topic 8 again lol
LACTIC ACID METABOLISM

at physiological pH (~7.4), lactic acid exists almost entirely in its deprotonated (ionized) form: lactate⁻.
Even during aerobic metabolism, tissues still produce some lactate.
Why?
Lactate dehydrogenase (LDH) is always active.
Pyruvate may not always be immediately taken up by mitochondria (due to limited proximity or transport rate), so it gets converted to lactate.
Not just muscle — other tissues make lactate too:
skin, liver, heart, renal *RBCs
Lactate turnover refers to the rate at which lactate is produced and utilized by the body. It's a measure of how much lactate is entering and leaving the bloodstream and being used for other metabolic processes
“Lactate can serve as oxidative energy substrate (H-LDH, gluconeogenesis), or be incorporated into AAs or proteins”
Lactate isn’t waste — it’s a valuable:
“lactate shuttle” = lactate produced in myofibers with increased rates of glycolysis (with increased amounts of M-LDH) used as energy by nearby or remote cells with oxidative capacity
This is the Lactate Shuttle Hypothesis (Brooks, 1985):
M-type LDH (muscle) favors pyruvate → lactate
H-type LDH (heart) favors lactate → pyruvate
Lactate moves from high glycolytic (Type II) to oxidative (Type I) tissues to be used as fuel.
lactic exchange
Exchange Type | Description |
|---|---|
Active ↔ Inactive fibers (same muscle) | Lactate made in active fibers can be used by nearby less-active ones |
Type II → Type I fibers (same muscle) | Fast-twitch makes lactate → slow-twitch oxidizes it |
Active ↔ Inactive muscles | Cross-training effect — lactate produced in legs used by arms or vice versa |
Blood ↔ Muscle | Lactate enters bloodstream → taken up by other muscles |
Muscle ↔ Liver | Classic Cori cycle — lactate → glucose |
Muscle ↔ Heart | Heart prefers lactate as energy during exercise |
**heart loves lactate
*within cytosol of same cell, [lactate] increases away from mitochondria, decrease in [lactate] close to mito
sarcolemma lactate (MCT) transporter: small amounts of lactate able to diffuse across cell membrane, vast majority crosses by symport with H+ (facilitated diffusion). *different isoforms.
they move lactate and a proton simultaneously in the same direction
Epinephrine = ↑BPM
“Infusion of epinephrine at rest sharply increases lactate released by muscle (↑ glycolysis, no effect on O₂/P)”
EXERCISE CONDITIONS
As soon as muscle contractions begin, anaerobic glycolysis activates rapidly, leading to lactate production.
The muscle starts releasing more lactate than it's consuming, creating a net output.
Simultaneously, lactate consumption also rises (e.g., by heart, liver, oxidative fibers).
✅ Net release underestimates total lactate produced
Some lactate is used within the same muscle or nearby tissues before entering the blood.
So, the actual lactate production is higher than what you see in blood measurements.
✅ Initial lactate release depends on muscle mass
The more active muscle mass, the more lactate produced.
as exercise at same sub max intensity continues , lactate release from muscles level off, consumption increases → drop in blood lactate
✅ Rate of lactate consumption depends on availability
The body clears lactate faster when there’s more available in blood.
Uptake by heart, liver, kidneys, Type I fibers increases as lactate levels rise.
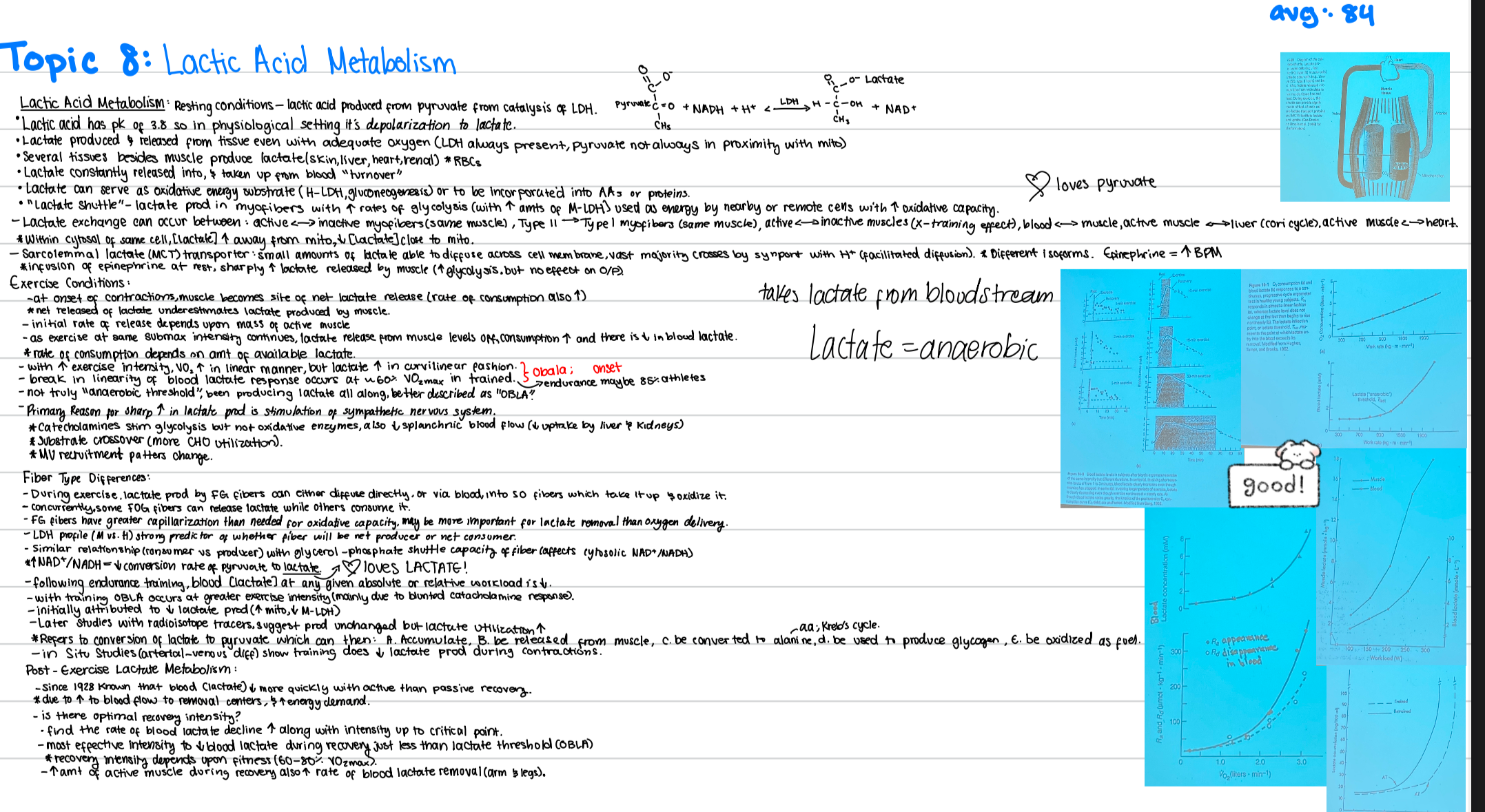
✅ “VO₂ ↑ linearly with exercise intensity, but lactate ↑ in a curvilinear fashion”
Oxygen consumption (VO₂) increases steadily with exercise intensity.
