Physiology Test Cycle 1
General Physiology
Describe the types of tissue found in the human body
Connective Tissue
Connect, anchor, and support structures of the body and perform additional functions
bone
adipose - stores fat
blood - suspends cells in a fluid matrix, carries everything
loose - most common, supports blood vessels
dense - like a ligament
cartilage -support
Muscle Tissue
Skeletal: Voluntary, striated, long
Smooth: involuntary, short, spindle-shaped in the walls of organs
Cardiac: only in the heart, striated cells joined at intracellular junctions, involuntary
Nervous Tissue
In the brain, spinal cord, and peripheral neurons
highly specialized and sensitive
initiate, integrate, and conduct electrical signals to other cells to regulate body functions
Epithelial Tissue
Widespread through the body
specialized for secretion, absorption, excretion, and protection
Characterized by shape, arrangement and function
Cuboidal - cube shaped
Columnar - elongated
Squamous - flattened
Ciliated - hair-like protrusions
Simple - one layer
Striated - multiple layer
Attaches to other tissues at the basement membrane
Opposite sides of the tissue can preform different functions
Form tight junctions (close leakage)
Discuss the major organ systems and their principal functions
Circulatory - Transport of blood throughout the body
Digestive - Digestion and absorption of nutrients and water, elimination of waste
Endocrine - Regulation and coordination of many activities in the body, including growth, metabolism, reproduction, blood, pressure, water and electrolyte balance, and others
Immune - Pathogen defense
Integumentary - protection against the outside world (injury, pathogens, and dehydration) and temperature regulation
Lymphatic - collect ECF and return it to circulation, immune defenses
Musculoskeletal - support, protection, movement, blood cell production
Nervous - regulation and coordination of many activities, detection and response to changes in environments, states of subconsciousness, learning, memory, emotion, etc
Reproductive
Male - Production of sperm, transfer of sperm
Female - Production of eggs, provision of nutritive environment for the developing embryo and fetus, nutrition of the infant
Respiratory - gas exchange, regulation of H+ concentration in body fluids
Urinary - regulation of plasma through controlled excretion of salts, water, and organic wastes
Define Homeostasis and describe how it is regulated
Homeostasis is a dynamic process of give and take that maintains the processes of the body
Homeostasis is regulated by:
Negative feedback system: countermeasure (works to oppose the stimulus)
Temperature control
Reflex action: rapid involuntary movement in response to a stimulus
touching a hot plate
muscles contract, glands release hormones
Positive feedback system: Let’s make it worse and see what happens (moves stimulus in the same direction
Uterine contractions in childbirth
Local Response: action takes place local to the stimulus (platelet coagulation on damaged blood vessels)
Chemical Messengers allow cells to communicate includes hormones, neurotransmitters, paracrine and autocrine substances
some potential inputs and outputs affect the “pool” of materials creating different states of total body balance
Net gain (positive balance)
Net loss (negative balance)
stable balance
Gap Junctions: sharing is caring, a physical channel between cells
Juxtacrine signaling: cell on cell action, a receptor on one cell connects to the signal molecule on another cell
Feedforward System: “Pavloving” our own self, works early to minimize the effect of a trigger
Circadian rhythms
Describe the principle mechanisms used to regulate movement of biomolecules
The cell membrane is picky (polar head with a non-polar tail) it really only likes small, non-polar, uncharged objects.
Endocytosis: eat’em
fluid (pinocytosis)
eat (phagocytosis)
receptor-mediated
Exocytosis: Yeet’em
movement out of the cell using vesicles
functions: replacement of cell membrane, addition of cell membrane, route of secretion
Passive transport (no energy)
Diffusion - high concentration to low concentration
Things to remember - heat speeds things up, big things move slower, low density means faster diffusion, shorter distance or larger surface area means we’re quicker on the draw
Osmosis - diffusion of water
Diffusion through ion channels - selective and specific, determined by pore size, charge, and binding sites, can exist as open or closed gates
Ligand
Voltage - depend on membrane potential, molecules just slide on in, no need to bind
Mechanical
Facilitated diffusion - a carrier protein (GLUTS) that spands the membrane has a binding site for a particular molecule (Glucose) when glucose binds the carrier protein changes it shape and pushes the molecule to the other side of the membrane. The carrier protein then returns to it OG shape.
