GI Tract Pathology
Pre-Knlowge of GI Tract
- the diaphragm separates the esoágues from the stomach
- parietal cells produce HCl and KCl (gastric acid) and excrete it in gastric glands
- What happens when someone vomits for days?
- hypochloremic (hyper chloride) in blood
- lower pH in the stomach
- PAS staining
- Staines the lining of the mucus → polysaccharides
- Bolus moves passively and actively through the esophagus( peristaltic movement)
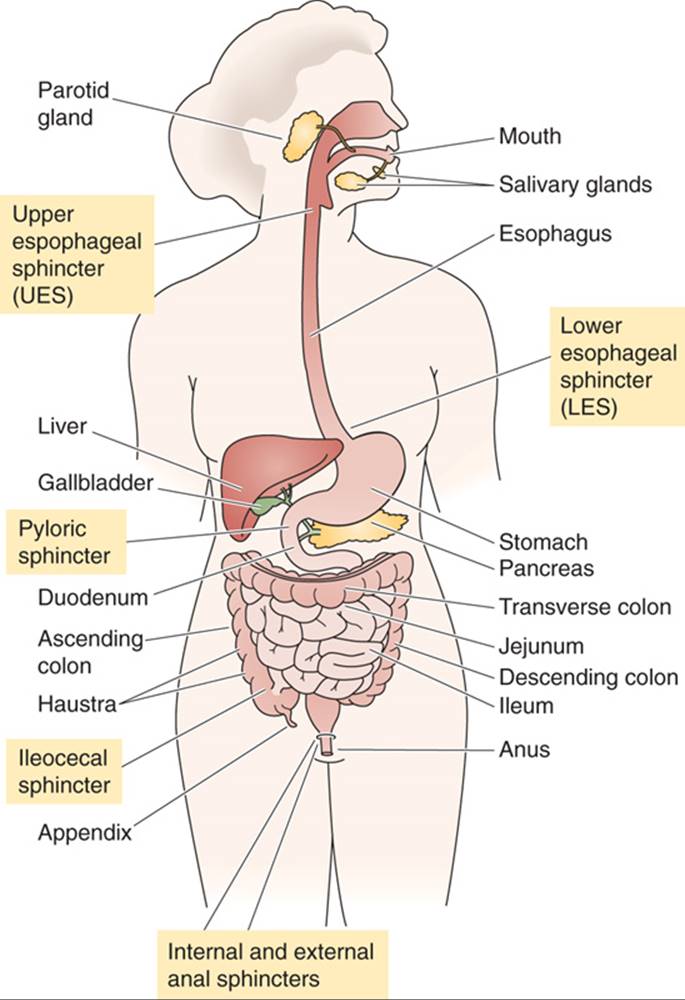
- Different squinters in GI tract
Functions and Characteristics of the GI tract
- %%Small intestines%% → absorption of carbohydrates, fats, minerals, proteins, water, and vitamins.
- %%Colon%%: absorption of water and electrolytes
- Peyers patches →patches of immune cells that are found in ilium that detect and respond to foreign substances
- most bacteria found( digest found + ferment food)
- %%Appendix%%: stores immune cells
| GI Tract Structure | Villi* | Crypts of Lieberkuhn** | Goblet Cells*** | the cell type that lines the surface |
|---|---|---|---|---|
| %%Esophagus%% | Absent | Absent | Absent | squamous cells**** |
| %%Stomach%% | Absent | Present in Gastric Glands | Absent | columnar cells ***** |
| %%Small Intestine%% | Present in the mucosa of the jejunum and ileum | Present | Present in the mucosa | columnar cells |
| }}%%Large Intestine%%}} | Absent | Present in the mucosa | Present in the mucosa | columnar cells |
*Villi: finger-like projections on the surface of the mucosa that increase the surface area for nutrient absorption to the lymphatic system and capillaries
→ they also have mussels to move bolus muscles
**Crypts: small tube-like structures that are located in the lining of the small intestine and the large intestine, produce digestive juices + harbor stem cells for epithelial lining
***Goblet cells: goblet cells secrete mucus that protects the mucosa from damage
**** Squamous cells: are flat and often found in barrier tissues
***** Columnar cells: are taller and typically found in tissues with secretory or absorptive functions.
Pathology of esophagus
- %%Heartburn%%
- normally prevented by the angle of the stomach and lower esophageal sphincter(LES)
- gastroesophageal reflux disease→ Barret disease of the esophagus (damaged and replaced by abnormal cells. This is usually caused by long-term acid reflux and is a risk factor for developing esophageal cancer)
- %%Eosinophilic esophagitis%%
- allergy in the esophagus and a lot of eosinophils → rectaion to what pathogen is unclear maybe food
- %%IBD%%:
- ==Two types of IBD== (systematic disease) → due to a genetic defect, all leukocytes attack microbes and food
- the peak of onset 20 and 60 → 25% of all IBD start in childhood !!!
