Hospital Theory
The History of Hospitals
The concept of hospital began in Indian and Egyptian cultures
Early hospitals were only for the insane, incurable and contagious
The military was the major face for the recent development of hospitals with need to look after the wounded
Now we have the Canadian Health Act which was enacted in Parliament in 1984
Health Care in Canada
Predominantly publicly financed
Medicare is also known as the Health Care Act founded by Tommy Douglas
Management and delivery is the responsibility of the individual province/territory
Federal Government gives the provinces money and they decide how to allocate it
Federal setting and administering of national principles
Principles of Medicare
Public Administration: nonprofit accountable to the provincial government ex. Hospitals
Comprehensiveness: all medically necessary services are offers by nurses and physicians
Universality: 100% of the population is insured (eligible residents)
Accessibility: reasonable access to hospitals and physicians without barriers; providing care regardless of where you live
Portability: ability to move to another province in Canada
Funding
Primarily taxation (money taken out of paychecks)
Provincial and federal (sales taxes,)
Sales taxes, payroll levels, lottery proceeds
Pharmacoeconomics
Relatively new
Pharmacoeconomics: analytical methods are used to identify, measure and compare costs and consequences of pharmacy products and services
Refers to the scientific discipline that can play compares the value of one pharmaceutical drug therapy to another drug therapy
Help make decisions on
Formulary inclusions
Drug-use policies
Clinical practice guidelines
Reimbursement and individual patient therapies
Used to compare cost and consequences of two or more competing products services and programs
Look at value for the money
Comparative effectiveness
Cost effectiveness
Value for money
Managed Care: Is quality care that uses only the most cost effective treatment and encourages preventative health strategies
Managed Care
Is quality care that uses only the most cost-effective treatments and encourages preventative health strategies
Health Care in Canada
cost escalated and the health of Canadians has not dramatically increased accordingly
cash starved provinces examining privatizations of services or user fees
not covering some services
Canadian Institution for Health Information (CIHI)
non-profit
collect and disseminate health information
data shows 331 billion of healthcare in 2022 (8,563 per Canadian)
Slowdown in economy and increase in healthcare spending
spending of drugs is 2nd largest portion of 26.1 billion in 2011 (84% Rx)
payment to physicians is 3rd (26.6 billion)
Factors' Affecting Spending
Geographic distribution
models of care
salary
benefits levels
age structure of provinces population
Suggested Overhaul of Medicare by Commissions Report
5 key areas
rural and remote access fund
diagnostic services fund
primary health care transfer
home care transfer
catastrophic drug transfer
Quebec Ruling
lengthy wait times unacceptable
currently prohibited people from buying insurance for services by health plan
court ruled it is unconstitutional ban private insurance where public system fails
Local Health Integration Networks
Transferer power to provinces
cannot run from one head office
Designed to plan, integrate and fund local health services including
Hospitals
Community Care Centers
Home Care
Longer- term care
Mental health services
Health Systems should be
safe
effective
patient centered
accessible
efficient
equitable
integrated
appropriately resourced
focuses on Population Health
What Can We Do as Consumers to reduce cost medication spending"?