Depends on solute concentration, transport affinity, number of transports, speed of conformational change
Active Transport - gotta have that ATP in some way, moves molecules against the gradient (low to high)
Primary - direct use of ATP
NA+/K+ATPase (main control of membrane potential)
Secondary - electrochemical gradient plus another molecule
transporters have 2 binding sites where one molecule kinda hitches a ride with the ion.
Cotransporters: same direction
Countertransporters: opposite direction
Discuss the influence of osmolarity and tonicity on movement of water across membranes
Important tip to remember is that water chases salt.
Osmolarity - the total solute concentration of a solution
So lets say we have one mol of CaCl2 (3 solvents) in 0.5 L of solution. We would have 6 milliosmols in 1 liter.
its based on the number of solvents, so each element in a molecule counts as one
High osmolarity means low water content
Hypertonic Solutions have a high salt content, water will rush out of the cell (chasing the salt) cell shrinks
Isotonic solutions are pretty close to whats already in the body so the water just kinda chills. (0.9 NaCl)
Hypotonic solutions have a low salt content so the water is going to rush inside of the cell to get to the more saltier area. Cell expands
Hematology
Describe the components of blood
Blood is made up of formed elements (WBCs and RBCs) and Plasma which is just cell fragments (platelets)
Hematocrit (Hct) is the percentage that formed elements make up in the blood
normal Hct is about 45%
Anemia Hct is about 30%
No enough RBCs
Anemic patients may dehydrate themselves so hematocrit rises, which will decrease symptoms
Polycythemia Hct is about 70%
Too many RBCs, blood is thicc and the heart has to work harder to move it
If a patient is dehydrated the plasma (mostly water) is depleted this will increase the fraction of the formed elements aka raising the Hct.
90% of blood is water, so less water means a high percentage of RBCs
There are many organs that can affect the elements in the blood
The liver produces proteins that help maintain the osmotic pressure, these work to pull water back into the blood vessels (water chases salt)
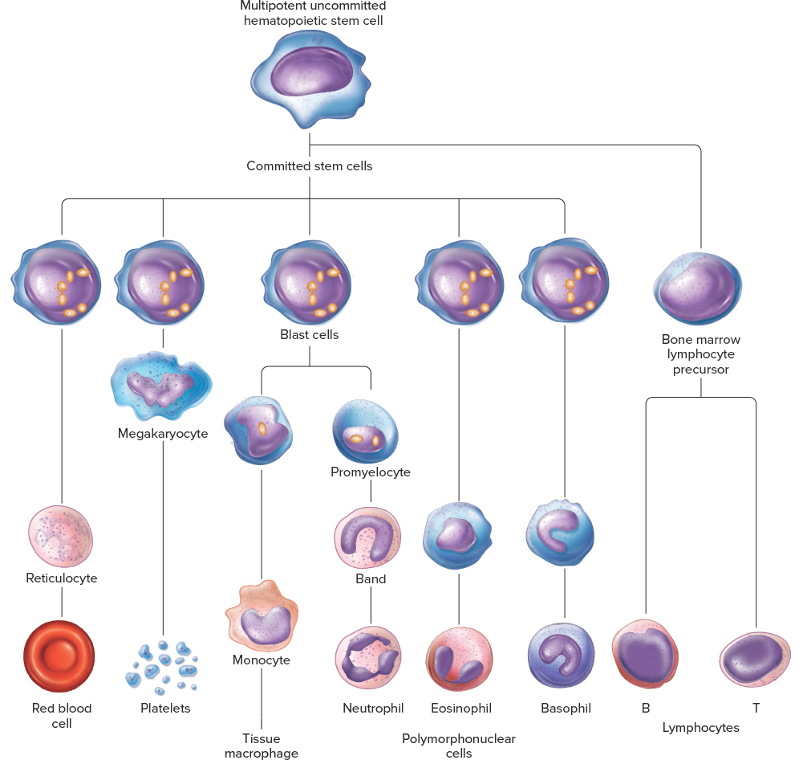
Discuss the synthesis and functions of various blood cells
Red Blood Cells - main function is gas exchange
Made in the red bone marrow
Live about 120 days
Recycled in liver and spleen
Reticulocytes - Baby RBCs, still contain ribosomes
Anemic patients will have increase numbers of Reticulocytes as they are trying to make up the difference
Platelets - come from megakaryocytes and clot the blood
Blast cell Lines
Promyelocyte → Band → neutrophils
