Human Physiology - Exam 5
DIGESTION
we need to break down the food we eat so that it can be metabolized by our own cells to make ATP
the digestive system is responsible for the intake, processing, and absorption of ingested nutrients and water
normal function of the digestive system is necessary for whole-body homeostasis as well as normal functioning of individual organ systems
Components of the Digestive (Gastrointestinal) System:
Gastrointestinal (GI, digestive) tract or alimentary system
the continuous pathway that transports food through the body
the lumen of the tract is continuous with the external environment, which means that its contents are technically outside the body
mouth → pharynx → esophagus → stomach → small intestine → large intestine → rectum → anus
Accessory Organs
organs that are not part of the food pathway, but contribute secretions to the digestion process
salivary glands, liver, gallbladder, pancreas
Breakdown of Macromolecules:
we ingest long chains of macromolecules that must be broken down into smaller molecules that the body can use
Carbohydrates are broken down into monosaccharides
Polysaccharides (starch and glycogen) → broken down into maltose intermediate products → produces glucose
Disaccharides (sucrose and lactose) → broken down into fructose and galactose during digestion, respectively
Proteins are broken down into amino acids
Polypeptide chains (ex: pepsin, trypsin, chymotrypsin) → broken down into peptide fragments (carboxypeptidase, aminopeptidase) → produces 20 different types of amino acids
Triglycerides
glycerol bound to 3 fatty acids + lipase → broken down into monoglyceride + 2 free fatty acids
Motility
Motility = contractions of smooth muscle in the gastrointestinal tract during secretion, digestion, and absorption
Serve two functions:
mix the luminal contents with the various secretions
move the contents through the tract from mouth to anus
In some cases, muscular movements travel in a wavelike fashion in one direction along the length of a part of the tract, a process called peristalsis, or peristaltic waves
Phases of Gastrointestinal Control: **named for the site at which the various stimuli initiate the reflex, not for the sites of effector activity*
Cephalic Phase
Initiated when sensory receptors in the head are stimulated by sight, smell, taste, and chewing
Various emotional states can also initiate this phase
The efferent pathways for these reflexes are primarily mediated by parasympathetic neurons carried in the vagus nerves that activate neurons in the gastrointestinal nerve plexuses, which in turn affect secretory and contractile activity
Gastric Phase
Within the stomach, distension, acidity, amino acids, and peptides that are formed during the partial digestion of ingested protein stimulate responses that are mediated by short and long neural reflexes and by release of the hormone gastrin
Intestinal Phase
Initiated by stimuli in the small intestine including distension, acidity, osmolarity, and various digestive products that stimulate responses
these responses are mediated by short and long neural reflexes and by the hormones secretin, CCK, and GIP, which are secreted by enteroendocrine cells of the small intestine
GI Tract Wall:
the mucosa is the surface where most of the processes of digestion and absorption occur (at the epithelium)
the submucosa contains blood vessels, as well as neurons that regulate the function of the mucosa
the muscularis externa contains smooth muscle that helps mix the contents of the small intestine
it also contains neurons that send signals to the submucosal neurons, and that receive inputs from the autonomic nervous system
