Ab Psych Exam 2 Review !
Anxiety Disorders: a group of disorders that share symptoms of clinically significant anxiety or fear
Fear vs. Anxiety:
- Fear: alarm reaction and response to an immediate danger. Fear is a basic emotion that keeps us safe in the presence of a clear danger.
- Involves the nervous system: made of the central & peripheral systems
- Peripheral is in 2 parts: the Autonomic (involuntary control, automatic responses) and the Somatic (voluntary control, like muscle movement)
- In FEAR: the Autonomic Nervous System provides the involuntary response involving heart rate, respiration, etc; it’s mainly the Sympathetic branch of the Autonomic NS which enables the FIGHT OR FLIGHT
- Three components of Fear:
- Cognitive component is thinking: “I’m in danger!!!”
- Physiological component is experiencing: increased heart rate
- Behavioral component is doing: either “Escape!” or “Fight!”
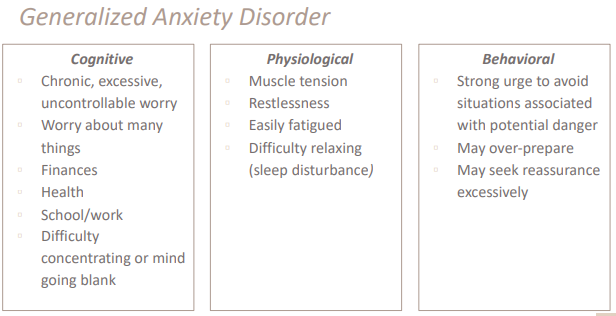
- Compared to fear, anxiety is: general feeling of apprehension in response to the possibility of future danger. No clear and present danger. Three components→
- Cognitive component is thinking: “Something bad might happen!”
- Physiological component is experiencing: muscle tension
- Behavioral component is doing: either “Avoid!” or “Over-prepare!”
- Fear become maladaptive when: fear is occurring in response to no immediate threat (ex: panic attacks when there is no present threat)
- Anxiety becomes maladaptive when: having a case of anxiety so severe that it causes dysfunction in daily life (ex: so anxious while taking a test, you have a complete meltdown and perform worse even though you studied a lot)
- Normal worry = you’re able to control your worrying and it doesn’t get in the way of daily activities - doesn’t cause significant distress, and limited to a specific & small number of realistic concerns - worrying lasts for only a short period of time
- GAD = worrying significantly disrupts your job, activities, or social life. You worrying is uncontrollable. Worries are extremely upsetting and stressful, worry about all sorts of things and tend to expect the worst. You’ve been worrying almost every day for at least six months.
Anxiety Disorders: GAD: Generalized Anxiety Disorder
^^Diagnostic criteria→^^
- excessive anxiety and worry (apprehensive expectation) occurs for at least 6 months, about a number of activities (work, school performance)
- individual finds it difficult to control worry
- 3 or more of the following symptoms (with some being present for at least 6 months):
- Restlessness, feeling on edge
- Easily fatigued
- difficult to concentrate, mind goes blank
- Irritable
- Muscle tension
- Sleep disturbance
- clinically significant distress or impairment in important areas of functioning.
^^Who is most at risk→^^
- Adults - Females more likely than Males (3.4% vs 1.9%)
- Most prevalent in 30-44, middle aged
- Adolescents (13-18) - Females more likely than Males (3% vs 1.5%)
- White Americans most diagnosed
- COMORBIDITY - risk of developing GAD for those with Panic disorder, OCD, Dysthymia, MDD, Substance use disorder, Cardiovascular disease, etc.
^^Theoretical perspectives on GAD→^^
- GAD Psychoanalytic perspective - GAD patients experience anxiety but don’t know why, it is because this anxiety is due to a threatened leakage of their unacceptable urges.
- GAD Learning (Behaviorism) perspective - GAD patients experience apprehension across many different situations b/c people are concerned about broad things; this perspective expresses the generalization of anxiety across many situations
- GAD Cognitive perspective - the Avoidance Theory of Worry and cognitive distortions discussed by Tom Borkovec: the idea that worry is a maladaptive response and attempt to solve a problem because it avoids the feared stimuli and thus maintains the worry through ^^inhibited emotional process^^ , no chance to face the fear.
- Thought vs. Imagery idea -- Worry is verbal/linguistic, allows for less imagery. Worry is language based, it is less likely to be imagery based. When people with GAD worry, they do it in thoughts, not in images. When you worry in images, it doesn't dampen the physiological stress arousal because you visualize it, so your worry goes down. But when you worry in thoughts, the discomfort remains constant b/c the physiological response that helps you cope with the distress is dampened.
- People with GAD believe worry helps them because it “helps them prepare” or “makes the feared event less likely to occur”
- Attentional Bias: Selective engagement with or selective disengagement from threat. GAD patients demonstrate a biased attention to threat. Exacerbated by misinterpretation of threat, tolerance of uncertainty. (they are uncertain of what the outcome may be)
- Anxious people’s brains are wired to interpret that anything may be a possible threat. They are always on the hunt for what they are worried about. More likely to interpret a non-threatening situation as threatening.
- GAD Genetics perspective - there can be a genetic predisposition for increased risk of GAD. → Includes the predisposition towards adopting ^^negative affect^^: whose basic personality trait is neuroticism; the higher-than-average tendency to experience negative moods, and an increased risk for anxiety disorders.
- Individuals with GAD have: an increased gray matter volume in the amygdala, decreased hippocampal volume, reduced frontolimbic structural connectivity, and greater right ventrolateral PFC activation.
