Chapter 11 Human Physiology
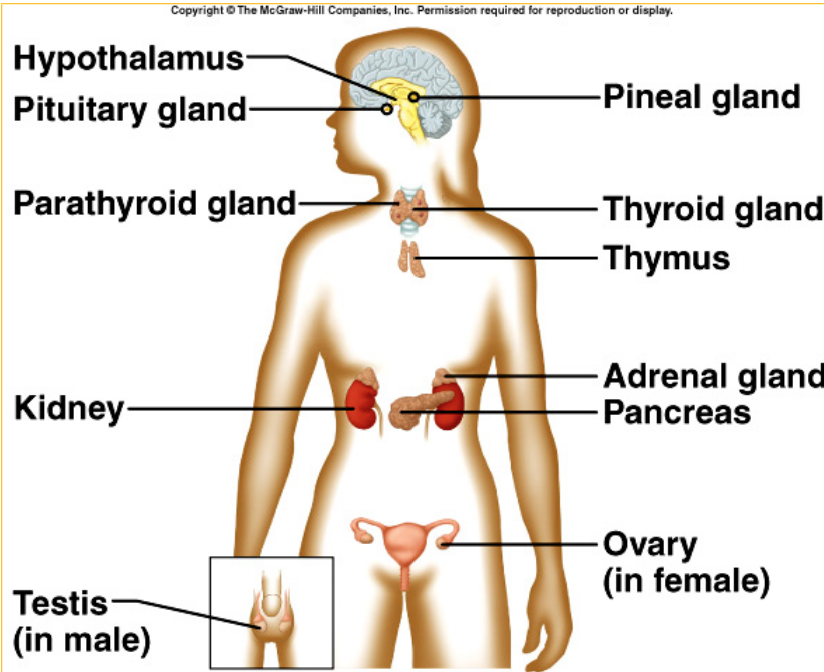
Endocrine System Overview
Introduction
- The function of the endocrine system is to provide a method of communication across the body
- The four structural components of the endocrine system are the endocrine glands, hormones, blood, and target cells
- The effectors of the endocrine system are the target cells
- Endocrine glands: Ductless organs or groups of cells that secrete hormones directly intothe blood or other body fluids
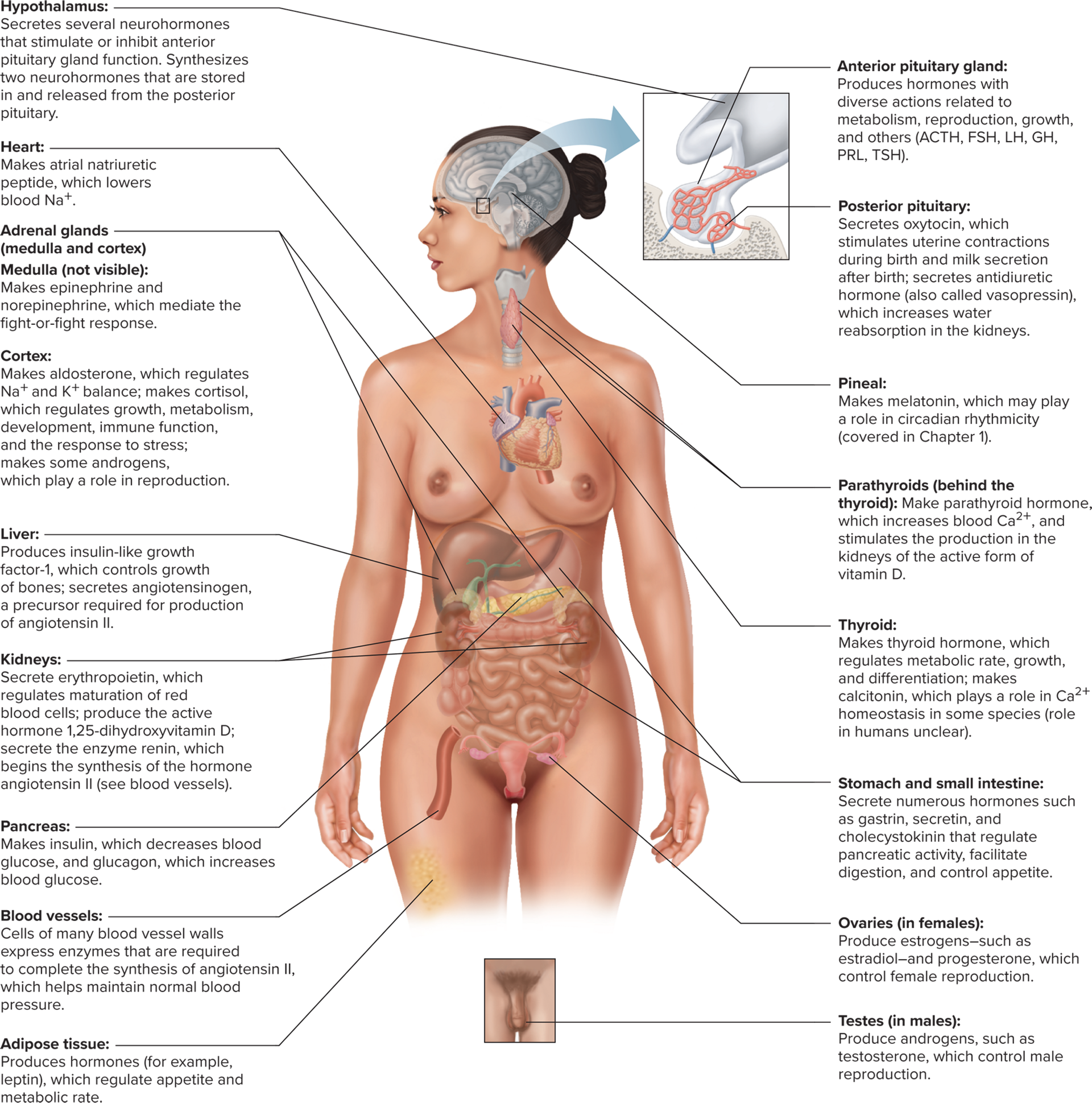
- Hormonal control systems help regulate homeostasis, stress responses, growth, and reproductive function
- True: T or F, A single gland can secrete more than one hormone
Structural Classes of Hormones
- The three major structural classes of hormones are amines, peptides/proteins, and steroids
- Amine Hormones
- Amine: Hormones derived from the amino acid tyrosine
- Amine hormones include thyroid, catecholamines, and dopamine
- Thyroid hormones: Amine hormones from the thyroid gland
- Catecholamines: Amine hormones form the adrenal medulla, such as epinephrine
- Dopamine: An amine hormone secreted by the hypothalamus
- Peptide/Protein Hormones
- Peptide and protein hormones are the most numerous class of all hormones
- Peptide and protein hormones are primarily polar molecules
- Synthesis
- Polypeptides are packaged into preprohormones by the rough ER, then into prohormones by the Glogi apparatus, and then the hormone is secreted by exocytosis
- Steroid Hormones
- Steroids: Hormones synthesized from cholesterol by gonads, adrenal cortex, and the placenta
- Steroid hormones are secreted via diffusion through the plasma membrane once they are made
- Steroid hormones circulate in the plasma and they are bound to plasma proteins (aka albumin)
Hormone Synthesis
- Adrenal Glands: Paired glands that sit atop the kidneys and are known for hormone synthesis
