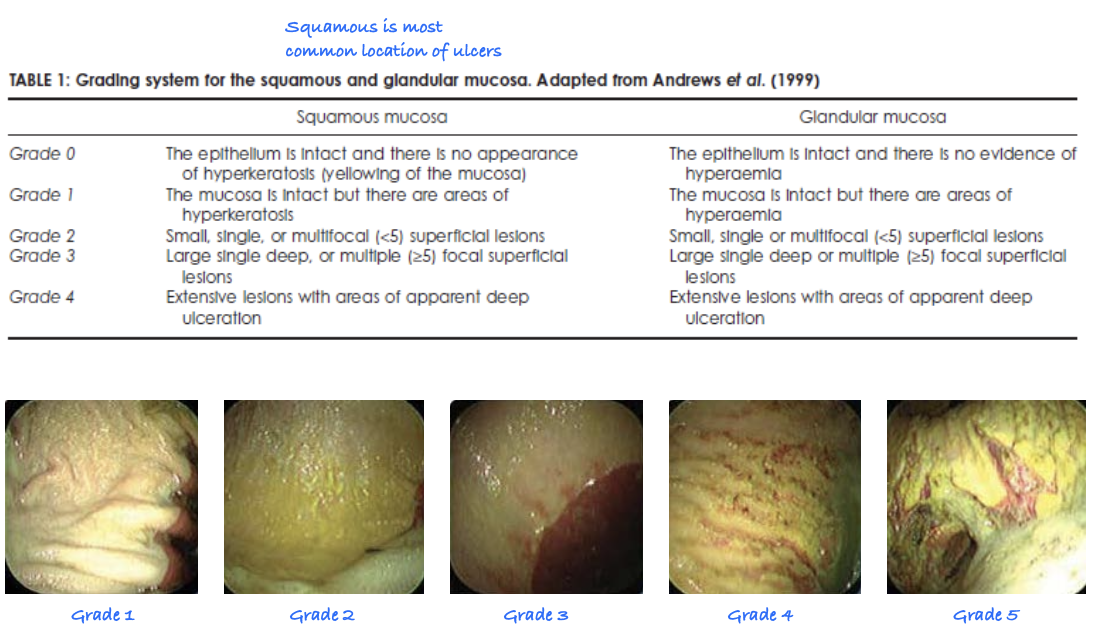
what is the grading system for squamous/glandular mucosal ulcers?
grades 0-4
0=normal, 4= extensive ulceration
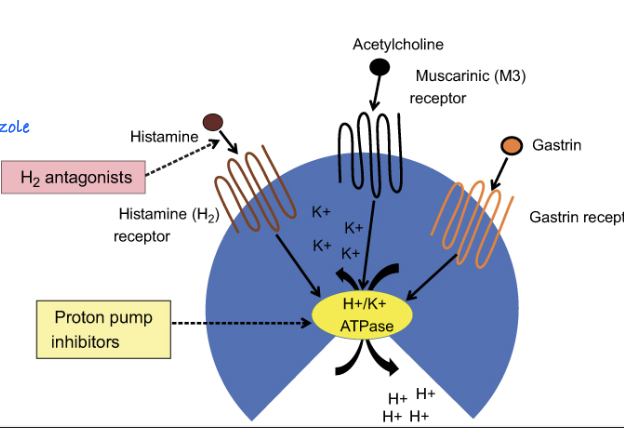
what is the treatment for gastric ulcers?
1. proton pump inhibitor (omeprazole)
2. GI protectant (sucralfate- improves healing when combined w/ omeprazole)
3. histamine 2 blockers (less effective than PPI)
4. antacid
5. misoprostol (for glandular ulcers)
what is the management and prevention of gastric ulcers?
-increase grazing time
-free access hay
-decrease amount of grain offered
-alfalfa (high in calcium, acts as buffer)
-lower dose of omeprazole

