hhd unit 3 outcome 2
Changes in health status in Australia over time
1. Infectious + parasitic disease
Transmitted from one person 2 another including disease tuberculosis, polio, smallpox hepatitis sti + illness: syphilis, venereal.
Parasites such as worms, skin mites, and body lice enter the body through contaminated food + water or contact w others w parasites on skin/hair
Cause sickness/death
Water + food contaminated supplies + rubbish was not well established
Leading to outbreaks of diarrhoea + disease.
HIV/AIDS + hepatitis C responsible for death rates
2. Concerns (neoplasm)
Cancer increased in the 20th century peaking in the 1980s, rising due to lung cancer from cigs/stomach cancer
3. Cardiovascular disease
Referred 2 as circulatory disease eg. heart attack, stroke, high blood pressure, ischaemic heart disease + cerebrovascular disease.
4. Injury + poisoning
From motor vehicles +to accidents, suicide, assault, poison, drowning, burns, toxic substances
5. Respiratory disease
It affects the lungs involving breathing eg. pneumonia, influencer, asthma, chronic obstructive pulmonary
Old public health
Government actions focused on changing the physical environment to prevent the spread of disease, providing safe water sanitisation, sewage disposals, improved nutrition + housing/work conditions.
Access to clean water/sanitation facilities was minimal, bad hygiene practices, litter in streets attract rats carrying diseases and overcrowded poor housing.
Quarantine laws:
prevented the arrival + transmission of infectious diseases from other countries.
Eliminating housing slumps/better quality housing
regulation to improve housing conditions introduced houses built with drains.
Improve food + nutrition:
food was a common transmitter of disease from bacteria, parasites, toxins, and viruses.
Improved working conditions:
providing better ventilation + toilets in the workplace + prohibiting employment of under 13
Hygiene birthing practices:
emphasis on providing safe + hygienic birthing conditions teamed + registered midwives/doctors reduction of maternal + infant mortality rate
Mass vaccination programs:
immunisation as associated with old public health.
The Biomedical Model of Health
bandaid/quick fix focus on physical/biological aspects of disease + illness
Focus mainly on the use of technology 2 diagnose + cure diseases + services provided by doctors, specialists + hospitals
Diagnosis is when a doctor identifies diseases + illnesses through the use of a test
Cure + treatment refers to intervention or steps taken to control illness eg. blood tests, tests, bypass surgery, chemotherapy
Focus on conditions and treatments considered the solution of disease.
Advantages:
advances in technology/research
Many common problems are effectively treated
Extends life expectancy
Improve the quality of life
Disadvantages:
relies on professional health workers + technology = costly
Don't always promote good H+W
Not every condition can be treated
Affordability
Biomedical models eg. cardiovascular system major death, and the introduction of sphygmomanometer + stethoscope enable doctors to measure blood pressure for the first time. A new X-ray enables doctors to view the action of the heart using dye inserted into a blood vessel.
New public health
Referred to an organised response by society to protect + promote health + to prevent injury, illness, disability
Medical technologies + knowledge of disease + illness developed expectations and beliefs that would solve H+W problems
Lifestyle diseases (CVD) have become the leading cause of death + Disability
Increase understanding of the significant influence that the physical, social, cultural + political environment
The Social Model of Health
Developed in the 1970s, addresses factors that lead to ill health + health inequality
Principles of a social model
Address broader determinants:
gender, culture, race, ethnicity, sex, geographical location, physical enviro
involves intersectoral collab:
government + non-government organisations + stakeholders involving all interests + concerned groups can social determinants be equally addressed
Acts to reduce social inequalities:
gender culture, race, sex, access to healthcare, social exclusion, physical environment
Empowers individuals + community:
participate in decision making empowering individuals and communities w knowledge + skills
Advantages:
promote good health + assist to prevent disease
Relatively inexpensive
Focus on the vulnerable population group
Education passed on from generation to generation
Disadvantages:
not every condition is preventable
Not promote the development of technology + medical knowledge
Does not address the health concerns of individual
Examples of programs
Closing the gap, sunsmart, breast screen aus, quit, then quit, be a man talk to your doctor about prostate cancer, swap it don't stop it
Ottawa charter
Aim to take action to achieve health for all.