the outer layer of the GI tract wall is a connective layer called the serosa, which supports the GI tract and connects it to the abdominal wall
Nervous System:
while the gastrointestinal tract is partially controlled by the central nervous system, it also has its own system of nerves in the walls of the intestines → called the enteric nervous system
also has its own endocrine + exocrine control
Long and Short Neural Reflex Pathways
long reflex system = receiving and processing information in the central nervous system via afferent nerves
short reflex system = local chemical and physical environment that can influence the enteric nervous system
How are Gastrointestinal Processes Regulated?
control mechanisms of the gastrointestinal system are governed by the volume and composition of the luminal contents, rather than by the nutritional state of the body
this means that the body is “designed” to absorb all the nutrients that are ingested, whether or not the body actually needs them to function at that time
Gastrointestinal reflexes are initiated by a relatively small number of luminal stimuli:
Distension of the wall by the volume of the luminal contents
Chyme osmolarity (total solute concentration)
(chyme = the mixture of ingested food particles and gastric secretions)
Chyme acidity
Chyme concentrations of specific digestion products like monosaccharides, fatty acids, peptides, and amino acids
these stimuli act on mechanoreceptors, osmoreceptors, and chemoreceptors located in the wall of the tract and trigger reflexes that influence the effectors — the muscle layers in the wall of the tract and the exocrine glands that secrete substances into its lumen
Neural Regulation of Gastrointestinal Processes
The GI tract has its own local neural control: a division of the autonomic nervous system known as the enteric nervous system
Comprised of two nerve plexuses: the myenteric and submucosal
these neurons either synapse with other neurons within a plexus or end near smooth muscles, glands, and epithelial cells
efferent neurons from both the sympathetic and parasympathetic branches of the autonomic nervous system enter the intestinal tract and synapse with neurons in both plexuses
Two types of neural-reflex arcs exist:
short reflexes from receptors through the nerve plexuses to effector cells all within the GI tract
long reflexes from receptors in the tract to the CNS by way of afferent nerves, and back to the nerve plexuses and effector cells by way of autonomic nerves
chemoreceptors are stimulated by chemicals, osmoreceptors are sensitive to changes in osmolarity (concentration of solutes, particularly ions), and mechanoreceptors respond to distension of the gastrointestinal wall
Hormonal Regulation of Gastrointestinal Processes
The hormones that control the gastrointestinal system are secreted mainly by enteroendocrine cells scattered throughout the epithelium of the stomach and small intestine
One surface of each endocrine cell is exposed to the lumen of the GI tract
at this surface, various chemical substances in the chyme stimulate the cell to secrete its hormones from the opposite side of the cell into the blood
the gastrointestinal hormones reach their target cells via the circulation
The four best understood GI hormones are: secretin, cholecystokinin (CCK), gastrin, and glucose-dependent insulinotropic peptide (GIP)
most of the hormones participate in a feedback control system that regulates some aspect of the GI luminal environment
most GI hormones affect more than one type of target cell
Components and Functions of Saliva
