Pathology of the Kidneys and Upper Urinary Tract
Hydronephrosis Causes
Blockage: Blockage of urine flow down the ureter.
Internal Blockage:
Calculi (kidney stones)
Scarring in the ureter
Tumors blocking the vesicoureteric junction (VUJ)
External Blockage:
Mass effect compressing ureter
Vesicoureteric Reflux:
Failure of bladder to empty properly
Common in babies and young children
Can be unilateral or bilateral
Urine flows back from bladder to kidneys, which can lead to infections and damage.
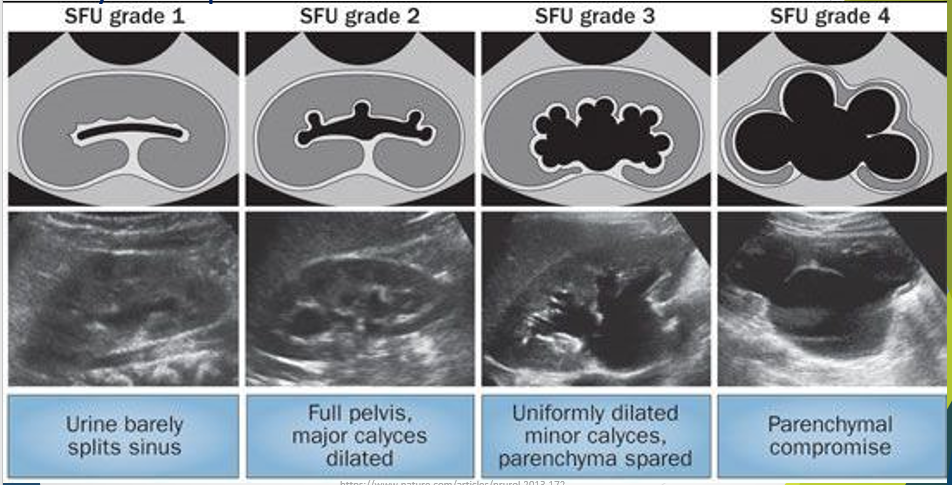
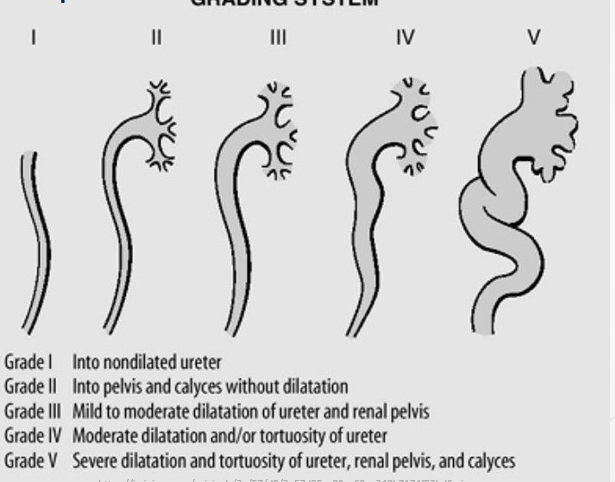
Hydronephrosis Grading System
Grade I: Into nondilated ureter.
Grade II: Into pelvis and calyces without dilatation.
Grade III: Mild to moderate dilatation of ureter and renal pelvis.
Grade IV: Moderate dilatation or tortuosity of ureter.
Grade V: Severe dilatation and tortuosity of ureter, renal pelvis, and calyces.
SFU Grading:
1 and 2 mild, 3 moderate, 4 severe
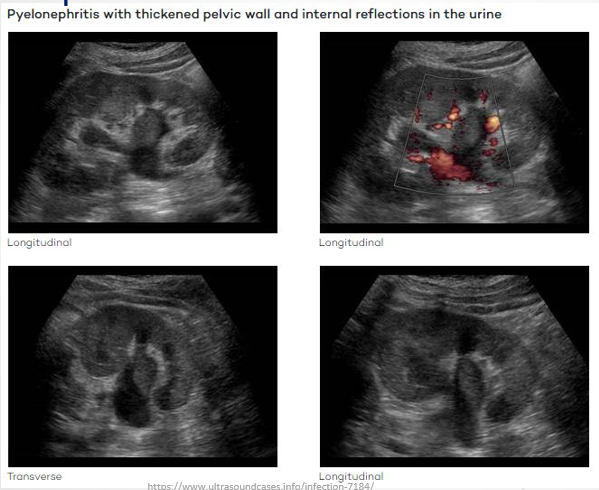
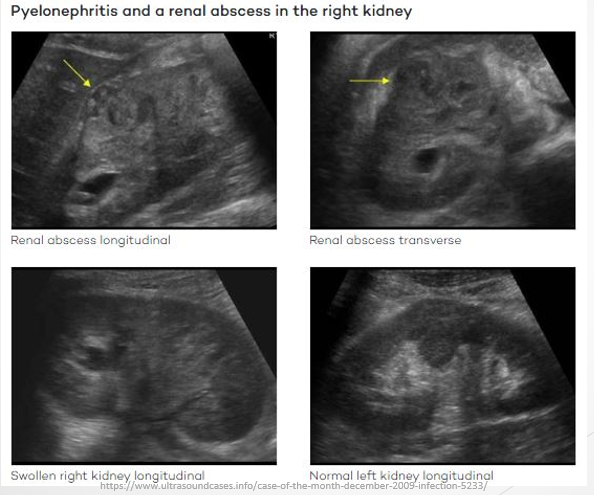
Pyelonephritis
Definition: Urinary tract infection that originates in the urethra or bladder, traveling to the kidneys.
