Splanchnic & Hepatic Circulation
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
81 Terms
The vascular beds of the different tissues are generally arranged in parallel. What are the 2 exceptions to this "strictly in parallel" rule
the splanchnic circulation
the renal system (kidney)
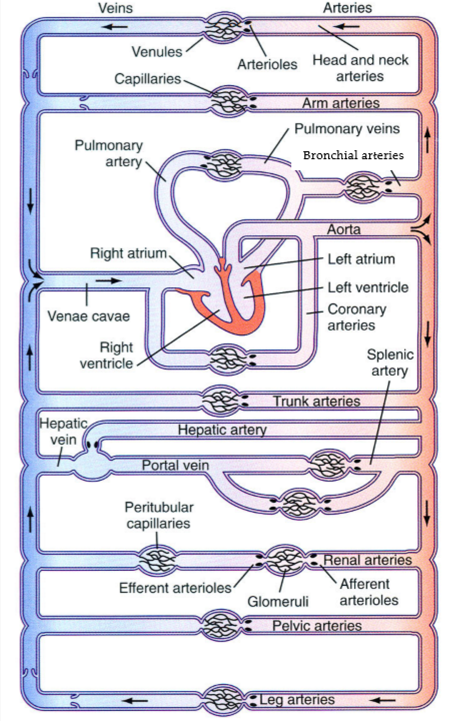
Cardiac output distribution (at rest)
• Gastrointestinal tract – __%
- Liver – __%
• Skeletal muscle – __%
• Kidneys – __%
• Brain -__%
• Skin – __%
• Heart – __%
• Others – __%
Cardiac output distribution (at rest)
• Gastrointestinal tract – 25%
- Liver – 25%
• Skeletal muscle – 20%
• Kidneys – 20%
• Brain -13%
• Skin – 8%
• Heart – 4%
• Others – 10%
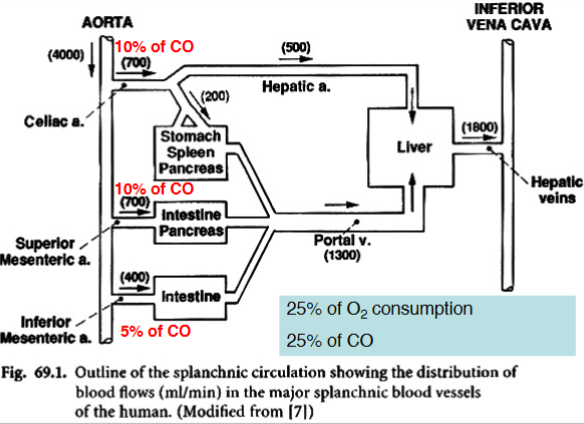
The liver accounts for what % of O2 consumption
25%
We know the GI system accounts for 25% of the total CO. From what branches of the aorta is this output coming (what % for each branch)
10% of CO → Celiac artery (supplies stomach, spleen, pancreas)
10% of CO → Superior mesenteric artery (supplies intestine, pancreas)
5% of CO → Inferior mesenteric artery (supplies intestine)
General structure of the gut wall - 4 layers
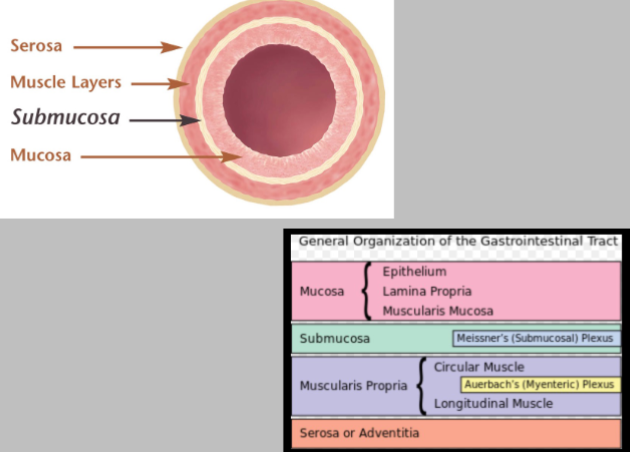
What is involved in microcirculation in the GI tract
Artery, arteriole, precapillary sphinchter, capillary, venule, vein
Blood flow to each layer (mucosa, submucosa, musclaris) is organised in what way? why?
