Week 5: Lipid Metabolism
Lipids: long chains of carbons varying in length and level of saturation
Categorised based on the number of carbons and types of bonding
Cholesterol is important as it stabilizes the membrane, it is important for bile acid, and vitamin D synthesis
Lipids cannot be carried in the blood as it is mostly water
—> lipids cannot be carried in the blood since it is mostly water
Types of lipids:
simple lipids: groups of lipids composed of fatty acids, glycerols and alcohols
fats, oils and waxes
complex lipids: groups of lipids that contain other groups apart from fatty acids and glycerols
phospholipids, lipoproteins, lipopolysaccharides
Lipoproteins: packaged fat and cholesterol
lipid core and a surface coat, phospholipids are surrounding it
apoproteins which surround it determine their function
4 main lipoproteins: lowest protein to highest protein (highest lipid to lowest lipid)
chylomicron = 90% TAG, 10% Cholesterol Esters
VLDV (very low density lipoprotein) = TAG and cholesterol esters
LDL = cholesterol esters
HDL = cholesterol esters
Chylomicrons = important for dietary TAG
ingested in the small intestine
Chylomicrons in the blood:
chylomicrons doc onto LPL
LPL breaks bonds that join fatty acids and glycerol
chylomicron remnants are taken through the blood into the liver
Basically:
chylomicrons from the gut goes through extrahepatic tissue first
TAG is sucked out leaving the chylomicron remnant
this is taken to the liver, cholesterol is recycled and can be used in in many ways
Chylomicron remnant in the liver —> cholesterol is removed
Cholesterol is important for bile, bile goes into the small intestine and helps to breakdwon fats, some bile is reabsorbed
Cholesterol is also carried in the LDL, LDL takes cholesterol from the liver to extrahepatic tissue (other tissue)
Steps:
liver released VLDL
muscles take TAG and use it through beta oxidation to break it down for energy
adipose tissue will also breakdown tag to release fatty acids to go to the muscles and liver
the glycerol will go back to the liver and is then converted into glucose through gluconeogenesis.
regulating fatty acid utilisation:
lipolysis of triacylglycerol results in free fatty acids
fatty acids undergo reesterification to repackage into TAG or they can be sent from adipose tissue where they are needed for energy
transport acyl-CoA into the mitochondria
availability of FAD and NAD for beta oxidation
hormone sensitive lipase
= lipase = enzyme that hydrolyses TAG = FA and glycerol
pacnratic lipase (digestive enzyme)
lipoprotein lipase (adipose epithelial cell)
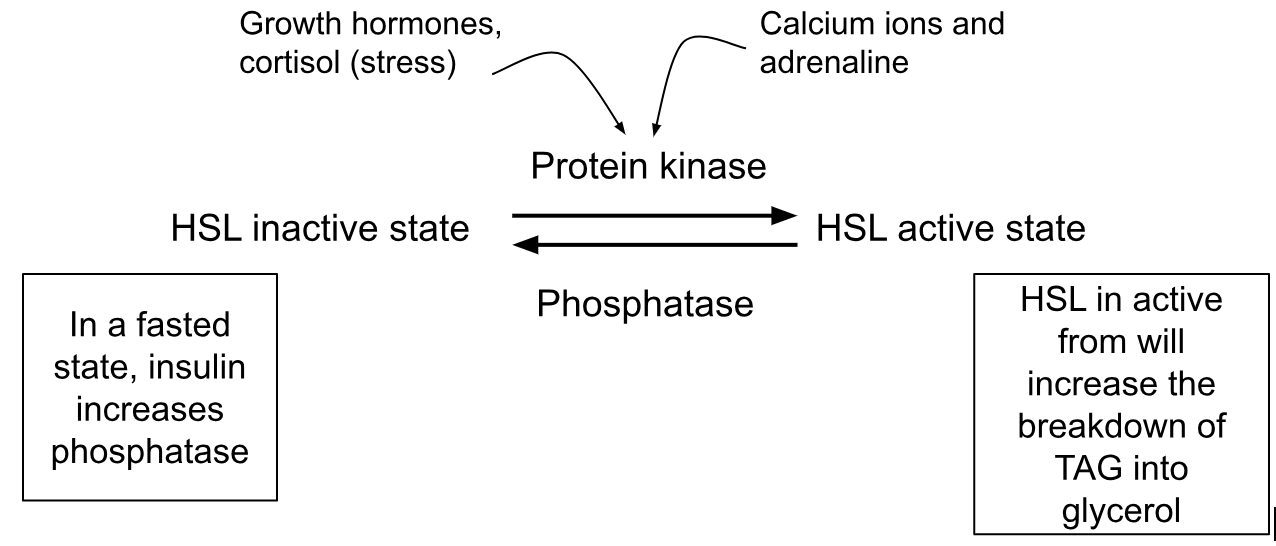
HSL activated by protein kinase
phosphorylated when active
HSL inactive form by phosphatase
REGULATING HSL:
Process of lipolysis and re-esterification:
when lipids are broken down in adipose tissue, they either release fatty acids and glycerol or will be repackaged. when needing to leave the cell, fatty acids will be encouraged to go out and be used for energy instead of being repackaged
Transportation of fatty acids across a membrane: fatty acid translocase
During exercise: interstitial fluid which is between the blood and the sarcoplasm of muscle recieves fatty acids through