Causes: Mainly caused by Gram-negative bacteria (e.g. E. coli) from fecal matter.
Symptoms:
Fever
Nausea
Frequent urination
Pain in back, side, or groin
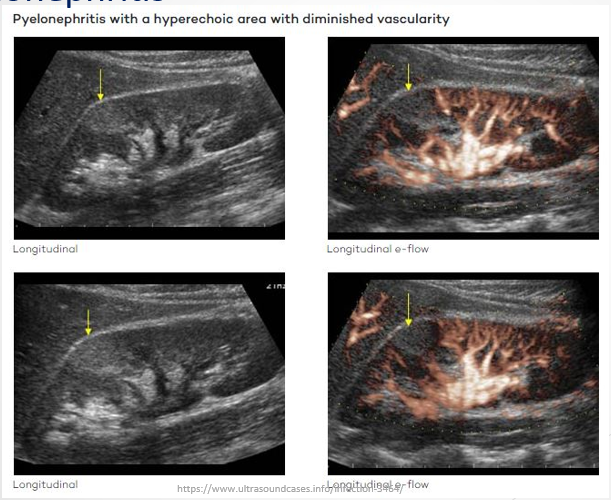
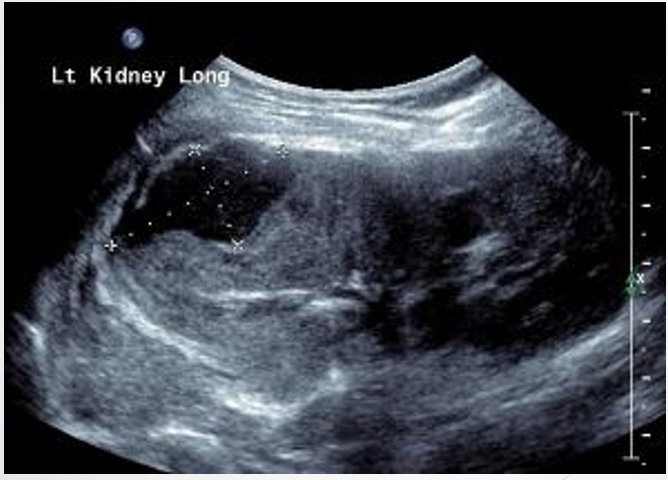
Sonographic Presentation:
Can affect one or both kidneys.
Can be focal or diffuse.
Echogenic wedge defect in partial cases. - not the same as the congenital defect
Loss of blood flow seen on colour Doppler.
Renal Abscess
Definition: A complication arising from pyelonephritis.
Types: Both start with tubular necrosis
Renal Abscess: Forms a distinct walled-off cavity.
Perirenal Abscess: Appears more diffuse between renal capsule and fascia.
Perirenal Abscess
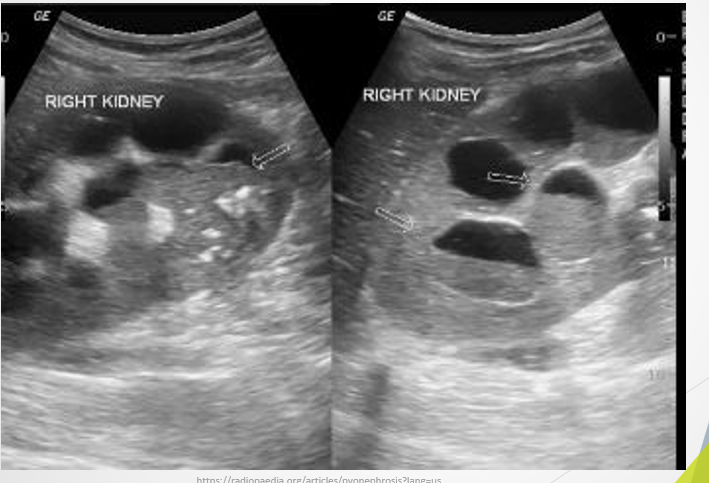
Pyonephrosis
Definition: Presence of pus, debris, or haemorrhage within a dilated pelvicalyceal system.
Sonographic Appearance:
Echoes within pelvicalyceal system.
May appear solid.
