Chapter 11 Human Physiology
Endocrine System Overview
Introduction
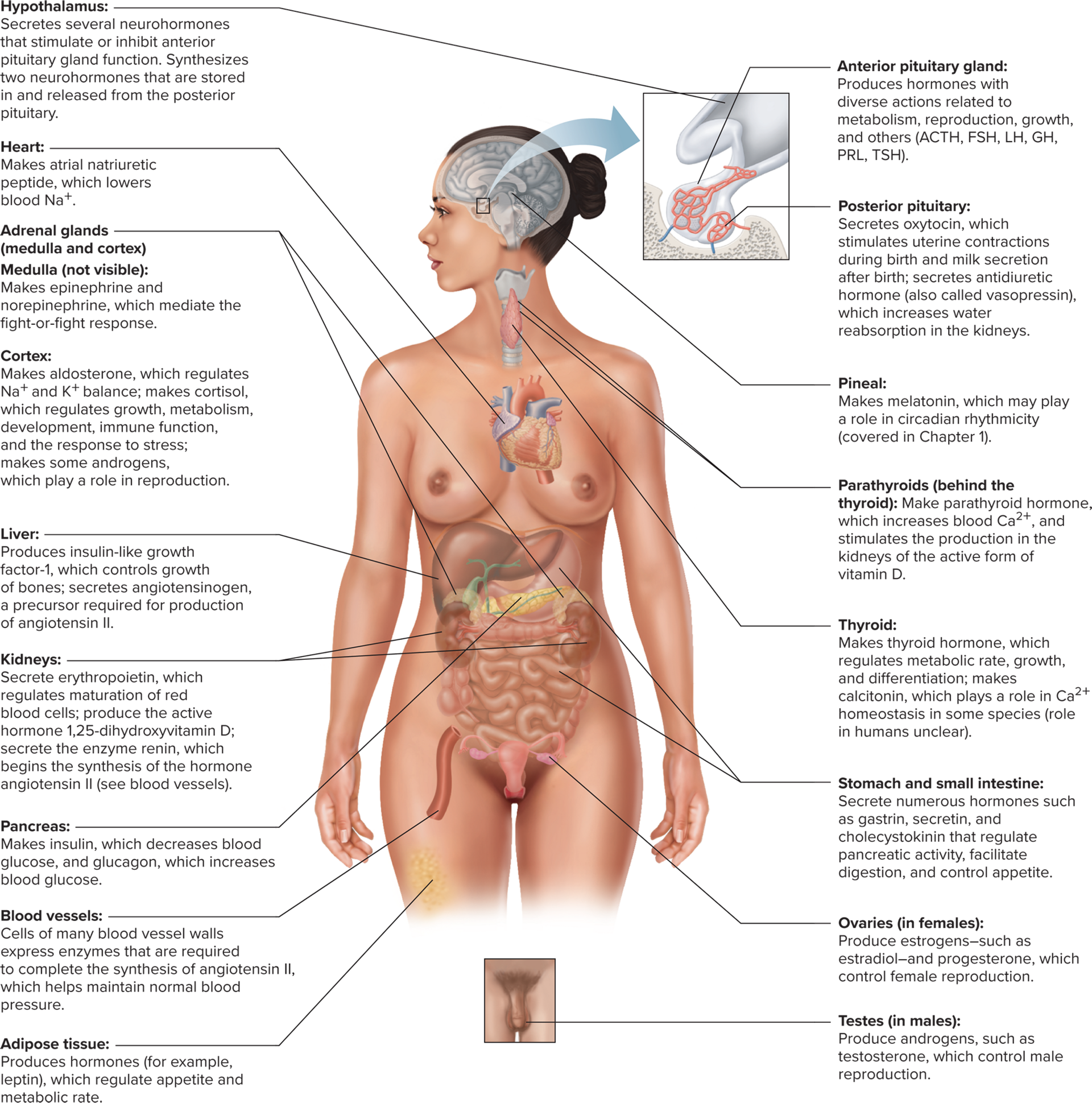
The function of the endocrine system is to provide a method of communication across the body
The four structural components of the endocrine system are the endocrine glands, hormones, blood, and target cells
The effectors of the endocrine system are the target cells
Endocrine glands: Ductless organs or groups of cells that secrete hormones directly intothe blood or other body fluids
Hormonal control systems help regulate homeostasis, stress responses, growth, and reproductive function
True: T or F, A single gland can secrete more than one hormone
Structural Classes of Hormones
The three major structural classes of hormones are amines, peptides/proteins, and steroids
Amine Hormones
Amine: Hormones derived from the amino acid tyrosine
Amine hormones include thyroid, catecholamines, and dopamine
Thyroid hormones: Amine hormones from the thyroid gland
Catecholamines: Amine hormones form the adrenal medulla, such as epinephrine
Dopamine: An amine hormone secreted by the hypothalamus
Peptide/Protein Hormones
Peptide and protein hormones are the most numerous class of all hormones
Peptide and protein hormones are primarily polar molecules
Synthesis
Polypeptides are packaged into preprohormones by the rough ER, then into prohormones by the Glogi apparatus, and then the hormone is secreted by exocytosis
Steroid Hormones
Steroids: Hormones synthesized from cholesterol by gonads, adrenal cortex, and the placenta
Steroid hormones are secreted via diffusion through the plasma membrane once they are made
Steroid hormones circulate in the plasma and they are bound to plasma proteins (aka albumin)
Hormone Synthesis
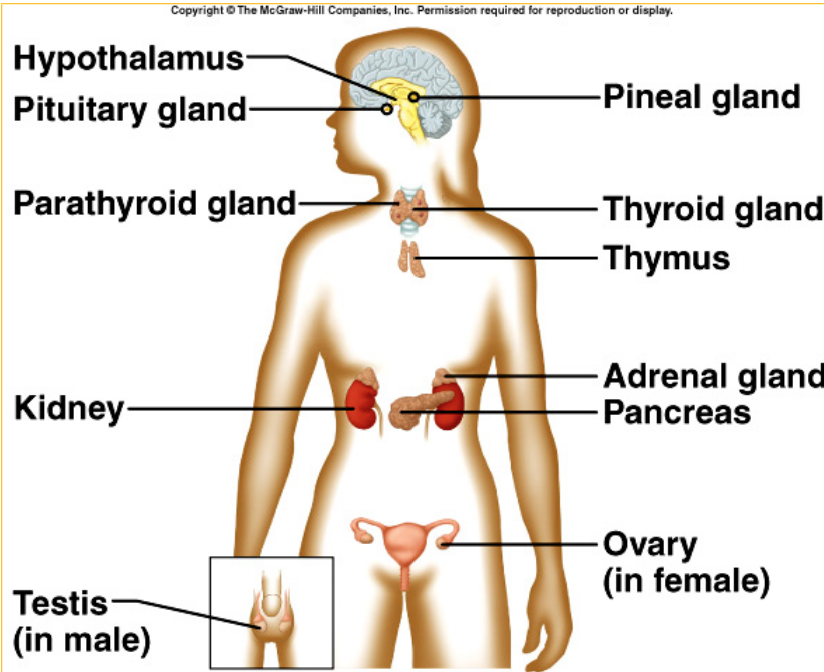
Adrenal Glands: Paired glands that sit atop the kidneys and are known for hormone synthesis