newer drug not always better
entire quantity of Rx medication need to be taken
directions need to be clear
physician or pharmacist provide info on drug
fill all medications at same pharmacy
Inventory Management
Inventory
up to 70% of a hospital pharmacy budgets is spend on pharmaceuticals
inventory budget includes IV solutions, sets, pumps, and other medical supplies
buyer manages inventory
works under the supervision of the pharmacist
Bidding and Purchasing Contracts
confidential process by which the pharmacy “locks in” medication costs from a prime wholesale vendor for one year
Pharmacy also bids with manufacturers of drugs and IV solutions. with longer contracts (5 years)
Buyer makes an accurate estimation of formulary medication use for the next calendar year
Ordering the Pharmaceuticals
Ordered from wholesaler such as McKesson Provider Technologies or Cardinal Health
IV solutions ordered from a medical device company such as Baxter or Hospira
Procedures for ordering non-formulary drugs and borrowing from other facilities vary from hospital to hospital
Receiving and Storage
Inventory control technician orders medications, all technicians assist in receiving and restocking orders
check order against invoice upon receipt
discrepancies must be resolved
Check for damaged goods
check for items not received due to drug shortages
pharmaceutical should be placed on inventory shelves or in the refrigerator
storage guidelines available in package inserts or some reference texts
Special Handling of certain pharmaceuticals
Narcotics
Controlled Substance ordering system
must be kept in a locked cabinet
physical inventory required every two years
destructions must be witnessed and documented
Investigational Drugs
separate, secure storage area
supplied directly from the manufacturer
not usually labeled with name and strength
packaging labeled with the lot number and expiration date
Performing Ongoing Inventory Responsibilities
Rotating Inventory
place drugs so that the products expiring first are used first
document the inspection of expired drugs
Checking for drug recalls
recall notice from the wholesaler/manufacturer will list the drug and lot number to be recalled
technician pulls drugs from the shelves, unit dose carts, crash carts, automated dispensing cabinets
technicians completes and signs a return from to the wholesaler to receive credit from wholesaler
copy the form kept in the pharmacy
Other Institutional Pharmacy Practice Settings
Specialized pharmacies provide residents of long-term care facilities (LCTFs) with unit doses medications, IV medications
Health Maintenance Organizations may have in-house pharmacies that serve their hospital facilities and clinics
Home infusions pharmacies supply sterile preparations such as TPNs to patient who are not living in institutions
A Dose of Medical Ethics
Top 10 Dilemmas
Conflict pitting doctors against pat/fam
Setting priorities related to medical waiting
Access to needed health-care resources
Shortage of family physicians Medical errors
Palliative treatment
Achieving informed consent
Issues related to research
Substitute decision-making Surgical innovations
…
Organisation and function
diagnosis and testing
treatment and therapy
patient processing
public health and wellness
preventative health initiatives
training health care professionals
CONDUCTING RESEARCH
Hospitals are classified according to certain characteristics
bed capacity
targeted patent population
type of service
affiliation
ownership
urban versal rural
financial status
Common Hospital Departments and their Acronyms
Ambulatory Patient Care (APC)
Emergency Room/Department (ER/ED)
Intensive Care Unit (ICU)
Labor and Delivery (L&D)
Neonatal Intensive Care Unit (NICU)
Operating Room (OR)
Transitional Care Unit (TCU)
Pharmacy and Therapeutics Committee (P&T)
Reviews, approves, and revises the hospital’s drug formulary
maintains hospital drug use policies
reviews studies on appropriate use of drugs within hospital
reviews investigational drugs for hospital use
monitors medication error reports
part of maintaining accreditation from the Joint Commission
Representatives form medical staff, hospital and nursing administration
director of pharmacy: records and disseminates meeting minutes
drug-information pharmacist: researches and makes objective drug formulary recommendations
Pharmacy Technician: collects data and performs audits for the drug-information pharmacist
Drug Formulary
List of drugs approved for use in the hospital
Provides most effective medications while limiting costs
To add a medication to formulary, physician submits a medication application form
Drug-information pharmacist reviews literature and compares cost, advantage, and disadvantage to existing formulary drug
Approval sometimes restricted to a specific medical service
If physician writes for nonformula drug, may need to justify use to P&T committee
Medication Error Reports
drug information pharmacist collects and analyzes reports from pharmacy, nursing, and medicine
Adverse drug events tabulated
identify and correct the system’s problem to prevent recurrence