Health promotion: Health promotion is the process of enabling people to increase control over, and improve their health
relationship between biomedical and social model
Improve technology in terms of better diagnosis and more effective treatments
Lung cancer + social model of health: anti-smoking promotion campaigns relationship between smoking and cancer + comprehensive anti-smoking media + policies eg. health warning on cigs reflects principles of the social model as it is empowering individuals and communities providing them with knowledge of smoking dangers
Diagnosis: test + procedures of chest x-ray, sputum cytology, fine needle aspiration, ct, pet, bone scan, surgery, radiotherapy
australia's health system
public
Public hospital
Medicare
Aus universal insurance scheme by fed gov
Give us permanent residence + reciprocal agreement to access subsided healthcare
Out of hospital:
medicare pay all/some fees relating to essential healthcare services eg. consultations, doctors, specialists, test, exams, extracts, blood test
Out-of-hospital expense schedule fee:
based on the amount thought to be reasonable for a particular service
Patient co-payment:
fee more than the scheduled fee responsible for paying difference
bulk bill:
If the doctor only charges a scheduled fee, the patient doesn't have out-of-pocket expenses and is bulk billed.
In-hospital expenses:
public patient in public hospitals, accommodation and treatment by doctors and specialists is covered by Medicare, initial treatment + aftercare.
Services covered by Medicare:
doctor + specialist consultations, most surgical and therapeutic procedures performed by gp, x-ray, eye test by optometrist pathology, fee-free treatment + accommodation, dental services
Medicare safety net:
provide financial assistance for out-of-pocket costs of Medicare, once contributed to a certain amount of own pocket to Medicare services in a calendar year medicare services are cheaper for the remaining year.
Funded by:
medicare levy (additional 2% tax placed on taxable income), levy surcharge(people with private health insurance earning more than a certain amount have to pay extra tax), general tax (revenue collected from levy + surcharge)
Not covered by Medicare:
any cosmetics/unnecessary procedures, costs associated with private hospitals, ambulance, allied health services eg. chiro, health-related aids, pharmaceuticals, dental exam
Advantage:
choice of doctor 4 out of hospital service, available to all us citizen, reciprocal agreement bw aus allow free healthcare access, cover test + exam, doctors, medicare safety net
Disadvantages:
no choice of doctor for in hospital, the waiting list for treatment, not cover alt therapy or not cover full doctor visit
PBS
Scheme subsided specifically prescribed pharecutuals
Aim to provide essential medicines to people who need them regardless of ability to pay
Medicines subsided + consumers make a copayment for most PBS subsidised medication
Individuals + families are further protected from overall expenses listed in medicines SafetyNet
Only pays concessional co-payment rate
Ndis
Provides services + support for people with permanent + significant disabilities and their family/carers
Funded through fed state + territory government
Work to assist individuals with disabilities to live an ordinary life