- Neurotransmitter irregularities associated with GAD: GABA (inhibitory neurotransmitter) and Serotonin
- Benzodiazepines (ex: Valium) increase GABA
- Antidepressants (ex: Paxil) help with Serotonin
^^Treatments for GAD→^^
- Gold standard is Cognitive Behavioral Therapy (CBT)
- Cognitive restructuring - targets distorted cognitions by addressing likelihood of worst-case scenario + ability to handle the potential threats.
- Behavioral component - controlled exposure to thoughts/images/ situations being avoided. Involves relaxation training and planning of pleasurable activities.
- Third wave CBT - treatments that combine REBT (Rational Emotive Behavior Therapy) and CBT
- Emotion Regulation Therapy (ERT) is one type of third wave CBT that trains clients to combat certain worries through changing of principles and therapeutic processes
- Comprised of traditional and contemporary CBT methods: Mindfulness, emotion regulation skills.
- Medications for GAD - Antidepressants and benzodiazepines
- Beneficial like CBT, but CBT is better long-term
- can be expensive and can have bad side effects, but medication management can combat this
- helps balance neurotransmitter activity
Anxiety Disorders: Phobic Disorders
Phobia - fear of an object disproportionate to the threat it poses
Types of Phobic disorders: Specific phobia, Agoraphobia, & Social Anxiety Disorder
Specific Phobia: persistent and excessive fear of a specific object that is out of proportion to the actual danger they pose.
- Types of Specific Phobia: Fear of animals, fear of natural environments, fear of blood-injection injury, fear of specific situations
Social Anxiety Disorder: Intense fear of social situations. Underlying problem - excessive fear of being rejected, humiliated, or embarrassed.
^^Diagnostic criteria for Specific Phobia→^^
- Marked fear or anxiety about specific object/situation
- Stimuli always provokes immediate fear/anxiety, and it is always actively avoided or endured with intense fear.
- Fear is out of proportion to the actual danger of the specific object, and according to the sociocultural context.
- Fear, anxiety, or avoidance is persistent and is lasting 6+ months
- Fear, anxiety, or avoidance causes significant distress + impairment
- Disturbance is not better explained by another disorder
^^Who is most at risk - Specific Phobia→^^
- Females (12.2%) more at risk compared to males (5.8%)
- Ages 18-29 (10.3%), 30-44 (9.7%), and 45-59 (10.3%) similarly likely at risk
^^Diagnostic Criteria for Social Anxiety Disorder→^^
- Fear or anxiety about one or more social situations in which individual could possibly be scrutinized
- Individual fears they will act in a way or show symptoms that will be negatively evaluated
- Social situations almost always provoke fear or anxiety in them and situations are avoided or endured with intense fear or anxiety.
- Fear/anxiety is out of proportion to actual threat posed by the situation
- Fear, anxiety, or avoidance is persistent for 6 months or more
- Fear, anxiety, or avoidance causes significant distress or impairment in social occupation+ other areas of functioning
- Not better explained by other disorder/condition
^^Who is at risk - Social Anxiety→^^
- Females (8%) more likely than males (6.1%)
- Ages 18-29 most likely (9.1%) to develop social anxiety disorder, compared to 30-44 (8.7%) and 45-59 (6.8%)
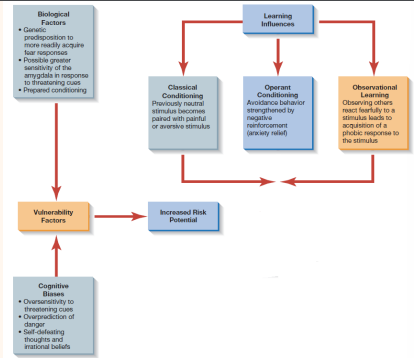
^^Theoretical Perspectives on Phobias→^^
- Phobias Psychodynamic perspective - Threatening urges are projected onto the feared object, and this fear is what prevents the urge from reaching consciousness
- Phobias Learning (Behaviorism) perspective - Phobias are learned and reinforced. Avoiding feared situation consistently leads to negative reinforcement - negative association formed
- Phobias Cognitive perspective - Maladaptive thoughts and beliefs related to phobic stimuli, such as an oversensitivity to threatening cues aka threat bias, over-prediction of danger, and having self-defeating thoughts (ex: person presented with feared stimuli start beating themselves down with how they will not be able to handle the situation, exasperates the symptoms even more)
- Phobias Biological perspective - there are biological causes for exaggerated fear: Genetic predisposition and/or greater sensitivity of the Amygdala and Pre-frontal cortex in response to threatening cues (amygdala is what induces response in face of fear)
^^Treatment for Phobic Disorders→^^
- Phobic Learning-based Approaches: gradual exposure to feared objects, creating a fear hierarchy, and systematic desensitization. Repeated exposure allows for panic to reach a peak, the point at which anxiety will now begin to coast and habituation occurs, leading to the mastery of anxiety.
- Fear hierarchy: ranked list of feared stimuli used in exposure exercises
- Two forms of Gradual Exposure - Imaginal = Imagining oneself in situation, and In Vivo = actual encounter in real life
- Systematic desensitization: clients gradually learning to handle distressing stimuli while maintaining relaxation - also uses fear hierarchy
- Flooding = client exposed to very high levels of fear-inducing stimuli either in imagination or in-vivo
- Cognitive Treatment Approaches for Phobias: cognitive restructuring and replacing self-defeating thoughts with alternative narratives.
- Cognitive restructuring = technique helping to identify and dispute irrational/maladaptive thoughts regarding phobias through processes such as Socratic questioning
- Medications for Phobias: Antidepressants, Beta Blockers, or Sedatives can help deal with phobia-induced fear, but only provides a temporary fix.
Anxiety Disorders: Panic Disorder & Obsessive-Compulsive Related Disorders:
^^Diagnostic Criteria for Panic Disorder→^^
- Recurrent and unexpected panic attacks.