In parallel
This arrangement allows blood flow to adjust to metabolic requirements of each layer by shunting blood from one layer to another without necessarily changing overall GI blood flow
What does splanchnic circulation consist of
It absorbs nutrients from the intestinal lumen and transports them to the liver for storage, transformation, or direct supply to general circulation
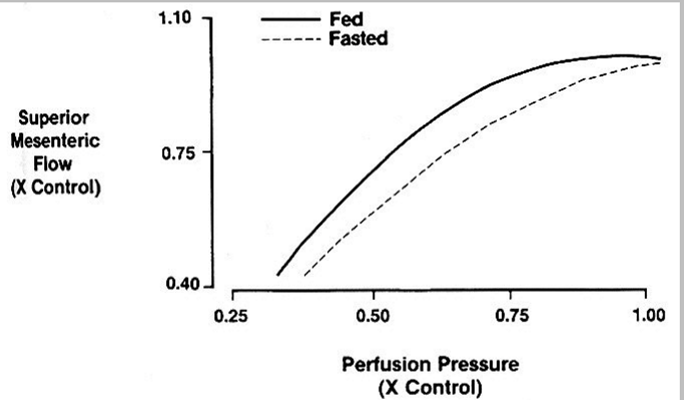
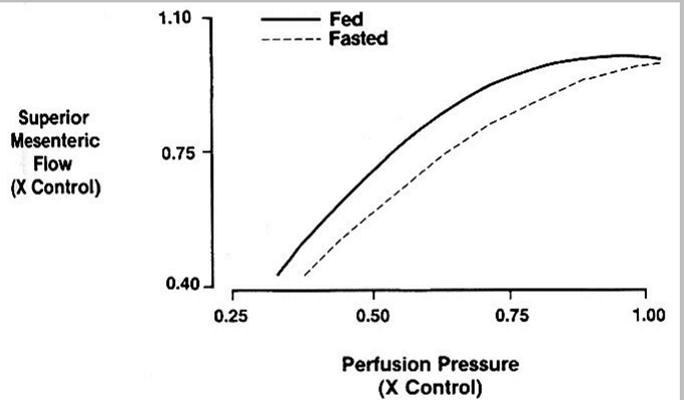
what does this show
In the fed state we exhibit flow at a regulation
(demonstrates an increased intensity of autoregulation during enhanced functional activity)
Explain regulation of splanchnic blood flow
Regulation of splanchnic blood flow
Autoregulation of blood flow in the GI tract occurs
- in the stomach, small intestine and colon
- more prominent in the fed than in the fasting state
- more prominent in the mucosa (metabolically more active)
How does the sympathetic nervous system regulate splanchnic blood flow
Blood vessels in the GI tract are heavily innervated by the sympathetic nervous system
Activation of the SNS causes a-adrenoceptor mediated vasoconstriction
Diversion of blood from the GIT to “vital organs” during reduction in MAP (200-300 mL)
During haemorrhage, GI blood flow can be reduced to 25% of resting flow following SNS activation
Effect of vasoconstriction of arterioles in GI on blood pressure
Vasoconstriction of arterioles in GI increases blood pressure (TPR)
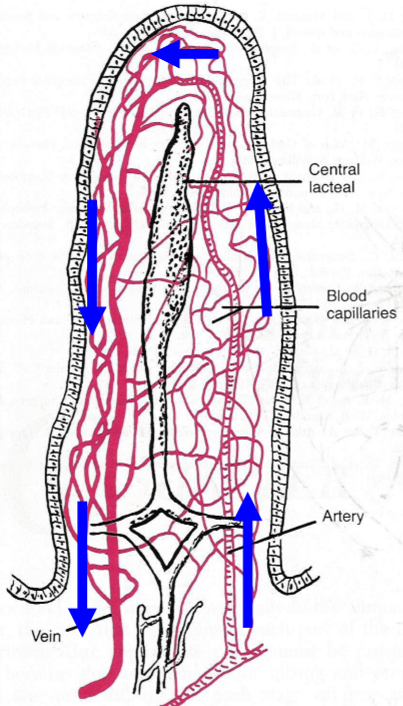
does this accurately represent blood flow
No - Blood flow decreases as you go up the villous to save oxygenated blood for parts of the GI tract that need it more (e.g. Liver)
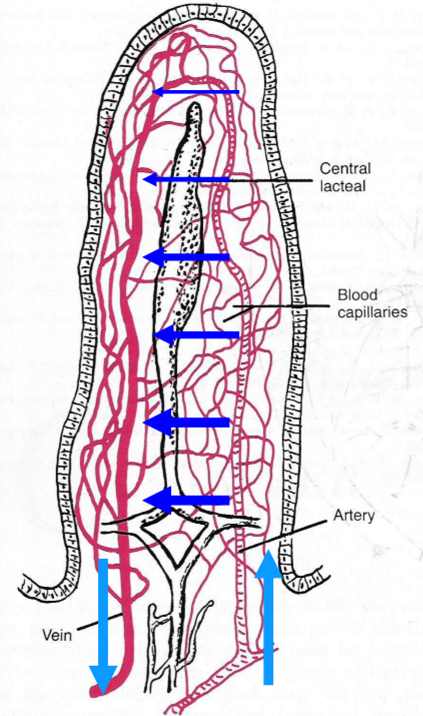