Meet age, residency and disability requirements
private
Private health insurance
Pay the premium fee in return for payment towards health-related costs not covered by Medicare
Optional form of insurance
Admitted as a private patient in a public hospital
Greater choice in terms of doctor/hospital
Strains public health system
Incentives private health insurance rebate:
the policyholder receives a 30% rebate/refund on the premium
Incentive lifetime cover:
take up PHi after 31 and pay an extra 2% on premium every year over 30
Incentive Medicare levy surcharge:
pay extra tax if not purchased (1-1.5%)
Advantages:
Enable access to private hospital care
Choice of doctor
Shorter waiting time eg. for elective surgery
Help cost of operating under control
High-income earners do not pay levy surcharge
Government rebate
Lifetimes cover
Disadvantages:
Costly in terms of premium
‘Gap’ insurance due to not covering individual pay difference
Complex policies
Private hospital
Cover general treatment extras cover to pay for services provided by dentists, physio, and chiro not covered by Medicare
Usually charge more than the scheduled fee
Medicare practitioners in private practice
Aus health system in promoting health
Sustainability
meeting the needs of the present without compromising the ability of future generations to meet their own needs
capacity to provide workforce infrastructure: eg. adequately staffed and highly trained, my health record
innovative responsive to emerging needs through disease prevention and early intervention: eg. breast screening + immunisation
research and monitoring: eg. support research to find new ways to cure treat prevent
The system must be equipped to evolve to ensure high-quality care continually available for anyone
Medicare: determine which services will be subsided
Pbs: reviewing medicines available through PBS greater benefit-keeping scheme sustainable
Ndis: individualised plan necessary funds for each person
Phi: incentives eg, rebate
Sustainability funding regulation: crucial to sustainability adequate funds be available to ensure the health system can continue to care for the needs of the population over time, regulating the health system help remain sustainable by promoting efficient use of funds + resources
Access
Ses: health system provides all people with access to quality services based on needs
Geographic: access in all geographical areas eg. royal flying doctor
Culturally appropriate: indigenous aus
medicare : provide all ses + funding for telephone + video
Pbs: aus citizen + permanent resident entitled to access subsided meds, essential meds to low income
Ndis: improve access to health services for people w significant disabilities
Phi: rebate increase access to PHI for low-income increase access to health services too expensive to afford
Funding
Financial resources that provide to keep the health system adequately staffed + resources such as hospitals, primary health care, referred medical services, research eg. infrastructure, trained professionals, published health services, essential mds
Medicare: parts/all fees associated with health services
Pbs: provide treatment for many conditions
Ndis: provide funding for a range of resources to support daily living, assistive technology eg. wheelchair