- Panic attack = abrupt surge of intense fear or discomfort that reaches peak within minutes, during which time four or more of the following symptoms occur: pounding heart palpitations, feeling dizzy, trembling, sensations of shortness of breath, feeling of choking, nausea of abdominal distress, fear of losing control, chest pain, sweating, chills or heat sensations, paresthesia (feeling of tingling pins or needles), derealization, and fear of dying.
- At least one of the attacks has been followed by one month or more of one/both of the following: 1) Persistent worry or concern about additional panic attacks and their consequences AND/OR 2) a significant maladaptive change in behavior related to the attacks
- Not attributable to physiological effects of a substance or medical condition
- Not better explained by another disorder
- Having panic attacks does not necessarily mean you have panic disorder.
^^Who is at risk - Panic Disorder→^^
- typically develops in late 20s, Ages 30-44 (6%) and 45-64 (6.1%) most likely
- Females more likely than males (6.7% vs 3.3%)
- Native Americans most at risk (9.3%), followed by White (5.6%) and Hispanic (3.6%)
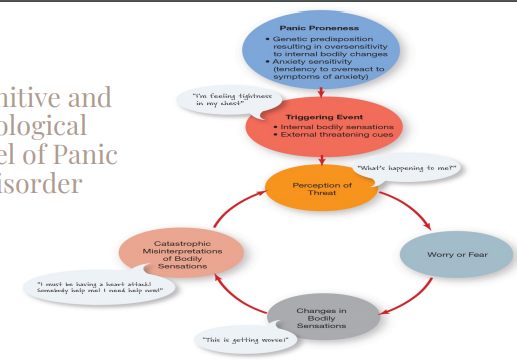
^^Theoretical Perspectives on Panic Disorder→^^
- Cognitive-Biological Model for Panic Disorder - Begins with a genetic predisposition resulting in oversensitivity to internal bodily changes, as well as anxiety sensitivity. This panic proneness coupled with a triggering event (i.e., internal bodily sensations and/or external threatening cues) leads the individual to have a perception of threat. →
- Sympathetic nervous system is activated and your fight or flight kicks in, increases in bodily sensation are mistakenly interpreted as a threat; can cause panic attack.
- Anxiety Sensitivity = fear of arousal-related bodily sensation, fear of fear itself - tendency to overreact to symptoms of anxiety
- Anxiety sensitivity is a transdiagnostic mechanism - meaning it is relevant to many disorders besides panic
- Biological Factors in Panic Disorder - Genetic predisposition increases risk of developing by a lot.
- Neurotransmitters: imbalances in gamma-aminobutyric acid (GABA) and serotonin cause heightened anxiety.
- Genetic variants of neurotransmitter system genes can influence development of pure/comorbid panic disorder
- studies show that during biological challenge, individuals with panic disorder are more likely to experience panic/anxiety symptoms
^^Treatment for Panic Disorder→^^
- Medications: Antidepressants & benzodiazepines help normalize activity of neurotransmitters ---- but bad side effects
- Cognitive Behavior Therapy for Panic Disorder: CBT combines techniques like self-monitoring, coping skills training, breathing training, relaxation training, exposure, and decatastrophizing
^^Diagnostic Criteria for Agoraphobia→^^
- Marked fear or anxiety about two or more of the following situations: using public transport, being in open spaces, being in enclosed places, standing in line or being in a crowd, being outside or being home alone.
^^Diagnostic Criteria for Obsessive Compulsive Disorder→^^
- Presence of obsessions, compulsions, or both.
- Obsessions are defined by = persistent thoughts, urges that are experienced at some time during the disturbance as intrusive and unwanted, and that in most individuals cause marked anxiety or distress. The individual will attempt to ignore these thoughts and urges, or to neutralize them through some other thought or action (i.e., performing a compulsion)
- Compulsions are defined by = Repetitive behaviors or mental acts that the individual feels driven to perform in response to an obsession. The behaviors are aimed at preventing & reducing anxiety, or preventing some dreaded situation; however these behaviors are not connected in a realistic way with what the individual believes they are designed to prevent; they are clearly excessive.
- The obsessions and compulsions are time consuming, or cause significant distress & impairment in important areas of functioning
- obsessive-compulsive symptoms are not due to a substance or medical condition
- the disturbance is not better explained by symptoms of another disorder
- OCD follows the vicious & repetitive cycle of: 1) Obsessive thought → 2) Anxiety → 3) Compulsive behavior → 4) Temporary Relief

Forms of OCD: Contamination, harm to loved ones, aggressive or inappropriate thoughts, religious (scrupulosity - fear of living in sin), symmetry & order, and sensorimotor (preoccupation with bodily sensations)
^^Who is at risk - OCD→^^
- Females more likely (1.8%) vs Males (0.5%)
- Most prevalent in 18-29 (1.5%) and 30-44 (1.4%) year olds
- Comorbid with anxiety disorders, depressive disorders, & other compulsive disorders.
^^Theoretical Perspective on OCD→^^
- Cognitive - OCD happens b/c of faulty interpretations that turn intrusive thoughts into obsessions. Five types:
- Threat overestimation: example in terms of religious OCD - thinking that cursing one time in church is equal to eternal damnation.
- Thought-action fusion: Believe that thinking about something makes it more likely to happen (ex - bad thoughts = bad deeds)
- Mental control: must get thoughts out of head to avoid doing something bad
- Intolerance of uncertainty: will continue with their routine only when they have perfect certainty that their fear won’t come true
- Perfectionistic beliefs: thinking that one impure thought means your whole service is ruined, so you restart from the beginning.