What % of blood O2 is transported from the arterioles into adjacent venules, via capillaries, without being carried to the tip of the villus
As much as 80% take this short-circuit (countercurrent blood flow)
When would short-circuit (countercurrent blood flow) in the villous be a problem
In circulatory shock, cells in tip of the villus may become ischaemic and die
Why is the GI tract highly sensitive to severe hypoperfusion
Severe hypoperfusion disrupts the mucosal barrier, allowing harmful substances like endotoxins (LPS) to enter the bloodstream.
What happens when the mucosal barrier of the GI tract is compromised due to hypoperfusion
The barrier function is reduced, allowing endotoxins (LPS) to enter the systemic circulation.
What is endotoxin (LPS - lipopolysaccharide), and why is it dangerous in systemic circulation
Endotoxin (LPS) is a component of Gram-negative bacterial cell walls that can trigger inflammation, septic shock, and multi-organ failure when it enters circulation
During digestion and absorption within 20 min after the ingestion of a meal, GI blood flow can increase __-fold
Can increase 6 fold
The increase in GI blood flow during digestion & absorption is almost exclusively confined to where
The mucosa
What are the mechanisms involved in regulating gastric mucosal blood flow
metabolic vasodilation (adenosine)
dilator action of GI hormones and neurotransmitters (cholecystokinin, vasoactive intestinal peptide, gastrin, secretin)
Name a GI neurotransmitter with vasodilatory properties & explain its function
Vasoactive intestinal peptide (neurotransmitter released from parasympathetic, cholinergic nerves) - acts on smooth muscle and glands -relaxes sphincters, increases pancreatic and intestinal secretion
(Only VIPs can cause GI vasodilation!)