required to maintain hospitals accreditation
Institutional Review Board
Reviews the use of investigational drugs or procedures in the hospital
investigational drug: used in clinical trials; not approved by the FDA
Representative from medicine, pharmacy, nursing, and hospital administration, and the public
Clinical research investigational study
requires IRB approval before it can begin
investigator submits application and informed consent
informed consent: document written in understandable language about the study for patient participants
IRB protects patients by ensuring adequate knowledge of study risks and confidential of medical information
IRB collects information on adverse reactions to investigational medications, evaluates whether studies with severe adverse reaction should continue
The Hospital Pharmacy Department
Services
administration (formulary, budget, inventory)
distribution (filling, delivering, medications)
clinical (consulting with prescribers, patients)
Educational ( training pharmacies, patients, public, other personnel)
Specialty services may include: satellite pharmacies located at patient care units, clinical pharmacists making rounds with physicians, drug information center
Location and Structure
designated areas such as unit dose cart fill, repackaging, narcotic and investigational drug storage, preparation of sterile products
typically staffed 24 hours a day 7 days a week
Director of Pharmacy responsibilities
pharmacist-in-charge oversees the day-to-day operations
determines the level and scope of pharmacy services
plans and monitors the budget
makes staffing decisions
develops the Policy and Procedure Manual

Specializing Pharmacists
clinical pharmacists go on rounds with doctors, nurses
in larger hospitals, specialist pharmacists are found in different departments including the emergency department, the neonatal Intensive Care Unit
Specialties include compounding, chemotherapy, or IV medications
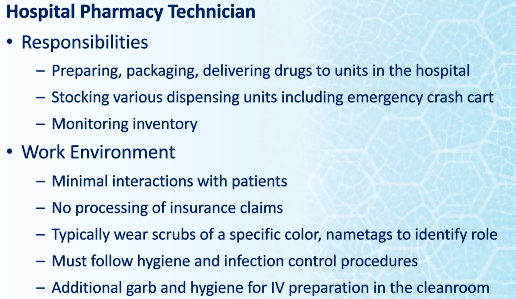
Technician Training and Orientation
require additional training on the job and regular retraining
train to perform all major department functions
most do not rotate through the cleanroom or hazardous compounding without specialized training
Technician Advancement and Specializations
medication reconciliation
sterile compounding
inventory management
training other staff
TCT Programs, technicians check each other’s work, adding an additional layer of medication safety
Types of Hospital and Institutional Pharmacy and Dispensing/ Returns
Long-Term care facilities
Provides rehabilitative services
restorative
ongoing skilled nursing care to individuals
Hospices
Provide palliative care and support services to individual at the end of their lives
also serves patients families
Open 24/7
Inpatients home and facilities
Provides pharmaceutical, physical, social, spiritual, and emotional care during last stages of life and bereavement period
Nursing Homes
Offer skilled and custodial care to older people who do not need the intensive acute care of a hospital
Wide range of medical conditions
Known as
Health Centers
Havens
Manors
Nursing Centers
Can range from 25-500 residents
Correctional Facilities
Prisons
Individual are physically confined and deprived of personal freedom
part of the criminal justice system
oversee the provision of pharmaceutical service to those confined to the facility
Hospital Pharmacies
Most prevalent type of health-system pharmacy
began as a charitable institution for the needy, aged, infirm or very young
Now where sick or injured people receive many levels of medical or surgical care
range from outpatient services to long-term care and intensive care
Types of Pharmacies
Centralized: is operated out of one primary location, the inpatient
all patient operations in one location
medications delivered through in one location
Decentralized (satellite): can consist of a central with multiple satellite pharmacies and outpatient pharmacy; typically specialized such as coagulation therapy
disadvantage is duplication of staff. inventory, and equipment
Medium and large facilities usually have to use this system
Inpatient Pharmacy
responsible for
Medication packaging
Centralized inventory
Sterile product preparation
Preparation and delivery of medication carts
Service to patients admitted to a facility
Outpatient: available to patients being discharged from the hospital
or being treated by physician but do not require overnight admission
retail-style pharmacy in hospital facility
CIVA Centers (sterile prep): responsible from processing and dispensing medication orders for individual patients
generally provide initial doses and emergency medications after which medications may be dispensed from floor stock
number and scope of practice varies by facilities
some for specific patient care areas
some have satellites based on location and access not by scope of service
Health-Systems Pharmacies Returns
returns are permitted if unused, unopened products
not permitted everywhere
safe
no waste
cost-effective
New Brunswick Prescription Drug Program
NBPDP
NB Electronic Health records
one patient, one record