- Learning perspective - OCD develops when compulsions are negatively reinforced
- Biological perspective - OCD develops because gene variations affect chemical balance and lead to over-arousal of “worry circuit”
^^Treatment for OCD→^^
- Exposure with response Prevention (ERP): involves Exposure (prolonged exposure to stimuli that evokes obsessive thoughts) and Prevention (preventing compulsive behaviors from occurring) → helps client learn how to tolerate anxiety
- Cognitive Behavioral Therapy: works on correcting cognitive distortions and overestimation of consequences
- Medication: Antidepressants (SSRIs) are effective.
- Psychotherapy is usually more effective than medication alone, combination treatment can boost effectiveness of the drug treatment
^^Criteria for Body Dysmorphic Disorder→^^
- Preoccupation with imagined or exaggerated physical defect (blemish, wrinkling, swelling of face, moles or spots)
- Flaw usually doesn’t exist or is exaggerated
- individual feels ugly & deformed
- Extreme fear they will be judged negatively due to this flaw
- Obsessions in BDD - obsessed with perceived defect and may feel compelled to check self in the mirror many times
- Compulsions in BDD - compelled to fix cover, or modify perceived defect
^^Who is at risk - BDD→^^
- Median age of onset- 15 years old
- Those who do substance use, have OCD, or have social phobia at risk of developing comorbid BDD
- There is a genetic predisposition of developing BDD if there are relatives who also have it or another OC-related condition
- People with certain personality traits (e.g., perfectionism) more at risk for BDD
- Culture and environment, those who don’t fit their surrounding society’s expectations of beauty may be more at risk
- Those with negative life experiences like childhood bullying and trauma more at risk for BDD
^^Treatment for BDD→^^
- Exposure with Response Prevention (ERP) - Exposure involves intentionally revealing the perceived defect in public and response Prevention involves avoiding mirror-checking or excessive grooming
- ERP generally combined with cognitive restructuring: Evaluating distorted thoughts and beliefs about appearance in light of evidence
Hoarding Disorder: excessive acquisition of and difficulty discarding possessions
- Clutter causes distress and interpersonal conflict & danger
- Obsessions in Hoarding - recurring thoughts about acquiring objects and fears over losing them
- Compulsions in Hoarding - repeatedly rearranging stacks of possessions and refusing to discard them
- But differs from OCD: OCD has a more distressive component. In OCD, one can’t control their compulsions and have to perform that behavior, while in hoarding it is less.
Trichotillomania: Repetitive hair pulling that results in noticeable hair loss - scalp, eyebrows, etc.
Excoriation: Recurrent skin picking, sometimes resulting in sores, infections, and scars
Mood Disorders: Depressive Disorders (MDD, PDD, and Premenstrual Dysphoric Disorder):
Mood: an affective state that is relatively long and stable
Mood disorders: disturbances in mood that are severe or prolonged, impair ability to function
Depressive disorders are unipolar, while bipolar disorders are bipolar
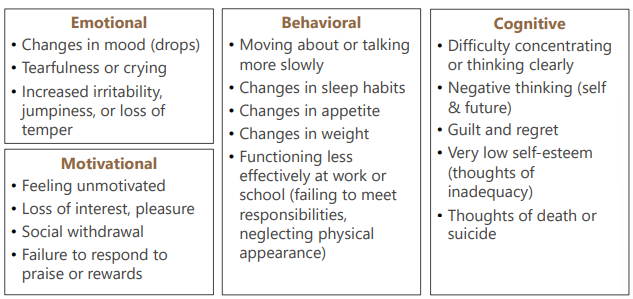
^^Diagnostic criteria for Major Depressive Disorder (MDD)→^^
- Mood disorder characterized by at least 1 major depressive episode, in the absence of mania or hypomania
- Depressive episode = depressed mood, feelings of hopelessness & worthlessness, changes in sleep patterns or appetite, & loss of motivation, interest, or pleasure
- MDD is characterized by 5 or more of the following symptoms: depressed mood, loss of interest/pleasure in almost all activities, significant unintentional weight gain/loss or decrease/increase in appetite, sleep disturbance, psychomotor changes (agitation/retardation), tiredness, fatigue, low energy, sense of worthlessness, excessive & delusional guilt, impaired ability to think, can’t concentrate, impaired decision making ability, recurrent thoughts of death.
- Symptoms cause clinically significant distress in important areas of functioning
- symptoms not due to any substance or medical condition
- symptoms do not meet criteria for a mixed episode
- No history of manic or hypomanic episode
- Not better explained by schizophrenia spectrum or psychotic disorder
^^Who is at risk - MDD→^^
- most common psychological disorder in US
- Females more likely at 26.1% vs males at 14.7%
- Gap between female vs male might be because of hormonal fluctuations (biological contributor), women tending to ruminate more than men (psychological contributor), women having higher stress burden than men (environmental contributor), and women being more likely than men to report depression (Sociocultural contributor)
- Age of onset is usually late teens to mid-30s
- Children: 3%, Adolescents 15-20%, and over 60: 11%
- Those who are multiracial or have multiple ethnicities are more likely to develop MDD, next most at-risk are Native Americans, and next after White.
- Biological risk factors: depression runs in the family -- heritable genetic predisposition
- Psychological risk factors: personality style, ways of thinking and problem solving
- Sociocultural risk factors: Female more likely than male, racial/ethnic differences
- Minority stress: Chronic, high levels of stress due to stigmatized social status
- LGBT at higher risk b/c of minority stress and experiences of rejection by family, coming out stress, or negative experiences in medical settings
- Environmental risk factors: early childhood trauma, major life events
- Chronic stress associated with increased risk for the onset and maintenance of MDD
- Stress life events: Interpersonal events (i.e., loss of loved one or relationship problems), job loss, physical illness, etc.