Name 3 GI hormones with vasodilatory properties & explain their functions
Cholecystokinin:
acts on pancreas, gallbladder and stomach
increases enzyme secretion, contracts gallbladder, increases gastric emptying
Gastrin:
acts on stomach
increases gastric acid secretion
Secretin:
acts on pancreas and stomach
releases bicarbonate and pepsin
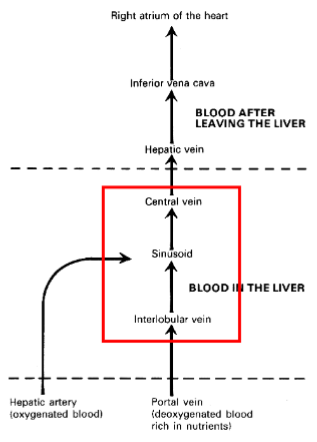
Venous outflow from the GI tract enters
The (hepatic) portal vein
The portal vein drains directly into the
Liver
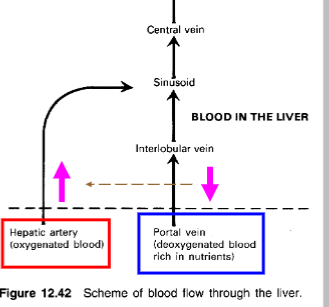
Other than the portal vein, where does the liver receive blood from
receives a blood supply from the aorta via the hepatic artery
Does blood flow form the hepatic artery and the portal vein ever mix in the liver
Yes
Blood exits the liver via the _____ and enters the ______
Blood exits the liver via the hepatic veins and enters the inferior vena cava (IVC)
How many L of blood flow to the liver per minute is normal
1-2 L/min
How does the liver act as a reservoir
Because the liver is an expandable/compressible organ, large quantities of blood can be stored in its blood vessels (sinusoids and hepatic veins)
Normal liver blood volume (in ml & % of total blood volume)
500 mL
10% of total blood volume
Role of liver in hypervolemia & hypovolemia
The liver is a large expandable venous organ capable of acting as a blood reservoir in times of excess blood volume (hypervolemia) and is capable of supplying extra blood in times of reduced blood volume (hypovolaemia)
In cardiac failure, when right atrial pressure rises, the volume of blood in the liver can rise to what
1L
How does the sympathetic nervous system use the liver to increase systemic circulation
In times of circulatory stress, the sympathetic nervous system causes vasoconstriction of the hepatic veins & sinusoids and a large volume of blood is discharged in systemic circulation within 1-4 min (this volume of blood mobilised can be as much as 350mL)
What is the single most important source of extra blood in times of need ((heavy exercise, severe haemorrhage)
Liver
True/False Portal blood is venous and is de-oxygenated
Semi true: Portal blood is venous and is partly de-oxygenated
Portal venous blood flow accounts for what % of total liver blood flow
Portal venous blood flow = 70- 80% of total liver blood flow
Is portal venous pressure high/low
Low
Portal venous pressure in mmHg
5-10 mmHg
Is hepatic arterial blood well oxygenated
Yes
Hepatic arterial flow accounts for what % of total liver blood flow
20-30%
Is hepatic arterial blood pressure equivalent to mean arterial pressure