- The adrenal glands have two separate areas, the adrenal medulla, and the adrenal cortex
- Adrenal medulla: A modified sympathetic ganglion that releases catecholamines in resposne to sympathetic activation
- The adrenal medulla releases about 20% norepinephrine and 80% epinephrine, which bind to adrenergic receptors
- Adrenal cortex: Outer region of the adrenal gland that produces steroid hormones
- Aldosterone: A mineralocorticoid that regulates sodium, potassium, and hydrogen ions to help with water balance; relelased by the adrenal cortex
- Cortisol: A glucocorticoid that regulates metabolism of glucose and other nutrients to deal with stress response; released by the adrenal cortex
- Adrostenedione: A less potent version of testosterone, used in sexual development; released by the adrenal cortex
- The gonads (the testes and ovaries)
- Gonads: Produce steroids that are important for sexual development and reproductive function
- Testes: Mainly secrete testosterone and small amounts of estrogens; often converted to estradiol in target tissues by way of aromatase
- Aromatase helps convert testosterone into estradiol
- Ovaries: Secrete estradiol (estrogen) and small amounts of testosterone, as well as progesterone
- Progesterone can be secreted by the corpus lteum in ovulation or the adrenal cortex
Hormone Signaling & Action
Hormone Transport in Blood
- The structural components of the endocrine system are endocrine glands, hormones, blood, and the target cells (effectors)
- Catecholamines & protein hormones are water soluble and are easily transported by being dissolved in the plasma after being released during exocytosis
- Steroid hormones are nonpolar, so they attach to plasma proteins (in a hormone-protein complex) to travel through the blood after being secreted via diffusion
- Most hormones are bound to carrier proteins, but a very small amount are not. This free hormone concentration is what ends up binding to receptors in target cells.