Phi: fund private hospitals responsible for 40% of treatments, federal govt funds the private health insurance rebate phi more affordable
Equity
Providing hospital care to all Australians fairness resources need to lead to good life take unfair circumstances into account the disadvantaged given the opportunity
Medicare:
safety net: requires frequent services covered by Medicare
Mental health plan: Mental health eligible for 10 therapy sessions per calendar year cost covered by Medicare
Pbs:
Safety net: protect individual + family from large expenses listed medicine
Concessional copayment: greater assistance to those who are unemployed + low income + indigenous qualify reduced PBS co-payment
● Ndis: individuals plan to ensure those w significant needs receive more assistance
● PHI: low income receive more financial assistance + aged 65+ greater rebate
roles of health promotion improving Population Health
smoking
population health
relates to the health and well-being or health status of a group or groups of people
eg. mental health and well-being of youth, the incidence of cancer among males, low socioeconomic status
why smoking is targeted
smoking is a preventable risk factor all smoking-related diseases and impacts are considered to be avoidable
smoking affects vulnerable population groups disproportionately, with people living outside major cities and people from indigenous and low ses backgrounds being more likely to smoke tobacco
half of all long-term smokers will die prematurely due to smoking
exposure to environmental tobacco smoke also causes disease and premature death in adults and children who do not smoke
health promotion interventions
Government laws and policies
federal law bans smoking in all Australian commonwealth government buildings on public transport airports and all international/domestic flights
laws on advertising, packing, smoke-free environment and tobacco taxes that work to increase the price of tobacco to reduce smoking rates
legislation includes
increase taxation on tobacco and the resulting higher price of tobacco is associated with a lower prevalence of smoking among all population groups
laws banning smoking in pubs and clubs have a bigger impact on lower socioeconomic status populations with a reduction in consumption
Victorian legislation includes:
smoking is banned in areas commonly used by children and young people for recreational and smoking activities
prohibited at all VIC-patrolled beaches
offence to smoke in vehicles when a person under 18 is present
ban on smoking on government school grounds
smoking in enclosed public places
reducing the risk of exposure to environmental tobacco smoke eg. creating a supportive physical environment for those who choose not to smoke
anti-smoking laws eg. healthy public policies work to make not smoking the easier and healthier choice
National tobacco campaign
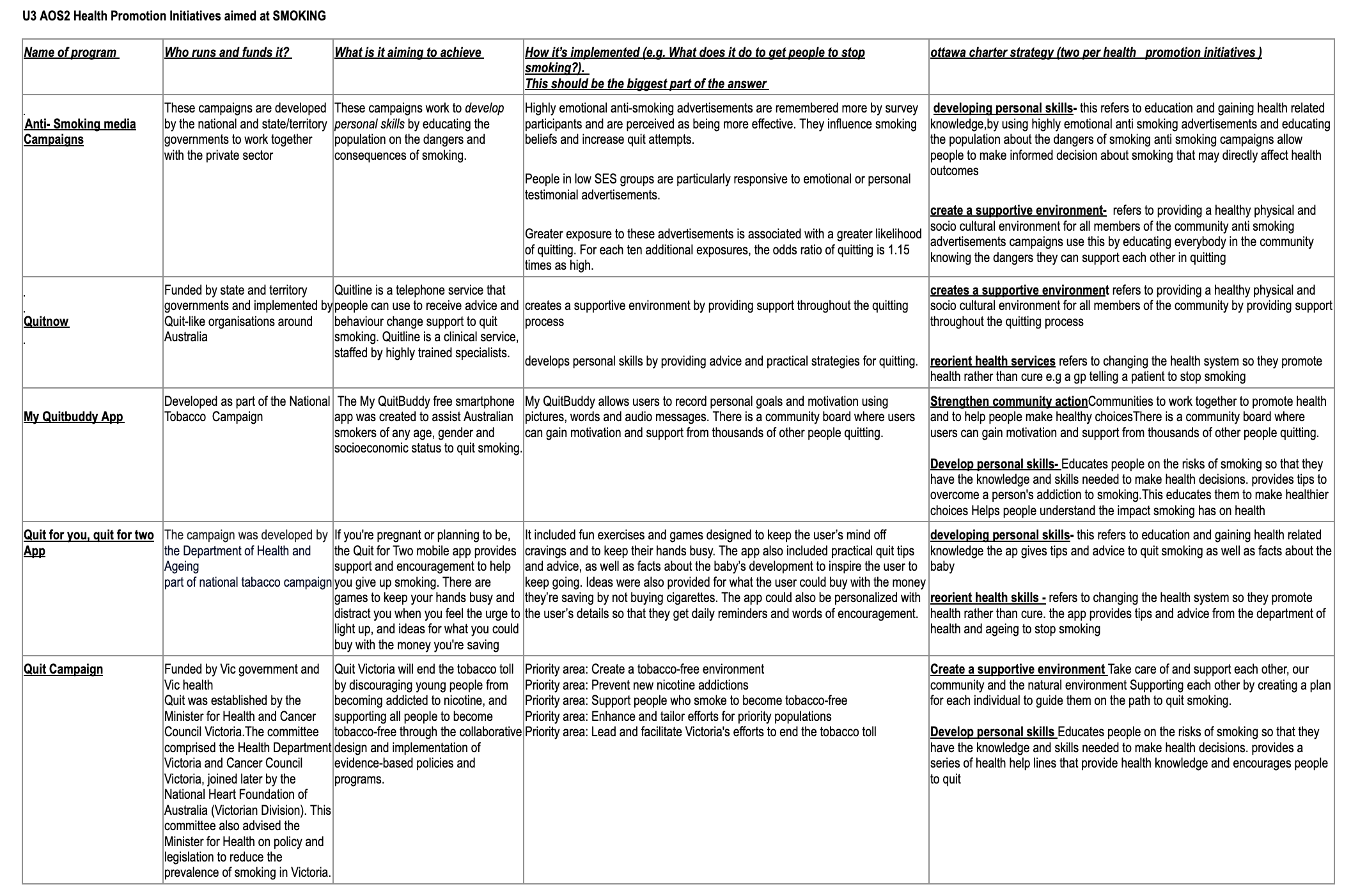
Anti-smoking media campaigns
work to develop personal skills by educating the population on the dangers and consequences of smoking
‘don’t make smokes your story’ create supportive environments by providing information on how to access resources to assist in quitting
Highly emotional anti-smoking advertisements are remembered more by survey participants and are perceived as being more effective. They influence smoking beliefs and increase quit attempts.