web enabled application that will 24/7 Rx history access
Role of Hospitals
They are vital part of Canadian healthcare system
They provide
Emergency Services
Medical or surgical treatments
rehabilitation services
ongoing medical care
Patient Care
diagnostic and testing
treatment and therapy
Patient processing
teaching
research
public health promotion
GOALS OF PHARMACY
Promote the rational use of medications
Establish the value of pharmacy services
to enhance the health of patients
About Horizon Health Network
A billion dollar organization
responsible for 14,000 staff including 1,00 physicians and 4,600 volunteers
Operates 12 hospitals and more than 100 facilities, community health centers and clinics, addiction services, mental health services, public health, and extra mural program
20 foundations and 19 auxiliary and Alumnae supporting our organization
Horizon provides major critical and trauma services and is responsible for unique programs such as:
Heart Center
Prenatal
Trauma
Rehabilitation
Vitalite Health Network
$660 million
1,197 beds
399,322 patients
21,232 surgery’s
245,180 Emerge visits
2,029 births
186,561 Extra Mural Program
Classification System of Hospital
teaching hospital
types of care provided
accreditation
length of stay: less time more patient treated
less time more prescriptions
less admission, longer waits for surgery
fewer services for tax dollar
Home Care: if downsizing is to work. must be services waiting for people who are discharges patients
Long-term care
65 licensed nursing homes in NB
NBANH.com
not enough
fill many hospital bed waiting for home
Ownership
most owned by public
some private in Canada
Some operated by religious orders
Collaborative Practice
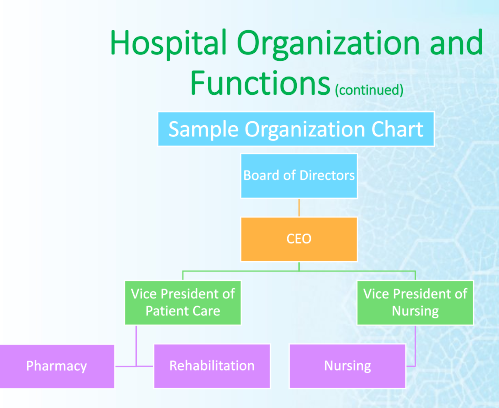
Organizational Chart
Technicians are intricate part of organizational structure
Mission Statement of Pharmacy
Accountability to hospitals and Patients
Commitment to providing good working environment for its staff
Ultimate goal is safe use of drugs by the public
Pharmaceutical Care
A relationship between a patient and a pharmacist in which the pharmacist accepts responsibility for drug use control functions and provides those services governed by awareness of, and commitment to, the patient’s interests’
Pharmacist, patient, and physical make a therapeutic plan
provide “definite outcomes which improve a patient’s quality of life”
Provide pharmacist follow-up
call patient at home
ask patient to call at specific dates
return to pharmacy
routine discussion with physician
Document follow-up activities
Role of technician in Pharmaceutical Care
helping pharmacists
order-entry
“first dose” fills
Prepare and check all IV and chemo
Note missed Doses
Self-medication reporting and filling
Other functions of the pharmacy department
drug procurement
safe preparation and distribution 5 rights
drug information
monitoring of appropriate drug use
monitoring ADR’s
Development of formulary
monitoring of drug expenditures
patient medication profiles
pharmacotherapy
investigational/ special release drugs
Pharmacy’s responsibility to administration
Annual reports must be submitted to inform admin of activities and achievements
Financial reports
staffing
supplies
workload monitoring
medication incident/errors
activity reports
critical indicators
measure taken for quality insurance
detection of major deviations
accreditations
Drug related Problem’’
Any physical or psychological signs or symptoms which is undesirable to the patient and which is in some way related to drug therapy
Eight General Ways drugs can cause problems in patients
taking drugs for no medically valid reason
need drug and one has not been suggested or prescribed
taking the wrong drug
taking too little of the drug
taking too much of the drug
needs a drug, has been prescribed, but not taking or taking inappropriately
experiencing adverse effects
experiencing drug reaction
Health Care Team
Medical Staff
MD or nurse practitioner
Therapy and other personnel
RT, PT, OT
Nursing Personnel
RN, LPN, Health Care Aid
Pharmacy Personnel
Pharm D, R.Ph, Technician, clerks
Formulary Medications
Formulary Drugs: Narcotics
Ordering by pharmacist or approved technician
May or may not be patient specific
Security: locked vault or acudose with a locked pocket (two people)
Physician's orders- signed within 24 hours
Prepackaging
Narcotics stored and dispensed from separate Narcotic room in pharmacy
Perpetual Inventory done regularly
Narcotics
Many institutional pharmacies require pharmacy technicians to carry out all aspects of pharmaceutical controlled substance-related duties:
Ordering Paling
Counting
Record keeping
Ming
Delivering
providing quality assurance
Placing the stock in s secure
Perpetual Inventory
Computer keeps track of medications going in and out
Some facilities manually record all withdrawals and additions in perpetual log books. The technician is often responsible for the record keeping (recording all controlled substance withdrawals and additions. perpetual log books,)
The perpetual log book is an official, legal record of all activity relating to medications stored in the narcotic cabinet/room.