Water = moistens food; dissolves molecules to facilitate chemoreception
Mucus = lubricates food and facilitates formation of a bolus for swallowing
HCO3- = neutralizes acids in foods and bacteria metabolites
Lysosome = kills bacteria to maintain health of gums and teeth
Amylase = begins the digestion of polysaccharides
Lipase = begins the digestion of triglycerides
Properties of Gastrointestinal Hormones
Gastrin
Main functions: causes parietal cells to produce HCl; stimulates gastric motility, causing muscle contractions to increase in intensity → move food through the stomach
also inhibits GIP hormone
Produced in: antrum of the stomach
Stimulated by: amino acids, peptides in stomach; parasympathetic nerves
Inhibited by: acid in stomach, somatostatin
Glucose-dependent insulinotropic peptide (GIP)
Main functions: stimulates pancreas to release insulin → insulin affects target cells throughout the body, facilitating glucose transport and nutrient utilization
Produced in: small intestine
Stimulated by: glucose, fat in small intestine
Secretin and Cholecystokinin (CCK)
Main functions: promote release of pancreatic enzymes and buffers; trigger bile secretion and ejection of bile from gallbladder → inhibit acid secretion and motility to provide time for absorption
Produced in: small intestine
Stimulated by:
Secretin — acid in small intestine
CCK — amino acids, fatty acids in small intestine
Example: CCK Secretion Pathway
The presence of fatty acids and amino acids in the small intestine triggers CCK secretion from cells in the small intestine into the blood
Circulating CCK then stimulates the pancreas to increase the secretion of digestive enzymes, causes the gallbladder to contract, and relaxes the sphincter that allows pancreatic and liver secretions to flow into the small intestine
As fatty acids and amino acids are absorbed, their concentrations in the lumen decrease, removing the signal for CCK release
Important Parts of the Stomach:
Two main regions — the body and the antrum
Body → secretes mucus, pepsinogen, and HCl
Antrum → mixing and grinding; secretes mucus, pepsinogen, and gastrin
Gastric glands are located in the body of the stomach, which contain two important secretory cells — parietal cells and chief cells
Parietal cells → responsible for lowering the pH (increasing acidity) of stomach lumen via H+ acid secretion → acidic environment helps break down bonds
secrete intrinsic factor = a protein that binds and allows the absorption of ingested vitamin B12
Chief cells → creates proenzyme called pepsinogen → helps break down proteins into smaller chunks of amino acids
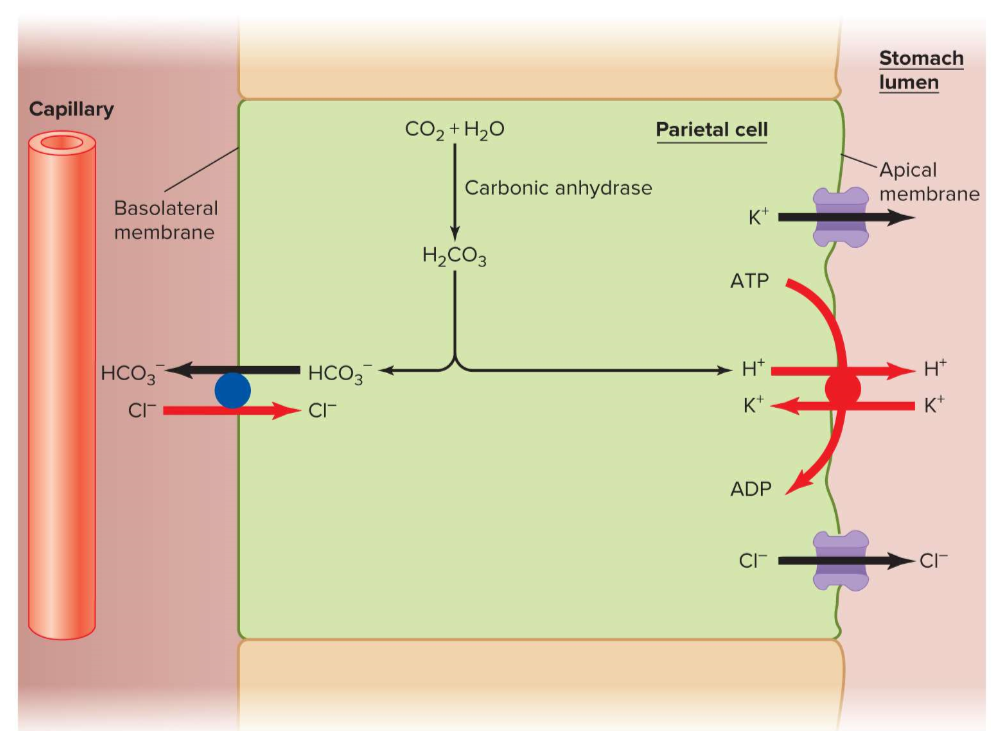
Parietal Cells - Production and Regulation of Hydrochloric Acid
Secretion of HCl
similar mechanism to kidney physiology → carbonic anhydrase synthesizes H2CO3 from CO2 and H2O → H2CO3 dissociates into bicarbonate and H+ ions
H+ ions are transported into the stomach lumen via proton pumps coupled to K+ ions (active transport mechanism) → increases acidity (lowers pH)
uses primary active H+/K+ -ATPase pumps in the apical membrane
bicarbonate ion is “kicked out” through HCO3-/Cl- exchange process
Regulation of HCl
major control coming from four hormones/neurotransmitters
parietal signaling molecules — lead to second messenger cascades
this process is analogous to that used for the transfer of water channels (aquaporins) to the apical plasma membrane of kidney collecting-duct cells in response to ADH
Gastrin, histamine, and acetylcholine: increase secretion of acid into the stomach → increase surface expression of H+ transporters
Somatostatin is inhibitory → prevents hydrogen pumps from being inserted into the lumen side of the stomach