A left shift is an increase in bands and present in infection as the body is trying to fight it off an infection
Monocytes
Monocytes become macrophages in the tissue
Eosinophils used to fight parasites and are a factor in immediate hypersensitivity reactions
Basophils secrete histamine and heparin
Bone Marrow Lymphocyte Line
B cells - immunoglobulins on surface
T cells -
Differentiate the major forms of anemia and know the causes
On a CBC anemia will look like low HGB, low RBCs.
Next we look at the MCV which is the mean cell volume
Microcytic anemia - low MCV
Iron Deficiency Anemia
Normocytic Anemia - MCV is in range
Anemia of Chronic disease (usually in CKD patients)
Macrocytic - High MCV
Folate or B12 deficiency Anemia
B12 is a vitamin that comes from eating animal products and assist in the uptake of folic acid.
Vegans have a low B12
Patients who have had a gastric bypass, are unable to absorb vitamins in their stomach, including B12
Discuss the key steps of hemostasis
A injury occurs in a vessel
Vascular spasm (aka vasoconstriction)
decrease the blood loss
hurt endothelial cells release endothelin which will activated smooth muscle contraction
Myogenic Mechanism
Nociorecptor activation
Platelet Plug Formation
Injured endothelials secret vWF (von Wilderbraun’s factor) which can attach to the exposed collagen
Platelets bind vWF and get activated.
Platelets secrete ADP, Thromboxane A2, serotonin which activate more platelets (platelet aggregation)
Platelets are linked by fibrinogen.
Thromboxane A2 and serotonin bind to the smooth muscle and cause contraction, increasing the vascular spasm
coagulation
Clot retraction and repair
platelet contraction
secretion of platelet derived growth factor
Secretion of vascular endothelial growth factor
Fibrinolysis (Clot busting)
Tissue plasminogen activator (tPA) on the cell membrane activates plasminogen (which is floating around) into Plasmin (aka PAC-Man)
Plasmin starts degrading fibrin mesh this will release D-dimer and Fibrinogen
D-dimer is an important marker for people with clots
Diagram the Blood Clotting Cascade
The liver is constantly creating clotting proteins that are floating around the bloodstream, but 9 times out of 10 they are usually inactivated
(Ca2+ is factor IV)
Intrinsic Pathway
More powerful
Factor XII floats on by our platelet plug, they interact. Factor XII is activated (XIIa).
Factor XI is activated by XIIa into XIa
Factor XIa activates IX into IXa
IXa activates VIII and they form a complex but they need the cofactor Ca+ and PF3 (platelet factor 3).
The Complex activates X to Xa. (common pathway starts here)
Xa reacts with V, PF3, and Ca2+ to form the prothrombin activator.