The perpetual log book contains pages entitled Perpetual Inventory Record forms or Controlled Substance Record forms.
Make all entries or additions into the perpetual log in black pen.
Record withdrawals and negative balances in red pen.
Note errors by drawing a single line through the entire line entry. The initials of the person making the correction should be written next to the strikethrough and circled.
Errors in the narcotic records must remain traceable and legible. Never cross or scribble out errors; note that it is never acceptable to use white-out or similar products.
Always record information in the perpetual log on the next available line. There should never be an open or empty line in the perpetual log
Never write information on the bottom of a perpetual log sheet below the preprinted spaces. Once you have filled the last available line on the page, you want start a new sheet.
To start a new sheet, transfer the drug name, strength, dosage form, manufacturer, and DIN number from the drug bottle onto the appropriate space at the top of the new sheet. Transfer the balance or actual count number into the first available balance space on this new sheet.
Formulary Drugs: IPOs
Individual prescription orders
Patient name appears on package
For 1-30+ days (most hospitals run on 24 hour patient supply)
May be packaged as unit dose, various quantities in prescription vials, baggies, or blister packs.
Formulary Drugs: Night Cabinet
General stock available in an area outside the pharmacy for access by approved nursing staff when the pharmacy is closed
Not patient specific
Usually a blinded system or automated dispensing cabinet
Procedure
When the pharmacy is closed there is a procedure to be followed to access the meds in the night cabinet.
A copy of the physician’s order to be verified by pharmacist (or if CPOE it will be in the system to verify next morning)
A record log is kept of all issues, indicating the patient, nursing unit, drug & strength, number of pre packaged units obtained.
A pharmacist is always on call after hours. Some drugs are monitored or restricted, therefore a pharmacist must give authorization.
Some hospitals the night cabinet is located in the SPD dept. which is open 24/7 and they are responsible for obtaining and delivering the med to the nursing unit.
Technicians Role- Night Cupboard
Replace all stock taken from the previous night.
Check the dating every month or week (items with shorter times, i.e. premixed IV bags) and replace any that will expire before the end of the month
Making sure the stock is appropriately rotated.
Sample Night Cabinet Report from Automated Cabinet
You will see here it tells you the medication that was taken and the amount you need to refill. You would pick the items needed in the stockroom and then go deliver and replenish the stock in the automated cabinet. Either by scanning the barcode or by typing in the drug name.
blank slide (15)
Some institutions store floor stock items in an automated dispensing machine (ADM).
Turnaround times can be long when pharmacies are busy.
The need to administer "STAT," "now," and initial doses quickly is the main reason for having floor stock.
Pharmacy technicians are responsible for timely and accurate filling and checking of floor stock items on the Floor Stock Request Form (FSRF).
Medications not included in Floor Stock
Critical care medications are commonly kept in a crash cart brought to the bedside for emergencies.
Medications requiring pharmacy compounding
Creams, ointments, special oral solutions, and IV solutions with additives that require compounding in the pharmacy are prepared as needed
Narcotics
These are kept in a separate, high-security area.
Access to narcotics is restricted to authorized personnel.
Special record keeping is required for their administration.
Sample Manual Method Floor Stock Request Form
In this example you have Par level or your possibly and min and max column. For the manual method this would involve going to the unit and counting what is on hand and then replenishing what is needed. Typically would have different days scheduled for each unit/floor. Some high volume areas may get checked 2 to 3 times per week. An emergency department would be a high volume area.