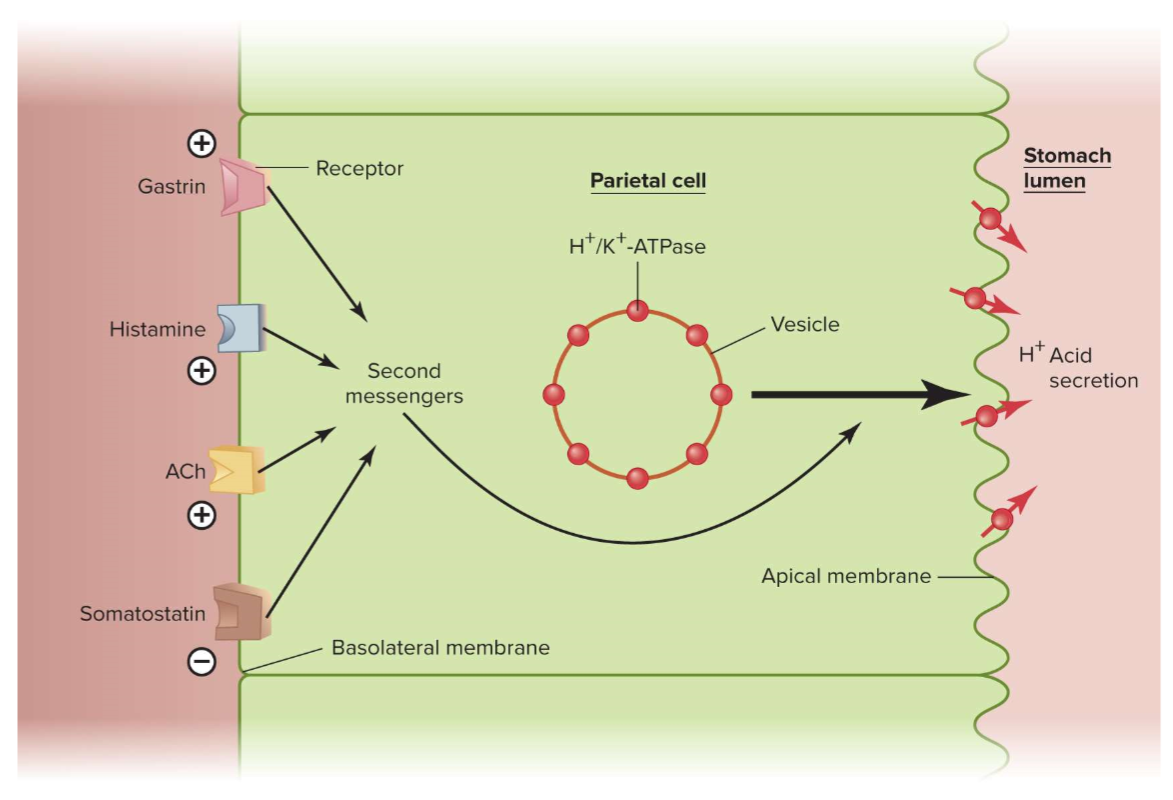
an increase in acidity inhibits the secretion of gastrin and somatostatin inhibits the release of HCl
both of these are negative feedback loops limiting overproduction of HCl
the protein in food is an excellent buffer, so as it enters the stomach, the H+ concentration decreases as H+ binds to proteins and begins to denature them
this decrease in acidity removes the inhibition of acid secretion
the more protein in a meal, the greater the buffering of acid and the more acid secreted
Pepsin Secretion
pepsin is an enzyme that is secreted by chief cells in the form of an inactive precursor called pepsinogen
Pepsin accelerates protein digestion but is not essential for it
exposure to low pH in the lumen of the stomach activates a very rapid, autocatalytic process in which pepsin is produced from pepsinogen
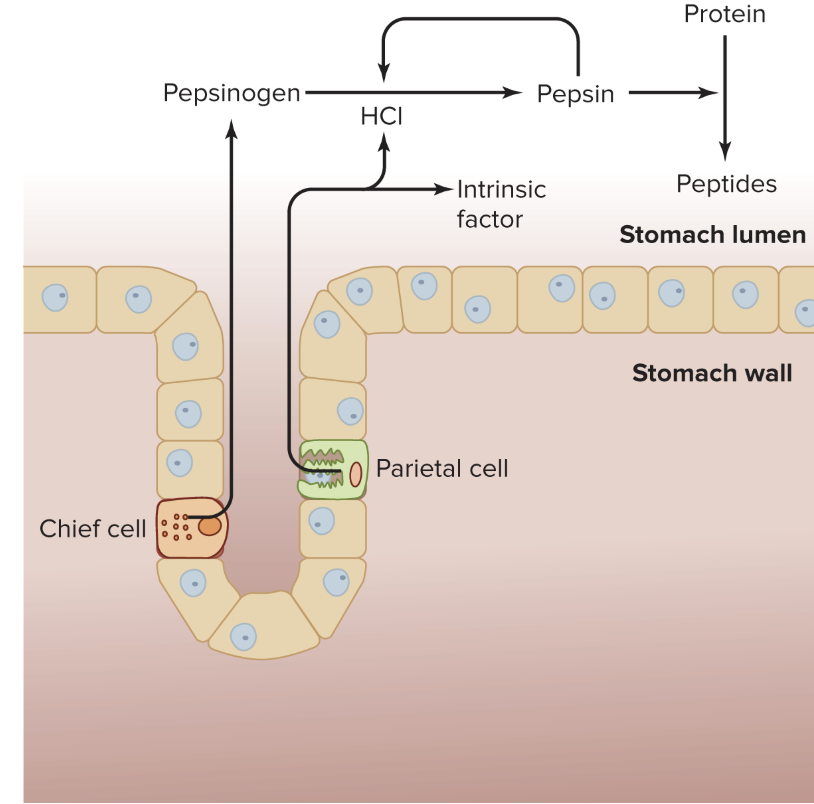
an increase in HCl acidifies the stomach contents
high acidity (low pH) maximizes cleavage of pepsin from pepsinogen
the pepsin thus formed also catalyzes its own production by acting on additional molecules of pepsinogen
pepsin is inactivated when it enters the small intestine, where HCO3- is secreted by the small intestine and pancreas neutralizes the H+
Anatomy of the Small Intestine
The small intestine is divided into three segments: an initial short segment — the duodenum, is followed by the jejunum, and then by the longest segment, the ileum
normally, most of the chyme entering from the stomach is fully digested and absorbed in the first quarter of the small intestine in the duodenum and part of the jejunum
The large surface area provided by the morphology of the small intestine allows for the highly efficient digestion and absorption of nutrients
One of the specialized anatomical structures are the circular folds = surface area specializations of the mucosa and submucosa that are covered with villi
Villi = fingerlike projections that increase surface area and contain blood vessels and lacteals, which function in the absorption of nutrients
Material absorbed by the lacteals reaches the general circulation by eventually emptying from the lymphatic system into large veins through a structure called the thoracic duct
The surface of each villus is covered with a layer of epithelial cells whose surface membranes form small projections called microvilli — known collectively as a brush border
Interspersed between these absorptive epithelial cells are goblet cells that secrete mucus into the lumen, where it lubricates and protects the inner surface of the wall of the small intestine
Intestinal epithelium at the base of the villi secretes a number of ions— notably, Na+, Cl-, and HCO3- —into the lumen, and water follows by osmosis
the osmotic gradient is enhanced when chyme entering the small intestine from the stomach is hypertonic due to high concentration of solutes resulting from the breakdown of large food molecules into many more small molecules
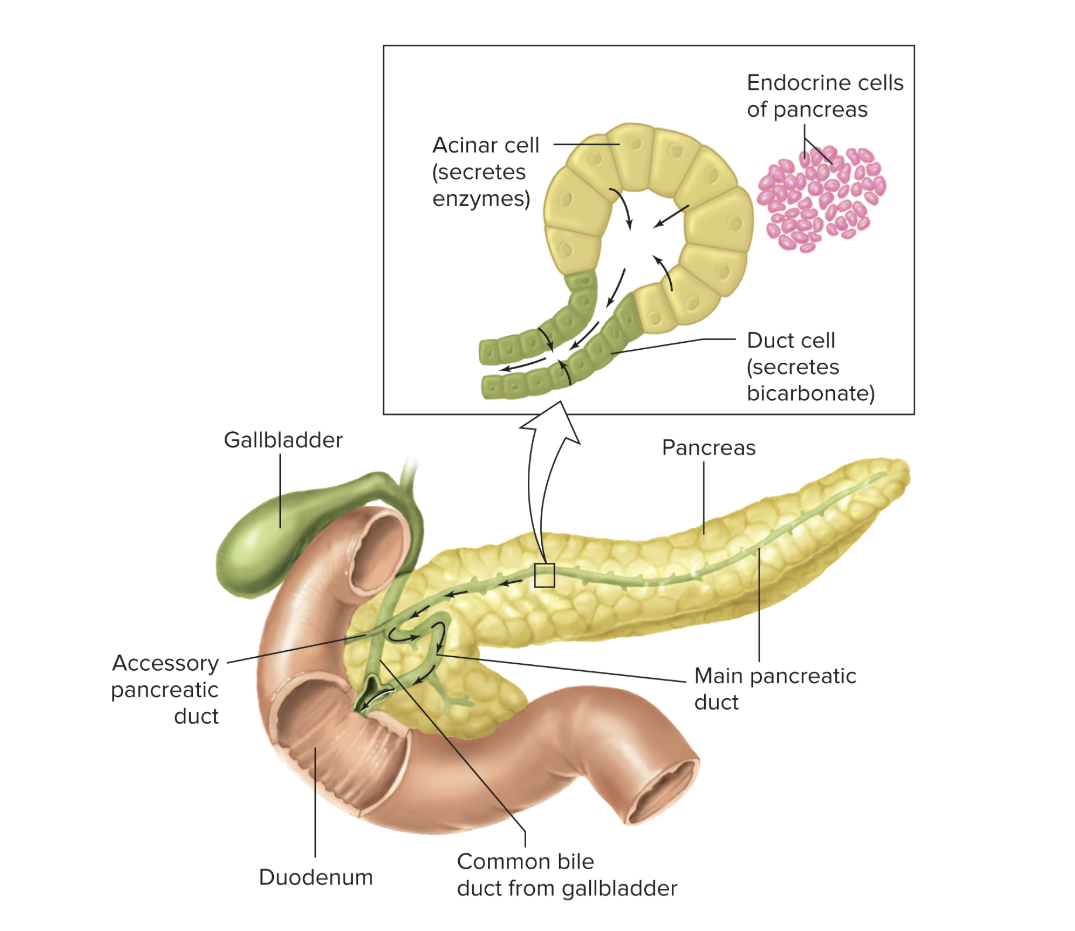
Anatomy of the Liver, Gallbladder, and Pancreas
The pancreas is an elongated gland located behind the stomach
The exocrine pancreas and the liver connect to the small intestine via ducts and produce secretions essential to the function of the small intestine
A large pancreatic duct delivers exocrine secretions of the pancreas into the duodenum
Bile is produced in the liver → the small bile ducts transport bile into the common hepatic duct
Between meals, bile is stored in the gallbladder — a small sac underneath the liver that branches from the common hepatic duct