Comorbidity of MDD - comorbid highly with anxiety disorders (59.2%), Substance use disorder (24%), and impulse control disorders (30%)
- Also most commonly co-morbid disorder in eating disorders
- Like GAD, environment and genetic factors may shape the development of MDD
^^Theoretical Perspectives on Depression→^^
- Original vs maintaining causes theory:
- Original cause: What started the problem and
- Maintaining cause: What keeps the problem going
^^Theoretical Perspectives on MDD→^^
- Cognitive perspective - MDD develops through distorted thinking about self, others, & world (Beck)
- Learned Helplessness Attributional Theory: MDD develops through helplessness & attribution style, People become depressed because they come to learn that they are helpless to change their circumstances AND attributional style when facing stressful life events. (Seligman)
- Seligman’s Attributional Styles: People explain causes of negative events through 3 styles of attributions -
- Internal causes (personal inadequacies) vs. external causes (outside factors)
- Internal - “It’s all my fault”
- External - “Also this exam was particularly hard”
- Stable causes (unchanging) vs. unstable causes (changeable)
- Stable - “I will always fail & this won’t ever change”
- Unstable - “I underestimated how much I’d need to study, but I can spend more time next time”
- Global causes (applying to main domains) vs. specific causes (limited to one area)
- Global - “I’m clearly stupid and not cut out for this”
- Specific - “I’m not so great at this style of exam”
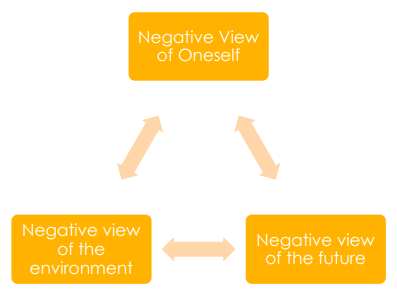
- Beck’s Theory of Depression: Distorted style of thinking increases risk of developing depression when faced with a stressful life event. Posits the Cognitive Triad of negative views (negative views of oneself, the future, and the environment)
- Beck’s Cognitive Distortions:
- All or nothing thinking - looking at things as either black or white, no in between shades of grey
- Overgeneralization - viewing one negative event as a never-ending pattern of defeat
- Mental Filter - dwelling on the negatives and ignoring the positives
- Disqualifying the positive - insisting that your accomplishments or positive qualities “don’t count”
- Jumping to conclusions - done through either (A) Mind reading: assuming that people are reacting negatively about you when there’s no evidence for it, and (B) Fortune telling: arbitrarily predicting things will turn out badly
- Magnification or Minimization - blowing things way out of proportion, or inappropriately minimizing the importance of things
- Emotional Reasoning - You reason based on how you feel (ex: “I feel like an idiot, so I must really be one” or “I don’t feel like doing this, so I’ll put it off”
- “Should” Statements - You criticize yourself or others with “should”, “shouldn’t”, “must”, or “have tos”.
- Labeling and Mislabeling - you identify with your shortcomings. Instead of saying “I made a mistake,” you tell yourself, “I’m a fool”, jerk or loser.
- Personalization and Blame - You blame yourself for something you weren’t entirely responsible for, or, alternatively, you blame other people and overlook ways that your own attitudes and behavior might contribute to a problem.
- All over Menfreed’s kitchen, dancing jumping magnificent Emo Eunhyuk shouldn’t label personalized bootys.
- Learning perspective - MDD develops when there is a lack of positive reinforcement (Lewinsohn, 1974)
- MDD develops when there are excessive demands for reassurance (Coyne, 1976)
- Lewinsohn’s theory - Changes in life circumstances alter the balance of effort and reinforcement (e.g., breakup, layoff) , so engaging in rewarding activities can reduce depression.
- James Coyne’s Interactional Theory of Depression - A lack of reinforcement results in problems in the depression-prone person’s relationships. Person may excessively seek reassurance, and subtle rejection cues deepen the depression.
^^Treatment for MDD→^^
- Psychoanalysis: Identify and understand underlying conflicts
- Behavioral: Develop and utilize social and interpersonal skills, increase participation in pleasurable activities
- Cognitive-Behavioral: combination of cognitive & behavioral techniques -- change negative dysfunctional thought patterns and develop adaptive behavior.
- Medication: Antidepressants, four classes --
- Tricyclics (many side effects)
- Monoamine oxidase inhibitors (MAO) - has many side effects
- Selective serotonin-reuptake inhibitors
- Serotonin norepinephrine reuptake inhibitors
- Electroconvulsive Therapy (ECT): last resort treatment, electrical current is passed through head to induce convulsion similar to seizure - for those who don’t respond to antidepressants
- lead to improvement in most, but can lead to side effects like memory loss and relapse risk also remains
MDD Specifiers:
- Seasonal effective disorder - MDD associated with the changing of seasons
- Postpartum depression - persistent and severe mood changes occurring after childbirth
^^Diagnostic Criteria for Persistent Depressive Disorder (PDD)→^^
- Formerly called dysthymia, applies to cases of chronic depression lasting for at least 2 years
- Symptoms same as MDD, but the intensity varies over a period of years
- Symptoms typically not severe enough to meet criteria for MDD
Premenstrual Dysphoric Disorder:
- More severe form of premenstrual syndrome (PMS)
- Range of symptoms in the week prior to menses: mood swings, tearfulness, depressed mood, feelings of hopelessness, anger/irritability, increased sensitivity
- Must be associated with dysfunction/impairment
Mood Disorders: Bipolar Disorders: Bipolar I, Bipolar II, and Cyclothymic:
- Bipolar Disorders: Mood shifts that are extreme from “up” to “down”.
- Manic episodes: the “up” mood shifts, feelings of elatedness, irritability, energized. Last at least 1 week, and may have psychotic symptoms.
