Pharm Test 1
Examine the basics of medication administration including nurse responsibilities, acceptable practice, rights of administration, types of prescriptions, and prescription components.
“Nurses are responsible for preparing and administering medications, which involves using technical skills and clinical judgment. Prior to administering any medication, it is important to understand the client’s medical condition and medication history (what currently taking? any interactions? any allergies? any assessments?)”
“The nurse is responsible for having up-to-date knowledge about medications. This includes knowing the purpose, mechanism of action, route of administration, safe dosage range, side effects, adverse effects toxic responses, precautions, and contraindications for each medication you administer.”
“Nurses also need to know about the legal implications of medication administration. The state boards of nursing regulate the scope of RN and PN practice through nurse practice acts. The components of te nurse practice acts vary by state, so familiarize yourself with the practice requirements and limitation for your level of practice within the state in which you are licensed.”
“Professional standards are in place to ensure medication administration is performed safely. The include the rights of administration. Failure to comply with these standards can result in charges of negligence or malpractice.”
“Always apply the rights of medication administration when administering medications. This is for client safety. These include the right client/ medication/ route/ dose/ time/ documentation/ assessment/ education/ evaluation/ refusal”
“Always make sure to administer the medication to the right client using at least two forms of identification to verify that you have the right client. These include name, DOB, MRN”
“Make sure to compare the identity with the MAR”
“The nurse assesses the client before administering the medication for contraindications, pertinent lab results, vital signs, allergies, and possible medication interactions to determine if the client requires the medication and if it is safe to administer it.”
“Follow several steps using clinical judgment to make sure you administer the right medication.Read the prescription carefully. Ask yourself if it makes sense for the client to receive this medication based on the client’s condition and diagnosis.
Compare the prescription with the medication administration record (MAR) three times—before obtaining the medication, when removing it from the container, and at the bedside right before administering it.
Look at the expiration date on the packaging. If the expiration date is in the past, the medication may no longer have its therapeutic effect, and it could harm the client.
If you are unfamiliar with the medication, consult a medication guide or a pharmacist to learn essential facts about it.”
“Many medications are available for administration via more than one route. Always use the route intended by the provider. Compare the label on the medication container with the prescription to verify the route. If the prescription does not include a route or the route is inappropriate for the client, clarify with the provider what route to use. Be especially careful with liquid medications. Make sure to give enteral preparations only orally or via enteral tubes and parenteral preparations only via injection or infusion.”
“Administer medications at the right time. This could be at specific intervals or at a time of day that the prescription specifies, such as at bedtime.”
“For routinely scheduled medications, the facility will provide parameters for the time frame in which to administer the medication, such as 1 hour before or after the scheduled time.”
“Time-critical medications (insulin, antibiotics) should be administered within 30 minutes of their scheduled time. Give medication that is prescribed before meals (AC) or after meals (PC) within 30 minutes of a meal. Administer a stat medication right away.”
“Ensure the right dose by checking the prepared dose against the prescription. Also, review a medication reference to ensure that it is an appropriate dose for the client. If you have any questions, clarify the dose with the provider. For example, is the dose beyond the usual range for this medication? Should the dose be lower because the client has a kidney or a liver disorder?If the dosage needed is different than the amount or strength provided by the pharmacy, the nurse might need to perform conversions or calculations to prepare the medication. Have a second nurse verify the calculations prior to administering the medication. Always double-check the math if the answer indicates administering a particularly large number of pills or volume of liquid.”
“Documentation of medication administration should occur immediately after administration. Do not document the medication on the MAR until it has been given in case the client refuses it. If it is not documented promptly, another nurse could think the client has not yet received the medication and administer another dose. It is also important to determine the time the last dose of the medication was administered. Follow facility guidelines for documenting information on the MAR and indicating that you gave the medication.”
“If the medication is PRN, the exact administration time should be entered in the MAR. In addition, the nurse should note in the client’s medical record why the PRN medication was administered and an evaluation of the effectiveness of the PRN medication.”
“Routine medications are prescribed for a specific time or frequency. For example, they may be prescribed daily, twice per day, three times per day, four times per day, at bedtime/hour of sleep, every other day, weekly, or monthly.”
“Standing prescriptions are protocol-based and contain a list of directives to implement in specific situations. For example, a critical care unit has standing prescriptions to treat a client who has asystole. Standing prescriptions can include regular, single, and PRN prescriptions and actions other than medication administration (diet, ambulation parameters, treatment). They can have a fixed end date and require renewal or remain in place until the provider changes them or the client is discharged. Assess the client frequently to determine whether standing prescriptions remain appropriate.”
