Week 4: CHO
Glycemic index; glucose vs starch: different CHO cause different spikes in blood glucose.
Fructose and metabolism:
location: mainly liver
can also occur in the liver, kidney and small intestine
Fructose is mainly used for liver glycogen
beneficial for active people; a small amount will be coverted into lactate and glucose.
unfavourable for sedentary individuals as it can lead to TAG synthesis, lipid accumulation due to inactivity which can lead to insulin deficiencies and issues like type 2 diabetes.
fructose uptake is not insulin dependent unlike glucose
Summary:
GLUT-1 diffuses glucose into astrocytes, also the main passage from glucose into the brain: insulin independent
GLUT-2 diffuses glucose form the blood into the liver: insulin independent
Glucose in the blood triggers insulin release, insulin binds to receptors and triggers glucokinase to create a concentration gradient, glucose enters into the liver and glucokinase adds a phosphate group onto the glucose to then be either synthesise glycogen or be put back into the blood by removing the phosphate group with enzyme glucose-6-phosphatase
GLUT-3 diffuses glucose in neurons: insulin independent
GLUT-4 used in skeletal muscle: insulin dependent / insulin independent
Glucose enters through GLUT-4 after insulin binds to the receptor and causes hexokinase to stimulate reactions and keep the concentration gradient.
BASICALLY:
Liver:
Transporter: GLUT-2
Enzyme: Glucokinase
insulin promotes glycogen synthesis for storage
Enzyme to remove phosphate group: Glucose - 6 - Phosphatase
Skeletal Muscle:
Transporter: GLUT-4
insulin promotes glycogen synthesis for storage
Enzyme: Hexokinase
Brain:
transporter: GLUT-3 (neuron), GLUT-1 (blood brain barrier, astrocyte)
insulin promotes glycogen synthesis for storage
enzyme: hexokinase
GLYCOGEN SYNTHESIS:
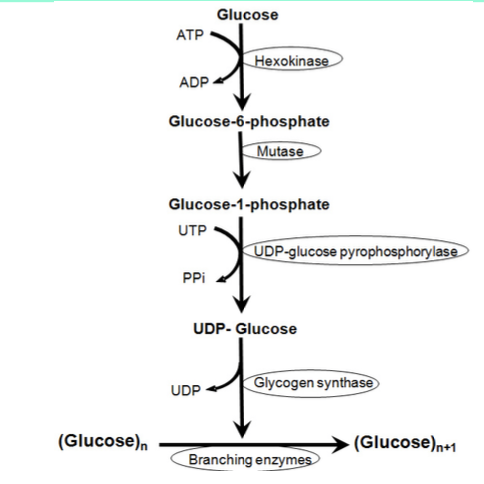
Glycogen synthesis: once glucose 6 phosphate is created, the enzyme mutase converts it into glucose 1 phosphate by changing its structure, reactions with UTP and UDP lead to glycogen synthase to ultimately convert glucose into glycogen
insulin activates protein phosphatase (remover of phosphate group) meaning glycogen can then be made
Adrenaline and calcium ions inactivate the glucose as they increase the release of kinase A which adds a phosphate group
SUMMARY - glycogen breakdown and synthesis enzymes:
glycogen synthase
role: active attatched UDP-glucose to glycogen (no phosphate gorup)
protein phosphatase:
role: removes phosphate group making glycogen synthase active
stimulated by: insulin
Protein Kinase A:
role: adds phosphate group making glycogen synthase inactive
stimulated by: calcium ions, adrenaline and glucagon
Glycogen phosphorylase active form:
role: breaks down glycogen to glucose-1-phosphate
inhibited by: high levels of G-6-P and ATP
Glycogen Phosphorylase phosphatase:
role: removes phosphate making glycogen phosphorylase inactive
stimulated by: insulin
inhibited by: high AMP
Glycogen phosphorylase kinase:
role: adds phosphate making glycogen phosphorylase active
stimulated by: clacium ions, adrenaline and glucagon
glycogen synthesis and breakdown: hormones
adrenaline: flight or fight, stimulates the breakdown of glycogen
insulin: released after CHO ingestion, reduces the breakdown of glycogen and stimulates storage
glucagon: released after periods of no food, stimulates breakdown and inhibits storage
glycolytic enzymes in muscle:
hexokinase
glycogen phosphorylase
phosphofructokinase
pyruvate kinase
lactate dehydrogenase
pyruvate dehydrogenase
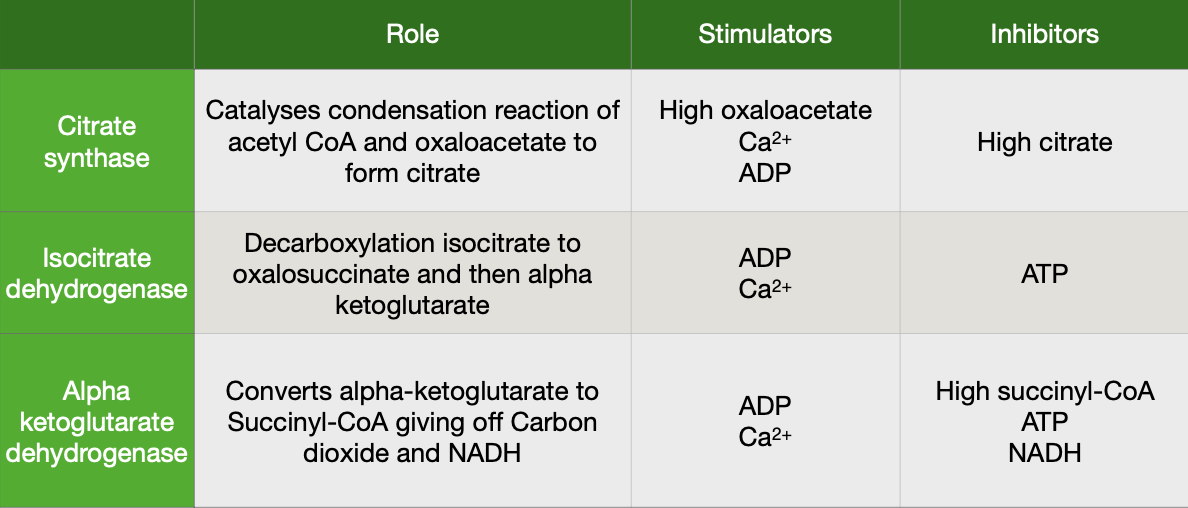
TCA cycle functions:
decarboxylation of acetyl-coA
ATP production
FADH2 production
NADH production
Amino acid breakdown, fat breakdown, carbohydrate breakdown feeds into the TCA cycle.
Electron transport chain:
4 large complexes
electrons pass from electron donors to electron acceptors
each electron acceptor wants the electron more than the last one
final =
Gluconeogenesis: liver (kidneys)
fatty acids can not restore glucose of the liver as it would be inneficcient
pyruvate to OAA, if there is lots of acetyl co a coming from fatty acids,
acetyl co a inhibits acetyl dehydrogenase due to the increase of fatty acids giving acetyl coa, this means pyruvate has to go in a difeferent way, it will be converted into oxaloacetate, this is sent out of the mitochondria into the cytoplasm and is using the malatatepaspartate shuttle