Health Psychology: Introduction
Health Psychology
Health promoting behaviors
Preventive rather than reactive
How do people stay healthy? (emphasis on HOW)
HEALTH:
- Complete state of physical, mental, and social well-being; not merely the absence of illness or disease, infirmity (WHO, 1948)
- WELL-BEING: optimum state of health
Foci of Health Psychology
- Health promotion and maintenance
- ^^Prevention^^ and treatment of illness
- Treatment: more cognitive behavioral therapy
- Etiology and correlates of Health, Illness, and Dysfunction
- Causes and factors
- Improvement of the Healthcare System and formulation of Healthcare Policy
Development of Health Psychology
- Mind-Body Relationship
- Human prehistory
- superstitious
- Evil Spirits = illness
- Treatment = exorcism (trephination)
- Exorcism: physical corporal punishment; rationalizing torture
- Trephination: drilling into skull to remove evil spirit; treatment for head injuries
- Ancient Greeks: Humoral Theory of Illness
- 4 humors
- blood (passionate personality)
- black bile (sadness/melancholy personality)
- yellow bile (angry disposition)
- phlegm (laid-back personality)
- Phlegmatic personality
- Excess of a particular fluid = personality
- Middle Ages
- Divine punishment = illness
- Treatment/Cure = physical/corporal punishment => penance (prayers and good works)
- Continued exorcism but illness is divine punishment
- Penance: undoing (defense mechanism)
- Extended superstition
- Renaissance
- advancement of the technical basis of medicine
- Invention of the microscope in the 1600s
- Increased dependence on laboratory/physical findings as basis for health and illness
- Clinical Eye: can use labs to confirm diagnosis but should not be too dependent on it
- Modern Times
- Psychodynamic Contributions
- Sigmund Freud: Conversion Hysteria
- Unconscious Conflict = physical disturbances that represent ^^repressed psychological conflicts^^
- Anna O. = diagnosed as having hysteria
- Physical manifestation of a psychological conflict
- Best treated with hypnosis
- Psychosomatic Medicine
- Flanders Dunbar (1930s) and Franz Alexander (1940s)
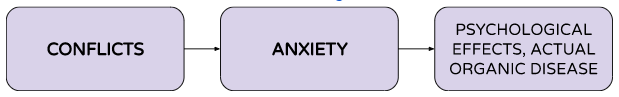
- Conflicts led to anxiety and anxiety show up as physiological symptoms and sometime actual organic disease
Current Perspectives
- Traditional East Asian medical philosophies and practices
- Acupuncture or acupressure
- Advancement of Neuroscience
- Development of Psychoneuroimmunology (PNI)
- Link between brain, physical symptoms and immunity
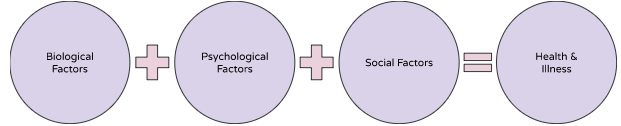
Biopsychosocial Model
- Consider biological, psychological, and social factors
- Help in planning treatment
Biomedical Model
- ALL illness can be explained on the basis of aberrant somatic/physical bodily processes.
- Psychological and social processes are IRRELEVANT to the disease process.
- Potential Liabilities of the Biomedical Model:
- Reductionistic single-factor model: reduces illness to simplistic cause
- Implicitly assumes a MIND-BODY DUALISM: mind is separate from body; psyche cannot influence physical body
- Emphasizes illness over health
- Fails to address certain puzzles related to health (e.g., Given 6 people exposed to measles, why do only 3 develop it?)
- Are there psychological and social factors that influence their health?
Advantages of the Biopsychosocial Model
- Biological, psychological, and social processes are ALL important determinants of health and illness.
- Mind and body cannot be distinguished in matters of health and illness.
- Mind influences body, what we feel physically can influence our mind as well
How do biological, psychological, and social processes interact if biological processes are micro-level processes and psychological and social processes are macro-level processes?
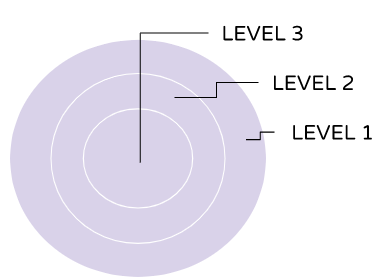
- Systems Theory Approach
- All levels of organization are linked to EACH OTHER hierarchically. A change in one level results in change in all the other levels.
- One would affect another based on their level
Clinical Implications of the Biopsychosocial Model
- Diagnoses and recommendations for treatment should consider interactions between and among all 3 factors (Bio, Psych, and Social factors)
- Makes explicit the Patient-Practitioner relationship as well as its significance
- The achievement and practice of health habits involve the interaction of all 3 factors as well.
- Ex social factor: support of family of them getting treatment
Current trends in medicine, psychology, and the health care system
Cases in Health Psychology: The Case of “Nightmare Deaths”
- 1970s: influx of refugees to the United States from Laos, Cambodia, and Vietnam
- Increase in sudden, unexpected, nocturnal deaths among males refugees from these countries.
- INITIAL CLUES: Deaths occurred within the first few hours of sleep; victim was noted to gurgle (like drowning) and move restlessly in bed; most victims had a rare, genetically-based malfunction in the heart’s pacemaker (have irregular heartbeat); autopsies showed NO SPECIFIC CAUSE OF DEATH
“Nightmare Deaths”: Bangungot?
- Psychosocial Clues:
- ONLY MEN from particular ethnic backgrounds were affected
- Deaths were clustered in certain families
- Survivors and victims’ relatives seemed to recall a dream that foretold the death
- Survivors said they experienced a severe night terror
- Many victims were noted to have either: watched a violent TV show prior to retiring to bed, or had a family argument, or were exhausted from working 2 jobs or from having full-time work AND learning English.
- Bangungot:
- acute pancreatitis (pancreas releases hormones and goes to shock and organ failure)
- Pancreas release hormones to digest the food
- Sudden flood of hormones = inflammation in the pancreas
- Cardiac arrest: part of multiple organ failure; heart dilates; cannot handle pumping blood efficiently
- “Asian Death Syndrome” : genetics may play in the occurrence
- Sleep paralysis: paradoxical sleep (you know you’re awake but you cannot move)
- Parasomnia, abnormal sleep features
- Death certificates = acute pancreatitis, multiple organ failures, septic shocks
The Need for Health Psychology
- Changing patterns of illness: Acute vs. Chronic Illness
- Examples of chronic illness: Lifestyle illness (hypertension, diabetes, high blood pressure), dementia
- Advances in technology and research: Genetic research & PNI
- Role of Epidemiology in Health Psychology: Morbidity and Mortality statistics
- What health behaviors can help prevent COVID-19
- Expanded Health Services: How can health psychologists help?
- Increased medical acceptance of health psychologists
- US, health psychologists work in clinics and hospitals; practice in tandem with psychiatrists, cardiologists
- Teaching medical doctors how to encourage patients
Career Paths in Health Psychology
- Practical Application: Medicine, Applied Medical Field
- Therapies (speech, physical)
- Research: public health, industrial/occupational health settings
- Types of Research: correlational studies, prospective and retrospective studies, longitudinal research, case studies
- Issues: promote health behaviors, prevent illness and accidents, control health care costs