“Single prescriptions are one-time doses, such as those seen with preoperative medications.”
“A stat prescription is implemented immediately one time. Providers generally prescribe stat doses in emergency situations. Document the exact time you administer the stat medication on the MAR. Stat prescriptions should be administered within 30 minutes of the provider placing the prescription.”
“A PRN prescription specifies the medication, dose, route, frequency, and reason indicating its implementation. An example of a circumstance is pain or temperature greater than a specified measurement. Use clinical judgment and the client’s subjective report, such as pain level or vital signs, to determine the appropriateness of administration. Document the indication for administering the medication along with the time and other required data.”
“Urgent, now, or ASAP (as soon as possible) prescriptions should be administered within 30 minutes to 1 hour after the provider’s prescription.”
“The components of a medication prescription can vary slightly with each facility. In general, a medication prescription includes the following.Date and time the prescription was written
Client’s full name
Name of the medication
Indication
Dose: amount, times or frequency of administration, and strength
Route of administration
Dispensing instructions related to quantity, directions for the client, refilling parameters, and any special cautions (such as to not take with food)
Provider’s signature”
Identify the steps of the nursing process: assessment and data collection, planning, implementation, and evaluation.
Assess: “During the assessment or data collection phase, gather all of the client's information about medication administration. This includes the client’s current status and history. Prior to administering some medications, the nurse might need to check the client's vital signs. Withhold the medication if vital signs are not within a specific range. The nurse might also need to monitor laboratory results, such as blood glucose or platelet count. This information can help you recognize cues that you may need to administer or withhold a medication based on parameters in the prescription. Check the client’s allergy record and medication record for possible interactions or contraindications. Make sure the medication prescription has all the essential elements and that you interpret the prescription accurately. Question the prescriber if you have any concerns.”
Diagnosis/Analysis: “Analyze cues to determine the indication for the medication to be administered to the client, identify any potential health problems based on assessment findings, and determine whether the medication and its prescribed dosage are appropriate for the client at this time.”
Planning/Solutions: “Avoid distractions when planning and preparing to administer medications. Interruptions during the medication process impact client safety, quality of care, and workload. Strategies to prevent interruptions can include designating the area around the automated medication dispensing system (AMDS) to prevent people from conversing with a nurse. Do not rush through the process or use workarounds when problems arise with the normal process of medication administration. Calculate and measure doses precisely. Use the prescribed strength.Identify goals and criteria for success related to the client’s needs. For example, if a client is starting a new prescription for insulin to be administered subcutaneously, the goals could include client teaching, demonstration for self-administration of the medication, and monitoring of blood glucose levels. Verify calculations for high-alert medications with another nurse and prioritize medication administration as needed. For example, administering a pain medication should become the priority if a client reports severe pain.”
Implementation/Action: “The implementation phase, taking action, includes correctly calculating dosages and providing instructions and information about the medication according to the client’s needs. Only administer medications that you prepare. Adhere to facility guidelines for the various routes of administration. Follow all laws and regulations for administering controlled substances. Delay administration if the client questions anything about the medication—such as its dose or appearance. The administration should be delayed until you can verify the prescription and alleviate the client’s concerns.”
Evaluation/Outcomes: “Evaluating outcomes occurs when you identify and document the client’s response to medications you administered. Is the medication having the intended therapeutic effect? Has the client developed any side or adverse effects? Are you aware of any errors in medication administration? If so, assess or collect data from the client and perform any necessary reporting and corrective actions.Include the client in the evaluation process. Ask the client to explain what they understand about their medication schedule and how to take them, especially if they are going home with a new prescription. Including clients encourages them to be more involved in their care.”
Examine common medication errors.
“A medication error is a variation from what the provider intended for the client.”
“Common types of medication errors involve errors in medication administration. Examples include the following.Administering the wrong medication
Administering the wrong medication strength
Infusing the wrong IV fluid
Diluting the medication with the wrong solution
Calculating the dose or infusion rate incorrectly
Administering the medication to the wrong client
Administering a medication by the wrong route
Administering medication at the wrong time
Administering a medication when the medical record indicates the client is allergic to it
Omitting a dose
Administering a medication beyond its expiration date
Erroneously discontinuing a medication or an IV fluid infusion
Medication errors can occur at any time along the prescription continuum. Prescribing errors can occur if the provider prescribes an incorrect medication or dose. For this reason, it is vital that to check each prescription for accuracy. Know what the medication is indicated for and what the safe dosage ranges are.”