Yes
How are the sinusoids protected from high pressures
Hepatic arterial resistance resides in the hepatic arterioles which protects the fragile sinusoid from high pressures
Hepatic arterial and portal venous blood flows meet where
Hepatic arterial and portal venous blood flows meet in the hepatic sinusoid (liver capillary)
Describe how the structure of sinusoids allows plasma proteins to pass through
Sinusoids are lined with a layer of endothelial cells
In the endothelium are clusters of pores or fenestrae
• The sinusoidal wall is very leaky and allows plasma proteins to pass through it
(SSSinuSSSoidal walls - you can hear them leaking “SSSssss…”)
The human liver has how many lobes
4 (right, left, caudal, quadrate)
Each lobe of the liver is made up of _________
Lobules (just visible to the naked eye)
Shape of lobules
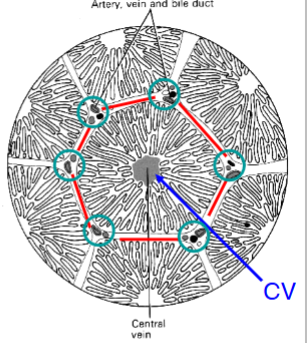
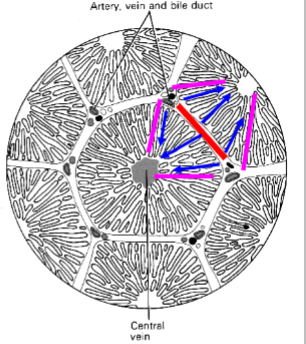
Hexagonal
Vascular arrangement in the liver
at each point on the hexagon of a lobule is an arrangement of vessels
- branch of portal vein
- branch of hepatic artery
- a bile duct
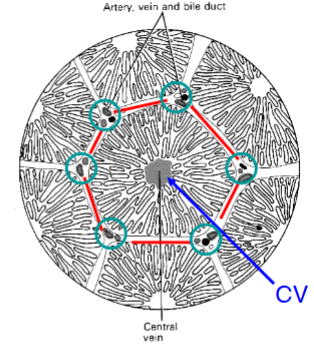
The arrangements of vessels is in the liver is called what
Portal tract
At the centre of the “classic” liver lobule is a
central vein
Lobule Structure explanation
The lobule is made up of parenchymal cells or hepatocytes arranged in pairs of columns radiating from the central vein.
Between 2 pairs of hepatocyte columns are the liver capillaries or hepatic sinusoids
A bile canaliculus runs between 2 columns of hepatocytes
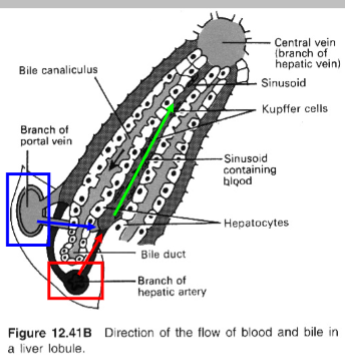
What does the bile canaliculus do
A bile canaliculus runs between 2 columns of hepatocytes & drains into a bile duct
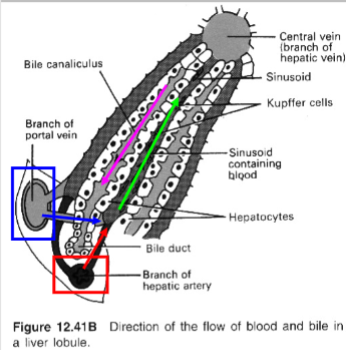
bile canaliculi run in the same/opposition direction as blood flow
Opposite
In the classic liver lobule, how many portal tracts lead to the central vein
6

The “portal vein lobule” involves the portal veins draining towards how many neighbouring central veins
The “portal vein lobule” involves the portal veins draining towards 3 neighbouring central veins
In the “portal vein lobule” model, how are the areas between portal tracts perfused with blood, if the flow is directly from the portal tracts to the central vein?
In the portal vein lobule model, blood flow is directed from the portal tracts to the central vein, which might seem to bypass the areas between portal tracts. However, these areas still receive perfusion due to capillary networks and diffusion.
