WK7: Drugs-Acting-on-Cardiovascular-System
systimetic = peripheral circulation, outside the heart circulation,
left side = pulmonary and cardiac problem
right side = edema, hepatomegaly
cholesterol is much riskier, more waxy,
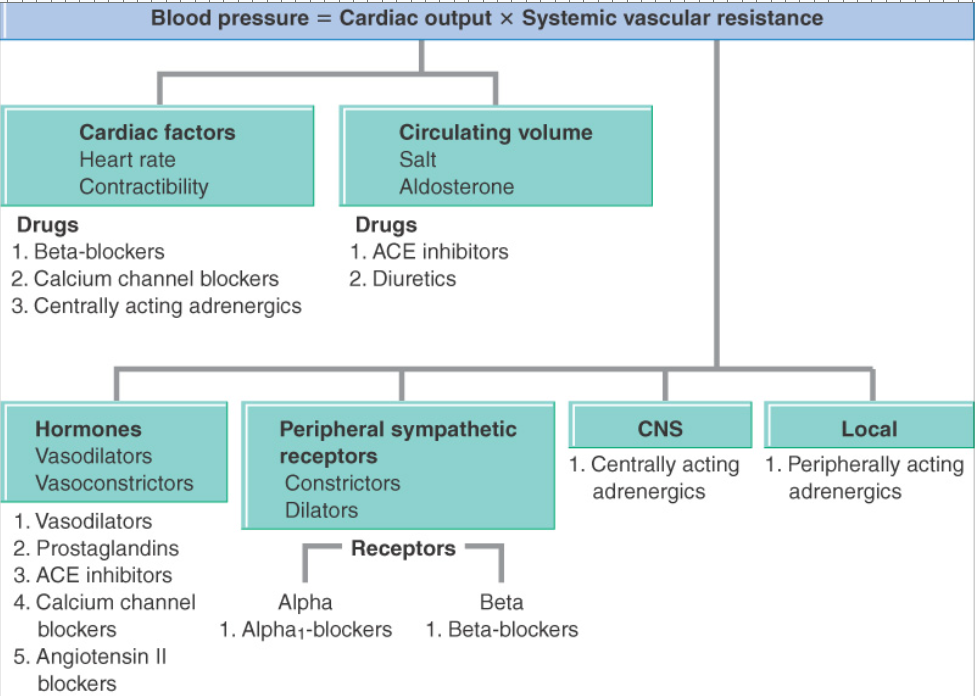
Drugs affecting blood pressure
Blood pressure = CO × SVR
CO = cardiac output
SVR = systemic vascular resistance (left, away, palabas ng puso)
Elements determining blood pressure
Heart rate
Stroke volume - amount of blood that is pumped out of the ventricle with eachheartbeat
Total peripheral resistance – resistance ofthe muscular arteries to the blood being pumped through
Categories rating the severity of hypertension
stages, based on BP measurements (adults) | dalawang beses na mataas(different days tinake), there could be high blood pressure, need doctor’s check up to make sure
Normal: < 130/85
High normal: 130-139/ 85-89
Stage 1: 140-159/90-99
Stage 2: 160-179/100-109
Stage 3: 180-209/110-119
Stage 4: 210 or greater/120 or greater
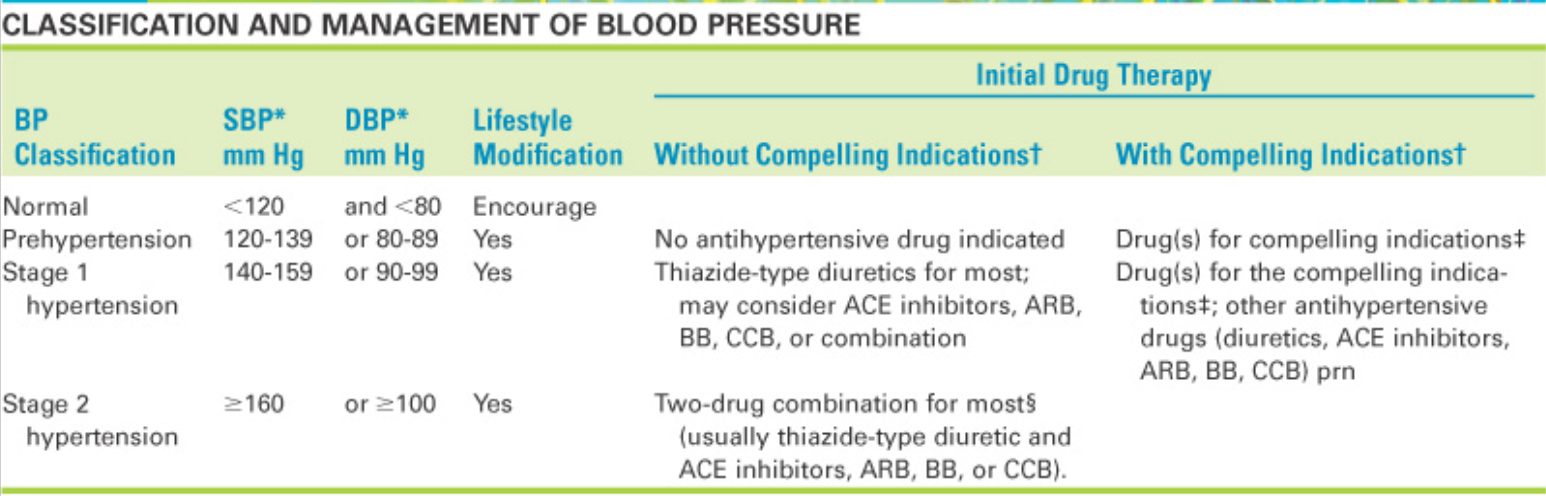
Classification of BP
Hypertension can also be defined by its cause
Unknown cause
– Essential, idiopathic, or primary hypertension
– 90% of the cases
Known cause (may dahilan)
– Secondary hypertension
– 10% of the cases
Ex. diabetes, tumor in brain
High diastolic BP (DBP) is no longer considered to be more dangerous than high systolic BP (SBP)
Studies have shown that elevated SBP is strongly associated with heart failure, stroke, and renal failure
Steeped care approach to treat hypertension
Step 1 lifestyle modification
Step 2 drug therapy is added (one type of drug)
Step 3 drug dose or class may be changed or another drug added
Step 4 includes all of the above measure with the addition of more antihypertensive agents until BP is controlled
Thiazide-type diuretics should be the initial drug therapy for most patients with hypertension (alone or with other drug classes)
The previous labels of “mild,” “moderate,”and “severe” have been dropped
smoking = vasocontriction
Anti-Hypertension Drugs