what are clinical signs of gastric impaction?
-decreased appetite
-acute and recurrent colic
-relapse of colic after food is introduced
what is the etiology of gastric impactions?
-poor dentition
-poor stomach motility
-outflow obstruction
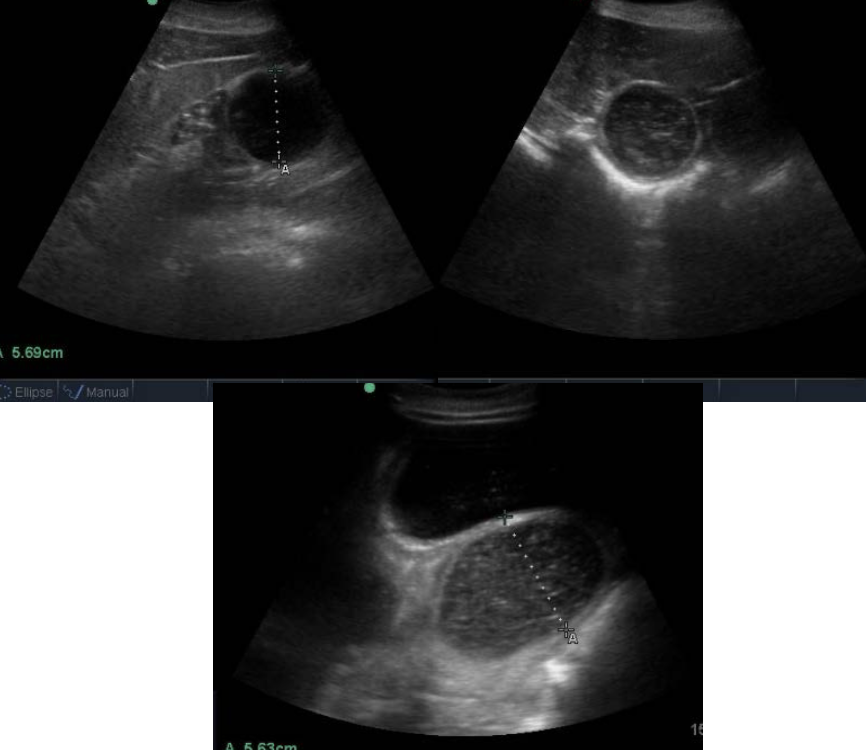
how are gastric impactions diagnosed?
gastroscopy: stomach is still full after appropriate fasting
U/S: shows stomach distension
what is the treatment for gastric impactions?
-fasting
-stomach lavage
-carbonate soda drink (caffeine free, diet - helps break down impaction but also causes ulcers so after some time, lavage)
-+/- pro-kinetic
-gastrotomy if no success (last resort- hard to surgically access stomach
-confirm resolution with scope/ultrasound
how are chronic cases of gastric impactions managed?
-address dental abnormalities
-low bulk diet
-prokinetic (bethanechol)
what is the most common gastric neoplasia in horses?
squamous cell carcinoma
may extend to esophagus, may met to other organs
usually by the time we find it, SCC has metastasized :(
what are clinical signs of gastric neoplasia?
weight loss, colic, reflux
how is gastric neoplasia diagnosed?
gastroscopy and biopsy
what is the prognosis of gastric neoplasia in horses?
poor :(
what are other names for proximal enteritis?
duodenitis-proximal jejunitis, anterior enteritis
what are clinical signs of proximal enteritis?
-colic
-depression
-large amount of reflux
-small intestinal distention
- +/- fever
-systemic illness
-improved pain once stomach is emptied/refluxed
what is the etiology of proximal enteritis?
-unknown
-c. difficile toxins have been isolated with horses with DPJ and other causes of reflux
-occasionally salmonella and c. perfringens
what diagnostics are used to diagnosed proximal enteritis?
1. NGT: large volumes of reflux, may be brown/bloody
2. rectal: distended SI loops, but not taught
3. U/S: generalized distention of SI, wall may be thickened
4. abdominal fluid: usually yellow, elevated TP, mildly elevated WBC
what clinpath abnormalities are seen with proximal enteritis?
-dehydration
-electrolyte loss (Na, Cl, K, Ca, Mg)
-inflammation
- >50% of cases have elevated liver values
what are differentials for proximal enteritis?
simple and strangulating small intestinal obstruction
what is the treatment for proximal enteritis?
-repeated gastric decompression (NGT)
-IV fluids
-promote acid-base and electrolyte balance
-lidocaine CRI +/- prokinetics
-laminitis prevention (ice boots)
-parenteral nutrition support
what is inflammatory bowel disease?
intestinal disorders characterized by inflammatory cell infiltration

what intestinal disorders of horses are included in the general category of IBD? (5)
1. granulomatous enteritis
2. lymphocytic-plasmacytic enteritis
3. basophilic enterocolitis
4. multisystemic eosinophilic epitheliotropic enterocolitis (MEED)
5. eosinophilic enterocolitis (idiopathic focal eosinophilic enteritis)
Great Lions Bring Majestic Energy