The portal vein branches into what going where
The portal vein branches into smaller terminal portal venules or perilobular veins which radiate from the portal tract towards the neighbouring portal tracts
Functional unit of the liver
The acinus
What is an acinus
The volume stretching between 2 portal tracts and out to the 2 nearby central veins
The acinus is divided up into 3 zones. What is the difference between the zones
zone 1 (periportal): high in O2 and substrates
zone 2 (intermediate): intermediate values-
zone 3 (pericentral): low in O2 and substrates
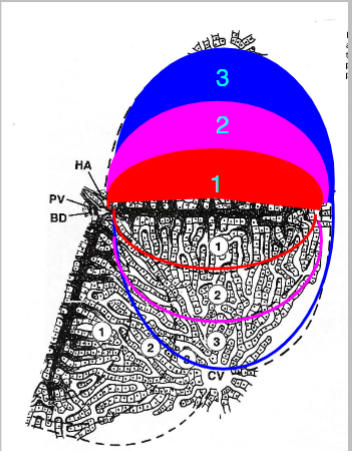
The function of hepatocytes in a single sinusoid depends on what
the acinar zone in which they reside
Function of hepatocytes in zone 1
oxidative metabolism
Function of hepatocytes in zone 3
Lipogenesis
(fat synthesis requires little to no oxygen so zone 3 is suitable)
Hepatocytes in what zone are susceptible to ischemic injury
Zone 3
(it is low in oxygen so that would make sense)
Is portal venous blood flow regulated by the liver
Portal venous blood flow is regulated not by the liver but is dependent on the vascular resistance of the GI tract
What regulates hepatic arterial blood flow
Hepatic arterial blood flow is under sympathetic tone (a-adrenoceptor mediated vasoconstriction)
Explain how the Hepatic arterial buffer response works
When the flow in the portal vein decreases (e.g., due to portal hypertension), the hepatic artery compensates by increasing its flow to maintain the overall blood flow to the liver. Conversely, if portal vein flow increases, the hepatic artery constricts to reduce its blood flow.
(the hepatic artery fixes whatever problems hepatic veins cause)
Would occlusion of the portal vein blood flow have any effect on mean arterial blood flow
Yes - Occlusion of the PVBF would cause an increase in mean arterial blood pressure (femoral artery) → increase in HA (hepatic artery) blood pressure → increase in HABF (hepatic artery blood flow) → Hepatic arterial buffer response
role of adenosine in the Hepatic Arterial Buffer Response (HABR)
adenosine acts as a key mediator in the HABR by stimulating vasodilation of the hepatic artery when portal flow decreases, thereby helping to stabilize hepatic blood flow and maintain liver function under varying hemodynamic conditions
Does adenosine have the same effect when administered via either the hepatic artery or the portal vein
Yes - in both cases it causes hepatic artery dilation
What is dipyridamole
An adenosine uptake blocker - increases adenosine concentration → increases the HABR (Hepatic Arterial Buffer Response)
What could be administered to reduce the HABR (Hepatic Arterial Buffer Response)
Administration of the adenosine receptor antagonist, MIX, reduces the HABR
(adenosine follows the rules & vasodilates the artery. MIX comes in to mix it up and work against rule following adenosine)
What is necessary for portal venous blood flow (PVBF) to wash away adenosine from the hepatic artery (HA)?
Portal venous blood must have access to the arterial resistance vessels.
Where are the small branches of hepatic arterioles, portal venules, and bile ductules located in the liver
They are located within the limiting plate of the portal triad.
What is the fluid space called where the small branches of the portal triad are located
the space of Mall
(the portal triad love trying things on in the mall)
In the hepatic arterial buffer response what happens when portal venous blood flow (PVBF) decreases (role of adenosine)
A decrease in PVBF causes the build-up of adenosine, which is usually washed away by PVBF
Adenosine builds up in the space of Mall (the area around the portal triad), and it is no longer washed away by the reduced PVBF. This accumulated adenosine diffuses into the hepatic artery (HA) where it causes vasodilation
How does adenosine affect the hepatic artery (HA)
When adenosine diffuses to the hepatic artery, it binds to purinergic receptors, and induces vascular smooth muscle relaxation.
What are the two mechanisms through which adenosine induces relaxation of the hepatic artery (HA)?
1) cAMP-mediated relaxation
2) Hyperpolarization-mediated relaxation
(adenosine calms hepatic artery (vasodilation) by camping in the north pole)
What happens to the hepatic artery (HA) when adenosine causes smooth muscle relaxation
The hepatic artery dilates, and the hepatic arterial blood flow (HABF) increases.
How does the liver maintain total blood flow despite changes in portal venous blood flow (PVBF)?
Total liver blood flow is maintained at a constant level, up to a maximum of 25%, by adjusting hepatic arterial blood flow (HABF).