- symptoms come in waves and increase over a lifetime
- loss of tolerance**
- impairment of mucosal defense
- epithelial barrier defects
- Environmental factors:
- The earlier the onset, the more genetic the IBD
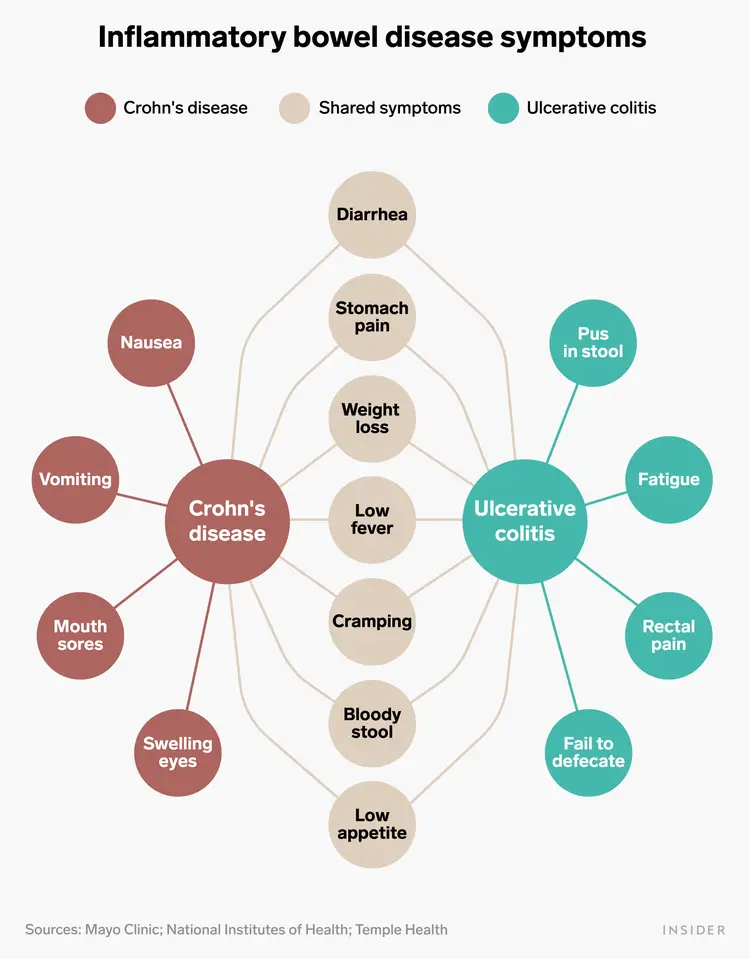
- Crohn’s disease
- vomiting
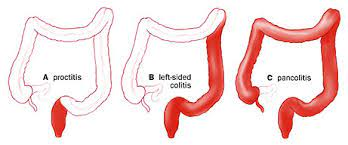
- Ulcerative colitis
- only concerns the colon → a lot of rectal symptoms that crawl upwards
- (difficult to diagnose because they look so similar (diarrhea with blood+ cramping + fever), but they are very different to treat
- red blood → inflammation colon
- black blood → small intestine
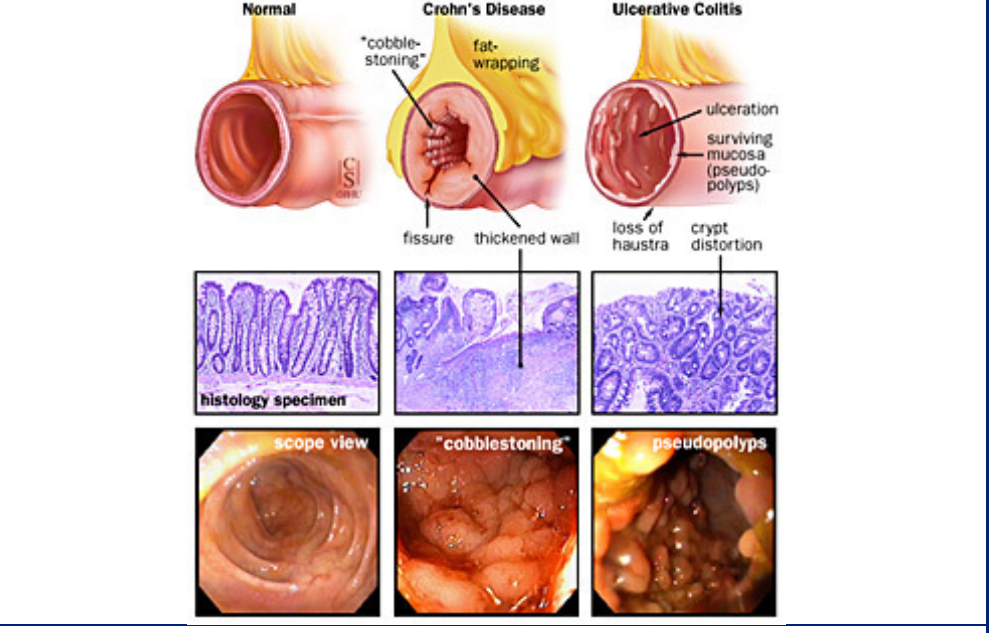
- ==Things that are specific to each disease==
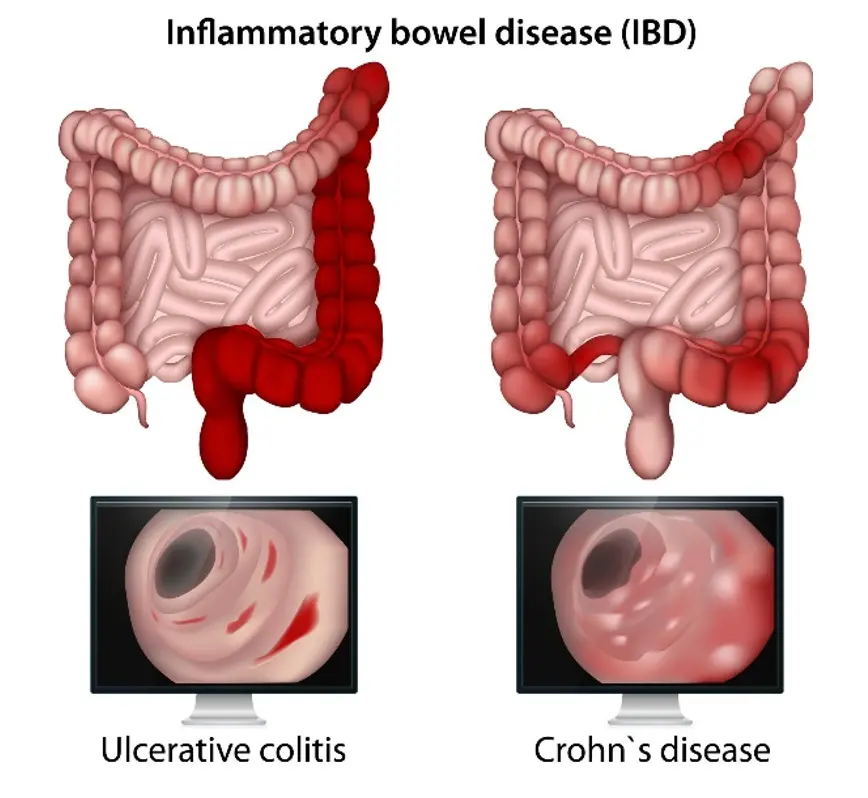
- Crohn’s
- the disease can skip passages in the colon and cause inflammation → patchy inflammation
- Fistulas: abnormal passageways that form between different parts of the body
- → transmural ( tears through the tissue of them muscle) inflammation → feces can end up in urine
- granulomas: clusters of cells that form when the body's immune system attempts to contain and eliminate foreign substances or bacteria
- muscle hypertrophy
- cobblestone appearance
- fat wrapping
- serological marker: ASCA
- @@Ulcerative colitis@@
- crypt distortions
- always originates in the rectum and then moves up until half of the colon or the entire colon
- serological markers: pANCA
- ulceration within the mucosa
- in children it does not have to start in rectum
- {{Manifestation of IBD{{
- code in the lymph node that triggers an intestine attack
- you can only have skin irritation and no intestine → due to gene alteration
- because innate immune system is not working( NOD 2 intracellular bacterial receptor) there is an overload of B and T cells → underlying explanation of IBD
- **Tolerance in immunology
- there is recognition of everything in our body by the immune system; in a normal state, there is a tolerant state; however, in IBD there is a loss of accepting new things
- inflammation vs. tolerance ( too much aggressive inflammatory cells or too few protective cells)
- }}Treatment options}}
- take out the colon in colitis to decrease inflammation →; however, inflammation will always stay because you can’t take out return
- in crohns you can’t take out the colon because inflammation will continue in small intestines
- steroids
- targeted immunosuppression for specific immune cells