- Some of the protein bound hormones in the blood dissacociate to reach receptor cells
- Plasma hormone concentration is affected by the rate of secretion into the blood and the rate of removal from the blood
- Rate of Removal
- Hormone removal from the blood is called hormone clearance
- Hormones that bind to the receptor end up decreasing the free hormone concentration
- Hormone clearance occurs in the liver and the kidneys
- In the blood the rate of removal of free proteins happens by enzymatic breakdown or binding
- Catecholamines take minutes to hours to break down (free hormones, so not as protected)
- Steroids and thyroids can stay from hours to days (why? they’re bound to transporters so they’re protected)
- Hormones can be activated by metabolism to increase binding to receptors
Hormone Action
- All tissues are exposed to circulating hormones, but only ones with the hormone receptor will respond
- Non-polar chemical messengers can bind to intracellular receptors after diffusing through the cell membrane
- Polar chemical messengers must have receptors built into the cell membrane
- Methods of regulating hormonal response
- Number of receptors (if a gland oversecretes, the target cells would down-regulate the receptor building so there isn’t too much taken in)
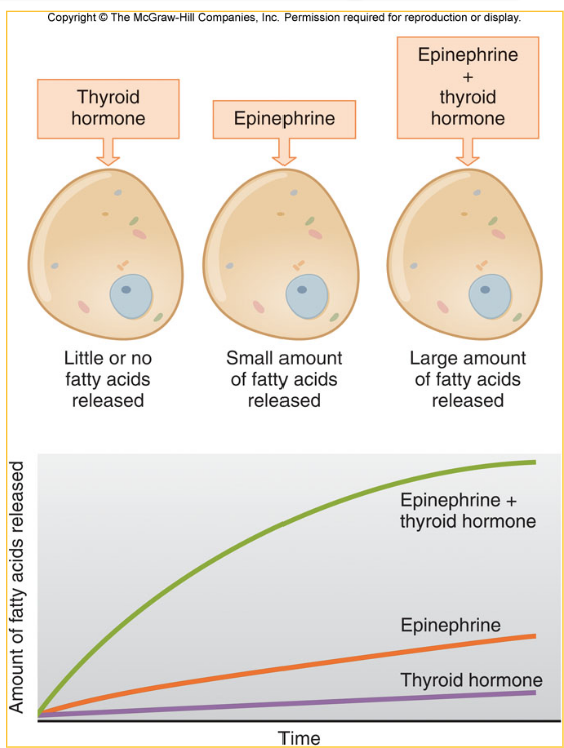
- Permissiveness: An up-regulation of the number of receptors for one hormone due to the presence of the second hormone, allowing for a larger response
- Cellular effects of polar hormones
- Catecholamines and peptide hormones cannot cross the cell membrane, so the receptor must be built into the cell membrane
- Most polar hormones activate a second messenger system upon binding to a receptor
- Polar hormones have fast, non-genomic effects (aka changing enzyme activity)
- Non-genomic: Effects of a hormone that have short-term effects, and the components are already built within the cell
- Less frequently, polar hormones can have longer-lasting genomic effects that do affect transcription
- Cellular effects of non-polar hormones
- Steroid and thyroid hormones bind to intracellular receptors after diffusing through the cell membrane
- Steroid and thyroid hormones form a hormone-receptor complex when the hormone binds inside of the cell
- The hormone-receptor complex of non-polar hormones act as a transcription factor
- Less frequently, non-polar hormones can bind to plasma membrane receptors to exert non-genomic effects
Control of Hormone Secretion
- Hormone secretion is regulated by changes in plasma concentration of subsances, neurotransmitters released by neurons synapsing upon endocrine cells, or other hormones
- Humoral Control: A modality of control for homone secretion where ion/nutrient concentrations within the blood act as the stimulus for hormone release
- Neural Control: A modality of control for homone secretionl where neurotransmitter release from the autonomic nervous system can influence hormone release from many endocrine glands
- Hormonal Control: A modality of control for homone secretion where one hormone can signal the release of a second hormone from a different endocrine gland
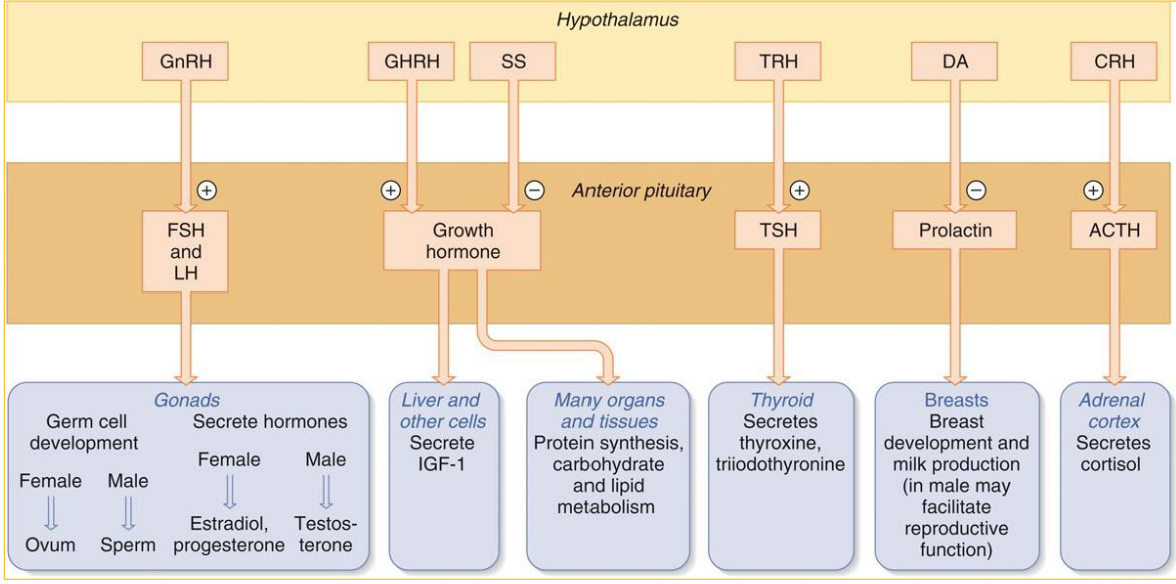
- Tropic: The hormone that singals the release of a second hormone from a different endocrine gland