- Depressive episodes: the “down” mood shifts, feelings of sadness, indifference, hopelessness
- Hypomanic episodes: episodes that are less severe than mania. Last at least 4 days, no presence of psychotic symptoms.
- Bipolar I: Manic episodes that last at least 7 days, manic symptoms that are usually more severe, to the point of needing emergent care. Depressive episodes will last approximately 2 weeks. --- At least one manic episode in the past, may or may not have had a major depressive episode in the past.
- Bipolar II: Not full blown manic episodes like in Bipolar I, patterns of depressive and hypomanic episodes. --- At least 1 hypomanic episode in the past AND at least 1 major depressive episode in the past too. No history of manic episode (If there is a manic episode, it’s Bipolar I)
- Cyclothymic: Periods of hypomanic & depressive symptoms lasting a period of 2 years, that do not meet criteria for actual hypomanic or depressive episodes.
- Milder form of bipolar disorder
- Long periods of mild mood swings (hypomanic & dysthymic moods)
- Few periods of normal mood lasting more than 1-2 months
- Begins Late adolescence
- 1 in 3 people with cyclothymic eventually go on to develop bipolar disorder
- ^^Diagnostic Criteria for a Depressive Episode→^^
- 5 or more of these symptoms are present during the same 2 week period and represent a change in previous functioning. At least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure:
- depressed mood, loss of interest/pleasure in almost all activities, unintentional weight gain/loss, decrease/increase in appetite, sleep disturbance, psychomotor changes (agitation/retardation), tiredness, fatigue, sense of worthlessness, delusional guilt, impaired ability to think, difficulty to concentrate, recurrent thoughts of death.
- ^^Diagnostic Criteria for a Manic Episode→^^
- distinct period of abnormally elevated, expansive, or irritable mood. Abnormally increased activity or energy lasting at least a week, and present most of the day, nearly every day.
- During this period of energy, 3 or more are present: Inflated self-esteem, decreased need for sleep, more talkative than usual, flight of ideas, distractibility, increase in goal-directed activity, excessive involvement in risky situations.
- Mood disturbance causes impairment in social or occupational functioning - may necessitate hospitalization to prevent harm to self/others, may also include psychotic features
- Episodes are not attributable to physiological effects of substance use, or other medical conditions.
- Bipolar Disorder Specifier #1: Rapid Cycling
- 4 or more full cycles of mania and depression within a year, without any intervening normal periods. - relatively uncommon, greater risk for suicide attempts
- Bipolar Disorder Specifier #2: “With Mixed Features”
- When symptoms of mania and depression occur within the same episode. Mood shifting between mania & depression. Less common
- Almost everyday for at least a week
- Someone with MDD could get this specifier, not enough symptoms to meet criteria for a bipolar disorder
- Bipolar with psychotic features
- ^^Who is at risk - Bipolar Disorder→^^
- Biological contributors: depression runs in the family, genetic predisposition
- Psychological contributors: personality style, ways of thinking and problem solving
- Sociocultural: Female more at risk, racial/ethnic differences
- Environmental: Early childhood trauma, major life events
- ^^Theoretical Perspectives on Bipolar Disorder→^^
- Biological: structural brain abnormalities may serve as risk factors. Abnormalities in:
- Volume of the striatum, left hemispheric white matter, thalamus, anterior cingulate, ventricles, hippocampus, subgenual prefrontal cortex
- Chromosomal regions & genes related to susceptibility to bipolar disorder: Serotonin transporter, Dopamine transporter (DAT), Brain-derived neurotrophic factor (BDNF), Mitochondrial DNA mutations, Glutamate receptors, Mitochondria-related genes, Chaperone genes, GABAergic neurons
- Stressful Life Events - both negative and positive life events may trigger a hypomanic or manic episode. Diathesis-stress model talks about how stressful life changes & biological influences interact with genetic predispositions to increase an individual’s vulnerability to bipolar disorder.
- Protective Factors - Social support from family and friends can buffer against negative impact of stress. Reduces likelihood of recurrent episodes.
- ^^Treatment for Bipolar Disorder→^^
- Psychotherapy: psychoeducation and focusing on targeting overly negative thoughts & overly positive thoughts present in mania
- Also promoting regular sleep + balanced lifestyle
- Family Focused Therapy: family involvement, working on communication skills. Uses psychoeducation too
- Interpersonal & Social Rhythm Therapy: resolving interpersonal problems (like grief, disputes, role transitions, isolation)
- Creating regular routines & schedules to make rhythm
- Medication: Lithium
- regulates glutamate in brain, too much glutamate causes mania, too little can cause depression
- An indefinite treatment (like insulin for diabetes)
- Side effects: headache, nausea, dry mouth, hair loss, lithium toxicity
Suicide:
Suicidal ideation - thoughts about self-harm with consideration of causing one’s death. Categorized as either active (statements displaying more of a willingness to take one’s life) or passive.
Aborted Suicide attempt - preparations to end life begin but not followed through
Interrupted Suicide Attempt - person begins attempt but is interrupted by external source
Suicide Gesture - appearance of attempt, without intent to die, but with the intention to communicate.
Suicide Cluster - 3 or more closely grouped deaths within three months (Types - Point cluster: close in time and location, Mass cluster: close in time only; usually influenced b media reports, and Echo clusters: occur over an extended time after the original cluster)
Mass Suicide - simultaneous suicide of members of the same social group.
Non-suicidal Self-Injuries (NSSI) - maladaptive coping mechanism, self-harm behaviors are not automatically considered suicidal behaviors because it’s important to also assess for intent.