The adrenal glands have two separate areas, the adrenal medulla, and the adrenal cortex
Adrenal medulla: A modified sympathetic ganglion that releases catecholamines in resposne to sympathetic activation
The adrenal medulla releases about 20% norepinephrine and 80% epinephrine, which bind to adrenergic receptors
Adrenal cortex: Outer region of the adrenal gland that produces steroid hormones
Aldosterone: A mineralocorticoid that regulates sodium, potassium, and hydrogen ions to help with water balance; relelased by the adrenal cortex
Cortisol: A glucocorticoid that regulates metabolism of glucose and other nutrients to deal with stress response; released by the adrenal cortex
Adrostenedione: A less potent version of testosterone, used in sexual development; released by the adrenal cortex
The gonads (the testes and ovaries)
Gonads: Produce steroids that are important for sexual development and reproductive function
Testes: Mainly secrete testosterone and small amounts of estrogens; often converted to estradiol in target tissues by way of aromatase
Aromatase helps convert testosterone into estradiol
Ovaries: Secrete estradiol (estrogen) and small amounts of testosterone, as well as progesterone
Progesterone can be secreted by the corpus lteum in ovulation or the adrenal cortex
Hormone Signaling & Action
Hormone Transport in Blood
The structural components of the endocrine system are endocrine glands, hormones, blood, and the target cells (effectors)
Catecholamines & protein hormones are water soluble and are easily transported by being dissolved in the plasma after being released during exocytosis
Steroid hormones are nonpolar, so they attach to plasma proteins (in a hormone-protein complex) to travel through the blood after being secreted via diffusion
Most hormones are bound to carrier proteins, but a very small amount are not. This free hormone concentration is what ends up binding to receptors in target cells.