People in low SES groups are particularly responsive to emotional or personal testimonial advertisements.
Greater exposure to these advertisements is associated with a greater likelihood of quitting.
the federal government, state and territory government
Quitnow (website for the National Tobacco Campaign)
website to strengthen community action by providing links to quit organisations in each state + territory
develop personal skills by producing a range of fact sheets and resources:
why quit — this section outlines the physical and social impacts of smoking and the benefits that occur when a smoker quits.
How to quit — users are supported by advice for preparing to quit, different methods of quitting and the support services available.
Having trouble quitting — this section provides advice on overcoming setbacks, ways to cope with cravings and how to plan another quit attempt if one fails.
Indigenous support — quitting information is provided for Indigenous youth and the benefits of quitting for the whole family are outlined.
My QuitBuddy (App developed as a part of the National Tobacco Campaign)
a free smartphone app was created to assist Australian smokers of any age, gender and socioeconomic status to quit smoking.
The app provides feedback to users enabling them to track how many cigarettes they haven’t smoked, how many grams of tar they’ve not inhaled, how much money they’ve saved each day and how many days they’ve been smoke-free.
This assists in developing personal skills by providing information that can assist in reducing the risk of smoking-related diseases.
My QuitBuddy creates a supportive environment by allowing users to:
record personal goals and motivation using pictures, words and audio messages. There is a community board where users can gain motivation and support from thousands of other people also quitting.
to program danger times at which the app will send reminders of the health and well-being benefits of quitting, and games are provided to play during times of craving to provide a distraction.
to share their quit journey and success stories with others on Facebook and Twitter.
Quit for you, quit for two apps (App developed as a part of the National Tobacco Campaign for pregnant women)
Developed as part of the National Tobacco Campaign, the Quit for You, Quit for Two free smartphone app was created to assist Australian smokers who are pregnant, or planning to be, to quit smoking.
app creates a supportive environment by including fun exercises and games to keep the user’s hands busy to help beat cravings.
personalisable to give users daily reminders and words of encouragement. entering baby's due date, sending messages detailing baby's growth and development
developing personal skills by providing practical quit tips and advice to quit smoking providing a running tally of how much saved by not smoking and what items could be purchased with that money including facts about baby development to provide more reason to resist any urges to smoke
Quit
Quit campaigns are run in each state and territory, sometimes as a joint venture between the state or territory government and the Cancer Council for the respective state or territory, although other organisations may be involved. This section focuses on the actions of Quit Victoria.
Quit Victoria is a program of the Cancer Council Victoria, which is funded by the Victorian Government and VicHealth, and is an example of strengthening community action.
Quit Victoria aims to decrease the prevalence of smoking by assisting smokers to quit and preventing the uptake of smoking in non-smokers. To achieve their aims, Quit employs a range of actions.
Ottawa charter relating to smoking
Aim to take action to achieve health for all.