^^Who is most at risk - Suicide→^^
- Lower and middle-income countries have higher suicide rates
- Older adults are group with highest suicide rates (70+ yrs old) and second leading cause of death for younger people (10-24 yrs old) is suicide
- Males die by suicide 2x more than females because they are more likely to use lethal means and thus are less likely to experience a failed suicide attempt
- American Indians & Alaskan Native likelier to die by suicide, followed by Caucasians
- LGBT minorities 2x likelier vs straight
- non-cisgender 2x likelier vs cisgender
- Cognitive & Behavioral Risk Factors - suicidal ideation, hopelessness, history of abuse, psychological disorders, history of NSSIs, traumatic life events, history of suicide attempts, substance abuse, sleep dysregulation, impulsivity
- Biological Risk Factors - Genetics, serotonergic systems, cortisol suppression = greater sensitivity to stress, HPA axis dysregulation, Chronic pain
- Environmental risk factors - unemployment, firearm access, divorce, media coverage, dictional media, real suicides, diseases
- We do not know when someone will make a suicide attempt because scales designed to measure the risk factors have very poor predictive value. There are many associated risk factors. - age, gender, geographic location, socioeconomic status, etc.
Protective factors: spirituality, social support, mental health services, lethal mean reduction
^^In what ways is risk different for different people→^^
- Different demographic groups are uniquely affected by suicide
- Social risk factors - stigma against mental illness, cultural distinctions, pressures of acculturation (American Natives), risk of upsetting social harmony (Asian Americans), navigating dual cultural contexts (African Americans), minority stress
- Important to tailor treatment and conduct research with cultural competence and humility.
^^Theories of Suicide→^^
- Theories that what leads to suicide may also be what leads to suicidal ideation, and previous theories didn’t provide that meaningful distinction between attempts and ideation
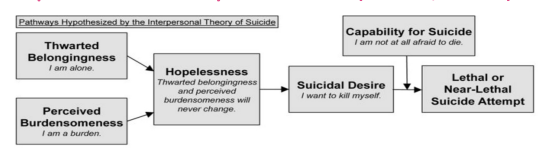
- Joiner’s Interpersonal Theory of Suicide: The presence of thwarted belongingness (“I am alone”) coupled with the presence of perceived burdensomeness (“I am a burden”) causes the formation of active suicidal desire. (Joiner 2005)
- This desire then transforms into intent when there is a presence of a lowered fear of death, which increases the individual’s capability for suicide (“I am not afraid to die and I want to kill myself, so I will”)
- So thwarted belongingness, perceived burdensomeness, hopelessness, reduced fear of suicide, and elevated physical pain tolerance are all present when any serious suicidal behavior occurs.
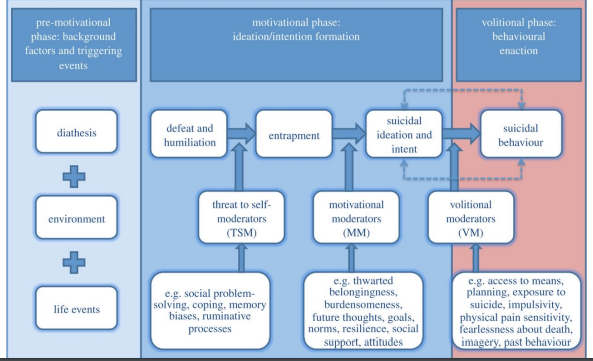
- O’Connor’s Integrated Motivational-Volitional Model: Three phases -
- Pre-motivational phase: background factors and triggering events like environment, life events, etc.
- Motivation phase: Life circumstances lead to feelings of defeat and entrapment which lead to the development of suicide attempt intention.
- Volitional Phase: addresses enactment of suicidal intent
- Motivational-Volitional Model differs from Interpersonal Theory because O’Connor focuses on defeat and entrapment while Joiner talks about belongingness and burdensomeness as root feelings.
- O’Connor’s theory also has the Volitional phase which expands beyond acquired capability and considers other factors.
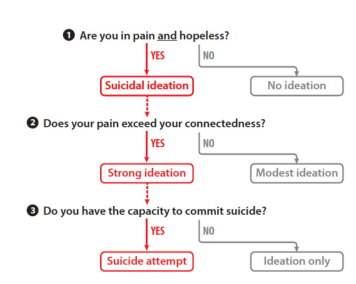
- Three-Step Theory by Klonsky & May: new theory on suicidal ideation, little research available
- Step one: pain + hopelessness = suicidal ideation
- Step two: Ideation escalates from passive to active when pain exceeds or overwhelms connectedness
- Step three: Strong suicidal ideation turns into an attempt when one has the capacity to attempt suicide - so dispositional contributors (genes), acquired contributors (repeated exposure to pain), and practical contributors (knowledge and access)
Stress and the Human Response:
Stress - pressures placed on organisms to adapt or adjust
Stress response is adaptive, but continuous activation of stress response is maladaptive
General Adaptation Syndrome: biological pattern of response to prolonged or excessive stress. Three stages:
- 1-Alarm stage - central NS awakens, body’s defenses are assembled and flight-or-flight is activated
- 2-Resistance stage - body begins to normalize heart rate, blood pressure, etc. Body enters recovery phase after initial shock but remains on high alert for a while.
- 3-Exhaustion stage - when activation in the first 2 stages continues over time, balance within body is broken down. This is when certain diseases may begin.
The Stress Response:
- HPA Axis - Hypothalamic Pituitary Adrenal Axis → central stress response system
- System regulated by negative feedback loop: In response to stress, the Hypothalamus releases ACTH hormone to the Adrenal glands. The adrenal glands produce adrenaline and cortisol, which cause increased heart rate, dilation of bronchioles, liver producing glucose, decreased digestive system activity, and increased blood pressure. -- activation of the fight or flight.