The cystic duct, which is the only duct leading into and out of the gallbladder, branches off from the common hepatic duct → together, these two ducts merge to form the common bile duct
The common bile duct and the pancreatic duct empty together into the duodenum, via the sphincter of Oddi
Main roles:
add additional digestive enzymes into the small intestine
make bicarbonate ions to help neutralize the acid contents coming from the stomach
Pancreatic Secretions
The pancreas has both exocrine and endocrine functions
The exocrine portion of the pancreas secretes HCO3- and a number of digestive enzymes into the duodenum
the enzymes are secreted from lobules called acini at the end of the pancreatic duct system → called acinar cells
HCO3- is secreted by the epithelial cells living in the pancreatic ducts
The endocrine portion secretes insulin, glucagon, and other hormones into the blood
The high acidity of the chyme coming from the stomach would inactivate the pancreatic enzymes in the small intestine if the acid were not neutralized by the bicarbonate in the pancreatic fluid
Pancreatic Enzymes
Trypsin, chymotrypsin, and elastase
break peptide bonds in proteins to form peptide fragments
Carboxypeptidase
splits off terminal amino acid from carboxyl end of protein
Lipase
splits off two fatty acids from triglycerides, forming free fatty acids and monoglycerides
Amylase
splits polysaccharides into maltose
Ribonuclease and deoxyribonuclease
split nucleic acids into free nucleotides
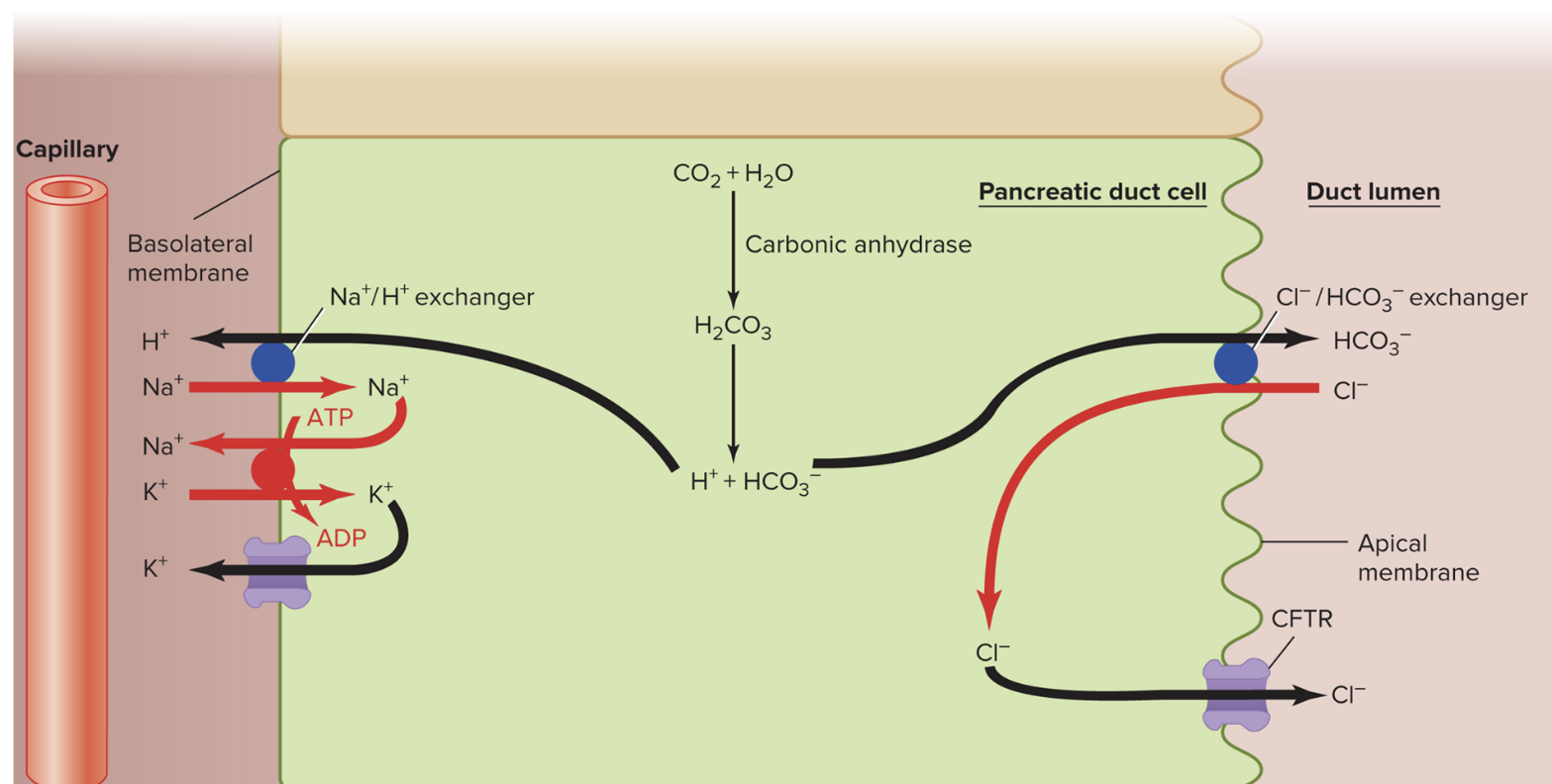
Regulation of Pancreatic Secretions:
Pancreatic secretion increases during a meal, mainly as a result of stimulation of the pancreas by the hormones secretin and CCK
secretin is the primary stimulant for HCO3- secretion, whereas CCK mainly stimulates acinar cell secretion
Major stimulus for secretin release is increased acidity in the duodenum
Neutralization of intestinal acid (increase pH by decreasing acidity) inhibits secretin secretion (negative feedback)
CCK stimulates the secretion of digestive enzymes, so the stimuli for its release are fatty acids and amino acids in the duodenum
Digestion of fats and proteins inhibits CCK secretion (negative feedback)
Liver Bile
Exocrine secretions from the liver enter the small intestine and are essential for normal digestion
One of the major functions of the liver in relation to the physiology of the gastrointestinal tract is to secrete bile
Bile contains bicarbonate, cholesterol, phospholipids, bile pigments, a number of organic wastes, and a group of substances collectively termed bile salts
the bicarbonate (HCO3-), like that from the pancreas, helps neutralize acid from the stomach, whereas the bile salts and phospholipids solubilize dietary fat
these fats would otherwise be insoluble in water, and their solubilization increases the rates at which they are digested and absorbed
the other components of bile are extracted from the blood and excreted as wastes
Bile secretion, followed by excretion of cholesterol in the feces, is one of the mechanisms for maintaining cholesterol homeostasis in the blood and is also the process by which some cholesterol-lowering drugs work
the bile salts, cholesterol, phospholipids, and bile pigments are secreted by hepatocytes, whereas most of the HCO3- -rich solution is secreted by the epithelial cells lining the bile ducts
secretion of HCO3- solution is stimulated by secretin in response to the presence of acid in the duodenum
the intestinal hormone CCK is the signal for gallbladder contraction and sphincter relaxation → stimulated by presence of fatty acids in the duodenum
What Happens to Macromolecules?