Health promotion
Health promotion is the process of enabling people to increase control over and improve their health
Lung cancer + social model of health: anti-smoking promotion campaigns relationship between smoking and cancer + comprehensive anti-smoking media + policies eg. health warning on cigs reflects principles of the social model as it is empowering individuals and communities providing them with knowledge of smoking dangers
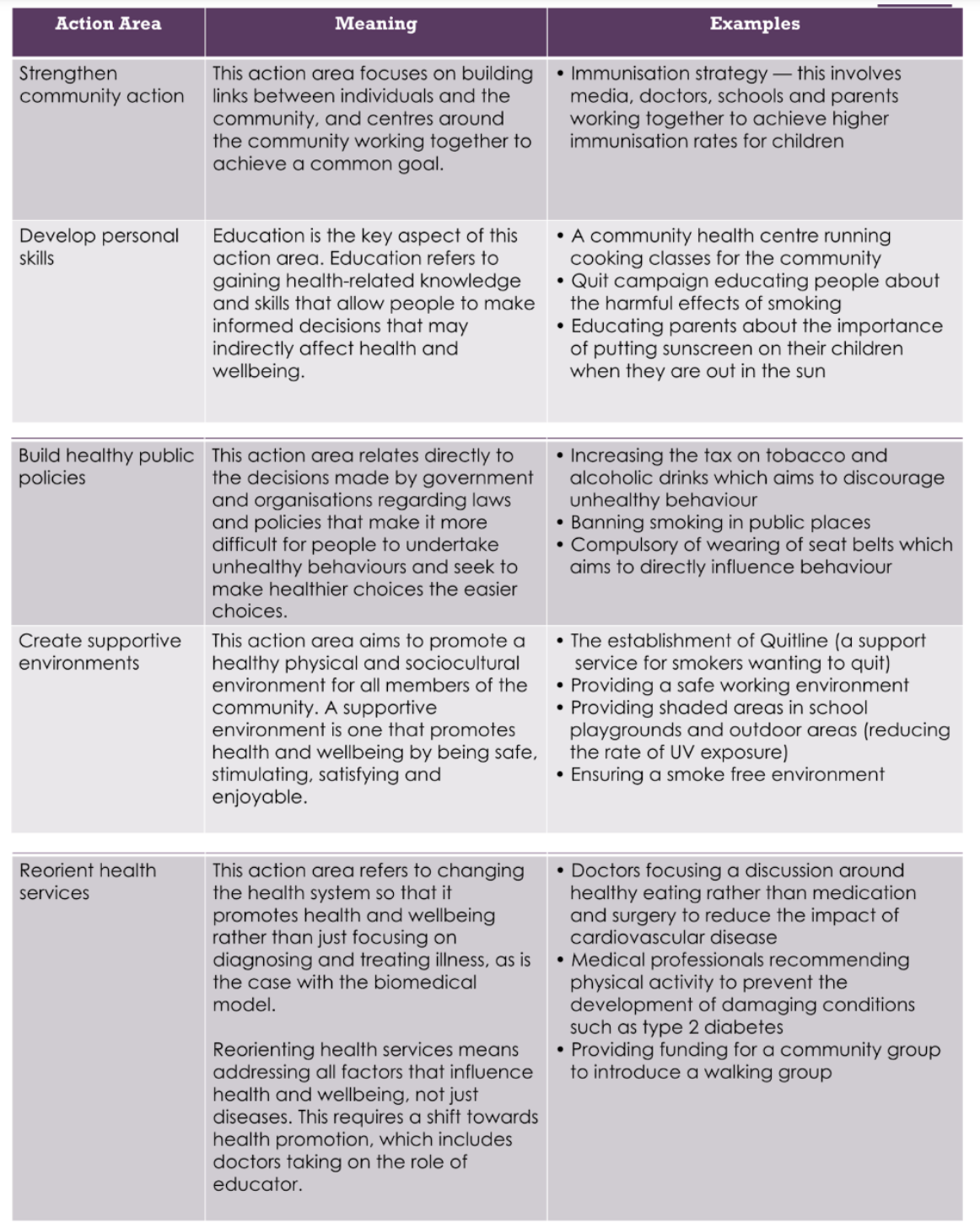
strengthen community action
focus on building links bw individuals + community to achieve common goal
Aboriginal Quitline strengthens community action by using Aboriginal quit specialists with additional training to assist people with smoking cessation in a culturally appropriate way.
Quit Victoria is a joint venture between the Victorian Government, VicHealth, the Heart Foundation and the Cancer Council.
develop personal skills
education gaining health-related knowledge + skills allow people to make informed decisions that indirectly affect h+w
National Tobacco Campaigns work to educate the population on the dangers and consequences of smoking. A recent campaign is the ‘Don’t make smokes your story’.
Quit provides information regarding tobacco smoking and the benefits associated with not smoking. This is achieved through a mass advertising campaign and via downloadable information on its website.
build healthy public policies
direct decisions made by governments regarding laws and policies that make it more difficult for people to undertake unhealthy behaviours and seek healthier choices
Anti-smoking laws and taxes work to make not smoking the easier and healthier choice.
Quit provides advice to the state government to implement legislation related to smoking.