The Prothrombin activator which activates II (thrombin) into IIa
IIa reacts with fibrinogen (liquid-like) and links them together to form fibrin (jelly-like). IIa also activates XIII (using calcium) into XIIIa
XIIIa cross-links the fibrin strands to create a mesh to hold the platelet plug in place (no embolisms in this house)
The fibrin mesh is laid over the platelet plug so it cannot go anywhere
Extrinsic Pathway
Lightning Mcqueen (fast), weaker
When Tissues are injured they produce factor III which reacts with factor VII converting it to VIIa
VIIa can stimulate the activation of IX (intrinsic) or activate X (Common)
Define the natural anti-clotting system
NO and PGI2 which is secreted by normal epthelial blood cells these molecules keep the platelet from activating
Heparin-sulfate is bound to the plasma membrane and binds anti-thrombin III. The Activation of anti-thrombin 3 cleaves and inactivates, clotting factor II, IX, X.
Thrombomodulin binds thrombin (factor II). This tag teams binds and activates protein C. This activation allows for protein C to degrade/inhibit factor V and VIII
tPA on cell membranes will activate plasmin to break down the clot
Understand the mechanism of action of aspirin, heparin, warfarin, tPA, as well as overdose treatments
tPA given in acute ischemic strokes to break up the clot.
Gotta have CT results showing ischemic and not hemorrhagic or you’ll kill’em
Heparin keeps blood naturally thin by interfering with antithrombin III of endothelial cells
Aspirin inhibits cyclooxygenase which decreases Thromboxane A2 and prostaglandin production
A low dose (84 mg) can be taken daily to lower the risk of stroke or heart attack because it “calms down” the clotting system
A high dose knocks out more of the clotting system
Warfarin affects the the creation of clotting factors by blocking the integration of vitamin K
To combat an overdose of warfarin you would use a vitamin K
Immunology
Describe the cells and cytokines involved in immune response (CELL LINES (see hematology))
Leukocytes (WBCs)
Neutrophils
made in the bone marrow
phagocytosis
release chemicals involved in inflammation leads to vasodilation and chemotaxis
Basophils
made in the bone marrow
similar to Mast cells (involved in allergies)
Eosinophils
made in bone marrow
parasite fighters
allergic reactions
Monocytes
Made in the bone marrow
enter into tissues and transform into macrophage
Cytokines (messages from cells, dispatch team)
We got a ton of chemicals that work in tandem to activate the process of an immune response (immune and adaptive)
promoters and messengers
Redundancy and Cross talk
IL-1, TNF-alpha, IL-6
come from antigen presenting cells
target helper Ts and induce fever, stimulate systemic response
IL-2
come from most immune cells
target helper T
Discuss the role of lymphocytes in immune responses
Lymphocytes are the B and T cells as well as the NK cells
B cells initiate antibody response
mature in the bone marrow
T cells have two types CD8+ (cytotoxic) and CD4+ (helper)
mature in the thymus
NK (natural killer cells)
Explain the innate and adaptive immune responses - whats the same what’s different
Innate (maybe she’s born with it) gives us time to create an adaptive immunity, recruits immune cells to infection sites (the person calling 911)
Defense at body surface
intact skin - barrier from infection
Hair in the nose
coughing, sneezing - expels potential infections
salivary glands
lacrimal glands
stomach acid - HCl acid, eats away the bad guys
mucus - makes it hard to move
ciliary action - captures the bad guy
Inflammation
Stages of inflammation
Bacteria is introduced (Example: splinter in hand)
Cytokines cause vasodilation and capillary permeability (makes it easy for help to get in)
Neutrophils (first responders) are recruited; margination
Diapedesis results in neutrophils entering the affected tissue
Bacteria is eaten by the neutrophils, capilliaries return to normal
Chemotaxis
damaged tissue releases cytokines, margination (WBCs bind to capillary walls so they can get all up in the tissue), diapedesis (gettin all up in the tissue), chemokines
Killing by phagocytes