- The body then must return to a state of homeostasis (parasympathetic kicks in)
- But increased cumulative burden of chronic stress can lead to physical or psychological health problems.
Persistent and prolonged stress = inflammation in immune system - weakened immune system
^^Diagnostic Criteria for Trauma exposure→^^
- Exposure to trauma through directly experiencing it, eyewitness to others being exposed to trauma, learning of trauma of close family/friend, repeated exposure to details of traumatic event
- One of more of these Intrusion symptoms: involuntary trauma memories, recurrent distress dreams, dissociative flashbacks to trauma, distress reminders, physiological reactions to reminders.
- One or more of these Avoidance symptoms: efforts to avoid internal trauma reminders, efforts to avoid external reminders
- Two or more of these Mood symptoms: Amnesia for parts of trauma exposure, exaggerated negative beliefs about self or others, distorted cognitions leading to inappropriate blame of others, persistent negative emotional state, loss of interest, estranged feelings, loss of positive emotions
- Two or more of these Hyperarousal symptoms: irritability, angry outbursts, self-destructive behavior, concentration problems, sleep disturbance
- Duration: greater than one month
- Significant Distress/Impairment
- Not attributable to another disorder
PTSD Specifiers:
- Dissociative symptoms: Depersonalization = persistent experiences of feeling detached from others, and Derealization = recurrent experiences of unreality of surroundings, world is dreamlike
PTSD Preschool subtype: for children 6 years and younger
PTSD with a Delayed response: when the full diagnostic criteria for PTSD is not met until at least 6 months after the event, even if the onset and expression of symptoms may be immediate.
^^Theories on PTSD→^^
- Foa and Kozak’s Emotional Processing Theory: Theory that pathological fear structures underlie anxiety disorders. Having a fear structure causing you to avoid your feared stimuli will cause you to maintain that fear structure. It will remain unchanged until you face it.
- Foa & Riggs’ theory of Emotional Processing and PTSD: that these two cognitions maintain the fear structure:
- Two Emotional processing types impacting PTSD - 1) “The world is a dangerous place” and, 2) “The self is incompetent”
- Cognitive Theory of PTSD: consistent PTSD occurs when one is processing traumatic events in a way that makes it a current sense of threat.
- Done through negative appraisal of the trauma, and disturbance of autobiographical memory, as well as avoidance.
- Abstract way of thinking about trauma, which makes dealing with the trauma difficult.
^^Who is at risk - PTSD→^^
- 9.7% females and 3.6% of males develop PTSD at some point within lifetime
- Yet, men are more likely to experience a traumatic event → Military personnel at increased risk
- Males are more likely to be exposed to a traumatic event, but Females are more likely to develop PTSD once exposed to a traumatic event.
- Things that increase risk for exposure of trauma: Extroversion, Neuroticism, being a male, lower college education, History of childhood conduct problems, and family history of psychiatric illness
- Things that increase risk of getting PTSD given exposure: being a Female, younger age, Low SES, Race, Pre-existing psychiatric illness, trauma severity, previous trauma, genetic predisposition.
- Highly comorbid with mainly Depression, anxiety, substance use, and Eating disorders
PTSD & Resilience:
- Those who develop PTSD are the ones who experience a traumatic event and have a huge spike in disruption in normal functioning, followed by a maladaptive form of reaching normal functioning.
- Four types of responses to a traumatic event:
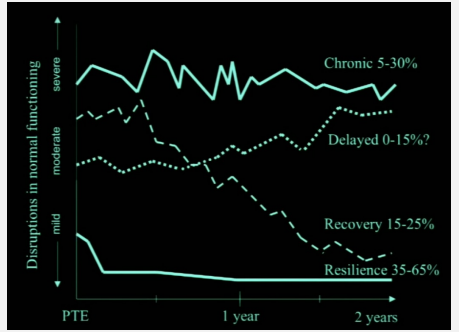
- Chronic: severe disruptions in normal function and then continuous maintenance of high level of disruption
- Delayed: Moderate disruptions and then disruptions decrease, but then get worse over time
- Recovery: Moderate disruptions and then there’s a sharp and abrupt decrease
- Resilience: Those who are resilient have mild disruptions in the face of trauma and the disruptions remain low over time. → Resilient interjectory is the most common response at 35-65%
^^PTSD Treatment→^^
- Psychotherapies: Prolonged exposure, CBT, CPT, Narrative exposure, Meaning making, Acceptance and acknowledgement
- CPT (Cognitive Processing Therapy): teaches client how to challenge and modify unhelpful beliefs related to the trauma - through trauma narrative & repeated exposure.
- Medications: Antidepressants, SSRIs, Antipsychotics
- Treatment resistant PTSD options: Psilocybin, MDMA, LSD, Ketamine
- Evidence for efficacy is low-moderate
^^Acute Stress Disorder:^^
- Differs from PTSD with an Onset of 0-28 days, symptoms have lasted from 3 days to 4 weeks, and symptoms include dissociative symptoms
- In comparison PTSD has an Onset of greater than or equal to 1 month, symptoms have lasted for one month to several years, and symptoms are more severe with Intrusive symptoms, hyperarousal, avoidance, and altered mood/cognitions
Reactive Attachment Disorder (RAD): disorder in children which includes a consistent pattern of inhibited, emotionally withdrawn behavior towards adult caregivers. Persistent emotional or social disturbance, and have experienced patterns of insufficient care.
Disinhibited Social Engagement Disorder - pattern of behavior where child interacts with adults (2 or more). Occurs in children who have experienced neglect or abandonment.
- Reduced reticence to approach or interact with unfamiliar adults
- Overly familiar verbal or physical behaviors (that is not culturally or age appropriate)
- Decreased “checking in” when the child wanders
- Willingness to go off with unfamiliar adults without hesitation