Diuretics
Diuretics are drugs that increase renal excretion of water, sodium & other electrolytes, thereby increasing urine formation & output
Used in the management of heart failure, renal & hepatic disease, hypertension
lythics = vasodilation
water + sodium = high blood volume/pressure
Thiazide diuretics
Decrease reabsorption of Na, water, Cl & bicarbonate in the distal convoluted tubule
Hydrocholorothiazide
Indapamide
Contraindicated in severe renal and hepatic impairment, hypokalemia, hyponatremia
Side effects are postural hypotension, hyperglycemia
Loop Diuretics
Inhibit Na & Cl reabsorption in the ascending loop of Henle
Frusemide
Bumetanide
CI : renal failure with anuria
SE: hyponatraemia
Potassium-Sparing Diuretics
Act directly on the distal tubule to decrease the exchange of Na for K
– Amiloride
– Triamterene
Spironolactone
– Block the Na-retaining effects of aldosterone in the distal tubule
CI: hyperkalaemia, renal failure
SE: dry mouth, rashes, with spironolactone gynaecomastiya can occur
ACE Inhibitors
ACE inhibitors and Angiotensin II receptor antagonists may cause first dose hypotension
Angiotensin-converting enzyme (ACE) inhibitors (activates angiotensin))
Block the enzyme (ACE) that normally converts angiotensin I to angiotensin II
Decrease vasoconstriction & decrease aldosterone production, reducing retention of Na and water Calcium Channel Blockers
Used to treat hypertension, heart failure, myocardial infarction, and diabetic nephropathy
– Enalapril
– Captopril (Capoten)
– Lisinopril
Side Effects:
– Can produce serious first-dose hypotension
– Cough, due to accumulation of bradykinin
– Hyperkalaemia, due to inhibition of aldosterone release
CI: In hypersensitivity to drug
Angiotensin II receptor blockers (ARBs) (inactivates angiotensin)
Compete with angiotensin II for tissue binding sites & prevent angiotensin II from combining with its receptors in body tissues
Used for hypertension, may be used as an alternative to ACE inhibitors in the management of heart failure and diabetic nephropathy.