most of the digestion and absorption of nutrients occurs in the small intestine
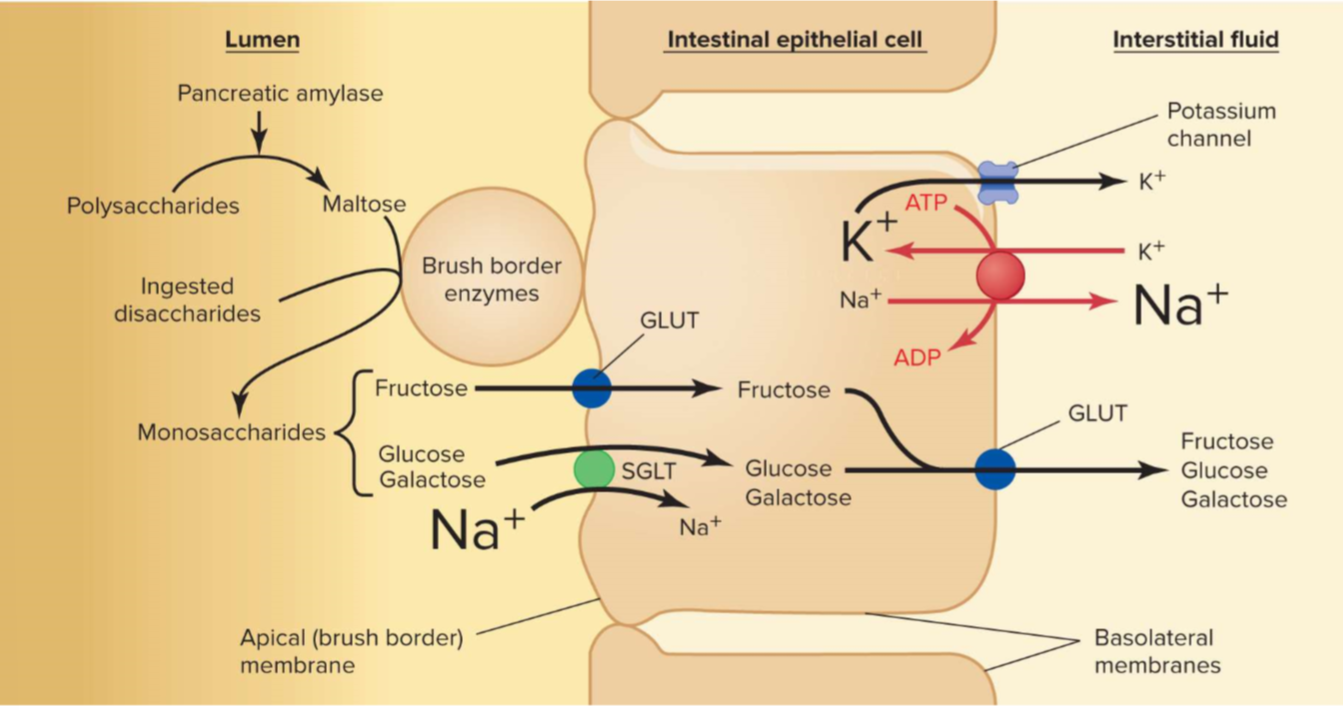
Carbohydrates
The products of both salivary and pancreatic amylase are the disaccharide maltose and a mixture of short, branched chains of glucose molecules
These products, along with ingested sucrose and lactose, are broken down into monosaccharides (glucose, galactose, and fructose) by enzymes located on the apical membranes of the small-intestine epithelial cells (brush border)
These monosaccharides are then transported across the intestinal epithelium into the blood
Two main transporters into the epithelial cell:
Glucose transporters (GLUT)
transport fructose
facilitated diffusion down concentration gradient
Sodium glucose transporters (SGLT)
transport glucose and galactose
uses free energy of sodium (Na+) → active transport
ion regulation: Na+/K+ pump maintains low Na+ on the inside
all sugars go through multiple GLUT transporters to get into interstitial fluid outside intestine
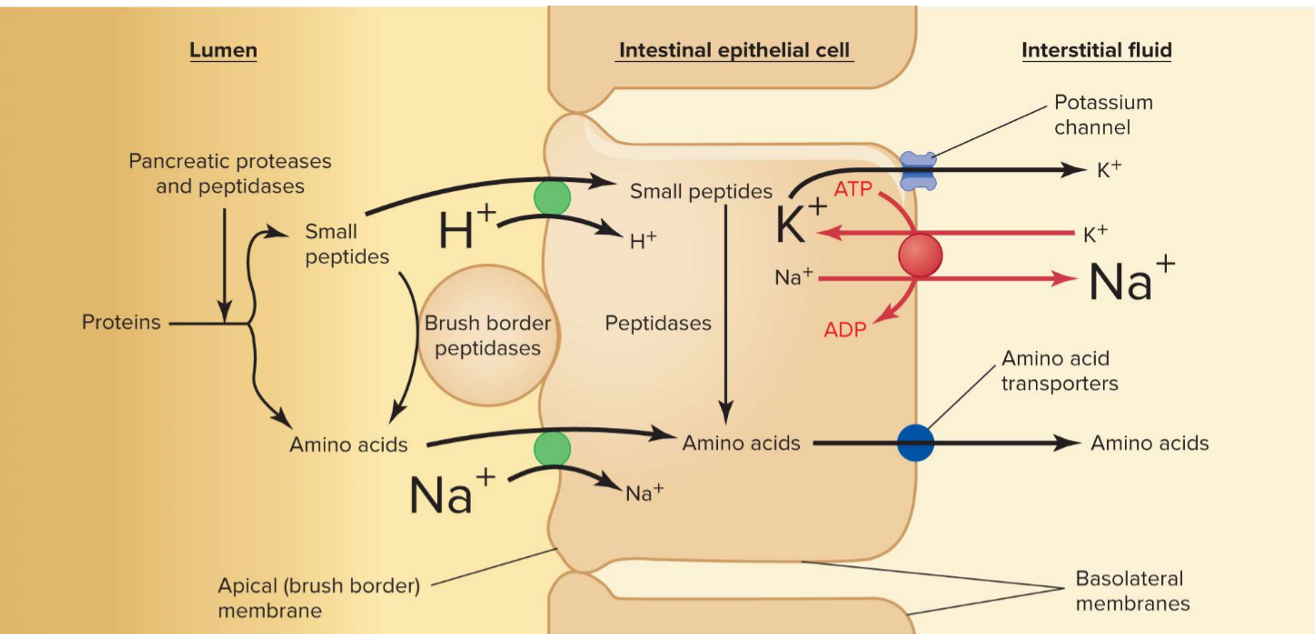
Proteins
Proteins are broken down to peptide fragments in the stomach by pepsin, and in the small intestine by the enzymes trypsin and chymotrypsin, the major proteases secreted by the pancreas
These peptide fragments are further digested to free amino acids by carboxypeptidases from the pancreas and aminopeptidases, located on the apical membranes of the small-intestine epithelial cells
At least 20 different peptidases are located on the apical membrane (the microvilli) of the epithelial cells
each peptidase breaks specific peptide bonds
The free amino acids then enter the epithelial cells by secondary active transport coupled to Na+
needs Na+/K+ pump on opposite side to maintain the ion gradient → allows Na+ energy to pull amino acids across the membrane via a co-transporter
Short chains of two or three amino acids are also absorbed by a secondary active transport coupled to the H+ gradient → broken down into amino acids inside the epithelial cell
Amino acids are transported into the interstitial fluid via amino acid transporters
Fats
Most dietary fats are triglycerides
Main digestive enzyme = pancreatic lipase → splits triglycerides into two free fatty acids and a monoglyceride
Fats are insoluble in water and aggregate (clump together) into large particles in the stomach
Lipase action occurs only at the surface of fat droplets, since it is a water-soluble enzyme
The speed of lipid digestion is increased by emulsification = the separation of large lipid droplets into smaller droplets to increase the surface area for lipase action
Lipid emulsification requires:
Mechanical breakdown of large lipid droplets → accomplished by the mixing and contractile movements of the stomach and small intestine
Emulsifying agents to prevent small droplets from reaggregating into large droplets → these are phospholipids from food and bile salts from bile
Formation of micelles — consist of bile salts, fatty acids, monoglycerides, and phospholipids all clustered together with the polar ends of each molecule oriented toward the micelle’s surface
Micelles increase absorption —> micelles and fatty acids are in equilibrium so that as fatty acids are absorbed, more can be released from the micelles (they are like “holding stations”)
Because fat is insoluble in an aqueous environment, micelles keep fat droplets from reaggregating and allow gradual absorption of fatty acids and other small lipids
Once broken down, free fatty acids can move (diffuse) across the intestinal epithelial membrane, since they are lipid-soluble
Inside the cell, they are reformed as a triglyceride droplet called a chylomicron — these complexes are what end up circulating throughout your blood
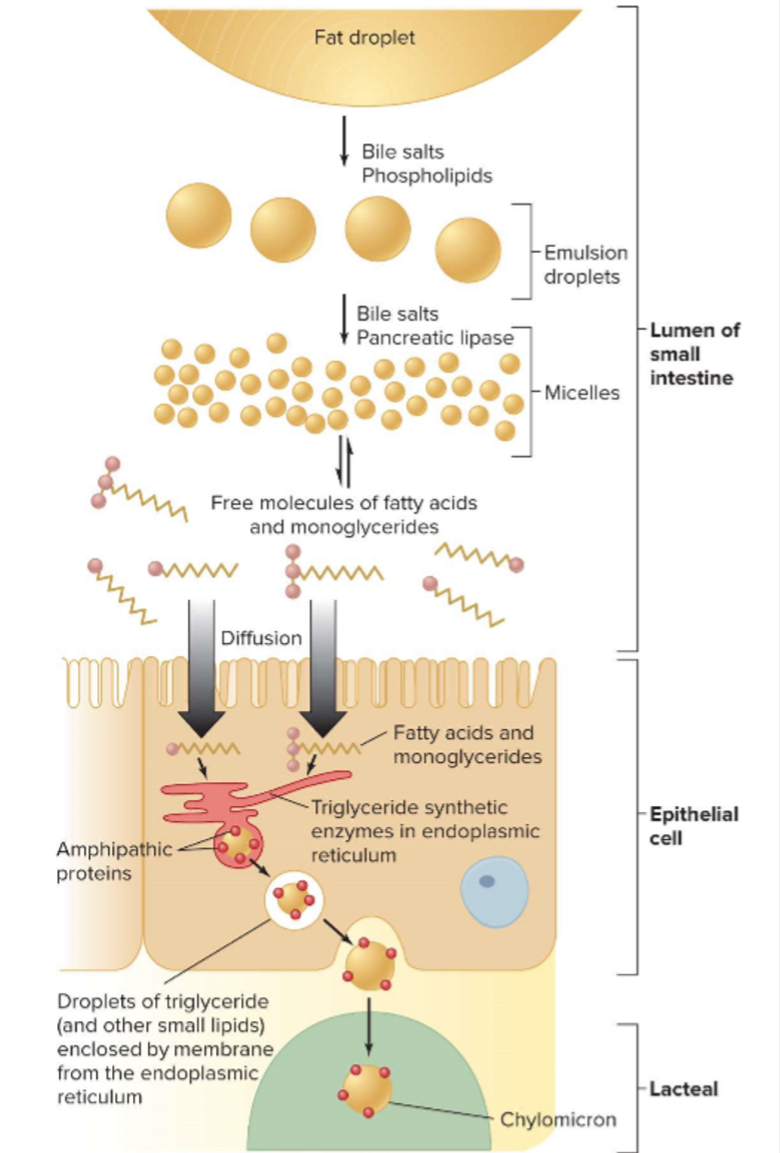
Absorption Pathways: getting nutrients into the bloodstream
Nutrients absorbed across the intestinal epithelium enter the blood by two different pathways:
Fats → absorbed into lacteals (lymphatic capillaries in the villi)