Can sometimes get layering - like sludge in the GB
Put colour on to see if it moves
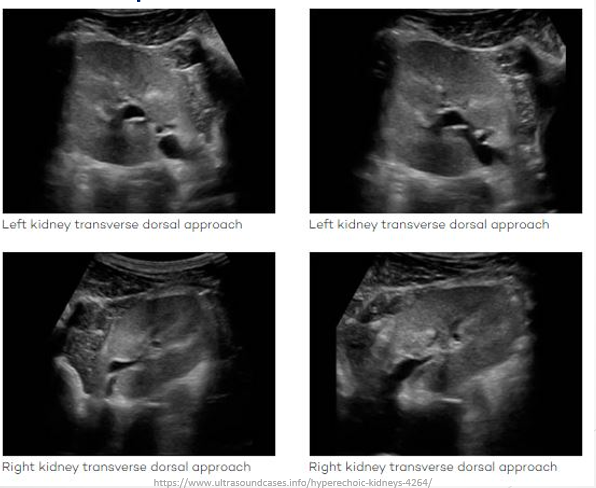
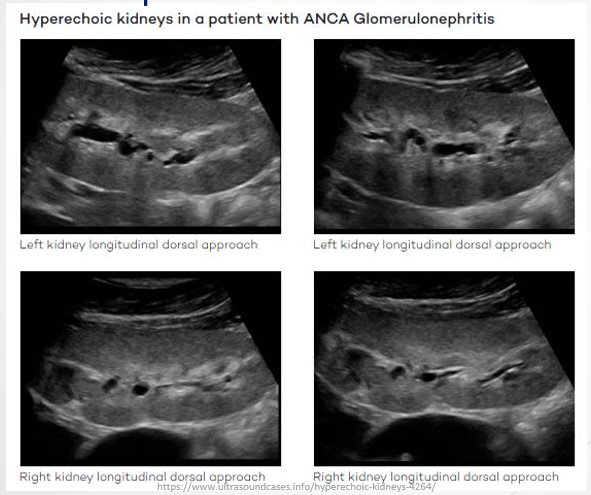
Glomerulonephritis
Definition: Inflammation of the glomeruli; acute or chronic.
Implications: Usually affects both kidneys; early diagnosis and treatment are vital to prevent renal failure.
Causes: Can arise from staphylococcal infections or immunologic illnesses.
Sonographic appearance: hyperechoic kidneys, collecting system not dilating
Key to distingush between pyelonephritis and glomerulonephritis would be patient hx - urinary infection (pyleonephirits)
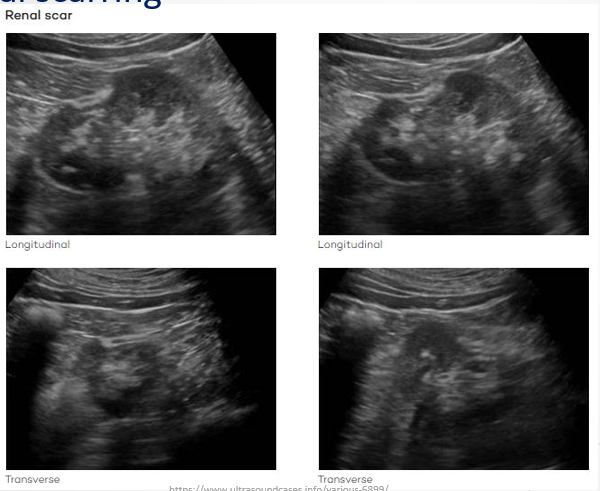
Renal Scarring
Causes: Usually due to recurrent UTIs, reflux, or pyelonephritis.
Effect: Causes permanent damage to renal parenchyma and reduces kidney function.
Sonographic Signs: Appears atop medullae, not between them; shows thinned parenchyma; fat fills the spot where the scarring occurs, which can lead to a characteristic echogenicity, indicating loss of normal renal architecture.
Renal Atrophy
Definition: Kidneys are smaller than expected for a person's age and height.
Causes: Can be congenital (renal hypoplasia) or acquired due to chronic infections or hydronephrosis.
Significance: Congenital cases typically do not require treatment unless parenchyma thickness is abnormally smaller
Acquired due to lower blood supply to the kidneys and or loss of nephrons

Renal Failure
Definition: End-stage kidney disease (ESKD) where kidneys cannot adequately filter blood or control bodily fluid levels.
Progression: GFR decreases significantly, with ESKD being defined as GFR <15 ml/min.
Sonographic Features:
Acute: Size may appear normal or enlarged with hypoechoic areas.
Chronic: Small, echogenic kidneys with structural abnormalities.
Duplex Kidney Pathology
Definition: Characterized by the presence of two collecting systems or ureters.
Anatomical Variations: Ureters may join before the bladder or have separate openings.
Issues: Ectopic ureters are more susceptible to reflux due to abnormal placement, leading to hydronephrosis, particularly in the upper moiety.
Sonographic Considerations: Identifying the location and functional status of both moieties is crucial.
Review Points
Describe pathologies using appropriate sonographic terminology and distinguish differential diagnoses.
Detail sonographic features of varying grades of hydronephrosis.
List and explain pathologies encountered in duplex kidneys using sonographic terminology.