Lactate stays low at first, then rises sharply once a certain intensity is reached.
This point is often called the “lactate threshold” or OBLA (onset of blood lactate accumulation).
In trained individuals, blood lactate begins to rise rapidly around 60% VO₂max.
In trained endurance athletes, around 85% VO₂max. (??)
**not truly a threshold bc been producing lactate all along
primary reason for sudden lactate rise because as intensity increases:
Sympathetic activation (fight or flight response) releases catecholamines (epinephrine, norepinephrine) but not oxidative enzymes
These stimulate glycolysis (↑ glucose breakdown) in muscle
also decrease in splanchnic blood flow(↓ uptake by liver and kidneys)
substrate crossover (more CHO utilization)
MU recruitment patterns change
➕ Additional Points:
Catecholamines stimulate glycolysis but not oxidative enzymes:
→ More pyruvate is made than mitochondria can handle
→ More lactate is formed
Reduced splanchnic blood flow (to liver/kidneys):
↓ lactate uptake by liver and kidneys → more remains in blood
Substrate crossover:
As intensity rises, the body shifts from fat to carbohydrates (CHO) as the primary fuel → ↑ glycolysis → ↑ lactate
Motor unit recruitment changes:
At higher intensities, more Type II (glycolytic) fibers are recruited → produce more lactate
Fiber Type Differences in Lactate Handling
during exercise, lactate produced by FG (fast glycolytic) fibers can either diffuse directly, or via blood into SO fibers which take it up & oxidize it.
concurrently, some FOG fibers can release lactate while other consume it
FG fibers have greater capillarization than needed for oxidative capacity. may be more important for lactate removal than oxygen delivery
LDH profile (M vs H) strong predictor of whether fiber will be net consumer or net producer
similar relationship (consumer vs producer) with glycerol - phosphate shuttle capacity of fibers (affects cytosolic NAD+/NADH)
During glycolysis, glucose → pyruvate → produces NADH
To keep glycolysis going, cells need to regenerate NAD⁺ (this is what the glycerol phosphate shuttle does)
If a muscle fiber has strong shuttle activity, it keeps the NAD⁺ / NADH ratio high in the cytosol → reduces the need to convert pyruvate into lactate
↑ NAD+/NADH = ↓ in conversion rate of pyruvate to lactate
following endurance training, blood [lactate] at any given absolute or relative workload is ↓
with training OBLA occurs at greater exercise intensity (mainly due to blunted catecholamine response)
initially attributed to ↓lactate production ( ↑ mito, ↓ M-LDH)
later studies with radioisotope tracers, suggest production unchanged but lactate utilization ↑
**refers to conversion of lactate to pyruvate which can then
a. accumulate
b. be released from msucle
c. be converted to alanine (AA;kreb’s cycle)
d. be used to produce glycogen
e. be oxidized as fuel
in situ studied (arterial - venous difference) show training does ↓ lactate production during contractions
Post-Exercise Lactate Metabolism:
since 1928 known that blood (lactate) ↓ more quickly with active than passive recovery *due to ↑ of blood flow to removal centers & ↑ energy demand
is there more optimal recovery intensity?
find that rate of blood lactate decline ↑ along with intensity up to critical point
most effective intensity to ↓ blood lactate during recovery just less than lactate threshold (OBLA) *recovery intensity depends upon fitness (60-80% VO2max)
↑ amount of active muscle during recovery also increases rate of blood lactate removal (arms & legs)