3.7 Homeostasis & The Kidney
Homeostasis & The Kidney
Negative Feedback- Changes in the internal environment are restored to their original level by Negative Feedback.
- There is a Set Point for each condition determined by the brain.
- Deviations from the set point are corrected by negative feedback so the set point is restored.
- Uses a receptor - Monitors the condition & provides information to the brain.
- Effector- coordinates the response to restore the set point.
- Eg ; Body Temperature - Temp Rises, Brain Detects, Vasodilation & Sweating
- Temp Falls, Brain Detects, Vasoconstriction & Shivering
Positive Feedback - Enhances the size of the stimulus, and causes movement further away from the set point.
Eg; the Oxytocin hormone stimulates contraction of the uterus during labour, which in turn stimulates the production of more oxytocin.
Excretion
Excretion- The removal of metabolic waste made by the body.
Metabolic Waste- Waste produced as a result of a metabolic process e.g Urine NOT FAECES.
Nitrogenous Waste- Fish release nitrogen as Ammonia (NH3).
Birds excrete their nitrogen as Uric Acid (C5H4N4O3)
Mammals excrete their waste as Urea.
Deamination- The amino group is removed from the amino acid to form Ammonia which is excreted as Nitrogen is toxic.
The remainder of the amino acid molecule is used in respiration.
Urea is made in the liver by combining 2 molecules of ammonia with 1 molecule of Carbon Dioxide.
Urea synthesis requires a lot of energy, but it is a lot less toxic than ammonia.
Urea is the main nitrogenous waste product in humans. It is carried from the liver to the kidneys in the bloodstream.
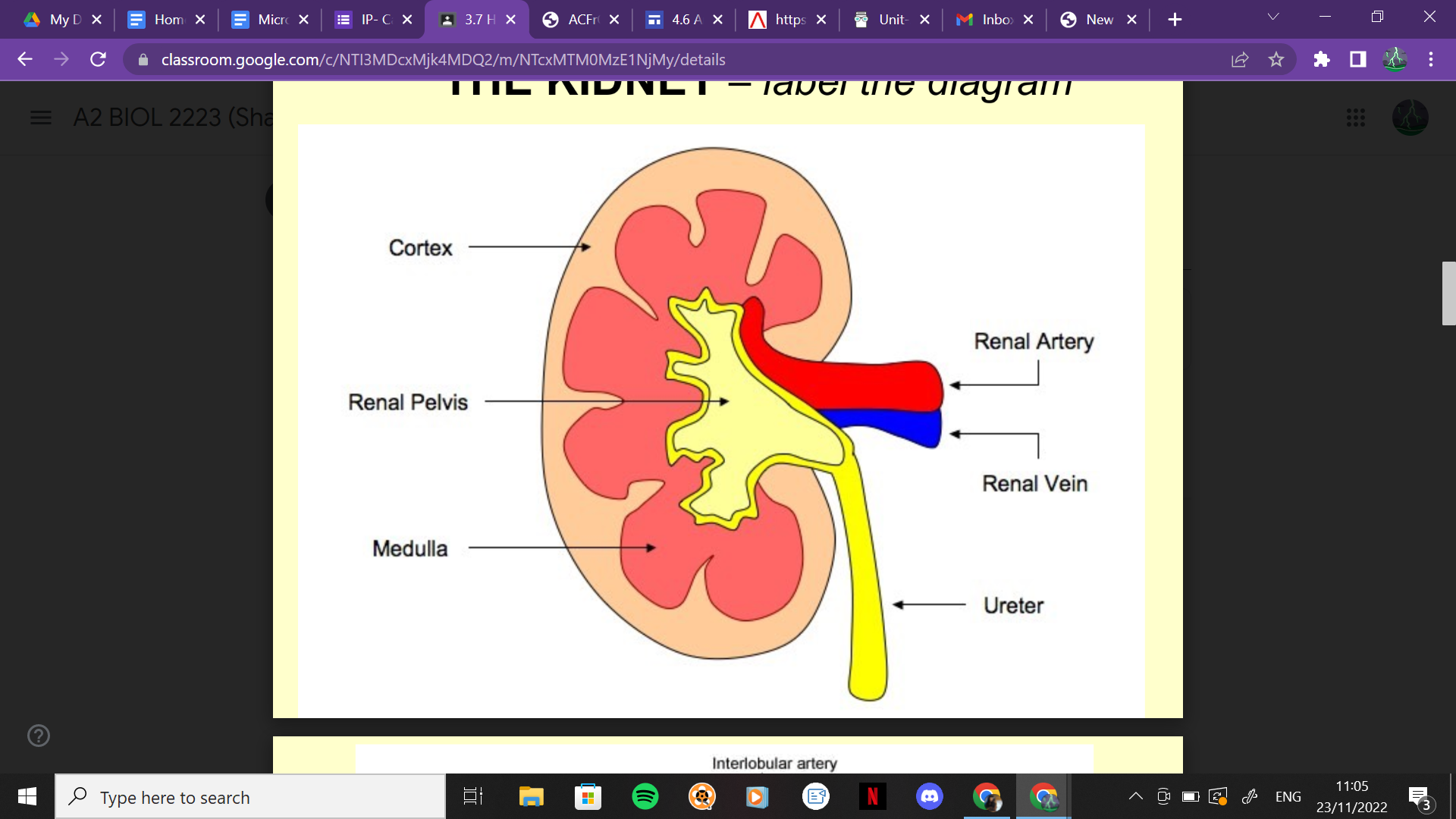
The Kidneys
Kidneys have 2 functions;
1. Excretion of Nitrogenous Waste
2. Osmoregulation - regulating the water content of body fluids.
- Blood in the kidney is under high pressure arriving from the renal artery
- Filtered Blood leaves the kidney in a renal vein.
23/11/22
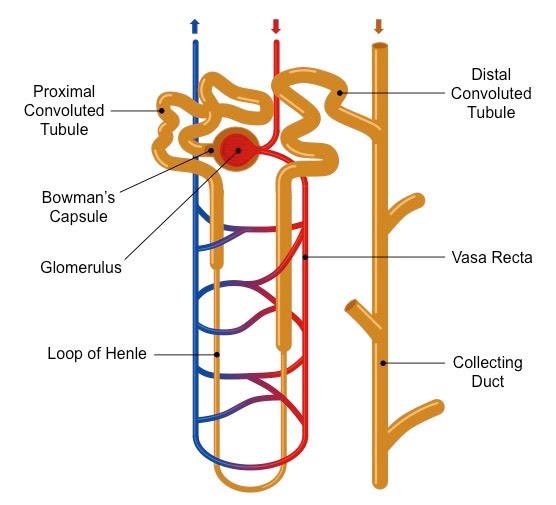
The Nephron
- The functional unit of the kidney
- Each kidney contains about 1 million nephrons.
- Has a rich blood supply.
- Most blood is carried to the glomerulus.
- The knot of Capillaries (glomerulus) sits in the Bowman’s Capsule.
- Fluid is forced out of the capillaries.