» Irbesartan
» Losartan
» Valsartan
Side-effects
– Hypotension
– Less likely to cause cough and hyperkalaemia than ACE inhibitors
Calcium Channel Blockers
Drugs the prevent calcium ions from entering cells
positive inotropic effect = pinapalakas ung puwersa
no vasoconstriction
Vascular Smooth Muscle:
– Calcium channels regulate contraction
– If channels are blocked, contraction will be prevented and vasodilation will result
– Act selectively on peripheral arterioles and arteries and arterioles of the heart (no effect on veins)
Heart:
– Regulate function of myocardium, SA & AV nodes.
– Myocardium
Positive inotropic effect (increases force of contraction)
Calcium is blocked, contractile force will diminish
– SA Node
Pacemaker activity regulated by calcium influx
Calcium is blocked, heart rate is reduced
– AV Node:
Excitability of AV nodal cells is regulated by calcium entry
Calcium is blocked, discharge of Av nodal cells is suppressed (decreases the velocity of conduction through the AV node).
Three chemical families in CCB’s
Verapamil:
– Blocks calcium channels in blood vessels and in the heart
– Used for:
Angina Pectoris (vasodilation) = chest pain (5mins) | myocardial (MI) = chest pain (15-20 mins)
Hypertension
Cardiac dysrhythmias
– Careful administration/contraindications:
Cardiac failure, AV block, sick sinus syndrome
CVA = cardiovascular accident (heart failure), cerebrovascular accident (stroke)
Diltiazem(Cardizem): similar to Verapamil
Nifedipine
Relaxes vascular smooth muscle and dilates coronary and peripheral arteries
More effect on vessels less on myocardium
– Used for:
Prophylaxis of Angina Pectoris (vasodilation)
Hypertension
– Careful administration/contraindications:
Cardiac shock, advanced aortic stenosis, within one month of MI, acute attack of angina
Sympatholytics (Adrenergic Antagonists)
Suppress the influence of the sympathetic nervous system on the heart, blood vessels, and other structures
Beta 1 = heart | Beta 2 = lungs | Beta 1 and Beta 2 (good for heart, bad for heart) Blocker = both for heart
Five Subcategories:
– Beta-blockers
Most widely used antihypertensive drugs
Four useful actions in hypertension:
– Blockade of cardiac beta1 receptors
Decreases heart rate and contractility(decreases cardiac output)
Suppress reflex tachycardia caused by vasodilators in the regimen
Blockade of beta1 receptors on juxtaglomerular cells of kidney reduce release of renin
– Reduces Angiotensin II vasoconstriction, aldosterone mediated volume expansion
Long term use reduces peripheral vascular resistance
– Adverse effects:
Bradycardia, decreased AV conduction, reduced contractility
– Contraindicated:
Sick sinus syndrome / AV blocks / asthma (bronchoconstrictive effects)
Two subgroups:
– Nonselective Beta Blockers (Propanolol Beta1& Beta2)
Reduce heart rate, decrease force of ventricular contraction, suppress impulse conduction through the AV node, suppress secretion of renin, bronchoconstriction, inhibition of glycogenolysis.
Propranolol hydrochloride (not for lung problem)
Sotalol
Timolol
Pindolol
Levobunolol
Nadolol
Metipranolol
– Cardioselective Agents (Metoprolol-Beta1only)
Same as nonselective except it does not block bronchial beta2 receptors so does not increase airway resistance.
Atenolol
Acebutolol
Metoprolol
Bisoprolol
Esmolol
Betaxolol
Nebivolol
– Alpha1 Blockers
Prevent stimulation of alpha1 receptors on arterioles and veins, thereby preventing sympathetically mediated vasoconstriction.
Resultant vasodilation results in lowered blood pressure
nit given as first drug therapy
Blockade of Alpha1 receptors can cause orthostatic hypotension, reflex tachycardia.