Certain carbs or lipids = PAMPS
opsonin - seasoning for phagocytes (makes the antigen look tastier to the phagocytes)(antibody or innate substance)
important in tissue repair
Inside the macrophage
endocytosis forms a phagosome, these connect with lysosomes (phagolysosome) who’s chemicals breakdown the bacteria, dead bacteria, exocytosis of remnants
Phagocytes do other things (not just big back behavior)
release of cytokines to continue the immune response
Helps regulate the inflammatory process (inflammatory mediators)
Activation of clotting/anticlotting pathways
Hormonal regulation of systemic response
Doubles down - extracellular removal of microbes
Complement Cascade
Bacteria (C3b) bind C3b receptors on phagocytes
locks it down (committed relationship), makes it efficient
Direct destruction via the MAC
Release of cytokines
Interferons
A type of cytokine
two families (I and II)
Work as an autocrine, paracrine, and endocrine agent
inhibits viral replication inside the cell
Cancer cells can mess with this factor, makes the body think they’re normal cells
Toll-like Receptors
Found on the surface of macrophages and dendritic cells
Release cytokines
IL-1, Il-2, Tumor necrosis factor
PAMPs (pathogen-associated molecular receptors)
pattern recognition of the bad guys and releases cytokines to begin the immune response
Adaptive is specific
lymphocytes are specific to their antigen, they have got to recognize and then clonal expand.
Lymphocytes are created in the thymus (Ts) and bone marrow (Bs) which are primary lymphoid organs
secondary lymphoid organs are sites where there can be lots of antigens (mouth, spleen, lymph nodes, etc).
Lymphocytes will divide here
Humoral response (antibody mediated)
activated B cells (antibody-antigen action and the go ahead from CD4+ Ts)
hang out in lymphoid tissue
Antibodies
multiple classes (IgM, IgG, ETC.)
2 heavy chains, 2 light chains
variable ends is where antigens bind
Constant ends are the same for most classes
IgM and IgG make up the bulk of specific immunity against bacteria and viruses in the ECF
IgE mediates immediate hypersensitivity and parasitic infections
IgA protects mucous membranes (think GI, respiratory, GU) and is secreted in breast milk (passive immunity)
IgD’s function is unclear
Bacteria gets in, antibody of B cell binds, B cell is activated by helper Ts (IL-2), clonal expansion into plasma (antibody making) and memory cells (so we’re quicker next time)
Antibodies only put a target on the back of a pathogen
enhance phagocytosis (opsonin)
active in complement system
Antibody Dependent Cytotoxity
Brings those NK cells into play
Cell Mediated Responses (T cell mediated)
Cytotoxic (CD8+)
attack cells - bind and secrete deadly chemicals (perforin)
Bind MHC I
Target infections inside the cell
Helper (CD4+)
absolutely necessary in activation of Bs, cytotoxic Ts, and macrophages, and NK
Keeps the body from attacking self
Bind MHC II
T Cell receptors - MHCs
MHCs have to bind to a presented complex where the cell breaks down the antigen and packages it up
2 Classes
MHC I - found on every cell except RBCs
MHC II - only found on macrophages, dendritic cells, and B Cells
Describe the role of antigen presenting cells in promoting immune responses
Gotta recognize we don’t want a reaction against self or non-dangerous things aka provides specificity
Macrophages, dendritic cells, and B cells (CLASS II MHC) eat a antigen and present the epitopes on its MHC II. Presented to Helper Ts
To activate the Helper Ts we still need a costimulus (provable self protein) and IL-1 and TNF-alpha
Any cell (basically) can act as a antigen presenting cell for cytotoxic Ts
Antigens can arise from inside the cell (the call is coming from inside the house)
cancer or virus
These are processed with MHC I and exocytosis and presented to the Cytotoxic Ts
NK Cells are lymphocytes but not antigen specific, no b or t cell receptors, they are enhanced by helper Ts
when enhanced by T helper cells NKs can kill intracellular viruses and cancer cells
Since NKs can secrete IL-2 they can increase their own response
Discuss the immune-tolerance immunity and immune memory