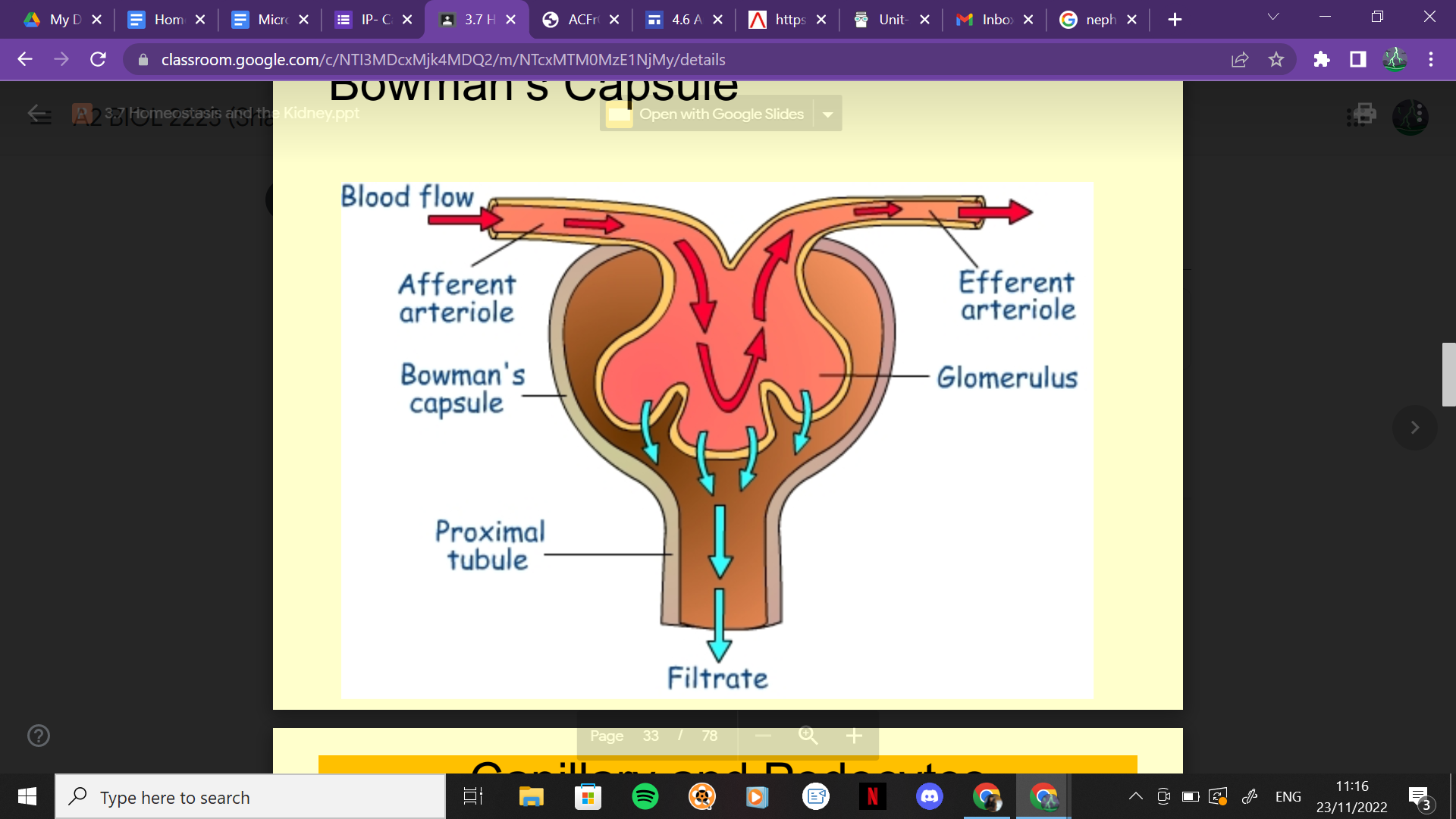
Ultrafiltration- High blood pressure in the capillaries of the glomerulus forces out the plasma of the blood. All molecules apart from blood cells and large proteins are squeezed out.
3 Layers of the Bowman’s Capsule
- Forestations- Gaps between the cells form the glomerular blood vessels creating a path of flow resistance away from the glomerulus.
- Basement Membrane- Filtration barrier, cells and large plasma protein macromolecules cannot pass through.
- Podocytes- form the inner membrane of the Bowman's capsule. The podocytes create gaps for the filtrate to pass between the cells.
Pressure forming filtrate
Pressure forming glomerular filtrate= hydrostatic pressure-osmotic pressure- Intrarenal pressure.
Selective Reabsorption
Selective reabsorption happened in the Proximal convoluted tubule.
It reabsorbs essential substances needed by the body.