– 1% of patients lose consciousness 30-60minutes after receiving their first dose
– NOT be used as first line therapy for hypertension.
Prazocin
Doxazosin
Indoramin
Terazosin
– Alpha/Beta Blocker
Block Alpha1 and Beta receptors
Blood pressure drops:
– Alpha1 blockade promotes dilation of arterioles/veins
– Blockade of cardiac beta1 receptors reduced heart rate and contractility
– Blockage of beta1 receptors on juxtaglomerular cells suppresses release of renin
– Reduce peripheral vascular resistance
Watch for:
– Bradycardia, AV heart block, asthma, postural hypotension
Prototypes: Carvedilol, Labetalol
– Centrally Acting antihypertensive
Methyldopa
Use for management of hypertension in pregnancy
Block sympathetic activity within the brain
– Adrenergic Neuron Blockers
Decrease blood pressure through actions in the terminals of the post ganglionic sympathetic neurons.
Inhibit/deplete norepinephrine release
– Resulting in decreased sympathetic stimulation of the heart and blood vessels
Watch for:
– Severe orthostatic hypotension
Guanethidine monosulphate
Derisoquine
Contraindicated in heart failure, phaeochromocytoma
Vasodilators
Vasodilators differ in respect to the types of blood vessels they affect.
– Dilation of arterioles
– Dilation of veins
– Uses:
• Hypertension, Angina, heart failure, myocardial infarction.
– Adverse Effects:
Orthostatic hypotension caused by relaxation of smooth muscle in veins.(dizziness, lightheadedness)
Reflex tachycardia places unacceptable burden on heart, tachycardia rises blood pressure
Expansion of blood volume-secretion of aldosterone—(diuretic may need to be added)
ANTIHYPOTENSIVE AGENT (sobrang bagsak ng BP) = MIDODRINE(pataas ng BP)
Hydralazine (sublingual, oral)
– Causes selective dilation of arterioles, has little or not effect on veins
– Peripheral resistance and arterial blood pressure fall
– Heart rate and myocardial contractility increase
inotropic, monotropic
– Uses:
Hypertension, heart failure
– Adverse Effects:
Reflex tachycardia, increased blood volume (sodium/water retention), Systemic Lupus Erythematosus-like syndrome (muscle pain, joint pain, fever, nephritis, pericarditis).
Sodium Nitroprusside
– Potent and efficacious vasodilator
– Fastest acting antihypertensive agent available
– Causes venous and arteriolar dilation
– IV infusion, onset is immediate
– Uses:
Hypertensive emergencies
– Potent and efficacious vasodilator
– Adverse Effects:
Excessive hypotension
Thiocyanate Toxicity (patients on med> 3 days)
– Administration:
Degraded by light--cover
ACE Inhibitors
Calcium Channel Blockers
Sympatholytics
Nitroglycerin
Antianginal drugs
Angina Pectoris
It is a coronary artery disease
Types:
Stable angina - no damage to heat muscle ; basic reflexes surrounding the pain store blood pressure (activity then rest)
Unstable angina - episodes of ischemia occur even when at rest
Prinzmetal’s angina - caused by spasm of the blood vessel, not just by vessel narrowing (bigla bigla nalang, whether rested or not)
Nitrates - Nitroglycerin (sublingual, patch dermal)
Nitrates are converted to NO in vascular smooth muscle
NO activates guanylate cyclase
Increase formation of cGMP so that the intracellular calcium levels decrease
Vasodilation
Used to treat or prevent angina
– Relieves anginal pain by relaxing smooth muscles in the blood vessels(vasodilation) by several mechanisms
Dilate veins
Dilate coronary arteries
Dilate arterioles
– Adverse Effects
Headache
Orthostatic hypotension
– Symptoms include lightheadedness and dizziness
Reflex tachycardia
Examples:
Glyceryl Trinitrate
Isosorbide Mononitrate(Ismo, Imdur)
Isosorbide Dinitrate (Isordil)
Nitroglycerin (Nitro.Bid,Nitrostat)
Nitrate of choice before chest pain begins
Calcium channel blockers - Diltiazem
Beta-adrenergic blockers - Metoprolol
Cardiac Glycosides
– Profound effects on the mechanical/electrical properties of the heart
inotropic
energy drinks = pampalakas ng puwersa
– Most widely used prescription drugs, they are the most dangerous (toxic—dysrhythmias)
– Prototype (Digoxin—only cardiac glycoside available in most countries)
– Uses:
• Heart failure, dysrhythmias
Cardiotonic Agents
Cardiac Glycoside - Digoxin
Phosphodiesterase Inhibitors - Inamrinone
Digoxin Antidote - Digoxin immune Fab
Digoxin
Exerts a positive inotropic action on the heart(increases the force of ventricular contraction,enhancing cardiac output)
Digoxin Uses:
– Heart failure:
Increased cardiac output by increasing myocardial contractility
–Sympathetic tone declines
Because Digoxin increases arterial pressure.