Recall where to find tools for safe medication practice, risk reduction, preventing medication errors.
“A variety of technological systems are available to help reduce the risk of medication errors. Automated medication dispensing systems and electronic medical records reduce manual errors in preparing medications and documenting their administration. Bar code scanning helps ensure adherence to the rights of medication administration.”
“The Institute for Safe Medication Practices (ISMP) is a nonprofit organization that educates providers and consumers about safe medication practices. A voluntary reporting system helps ISMP learn about errors and share how to prevent them.ISMP provides tools to reduce the risk of errors on its website.
Drug name suffixes
Tall Man letters:Tall Man lettering is the practice of writing medication names with a mix of upper- and lower-case characters. These characters highlight distinctions that help recognize them from look-alike medications.
High-alert medications: Some medications can significantly harm clients if received in error. Because they have the potential for serious consequences, exercise caution when administering them. Examples include anticoagulants, chemotherapeutic agents, opioids, and hypoglycemic medications.
Look-alike and sound-alike medications
Error-prone abbreviations
Recognize adverse reactions to medications.
“Every medication could result in an adverse effect. Adverse effects are undesired, unintended responses to medication. They can range from mild, such as drowsiness following the administration of an antihistamine, to severe. Severe adverse effects include dysrhythmias, severe colitis, and seizures. Anaphylaxis is a life-threatening allergic reaction to a medication and can result in respiratory and cardiovascular failure”
“Adverse effects can occur suddenly, shortly after the medication is administered, or over a longer period of time. Even clients who have been taking a medication for a while can develop an adverse effect.”Describe the role of the nurse and the patient in preventing medication errors.
Differentiate generic vs brand or trade names of drugs, and over-the-counter and prescription drugs.”
“a pharmacaceutical company develops a medicationa nd gives it an official name. That becomes the generic name of the medication. Generic names are not capitilized. The brand, or trade, name is a medication’s commercial or proprietary name, which is capitalized and may vary according to the company producing and marketing it.”
“There may be several different brand names for one generic medication, depending on the manufacture.”
“they have the same chemical composition, and there is no difference between the potential for abuse or dependence”
“The US Food and Drug Administration (FDA) conducts studies to make sure that each new generic medication has the same therapeutic equivalence as the original brand-name medication.”
“Pending approval from the client’s provider, the generic medication is interchangeable with the brand-name medication”
Ex: acetaminophen v/s Tylenol
“medications that require prescriptions are prescription medication while other nonprescription medications are available over-the-counter”
“The federal government identifies prescription medications as potentially harmful if there is no supervision of administration by a licensed health provider, such as a physician, nurse practitioner, or physician’s assistant.”
“over-the-counter medications do not require a prescription because they have a designation from the FDA that says they are relatively safe to take without supervision.”Explain the meaning of half-life of a drug.
“The half-life of a medication is the time it takes for a medication that enters the body to decrease in amount by half. This decrease reflects how quickly and efficiently a medication metabolizes and excretes. You might need to administer medications with a short half-life several times a day. Likewise, you might need to give medications with a long half-life only once a day. Since most medications are metabolized in the liver and excreted in the kidneys, clients who have decreased functioning in either of these organs may experience adverse and toxic effects of medication more easily if the provider does not adjust the dosage and frequency of the medication.”Explain pharmaceutics, pharmacokinetics, and pharmacodynamics.
“Pharmaceutics address how various medication forms affect the dissolution of a medication, the absorption rate of a medication, and, subsequently, its onset of action.”
“Many clients take medications by mouth; these are known as oral medications. These medications come in tablet, capsule, powder, or liquid forms. medications that a client takes through the mouth but inhales into the lungs, are usually in powder form. The form of an oral or inhaled medication influences its rate of absorption. Some oral medications come in forms that delay release of the medication. For example, enteric-coated medications, sometimes abbreviated as EC, dissolve when the medication reaches the intestine. Extended-release medications, sometimes abbreviated as ER, release over a period of time. Tablets that are scored, or marked with a line in the center, may be split. Although tablets may sometimes be crushed if a client is unable to swallow tablets and a liquid form of a medication is not available, capsules and extended- or sustained-release forms of medications should never be crushed.”