what are clinical signs of IBD in horses?
-weight loss despite good appetite
-intermittent abdominal discomfort
-peripheral edema (hypoproteinemia)
-may have diarrhea, esp. if affecting large colon
-MEED (multi-systemic eosinophilic epitheliotropic disease) shows dermatitis
-acute colic (IFEE- mural bands)

what clinpath changes are seen with IBD?
-hypoproteinemia
-hypoalbuminemia
-anemia
-malabsorption of glucose and d-xylose
what changes are seen on ultrasound in horses with IBD?
thickened wall of small intestine (>5mm) due to cellular infiltration
what tissues are biopsied for diagnosis of IBD? how are these biopsies obtained?
1. rectal mucosa via uterine biopsy tool
2. duodenal mucosa via gastroscopy (get tiny bite of mucosa only so can have many false negatives)
3. full thickness via laparoscopy/laparotomy
what is the treatment for IBD in horses?
1. steroids (immunosuppression w/ dexamethasone injectable initially, at least 3 month course - long term dex risks laminitis)
2. dietary changes
3. larvicidal deworming (dewormers addressing larval stages)
4. for IFEE (idiopathic focal eosinophilic enteritis): surgery
what is the prognosis of IBD in horses?
guarded
which ages of horses do ascarid impactions mostly affect?
weanlings, ages 4-24 months

how do ascarid impactions occur?
horses with high parasite burden that are then dewormed with effective product--> dead worms cause impaction
colic in 1-5 days after deworming

what are clinical signs of ascarid impactions?
signs of small intestinal obstruction: colic, reflux
how are ascarid impactions diagnosed?
-signalment
-history of recent deworming
-signs of small intestinal obstruction
-ultrasound

what is the treatment for ascarid impactions?
medical: frequent stomach decompression, supportive care (will usually have to go to surgery)
surgical: manual evacuation into cecum of enterotomy

what is the prognosis of ascarid impactions?
guarded to poor
due to worms releasing toxins causing ileus
what are risk factors for ileal impactions?
-geographic location (SE US)
-feeding bermuda hay
-lack of deworming for tapeworms (since like to hang out at ileocecal junction)
how are ileal impactions diagnosed?
-SI distention on U/S and rectal exam
-might be able to palpate impaction
-normal abdominal fluid (bc no strangulation)
what is the treatment for ileal impactions?
-medical management w/ stomach decompression
-pain management
-IV fluids
surgery if the above dont resolve impaction
what are clinical signs of small intestinal strangulating obstructions?
-marked initial pain, may progress to depression/obtunded
-poor response to NSAIDs, pain recurs after sedation
-sweating/trembling
-systemic compromise (elevated HR, injected MM, prolonged CRT, shock)
-self-trauma
-reflux

how are small intestinal strangulating obstructions diagnosed?
1. rectal exam
2. NGT (will reflux eventually)
3. abdominal fluid
4. US

what is felt on palpation in horses with SI strangulating obstructions?
may palpate distended, taught SI loops
absence of SI does not rule out

what is seen on ultrasound in horses with SI strangulating obstructions?
distended, amotile small intestine. may see localized thickening of SI wall
usually 2 populations- one distended, other is normal
what abnormalities are seen with abdominal fluid in horses with SI strangulating obstructions?
-serosanguinous
-elevated protein and cell count
-elevated lactate when compared to blood (usually 2x blood lactate)
what is the treatment for SI strangulating obstructions?
shock treatment, fluids, NSAIDs, analgesic
surgery
what is the prognosis for SI strangulating obstructions?
guarded- early surgical intervention is key
what is intussusception?
telescoping of the intestine: one segment (intussusceptum) passes inside an adjacent segment (intussuscipiens)
causes venous occlusion (edema, engorgement, and thickening)
which animals is intussusception most commonly seen in?
young foals, yearlings
what is the most common site of intussusception?
ileocecal (ileum going into cecum)
other sites: ileoileal, jejunojejunal, cecocolic
how is intussusception diagnosed?
1. NGT: reflux
2. rectal: SI distention, mass may be palpated at cecal base
3. US: SI distention and target lesion
4. abd. fluid: variable results since strangulating bowel is contained in adjacent bowel

what is the treatment for intussusception?
surgery (resection, or reduction if viable)