Heart rate is reduced, allowing more complete ventricular filling
–Increased urine production
Increased cardiac output increases renal blood flow
Loss of water (urine) decreases blood volume which reduces cardiac distension, pulmonary congestion, and peripheral edema.
–Decreased Renin Release
In response to increased arterial pressure, decrease in Angiotensin Decreased aldosterone decreases retention of sodium/water, reducing blood volume
Digoxin overall effects on CHF:
– Cardiac output improves, heart rate decreases, heart size declines, constriction of arterioles and veins decrease, water retention reverses, blood volume declines, peripheral and pulmonary edema decrease, weight is lost, exercise tolerance improves, fatigue is reduced.
Digoxin treats dysrhythmias:
– Through a combination of actions, digoxin can alter the electrical activity in non contractile tissue (SA & AV nodes, Purkinje fibers), as well as the ventricular muscle.
Toxicity:
– Dysrhythmias: AV block, ventricular flutter, ventricular fibrillation
– Predisposing factors:
Hypokalemia (usually secondary to the use of diuretics)
Elevated digoxin levels–Narrow therapeutic range
Heart disease
– Side Effects: anorexia, nausea, vomiting, fatigue, visual disturbances
– Administration: Count heart rate—less than60 or change in rhythm detected HOLD THEDOSE AND CALL THE PHYSICIAN!
Antidysrhythmic Medications (Antiarrhythmic Agents)
Class IA – Disopyramide (Norpace)
Class IB- Lidocaine (Xylocaine)
Class IC – Fleicanide(Tambucor)
Class II- Propanolol (Inderal)
Class III- Sotalol (Betapace)
Class IV- Diltiazem (Cardizem)
Dysrhythmia (Arrhythmia):
– Defined as abnormality in the rhythm of the heartbeat.
– Associated with high degree of morbidity/mortality
Types:
– Tachydysrhythmias
– Bradydysrhythmias
Vaughan Williams Classification:
– Class I: Sodium Channel Blockers
– Class II: Beta Blockers
– Class III: Potassium Channel Blockers
– Class IV: Calcium Channel Blockers
– Class V: Other Antidysrhythmic Drugs ( Adenosine, Digoxin)
– Class I: Sodium Channel Blockers
Sodium Channel Blockers:
– Block cardiac sodium channels
– Decrease conduction velocity in the atria, ventricles, and Purkinje system
– Class IA agents for atrial fibrillation, flutter; supraventricular & ventricular tachyarrhythmias
Eg: Quinidine, procainamide
SE: tachycardia, dry mouth, urinary retention, blurred vision
– Class IB agents for ventricular tachyarrhythmias (VT)
Eg: Lidocaine
– Class IC for life-threatening supraventricular tachyarrhythmias (SVT) and ventricular tachyarrhythmias (VT)
Eg: Flecainide
These drugs will be contraindicated in atrioventricular block
– Class III: Potassium Channel Blockers
Potassium Channel Blockers:
– bind to and block the potassium channels that are responsible for repolarization
Bretylium
– For life-threatening ventricular tachycardia and fibrillation
– can lead to hypotension
Amiodarone
– Effective against both atrial and ventricular dysrhythmias (only for life-threatening because of toxicity—lung damage/visual impairment
Other Antidysrhythmic Drugs
Adenosine:
– Slows conduction through the AV node
– Treats SVT
– Short plasma half life (less than 10 seconds)
Given IVP—closest IV site to the heart,followed by push of saline
Digoxin
Principles of Antidysrhythmic Drugs
Treat only if there is a clear benefit and then only if the benefit outweighs the risks
Treatment reduces:
– Symptoms (palpitations, angina, dyspnea, and faintness)