“You can administer parenteral, or injectable, medications one of three ways: intravenously into a vein, which is commonly abbreviated as IV; subcutaneously into subcutaneous tissue, commonly abbreviated as SUBQ; or intramuscularly into muscle tissue, commonly abbreviated as IM. The onset and absorption of parenteral medications vary depending on which method you use to give the medication. The absorption of intravenous medications is immediate and complete, resulting in an immediate onset of action. In contrast, the absorption of subcutaneous and intramuscular medications is variable. If the medication is water-soluble and the client has good circulatory blood flow and tissue perfusion, the absorption of the medication is rapid. If the medication either is not water-soluble or is poorly water-soluble, the absorption is slower. Also, if the client has slowed or impaired circulatory blood flow or tissue perfusion, the absorption of the medication is slower. Depending on the solubility of the medication and the client’s circulatory status, the onset of action for a subcutaneous or intramuscular injection varies.”
“Topical or transdermal medications are medications that you apply to a client’s skin, eyes, ears, nose, rectum, vagina, or lungs. Topical medications deliver a constant amount of the medication over an extended period of time, have a slower onset of action, and a longer duration of action than oral or parenterally administered medications.”
Pharmacokinetics= what the body does to the drug, “refers to how the medications travel through the body. They undergo a variety of biochemical processes that result in absorption, distribution, metabolism, and excretion (ADME)”
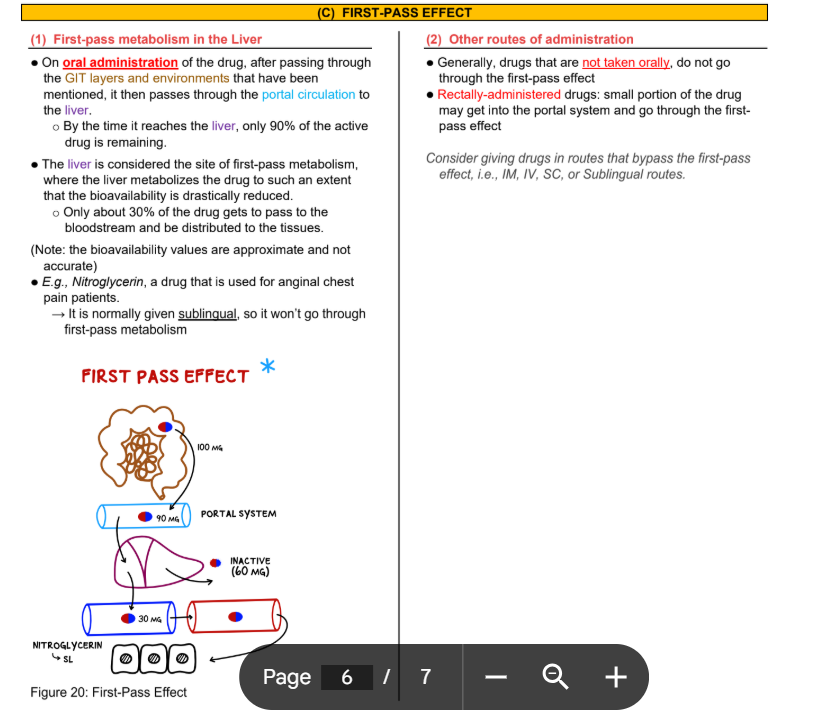
“Absorption is the movement of the drug from the site of administration to the various tissues of the body. For example, oral drugs must absorb through the intestinal wall and enter the portal vein before passing through the liver and into the body's circulation. Since part of the drug may deactivate when it passes through the liver, the actual amount available to the body can be less than what the client ingested orally.”
“Distribution is movement of the medication by the circulatory system to its intended site of action. Medications enter the blood after they absorb through the intestinal wall or alveoli in the lungs, or after direct or indirect injection. Areas of the body that have a rich blood supply, such as the liver, kidneys, and heart receive the highest level of the medication. Areas of the body that do not have a rich supply of blood, such as the bones, or areas that have a natural barrier, such as the brain's blood brain barrier, won't receive a very high level of the medication.”
“Metabolism is the change that occurs in a medication into a more or less potent form of the medication, more soluble form of the medication, or an inactive form of the medication. The liver is responsible for most of the metabolism of medications that occurs in the body. The word metabolite indicates it is a by-product of metabolism.”