albumin, VLDL, or chylomicrons take fatty acids
LPL which is on the endothelial cells of the capillary, transports FA down a concentration gradient into the sarcoplasm
mostly done by FAT CD36 (fatty acid translocase)
Storage in muscles:
If we dont want to use fatty acid as energy, LPL will get active and take the fatty acids into the cell and we will store it in muscle
fatty acids will get activated by acyl-CoA
in a trained individual, lipid droplets are closer to the mitochondria as this is the site for beta oxidation which will need quick access to the lipid droplets
after exercise, lipid droplets decrease in size by a half, intramuscular TAG can potentially increased in trained individuals.
Lipolysis of intramuscular triacylglycerol:
Protein Kinase activates inactive HSL
stimulated by the release of calcium ions, adrenaline and AMP
Protein Kinase phosphorylates HSL and makes it active
SUMMARY: nothing is rate limiting
fatty acids leave adipose tissue down a concentration gradient
fatty acids bind to albumin (a protein) in the blood
fatty acids are removed from the blood and enter the cell through a concentration gradient
Carnitine shuttle:
Once fatty acids are in the cell, they must be transported into the mitochondria for beta oxidation to give Acetyl CoA
mitochondria has 2 membranes
outer membrane = permeable to lipids
inner membrane = impermeable to lipids
CPT1 sits on the outer membrane and attaches to the acyl, removing the CoA and replacing it with carnitine
CACT helps the carnitine acyl into the mitochondria
Acyl carnitine needs to be removed and replaced with the CoA
CPT2 removers the carnitine and reattaches the CoA
Basically:
CPT1: takes off the CoA
CAPT: moves acyl carnitine across the impermeable membrane
CAPT2: removes the carnitine and replaces it with CoA
Acetyl CoA now enters the TCA cycle, producing NADH and FADH2 to give us ATP
B-oxidation; B-HAD is a rate limiting enzyme
beta oxidation repeats itself until there are not carbons left to be converted into Acetyl CoA
When comparing energy from fat oxidation is 39.4, grams oxidised per min is more but there is less energy in each gram compared to CHO which burned 15.6 grams.
Fatty acid increase drives fatty acid oxidation increase
more fatty acids in the blood = more fatty acid oxidation, increases muscle glycolysis = increase of fatty acids in the mitochondria
Cholesterol
Too much LDL can be dangerous as it can result in problems in blood vessels.
LDL has a very long life, it sits in the body for 1.5 to 2 days
because they are in the bloodstream for so long, they are subject to damage
Why is HDL seen as “good”?
HDL is the best single lipid predictor of CVD as it is negatively related
Its life cyle is complex, when a cell has too much cholesterol, it will express SRB
HDL attaches on to SRB to remove excess cholesterol and transport it to the liver
bile, steroid hormones, membrane stability and support
How can we change lifestyle to reduce cholesterol?
a study showed that plant sterols cause less cholesterol to be less abosrbed
aerobic training and resistance taining
high fat diet- increase chylomicrons
 Knowt
Knowt