– Mortality
Antidysrhythmics : Bradydysrhythmias
Atropine:
– Muscarinic Antagonist
Competitively block the actions of acetylcholine
Stimulation of muscarinic receptors decreases heart rate
–Blocking these receptors will INCREASE heart rate
Isoproterenol:
– Acts on Beta-adrenergic receptors
– Activates Beta1 receptors on the heart-overcomes AV block, restarts the heart following cardiac arrest, increases cardiac output during shock
Anticoagulants
Prevent formation of new clots and extension of clots already present
Heparin and warfarin (Coumadin) are commonly used
Used to prevent or manage thrombophlebitis, DVT, and PE
Main adverse effect is bleeding
Drugs Affecting Blood Coagulation
Antiplatelet Drugs – Aspirin (generic)
Anticoagulants – Heparin (generic)
Low-Molecular Weight Heparins
Anticoagulant Adjunctive Therapy
Hemorrheologic Agent
Thrombolytic Agents – Streptokinase (Streptase)
Actions of anticoagulants
Anticoagulants
Antiplatelets
Thrombolytic drugs
Drugs Used To Control Bleeding
Antihemophilic Agents - Antihemophilicfactor (Bioclate)
Systemic Hemostatic Agents – Aminocaproic acid (Amicar)
Topical Hemostatic Agents
Heparin (unfractionated)
Intrinsic pathway is affected
Its major anticoagulant effect by inactivating thrombin and activated factor X (factor Xa) through an antithrombin (AT)-dependent mechanism.
Intravenous therapy
Require a PTT monitoring (Activated partial thromboplastin time)
Uses: Inhibit additional clotting, allowing body tolyse
current clot – Treatment and Preventative uses(hospital)
Pulmonary embolism (PE)
Stroke evolving
Massive deep venous thrombosis (DVT)
Adverse effects
Hemorrhage
Heparin-induced thrombocytopenia
Hypersensitivity reactions
Contraindications: GI ulcers, blood dyscrasias
Protamine (reversal agent)
Low-Molecular-Weight Heparin
Fixed dose schedule, don’t require aPTT monitoring• Can be used at home (unlike Heparin)
Much less likely to cause thrombocytopenia (than Heparin)Therapeutic use• 1st line therapy to prevent and treat DVT
Prevention of DVT following surgery
Treatment of established DVT
Prevention of ischemic complications
Adverse effects and interactions
Bleeding
Example
Enoxaparin
Warfarin
Oral anticoagulant
Antagonist vitamin K
Blocks the biosynthesis of factors VII, IX,X, II
Anticoagulant effects occur 3-5 days afteroral use
No effect on circulating clotting factors or platelets
Therapeutic uses
Long-term prophylaxis of thrombosis
Prevention of venous thrombosis and associated pulmonary embolism
Prevention of thromboembolism (inpatients with prosthetic heart valves)
Prevention of thrombosis during atrial fibrillation
Adverse effects
Hemorrhage
Fetal hemorrhage and teratogenesis from use during pregnancy
Do not use during lactation
Antiplatelet
Aspirin
Suppress the production of prostaglandins and thromboxanes due to its irreversible inactivation of the cyclooxygenase (COX)enzyme
Normally COX produces prostaglandins, most of which are pro-inflammatory, and thromboxanes, which promote clotting
Low-dose, long-term aspirin use irreversibly blocks the formation of thromboxane A2 in platelets, producing an inhibitory effect on platelet aggregation
This anticoagulant property makes aspirin useful for reducing the incidence of heart attacks
Adverse effect
Increase risk of GI bleeding
Clopidogrel
Irreversibly inhibits ADP receptor on platelet cell membranes, which is important in aggregation of platelets and cross-linking by the protein fibrin.