Immune Tolerance
Look at some point your body made antibodies and T cells against your own self
Clonal deletion - testing your T/B cells if they fail they die
Clonal inactivation - if your T/B cells start doing to much they get fired
The costimulus is only released if the antigen-presenting cells find something dangerous
Immune Memory
As a part of clonal expansion, B cells will divide into memory B cells so we’re quicker next time
Active immunity - exposing the patient to the antigen
slow
vaccines
Passive immunity - direct transfer of antibodies
not long lived but fast
Antibodies from mom to baby
When treating Rabies you don’t have time to wait for the active immunity from the vaccine to kick in, so you also give them human rabies immunoglobulin (passive) to hold them over
Identify systemic manifestations or responses to infection
A response of organs and tissues that are away from the site of infection/immune response
AKA acute phase responses - no indicators of disease
Usually triggered by cytokines released from macrophages
Examples -
Fever (brain)
secretion of acute phase proteins by the liver
liver also retains zinc and iron which are necessary for bacterial replication
Increase of release of WBCs
lipolysis - increase in available energy
Cortisol is dumped
STEROIDS SUPPRESS THE IMMUNE SYSTEM (NEGATIVE FEEDBACK)
Explain the factors that might alter the resistance to infection
Protein (malnutrition) - no amino acids for essential proteins
single greatest contributor to decreased resistance to disease
pre-existing disease
like DM
AIDs (kills CD4+ cells)
Caused by HIV which is a rRNA virus so hella high viral replication
Stress
low stress is good
high stress can make it worse
Moderate exercise
Genetic concerns
some people don’t make T/B cells (bubble boys)
the amount of sleep
Antibiotics
can disrupt bacterial cell-wall synthesis, protein synthesis, DNA replication
won’t affect the replication of human cells
BE CAREFUL
allergic reactions
some are toxics
bacteria can develop resistance
Summarize the common harmful or unwanted, human immune responses
Graft rejection
transplanted organs get attacked by cytotoxic Ts
have to do with a difference of MHCs, cytotoxic Ts target the MHC class I proteins on the transplanted organ
Cyclosporine and steroids suppress rejection but you gotta take them FOREVER
non specific immuno-suppression so the entire immune system is messed with
Transfusion rejection
Has to do with the antigens already found on our blood cells (A,B,O)
B cell response
A blood type people have antibodies against B
B blood type people have antibodies against A
AB blood type people have no antibodies against these antigens
O people have both antibodies (A and B)
recipients antibodies hemolyze the transfused cells
Gotta cross-match (unless its a code)
Rh negative vs. positive
Has to be exposed if they are Rh negative for there to be response.
If a mother is Rh- and in her first pregnancy is Rh+ baby is fine, mom gets exposed to the antigen
in future pregnancies the antibodies are already there so they can cross the placenta and mess with the baby leading to hemolytic disease of a newborn.
can prevent with passive immunity to mitigate the antibody response
Hypersensitivity (allergies)
immune response causes the damage
1st exposure causes sensitization, following immune exposures lead to the issues
Immediate (allergy)
most common and rapid onset, usually at the entry point of the allergen
antibody (IgE) mediated
IgE antibodies bind to Mast Cells (constant chain part) this is gonna trigger the release of histamines and other cytokines initiating a local inflammatory response
Anaphylaxis may result if a large amount of allergen is seen noted by vasodilation and bronchial constriction
Late-phase reaction - eosinophils secrete more inflammatory mediators and further sensitize the tissue so less allergen is needed
Eosinophils were originally important in killing parasites
Cytotoxic
Mediated by antibodies as in hemolytic disease of a newborn
Immune-complex
mediated by antigen-antibody complexes in their tissues, get trapped in capillary walls.