Examples of policies include laws relating to smoking in public places, tobacco advertising, the display of cigarettes in retail outlets, tobacco packaging and tobacco taxes.
Increasing tax on tobacco banning in public places
create a supportive environment
that aims to promote physical and sociocultural environment promote h+w by being safe + enjoyable
National Tobacco Campaigns provide information on how to access resources to assist in quitting at no cost.
My QuitBuddy allows users to record personal goals and motivation using pictures, words and audio messages. There is a community board where users can gain motivation and support from thousands of other people quitting.
reorient health service
change health system so it promotes h+w focus on diagnosing and treating illness
Quit invests millions of dollars in smoking prevention research. This research then provides best practice techniques for health professionals in assisting preventing people from starting smoking and assisting smokers to quit.
Quit provides a free online learning training program for health professionals. Quit Victoria’s Smoking Cessation Essentials course and Smoking Cessation Brief Intervention videos provide health professionals with knowledge and skills relating to assisting smokers to quit.
initiatives addressing indigenous H + W
closing the gap
The Council of the Australian government include Australian, state, territory and local government representative along with indigenous leaders
agreed to ‘work together to achieve equality in health status and life expectancy between Aboriginal and torres strait islanders peoples and non-indigenous Australians by the year 2030
represent healthy public policies
2031, close the gap in life expectancy within a generation
increase the proportion of Aboriginal and Torres Strait Islander babies with healthy birth weight, employment, education, housing, reduce abuse, suicide
eg.
The deadly choice initiative: create supportive environments- The Deadly Choices program provides culturally appropriate healthcare using people from the local community.
learn to earn legend: Learn to Earn Legend! is strengthening community action as it is delivered by community leaders, sports stars and local community members whom young Aboriginal and Torres Strait Islander people respect and aspires to emulate.
2 Spirits program: develop personal skills- community forums focusing on HIV/AIDS, sexual health and wellbeing, injecting drug use, discrimination and sexuality issues. These forums increase knowledge and understanding within Aboriginal and Torres Strait Islander communities.
Evaluating initiatives about their capacity to improve Indigenous health and wellbeing
1. Actual improvements in health and well-being that have been made as a result of the initiative —
effective initiatives conduct research to determine the level of success achieved.
evidence of the actual successes of the initiative and the improvements to health and wellbeing
2. The number of people who have accessed or been involved in the initiative —
many programs keep records of the number of people taking part.
An increase in participants over time and/or participants taking part over an extended period can indicate that the target audience is engaged with the initiative, assisting in achieving its goals.
3. Feedback provided by participants —
those taking part in the program often provide information on their personal experiences which can indicate their success in promoting Indigenous health and wellbeing.
4. Action areas of the Ottawa Charter that are evident in the initiative, including:
develop personal skills through the provision of education — education is a resource that people can use to promote their health and well-being long after the program finishes.
strengthen community action by the involvement of various stakeholders and other concerned groups in the planning and implementation of the initiative — when various stakeholders are involved in the planning or implementation of the program, each can bring their strengths and expertise, contributing to the success of the program.
5. Whether the initiative is culturally appropriate for Indigenous Australians-
including consultation, use and training of Indigenous personnel in planning/delivering the program.
Indigenous culture is a strong influence in the lives of many Indigenous Australians.
Ensuring interventions are culturally appropriate can assist in increasing participation in the program/improving health and well-being outcomes.
6. Whether the initiative has taken the specific needs of the target group into account-
including the specific needs relating to the health and well-being of Indigenous people.
significant gains in health outcomes occur when the areas requiring the most attention are the focus.
7. Funding that has been provided to implement the initiative —
most interventions require some sort of financial support to ensure they are planned and implemented appropriately.
The provision of adequate funding, therefore, assists the intervention in achieving its goals.
8. Whether the initiative addresses a significant health issue for Indigenous Australians-
why it is important to address this issue.
For example, food intake is a key contributor to negative health and well-being outcomes for many Indigenous Australians.
Focusing on this factor can therefore contribute to significant improvements in health and well-being for Indigenous Australians.
 Knowt
Knowt