Some of the protein bound hormones in the blood dissacociate to reach receptor cells
Plasma hormone concentration is affected by the rate of secretion into the blood and the rate of removal from the blood
Rate of Removal
Hormone removal from the blood is called hormone clearance
Hormones that bind to the receptor end up decreasing the free hormone concentration
Hormone clearance occurs in the liver and the kidneys
In the blood the rate of removal of free proteins happens by enzymatic breakdown or binding
Catecholamines take minutes to hours to break down (free hormones, so not as protected)
Steroids and thyroids can stay from hours to days (why? they’re bound to transporters so they’re protected)
Hormones can be activated by metabolism to increase binding to receptors
Hormone Action
All tissues are exposed to circulating hormones, but only ones with the hormone receptor will respond
Non-polar chemical messengers can bind to intracellular receptors after diffusing through the cell membrane
Polar chemical messengers must have receptors built into the cell membrane
Methods of regulating hormonal response
Number of receptors (if a gland oversecretes, the target cells would down-regulate the receptor building so there isn’t too much taken in)
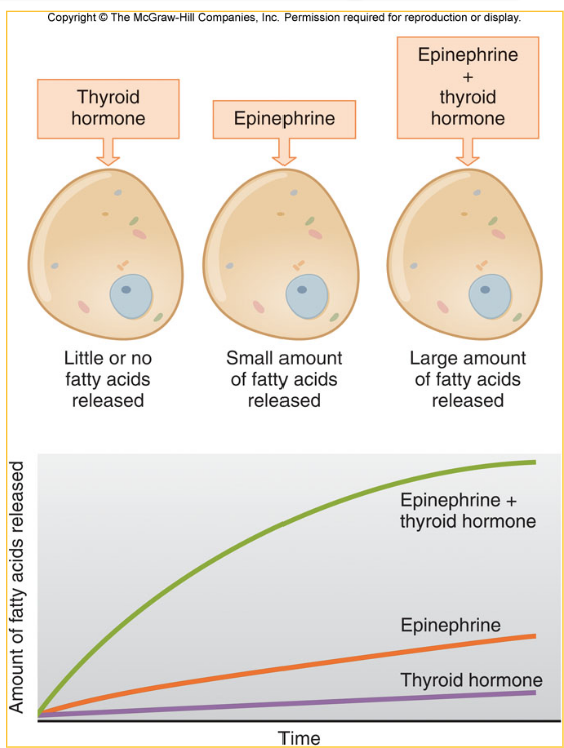
Permissiveness: An up-regulation of the number of receptors for one hormone due to the presence of the second hormone, allowing for a larger response
Cellular effects of polar hormones
Catecholamines and peptide hormones cannot cross the cell membrane, so the receptor must be built into the cell membrane
Most polar hormones activate a second messenger system upon binding to a receptor
Polar hormones have fast, non-genomic effects (aka changing enzyme activity)
Non-genomic: Effects of a hormone that have short-term effects, and the components are already built within the cell
Less frequently, polar hormones can have longer-lasting genomic effects that do affect transcription
Cellular effects of non-polar hormones
Steroid and thyroid hormones bind to intracellular receptors after diffusing through the cell membrane
Steroid and thyroid hormones form a hormone-receptor complex when the hormone binds inside of the cell
The hormone-receptor complex of non-polar hormones act as a transcription factor
Less frequently, non-polar hormones can bind to plasma membrane receptors to exert non-genomic effects
Control of Hormone Secretion
Hormone secretion is regulated by changes in plasma concentration of subsances, neurotransmitters released by neurons synapsing upon endocrine cells, or other hormones
Humoral Control: A modality of control for homone secretion where ion/nutrient concentrations within the blood act as the stimulus for hormone release
Neural Control: A modality of control for homone secretionl where neurotransmitter release from the autonomic nervous system can influence hormone release from many endocrine glands
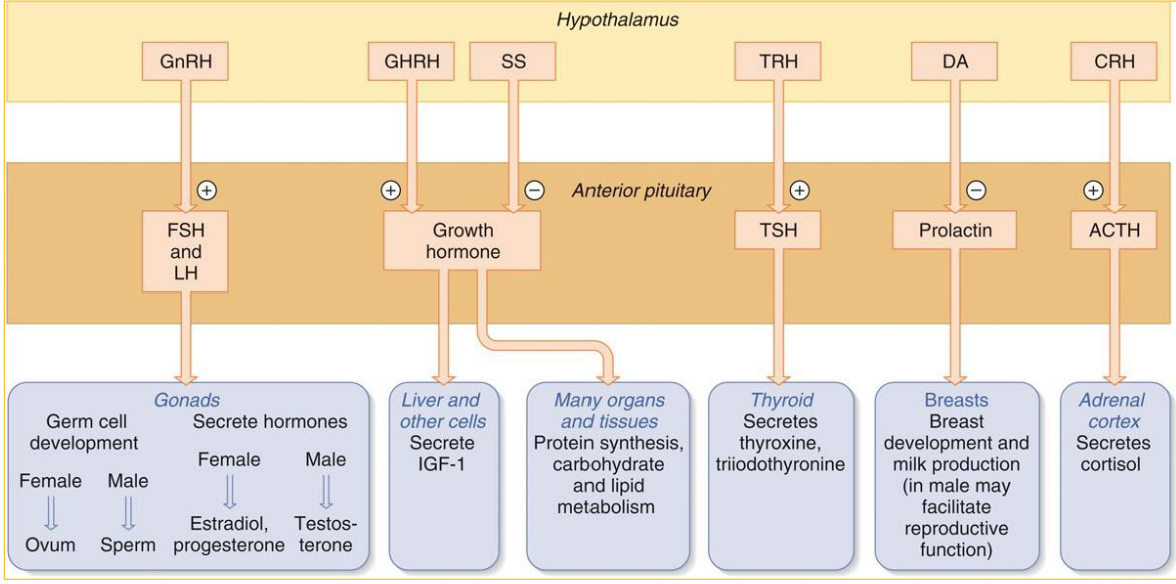
Hormonal Control: A modality of control for homone secretion where one hormone can signal the release of a second hormone from a different endocrine gland
Tropic: The hormone that singals the release of a second hormone from a different endocrine gland