Used to inhibit blood clots in coronary artery disease, peripheral vascular disease, and cerebrovascular disease
Adverse effects include hemorrhage, Severe neutropenia, and Thrombotic thrombocytopenic purpura (TTP)
Aspirin and clopidogrel given orally
Fibrinolytic drugs
First Generation – Streptokinase
Second Generation – Altepase (tPA)
Third Generation – reteplase recombinant (retavase)
Streptokinase
A protein (secreted by several species of streptococci) can bind and activate humanplasminogen
Uses
Acute coronary thrombosis (acute MI)
Deep venous thrombosis (DVT)
Massive pulmonary emboli
Plugged AV shunt, central lines
Adverse effects
Bleeding
Antibody production
Hypotension
Fever
Contraindications Absolute
Previous intracranial bleeding at any time, stroke in less than a year, active bleeding, uncontrolled high blood pressure (>180 systolic or >100 diastolic).
Streptokinase is contraindicated in patients who have been previously treated with streptokinase, as there is a risk of anaphylaxis, a life-threatening allergic reaction, due to the production of antibodies against the enzyme.
Current anticoagulant use, invasive orsurgical procedure in the last 2 weeks,prolonged cardiopulmonary resuscitation(CPR) defined as more than 10 minutes,known bleeding diathesis, pregnancy,hemorrhagic or diabetic retinopathies,active peptic ulcer, controlled severehypertension
Recombinant tissue plasminogenactivator (t-PA, alteplase)
t-PA is produced by endothelial cells
It is nonantigenic and causes a more selective thrombolysis than streptokinase.
Alteplase, the recombinant t-PA, is produced by recombinant DNA technology.
Uses:
Acute myocardial infarction.
Acute cerebrovascular thrombosis.
Pulmonary embolism.
Central venous catheter occlusion
Adverse effects:
Major bleeding.
Cardiac arrhythmias.
Anaphylactoid reaction.
Cerebrovascular accident.
Intracraneal hemorrhage.
Reteplase
It has an increased half life than t-PA andincreased specificity for fibrin.
Its efficacy and adverse effect profile aresimilar to those of streptokinase and t-PA
Antifibrinolytic drugs
Interfere with the formation of the fibrinolytic enzyme plasmin from its precursor plasminogen by plasminogen activators
Block the binding sites of the enzymes or plasminogen respectively and thus stop plasmin formation
Aminocaproic acid and tranexamic acid
Use in bleeding tendencies
Lipid-lowering agents
HMG-CoA Reductase Inhibitors –Atorvastatin (Lipitor)
Fibric acid derivatives (Fibrates)
Bile Acid Sequestrants – Cholestyramine (Questran)
Nicotinic acid (niacin)
Cholesterol absorption inhibitors –Ezetimibe
HMG CoA reductase inhibitors(Statins)
Inhibits HMG CoA reductase, the rate-limiting enzyme in cholesterol synthesis
Increase LDL receptors in hepatocytes
This enables hepatocytes to remove more LDLs from the blood
Also decrease VLDL levels and increase HDL levels
Atorvastatin
Fluvastatin
Pravastatin
Simvastatin
Adverse Effects
Headache, GI side effects (e.g.abdominal pain, flatulence, diarrhoea,nausea andvomiting)
Hepatoxicity
Myopathy
Fibric acid derivatives (Fibrates)
Increase oxidation of fatty acids in liver and muscle tissue, decrease hepatic production of triglycerides, decrease VLDL cholesterol and increase HDL cholesterol
Main indication is hypertriglceridemia (high plasma triglycerides)
Adverse Effects
Nausea, vomiting and GI upset
Cholelithiasis (stones in the gallbladder) and cholecystitis (inflammation of the gallbladder)
Myopathy
Clofibrate
Fenofibrate
Gemfibrozil
Bile acid sequestrants
Bind bile acids in the intestinal lumen. This causes the bile acids to be excreted in feces and prevents them being re-circulated to the liver
Mainly used as an adjunct to Statins to decrease LDL cholesterol levels
Cholestyramine
Adverse effects
Constipation, diarrhea, nausea, vomiting, gastro-intestinal discomfort
Decreased absorption of fat-soluble vitamins
Nicotinic acid
Inhibits mobilization of free fatty acids from peripheral tissues, there by reducing hepatic synthesis of triglycerides and secretion of VLDL, which leads to decreased production of LDL cholesterol
Besides reducing LDL and VLDL levels, also effective in increasing HDL levels
Adverse effects
Flushing, itching, nausea, vomiting, diarrhea
Hepatotoxic
Hyperglycemia and hyperuricemia