Immune complexes activate complement which can affect the tissue around the area
Delayed
TB Skin test
Autoimmune Disease
due to attacking self (no clonal deletion or inactivation)
Examples: MS, Type I DM, RA
Excessive inflammatory resposnses
Septic Shock
Secretion of nonspecific toxins, if there’s a lot of them you can kill the patient
the cytokines not the bacteria that causes septic shock
vasodilation (decreased bp)
high fevers
HIV can attack microglia cells which can cause “dementia”
Endocrinology
Describe and recognize the selected hormones’ synthesis, transport, metabolism, and excretion
Amine Hormones (AKA the catecholamines, thyroid hormones, and dopamine)
Catecholamines are made in the adrenal medulla by chromaffin cells that synthesize and release Epi and NorEpi
Amines are transported unbound in blood and interact with receptors on cell surface
Amines have a short life span (minutes-hours) and are inactivated by enzymes in the blood
Peptide hormones
Synthesized on ribosomes as pre-prohormones, cleaved by proteolytic enzymes in the rough ER into pro-hormones, packaged into vesicles by the golgi apparatus where the prohomone is cleaved into its active hormone and “left overs,” released via exocytosis
Transported unbound in blood and interact with receptors on cell surface
Short life span and are inactivated by enzymes in the blood
Steroid hormones
In the mitochonidria, cholesterol is converted to pregnenolone using the cytochrome 450 pathway and dehydrogenases. Intermediates are shuttle between the smooth ER and the mitochondria, diffuse into the blood
Since steroid hormones are lipophilic they need a protein buddy to travel through the blood. They bind intracellular receptors
Resistant to enzyme degradation and have a long life span (hours to days)
Thyroid Hormones (technically Amines but they’re getting their own sections)
Thyroid hormone is tightly regulated, when low levels are indicated the hypothalamus will release TRH which leads to the anterior pituitary releasing TSH which will increase protein synthesis in follicular epithelial cells of the thyroid. In the thyroid, Iodide is cotransported in with Na+, iodide will then diffuse across the follicle cell and into the lumen of the colloid, there it is oxidized and attached to a ring of tyrosine in thyroglobulin (TG), the iodinated rings of one MIT or DIT is added to a DIT at another spot (this determines T3 vs T4), endocytosis of thyroglobulin containing T3 and T4 molecules, Thyroglobulin is cleaved, at this point iodide can either be recycled or the hormones can be secreted
Thyroid hormones require a protein buddy in the blood and bind intracellular receptors
T4 is activated into T3 by metabolism (deiodinases)
Compare and Contrast the general characteristics of the presented hormones and hormone classes
Peptides and catecholamines bind to receptors on the cell membrane and free float in the plasma
Peptides and catecholamines are short-lived (minutes to hours) and quickly inactived by enzymes in the blood
Protein-bound fractions of steroid hormones a resistant to enzymatic degradation and have a long lifespan (hours to days)
Steroids and thyroid hormones need a protein buddy in the plasma and operate on intracellular receptors
Testosterone (steroid androgen) and thyroxine (amine thyroid) have little metabolic activity until they are activated in the target tissue
Differentiate between individual mechanisms of action of the selected hormones on their target tissues
Specific receptors on target cells respond to specific hormones
Up regulation increase hormone receptors to increase sensitivity
Down regulation decrease in the number of hormone receptors due to high hormone concentrations to decrease sensitivity
Permissive action (permissiveness) is where the presence of one hormone is required for full activity of a second hormone
One hormone acts to up or down regulate the number of receptors for a second hormone
Example Thyroid hormone and Epi
Neither thyroid hormones or Epinephrine can mobilize fatty acid from triglyceride stores in adipose. Thyroid hormones plus epi up-regulated epi receptors to allow for maximal effect