Hormone System Regulation & Endocrine Disorders
The Hypothalamus & Pituitary Gland
The hypothalamus is part of the diencephalon & works with the pituitary gland
Infundibulum: The pituitary gland and the hypothalamus are connected by this tissue.
The infundibulum includes axons and mood vessels to connect the hypothalamus and the pituitary gland
The anterior pituaitary glands have more emphasis on blood vessels for hormone transport
Hypothalamus controls the release of anterior pituitary hormones via release of hypophysiotropic hormones
Hypophysiotropic refers to hormones from the anterior pituitary gland that causes the release of another hormone
Portal system: This modality includes veins are in between two separate capillary beds are portal veins that make up the system that supports hypophysiotropic hormone transport
Pros of the portal system include that it’s faster & less diluted instead of travelling all the way through the heart and wait for a wrap around back to effectors
Three-Hormone System
The first hormone in a three-hormone system is released from the hypothalamus and has a hypotropic effect on the anterior pituitary gland
The second hormone in a three-hormone system is released from the anterior pituitary gland and effects the third gland
The third hormone in a three-hormone system is released from a gland, that targets the effector
/
Hypophysiotropic hormone secretion is controlled by neural inputs & influenced by sensory info, biological rhythms, and developmental stages
Long-Loop: The third hormone in a three-hormone system can have a negative feedback on the hypothalumus or the anterior pituitary, also called ______ negative feedback
Short-loop: The second hormones can exert negative feedback on the hypothalumus, called _________ negative feedback
Mechanisms of Endocrine Disorders
Hyposecretion issues
Hyposecretion: There is a reduction in the amount of the hormone within the plasma, causing an impaired response
Primary hyposecretion: The reduction of hormones in the plasma is caused by the hormone-producing gland (the third hormone in sequence), caused by destruction of the gland, enzyme deficiency, or dietary deficiency
Secondary hyposecretion: There is too little stimulation by a tropic hormone, causing an unsafe reduction in hormone concentration; the second hormone is not doing enough so the final hormone cannot be released
If there are high levels of the tropic hormone, the hyposecretion is probably primary
If there are low levels of the tropic hormone, the hyposecretion is probably secondatry
Hypersececretion issues
Hypersecretion: Increased circulating hormone concentrations
Primary hypersecretion: The gland is producing too much hormone
Secondary hypersecretion: Excessive stimulation by the tropic hormone on the final hormone producer
Hyporesponsiveness issues
Hyporesponsiveness: The cell has a diminished response to hormonal inputs, despite a proper amount of hormone being present
Hyporesponsiveness can be caused by not enough receptors, dietary issues, or the signal transduction mechanisms
Hyperresponsiveness issues
Hyperresponsiveness: The cell has a very much increased response to hormonal inputs, although hormone levels are normal
 Knowt
Knowt