All Glucose and amino acids are reabsorbed by Co-Transport with Sodium Ions into the cuboidal epithelial cells by facilitated diffusion. They are then actively transported into the blood capillary.
The Kidneys have a Glucose Threshold. If the concentration of glucose is too high, there are insufficient molecules to transport and reabsorb all of the glucose into the blood, so some are lost in the urine.
- Water is reabsorbed by osmosis.
- 50% of URea and small proteins are reabsorbed.
- At the base of the PCT, the filtrate is isotonic with the blood.
Isotonic- Same water potential.
24/11/2022
The Loop of Henle
- Loop of Henle sits in the Medulla
- The filtrate flows down the descending limb and flows up the ascending limb.
- As the filtrate flows down, water moves out by osmosis into the tissue fluid of the medulla and then into the blood capillaries.
- As this happens, NaCl moves into the descending limb and the concentration of ions increases.
- At the bottom of the loop, the filtrate is at its lowest water potential.
- As it ascends, NaCl moves out of the ascending limb and into the descending limb.
- This has a Counter-Current system, there is always a concentration gradient.
- The walls of the Ascending limb are impermeable to water, so only ions can move out.
- The filtrate enters the collecting duct and the presence of ADH tells the kidney how much water to conserve.
- The filtrate is at its most concentrated at the end of the collecting duct and forms urine.
Salt Regulation
- The aldosterone hormone increases the kidney's salt retention.
- The adrenal glands release aldosterone in response to low sodium concentration in the blood plasma or low blood pressure.
- Some H20 reabsorption always follows Na+ reabsorption.
Anti-Diuretic Hormone (ADH)
- ADH is for Osmoregulation
- Controls the water balance of the blood, tissue fluid and cytoplasm of cells.
- Under the control of Osmoreceptors in the hypothalamus.
- Hypothalamus controls thirst and the endocrine secretion of ADH.
- ADH is released from the pituitary gland and causes the opening of cell membrane pores called aquaporins, allowing water reabsorption into the blood.
- ADH regulates water reabsorption in the Distal Convoluted Tubule.
- Posterior Pituitary gland in response to signals from the hypothalamus which senses the osmotic pressure.
- ADH increases the permeability of the DCT and collecting duct to allow more water to be reabsorbed from the medulla and urine is more concentrated.
ADH mechanism
- ADH binds to receptors in the DCT.
- Cyclic AMP is produced.
- Vesicles containing aquaporins move and fuse with the cell membrane.
- Water passes through the aquaporins in the membrane down a gradient.
Adaptations of the LOH
- The relative length of the loop of Henle is adapted to the typical availability of water in the environment.
- Humans - Short LOH
- Beavers- Very short LOH
- Kangaroo Rats- Long LOH
Kidney failure & Treatments
Causes: Diabetes, High Blood Pressure, autoimmune disease, injury.
Treatments: Balance fluids in the blood, Medication to control K+ and Ca+, Low protein diet, Drugs to reduce blood pressure, Dialysis & Kidney Transplant.
Haemodialysis
- Tube is attached to arm
- Blood passes along the tube and into an external filtering machine.
- Happens 3 or more times a week.
- Requires a hospital visit.
- Uses an external machine.
- Heparin is put into the blood to thin and reduce clotting.
- Machine maintains a temperature of 40℃, to resemble body temperature, allow diffusion and ensure blood doesn't cool.
- Takes several hours.
- Blood flows in a counter-current system to maintain a concentration gradient and allow all the urea to diffuse out of the blood.
Peritoneal Dialysis
- Uses the inside of the abdomen as the filter due to the vast amount of blood vessels that act like a filter.
- An incision is made into the belly and a catheter is inserted into the peritoneal cavity.
- Fluid is pumped into the peritoneal cavity through the catheter, blood passes through and waste products and excess fluid are drawn into the dialysis fluid and drained into a bag.
- Happens 3-4x a day, and takes around 30-40 minutes.
- Can be carried out at home.
- Fewer dietary restrictions.
- Inside the abdomen, able to work and move around whilst the dialysis is taking place.