“Excretion is the elimination of a medication or its metabolites through various parts of the body. For instance, the kidneys eliminate many medications through the urine. The kidneys may even reabsorb some of the medication through the kidneys, allowing it to pass through the body again before excretion actually occurs. Excretion can also occur through the gastrointestinal tract, the skin, or the lungs.” (This means that a patient with any sort of kidney problem may have trouble removing a drug from the body and thus may be at higher risk of toxicity, etc…)
Pharmacodynamics= what the drug does to the body, “describes the interaction between medications and target cells, body systems, and organs to produce effects which result in functional changes that are the mechanism of action of the medications.” “Pharmacodynamics are the biochemical changes that occur in the body as a result of taking a medication.”
“Changes in cellular function precipitate a greater or lesser response than what typically occurs. Agonists are medications that bind with a receptor and precipitate a greater-than-typical response. Antagonists are medications that bind with a receptor and either block a response or precipitate a less-than-typical response. Medications that are antagonists exert their effect in either a competitive or noncompetitive manner. Antagonists that compete with an agonist for receptor sites are considered “competitive antagonists.” Antagonists that block an agonist’s access to receptor sites are considered “noncompetitive antagonists.” When you give in high enough doses, noncompetitive antagonists can completely block the typical response caused by an agonist. Competitive antagonists that you give in increasingly high doses will decrease the typical response by an agonist but will rarely completely block it.”
“Changes in the cellular environment occur when medications interfere with the structure of a cell, such as the cell wall or one of a cell’s critical processes like replication. For example, penicillin-type antibiotics inhibit cell wall synthesis of certain types of bacteria, resulting in the destruction and death of the bacteria. Sulfa-type antibiotics inhibit the replication of certain types of bacteria by preventing folic acid from helping to make DNA and RNA.”
“Therapeutic effects are the intended effects of the medication.”
“Adverse drug reactions are the unintended effects of the medication.”Analyze factors that can influence the effectiveness of drugs in the body.
Provide examples of therapeutic effects and adverse drug reactions.
Explain the difference between the expected pharmacologic action and the therapeutic use of a medication.
“The action a medication exerts in the body is a medication’s expected pharmacologic action. A provider chooses medications for a client’s treatment plan based on the expected pharmacologic actions of those medications. For example, antibiotics or anti-infectives have the ability to kill or inhibit the reproduction of bacteria, so they are prescribed for clients who have an infection. In this example, infection is the indication, or the condition for which the medication is prescribed.”Differentiate between medication side effects and adverse effects.
“ADRs are the nontherapeutic, unintended effects of a medication that occur at a therapeutic dose. They may be predictable and well-known or unpredictable. These can range from annoying but tolerable to life-threatening.”
“Other more serious, possibly life-threatening ADRs include confusion, uncoordination, dizziness, and convulsions in some older adults. It can also cause hyperactivity and excitation in children.”
“The most severe type of adverse drug reaction is an allergic reaction. The severity of an allergic drug reaction can range from itching and rash or hives to life-threatening anaphylactic shock. Clients who experience a mild drug reaction need to avoid taking the medication again due to the risk of anaphylaxis. The client’s previous exposure increases their sensitivity to the medication and may precipitate a more severe reaction upon second exposure to the medication.”Explain medication tolerance, cumulative effect, and toxicity of medications.
“Medication tolerance is the body’s decreased response to a medication it receives over a period of time. For the medication to continue to exert a therapeutic effect, providers must increase the dosage. Whereas medication dependence is a physiologic or psychological need for a medication. Withdrawal syndrome can occur in clients who are psychologically and/or physically dependent. The client can experience a variety of physical and mental manifestations when they are no longer taking the medication.”
“Medication sensitivity, or a cumulative medication effect, may occur in clients secondary to metabolic changes, such as impaired hepatic and renal function, resulting in poor excretion of medications. The body is unable to metabolize and excrete the single dose of the medication before another dose is administered. Nurses should pay particular attention to interventions, such as assessing clinical signs and monitoring laboratory results, that will help reduce ADR in these clients.”
“Medication toxicity occurs when a client receives medications in excessive dosages, resulting in negative physiologic effects. Providers should prescribe the lowest effective dose possible to achieve therapeutic effects. It can also happen when impaired excretion of the medication allows it to build up in the body. Eventually, this reaches levels where toxic effects are evident. Providers must be cognizant of impaired metabolic and excretory functions of clients and adjust dosages as needed. Periodic laboratory tests are essential in monitoring serum medication levels. The effects of medication toxicity may be irreversible and life-threatening. For example, vancomycin may cause permanent damage to cranial nerve number eight, resulting in decreased hearing or even deafness. Acetaminophen may cause temporary damage to the liver or permanent damage that results in liver failure.”Differentiate between medication precautions and contraindications
“Take precautions when providers prescribe medications that have the potential to cause adverse drug reactions in certain populations or in combination with other medications or certain foods. Only use these medications when necessary and when the benefits outweigh the risks. Take extra precautions when providers prescribe medication for clients with chronic or multiple medical conditions. For example, if a client experiences a stroke, that might require anticoagulant therapy. Extra precaution includes physical assessment and laboratory monitoring in order to prevent gastric bleeding if the client also has peptic ulcer disease. Other precautions might require limiting certain types of food or concurrent administration of specific types of medications rather than restricting the medication itself.”