they travel through the lymphatic system and are emptied into the blood via the subclavian veins
then, chylomicrons circulate through the blood and deliver lipids to the body cells
Other nutrients → absorbed by intestinal blood capillaries that drain into veins
venous drainage from the stomach, pancreas, and small and large intestines does not empty directly into the inferior vena cava — it passes first into the liver via the hepatic portal vein
the liver capillaries process the nutrients and adjust their concentrations
the blood then drains into the hepatic veins and joins the general circulation by entering the inferior vena cava
The Absorptive and Postabsorptive States
Two functional periods that the body goes through, in providing cellular energy:
Absorptive State:
Period in which ingested nutrients enter blood from the GI tract
Occurs after a meal and lasts for about four hours — this is the amount of time it takes for an average meal to be digested and absorbed
During this time, nutrients are absorbed → some are used for cellular energy, and some are placed into storage
Postabsorptive State:
Period in which the GI tract contains no nutrients (not ingesting food)
Body’s energy stores must supply energy
Follows the absorptive state → body must use the energy stores created during the absorptive state
Summary of Nutrient Metabolism During the Absorptive State
Energy is provided primarily by absorbed carbohydrates in a typical meal
There is a net uptake of glucose by the liver
Some carbohydrate is stored as glycogen in the liver and muscle, but most carbohydrates and excess fats not being used for energy are stored as triglyceride in adipose tissues (fat cells)
the three major sources of the fatty acids found in adipose-tissue triglyceride are:
Glucose that enters adipose tissue and is broken down to provide building blocks for the synthesis of fatty acids
Glucose that is used in the liver to form VLDL triglycerides, which are transported in the blood and taken up by the adipose tissue
Ingested triglycerides transported in the blood in chylomicrons and taken up by adipose tissue
There is some synthesis of body proteins from absorbed amino acids
the remaining amino acids in dietary protein are used for energy or used to synthesize triglycerides
the three major fates of glucose during the absorptive state are:
Utilization for energy
Storage as glycogen in liver and skeletal muscle
Storage as triglyceride in adipose tissue
Summary of Nutrient Metabolism During the Postabsorptive State
Glycogen, fat, and protein syntheses are reduced, and net breakdown occurs
Three significant sources of blood glucose:
Glycogenolysis — the hydrolysis of glycogen stores to monomers of glucose 6-phosphate in the liver → is then enzymatically converted to glucose, which then enters the blood
Lipolysis — the catabolism of triglycerides in adipose tissue, which yields glycerol and fatty acids → these enter the blood by diffusion → glycerol reaching the liver is used to synthesize glucose
Protein breakdown — supplies large quantities of amino acids, which enter the blood and are taken up by the liver → some can be metabolized via the alpha-keto acid pathway to glucose
Glucose is formed in the liver, both from the glycogen stores and by gluconeogenesis from blood-borne lactate, pyruvate, glycerol, and amino acids
The kidneys also perform gluconeogenesis during a prolonged fast
The glucose produced in the liver and kidneys is released into the blood, but its utilization for energy is greatly decreased in muscle and other nonneural tissues
Lipolysis releases adipose-tissue fatty acids into the blood, and the oxidation of these fatty acids by most cells provides most of the body’s energy supply
Free fatty acids provide energy in two ways:
They first undergo beta oxidation to yield hydrogen atoms (which go on to participate in oxidative phosphorylation) and acetyl CoA
The acetyl CoA enters the Krebs cycle and is catabolized to carbon dioxide and water