Hormone System Regulation & Endocrine Disorders
The Hypothalamus & Pituitary Gland
- The hypothalamus is part of the diencephalon & works with the pituitary gland
- Infundibulum: The pituitary gland and the hypothalamus are connected by this tissue.
- The infundibulum includes axons and mood vessels to connect the hypothalamus and the pituitary gland
- The anterior pituaitary glands have more emphasis on blood vessels for hormone transport
- Hypothalamus controls the release of anterior pituitary hormones via release of hypophysiotropic hormones
- Hypophysiotropic refers to hormones from the anterior pituitary gland that causes the release of another hormone
- Portal system: This modality includes veins are in between two separate capillary beds are portal veins that make up the system that supports hypophysiotropic hormone transport
- Pros of the portal system include that it’s faster & less diluted instead of travelling all the way through the heart and wait for a wrap around back to effectors
Three-Hormone System
- The first hormone in a three-hormone system is released from the hypothalamus and has a hypotropic effect on the anterior pituitary gland
- The second hormone in a three-hormone system is released from the anterior pituitary gland and effects the third gland
- The third hormone in a three-hormone system is released from a gland, that targets the effector
/
- Hypophysiotropic hormone secretion is controlled by neural inputs & influenced by sensory info, biological rhythms, and developmental stages
- Long-Loop: The third hormone in a three-hormone system can have a negative feedback on the hypothalumus or the anterior pituitary, also called negative feedback
- Short-loop: The second hormones can exert negative feedback on the hypothalumus, called _ negative feedback
Mechanisms of Endocrine Disorders
Hyposecretion issues
- Hyposecretion: There is a reduction in the amount of the hormone within the plasma, causing an impaired response
- Primary hyposecretion: The reduction of hormones in the plasma is caused by the hormone-producing gland (the third hormone in sequence), caused by destruction of the gland, enzyme deficiency, or dietary deficiency
- Secondary hyposecretion: There is too little stimulation by a tropic hormone, causing an unsafe reduction in hormone concentration; the second hormone is not doing enough so the final hormone cannot be released
- If there are high levels of the tropic hormone, the hyposecretion is probably primary
- If there are low levels of the tropic hormone, the hyposecretion is probably secondatry
Hypersececretion issues
- Hypersecretion: Increased circulating hormone concentrations
- Primary hypersecretion: The gland is producing too much hormone
- Secondary hypersecretion: Excessive stimulation by the tropic hormone on the final hormone producer
Hyporesponsiveness issues
- Hyporesponsiveness: The cell has a diminished response to hormonal inputs, despite a proper amount of hormone being present
- Hyporesponsiveness can be caused by not enough receptors, dietary issues, or the signal transduction mechanisms
Hyperresponsiveness issues
- Hyperresponsiveness: The cell has a very much increased response to hormonal inputs, although hormone levels are normal