“There are some medications that a provider should not prescribe because they have the potential to cause serious or life-threatening adverse drug reactions. This is called a contraindication. Some medications are contraindicated for use with certain populations or in combination with other medications and certain foods. Providers should not consider the use of medications in these situations except under extremely unusual circumstances.”Define key terms:
generic drug
brand or trade name drug
prescription drugs
over-the-counter drugs
pharmaceutics: addresses how various medication forms affect the dissolution of a medication, the absorption rate of a medication, and its onset of action
parenteral drugs: injectables (IV, IM, SQ, ID),
pharmacokinetics
first-pass effect
bioavailability:
drug half-life
peak drug level: the point in time when the medication is at its highest level
trough drug level: the point in time when the medication is at its lowest level in the body
pharmacodynamics: the biochemical changes that occur in the body as a result of taking a medication
agonists
antagonists
Side Effect
Adverse Effect
Tolerance
Cumulative Effect
Toxicity
Precautions
Contraindications
Anaphylactic Shock
Allergic Reaction
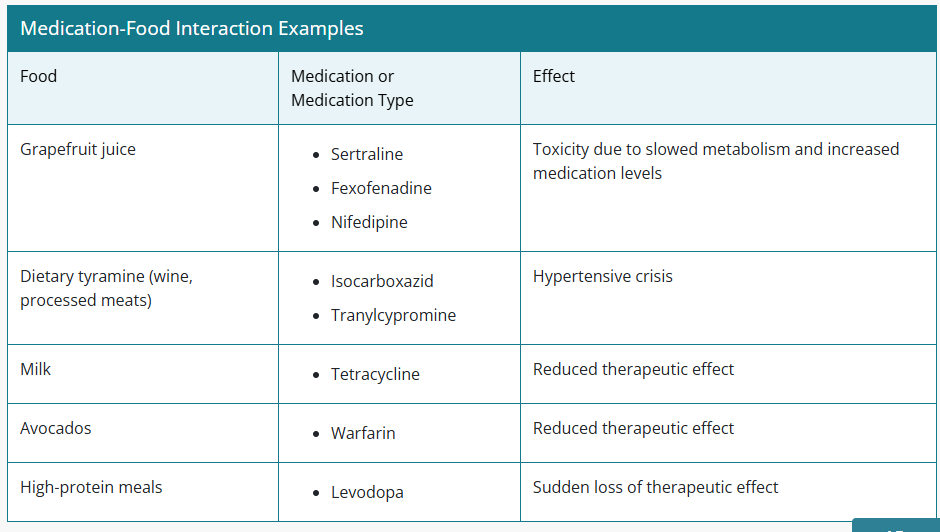
Common Drug-Food Interactions:
“Medication-medication and medication-food interactions can radically change the action of medication in the body. Precautions may require limiting certain types of food or concurrent administration of certain types of medications rather than restricting the medication itself. Grapefruit juice is a drink that can decrease the enzymatic metabolism of certain medications, increasing their potency and risk for toxicity. For example, avoid grapefruit juice if a client is taking the antidepressant sertraline, the antihistamine fexofenadine, or the calcium channel blocker nifedipine. If a client drinks grapefruit juice with these medications, they may accumulate in the body and have serious consequences. Wine and processed meats that contain tyramine can cause a hypertensive crisis in clients taking isocarboxazid or tranylcypromine. The calcium in milk products binds to tetracycline, thereby reducing its absorption. Eating dark green vegetables such as avocados that are high in vitamin K counteracts the anticoagulant effects of warfarin. Finally, ingestion of a meal high in protein decreases the absorption of levodopa, causing manifestations of Parkinson’s to abruptly increase.”
“Medication-food interactions occur when a food changes the way a medication affects the body. This can result in increased levels of the medication in the body, which occurs when food increases the amount of a medication the body absorbs or the rate at which it is metabolized.”