Ketones are also produced in the liver due to the breakdown of fats
The brain continues to use glucose but also starts using ketones as they build up in the blood, since the nervous system cannot break down fats on its own
Hormonal Control of Metabolism: Insulin
Insulin = a peptide hormone of the pancreas; the most important regulator of organic metabolism
The main targets of insulin are skeletal and cardiac muscle, adipose and liver cells
Insulin secretion and blood concentration increases during the absorptive state, and decreases during the postabsorptive state
in the absorptive state, glucose is broken down for energy, and nutrients are stored
in the postabsorptive state, many nutrients other than glucose are broken down for energy, and stored nutrients are mobilized
After binding to receptors in the cell membranes of fat and muscle cells, insulin increases insertion of glucose transporters (GLUTs) into the cell membrane → this increases the facilitated diffusion of glucose into the cell
the transporters can be inserted (by exocytosis) or removed (by endocytosis) to regulate glucose uptake
vesicles storing transporters are sorted and distributed by endosomes
Increased amino acid concentrations stimulate insulin secretion
amino acid concentrations increase in the blood after ingestion of a protein-containing meal → the increased plasma insulin stimulates the uptake of these amino acids by muscle and other cells, thereby lowering their concentrations
Incretins = family of hormones secreted by enteroendocrine cells in the gastrointestinal tract in response to eating → amplifies insulin response to glucose
major incretins: glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP)
Glucose-Counterregulatory Controls
Glucose-counterregulatory controls = neural and hormonal factors that oppose the action of insulin
Glucagon
Epinephrine
Cortisol
Growth hormone
Sympathetic stimulation
Effects of glucagon:
Stimulates glycogenolysis
Stimulates gluconeogenesis
Stimulates the synthesis of ketones
Effects of epinephrine:
Stimulates glycogenolysis in both the liver and skeletal muscle
Stimulates gluconeogenesis in the liver
Stimulates lipolysis in adipocytes
SUMMARY: Functions of the Organs of the Digestive System
Mouth and pharynx
Functions: chewing begins; initiation of swallowing reflex
Salivary glands
Secretion of mucus → lubrication
Secretion of amylase → polysaccharide-digesting enzyme (relatively minor function)
Secretion of antibodies and other immune factors → help prevent tooth and gum decay
Esophagus
Function: move food to stomach by peristaltic waves
Secretion of mucus → lubrication
Stomach
Functions: store, mix, dissolve, and continue digestion of food; regulate emptying of dissolved food into small intestine
Secretion of HCl → solubilization of some food particles; kills microbes; activation of pepsinogen to pepsin
Secretion of pepsin → begins the process of protein digestion in the stomach
Secretion of mucus → lubricates and protects epithelial surface
Pancreas
Functions: secretion of enzymes and bicarbonate; also has nondigestive endocrine functions
Secretion of enzymes → digest carbohydrates, fats, proteins, and nucleic acids
Secretion of bicarbonate → neutralize HCl entering small intestine from stomach
Liver
Function: secretion of bile
Secretion of bile salts → solubilize water-insoluble fats
Secretion of bicarbonate → neutralize HCl entering small intestine from stomach
Secretion of organic waste products and trace metals → elimination in feces
Gallbladder
Function: store and concentrate bile between meals
Small intestine
Functions: digestion and absorption of most substances; mixing and propulsion of contents
Secretions → digestion of macromolecules; maintain fluidity of luminal contents; lubrication and protection
Large intestine
Functions: storage and concentration of undigested matter; absorption of ions and water; mixing and propulsion of contents; defecation