Thyroid Hormones have major 3 functions: metabolic actions, permissive actions, growth and development
Metabolic action: maintains energy for sodium-potassium pump and represents a significant portion of a person’s total generated heat
works on the small intestine to metabolize carbs
Works on the adipocytes to metabolize lipids
Permissive action
Necessary for GH release
up-regulates Beta receptors in many tissues (permissive to epi)
Growth and development
Helps in the synthesis of axon terminals, synapses, dendrites, myelin sheaths
required in pregnancy for proper development
w/o it we get congenital hypothyroidism (cretinism)
Required in adults for nerve and muscle reflexes as well as normal cognition
PTH works to maintain calcium balance
Bones: breakdown (osteoclasts)
Kidneys: increase calcium uptake and converts vitamin D to calcitrol
Calcitrol also helps in calcium balance
works on intestine to increase calcium absorbtion
Calcitonin the anti-flash to PTH
Bones: works to remodel bones (osteoblasts)
Kidneys: works to decrease calcium uptake
Cortisol
Muscles: works to increase amino acids in the plasma and to release glucose from muscular glycogen
Liver: increase glucose through hepatic gluconeogenesis
Adipose: release glycerol and free fatty acids
Pancreas: decrease insulin, increase glucogon to increase gluconeogenesis and lipolysis
Permissive to glucagon and epi
Epi and Norepi (Norepi only binds alpha-1, beta-1)
Alpha-1 receptors: increased intracellular calcium which leads to vasoconstriction leading to increase resistance which raises the MAP. Increased venous return. Pupil dilation. urine retention
Beta-1 receptors: Mostly in the heart, increased force and speed of contraction. No vessel influence. May influence renin to raise bp.
Beta-2 receptors: vasodilation, decreased systemic resistance and diastolic pressure. In the lungs it causes bronchodilation. In the liver, gluconeogenesis.
Aldosterone works on the kidney to increase sodium and water retention
Recognize and differentiate between the various input that control hormone secretion
Hypothalamus releases hyophysiotrophic hormones that act on the anterior pituitary gland
Corticotropin releasing hormone (CRH) → Stimulates secretion of ACTH
Thyrotropin releasing hormone (TRH) → stimulates secretion of TSH
Growth hormone releasing hormone (GHRH) → stimulates secretion of GH
Somatostatin (SS) → inhibits secretion of GH
Gonadotropin-releasing hormone (GnRH) → stimulates secretion of LH and FSH
Dopamine (DA) → inhibits prolactin
Anterior pituitary hormones act on tissues
FSH and LH → act on the gonads to secrete hormones (estradiol/progesterone (female) and testosterone (men))
GH → stimulates the liver to secrete IGF-1 as well as other organs to synthesize proteins and metabolize lipids and carbohydrates
TSH → stimulates the thyroid to secrete T3 and T4
Prolactin → stimulates milk production
ACTH → stimulates the adrenal cortex to secrete cortisol
cytokines and vasopressin can also cortisol
Hypothalamic-pituitary axis (HPA) describes the complex feedback loop
Short loop feedback: Negative feedback from the pituitary the the hypothalamus
GH inhibits GHRH release
Long loop feedback: Negative feedback from a pituitary target like the adrenal cortex
Cortisol inhibits CRH and ACTH release
Lots of things can affect the rate of hormone secretions
Can be multiple, stimulatory, and/or inhibitory simultaneously
Ions or nutrients (no ingredients no cake)
Neurotransmitters
Other hormones
Secretion rate: balance of negative and positive inputs
Example: Blood Sugar Control
Insulin is the only blood sugar lowering hormone in the body, its produced in the beta cells of the Islets of Langerhans
Promotes the storage of energy (glycogen, proteins, lipids)
suppresses the breakdown of nutrients
targets are the liver, muscles, and adipose tissue
these will pull glucose out of the ECF into the cell
release is controlled by blood glucose levels, glucagon, or indirectly by GH, glucocorticoids, and thyroid hormones
Glucagon is produced in the alpha cells of the Islets of Langerhans and work to increase blood glucose levels
increases blood glucose levels by stimulating insulin release
 Knowt
Knowt