This is how the automated dispensing cabinet let's us know it needs replenishing
These reports will print in the pharmacy alerting the technician's that the medication needs replenishing and which unit it is. Also note it tells you the quantity needed.
Formulary Drugs: Emergency Box (specialty Carts)
OR (operating room) cart
ER (emergency room) cart
Crash (for codes) cart
All contain medications, pertinent to their area, in forms/packaging that is quick and easy to administer in critical situations
Meds are usually on a portable cart with drawers / shelves
Technicians responsibilities
Pediatric Crash Cart
Crash carts are kept on hand for treating respiratory or cardiac arrest and other potentially fatal emergency conditions.
Many large facilities keep a crash cart on each floor or nursing unit.
Contents of crash carts are tailored to the types of patients in the facility.
Due to differences in body size and physiology, the types and strengths of medications in adult facilities would be different from those used in pediatrics.
Most of the items in the crash cart will be for parenteral use, meaning any route of administration other than sublingual, enteral, or topical, such as intravenous or intramuscular.
Generally, adult crash carts are stocked with emergency medications such as epinephrine, atropine, and nitroprusside.
The cart may also contain standard IV base solutions, IV tubing, and a limited supply of syringes, needles, and other medications or supply items.
Facilities often use tamper-evident plastic locks, which can be easily opened in emergency situations.
When a hospital patient goes into cardiac or respiratory arrest, a code is called.
A code is a life-threatening situation when a patient is in cardiac or respiratory arrest.
code blue respiratory arrest
code red: fire
yellow missing persons
A code team responds and assumes treatment of the patient, unlocking the crash cart.
Except during code use, the crash cart must remain locked.
Once the code has ended, the crash cart is returned to the pharmacy to be refilled.
Define:
crash cart: also known as "crash tray.” "code cart," "tackle box" or other term that individual facilities may develop
parenteral: also known as "crash tray." "code cart," "tackle box" or other term that individual facilities may develop
code: a life-threatening situation when a patient is in cardiac or respiratory arrest
code team: a group of doctors and nurses trained in emergency medical care
par level: the amount of a certain medication normally kept in the crash cart
Alcohol and Spirits
Pharmacy responsible to order and dispense
Perpetual inventory
Document when used in compounds
Beer can be ordered to patients on physicians' orders, with appropriate records maintained in a perpetual inventory log book.
Formulary Drugs: Weekend Passes
Patient orders which are needed for a limited time period, outside the hospital
label must contain information required by law in NB community pharmacies (including auxiliary, safety caps and directions)
Patient specific
Patient Prescriptions
Most inefficient because of waste and inability of the pharmacy department to properly monitor it
After reviewing medication orders for a floor, the technician takes the medication is filled and checked and then taken to the floor
Orders can be for several days supply
Once opened cannot be returned to the pharmacy because it has left the closed system of the pharmacy
Not prepackaged or unit dose medication
Being dispensed in vials
Inventory Management
Inventory
Up to 70% of a hospital pharmacy budget is spent on pharmaceuticals
Inventory budget includes IV solutions, sets, pumps, and other medical supplies
Buyer managers inventory
Works under the supervision of the pharmacists
Bidding Pharmaceuticals and Purchasing Contracts
Confidential process by which the pharmacy locks in medication costs from a prime wholesale vendor for one year
pharmacy also bids manufacturers of drugs and IV solution, with longer contracts 5 years
Buyer makes an accurate estimate of formulary medication use for the next calendar year
give ordering card to buyer ordering box
Ordering the Pharmaceuticals
Ordered from wholesaler such as Mckesson Provider Technology or Cardinal Health
IV solutions ordered from a medical device company such as Baxter or Hospira
Procedures for ordering non formulary drugs and borrowing from other facilities vary from hospital to hospital
Receiving Storage
Inventory control technicians orders medications, all technicians assist in receiving and restocking orders
check order against invoice upon receipt
discrepancies must be resolved
Check for damaged goods
check for items not received due to drug shortages
pharmaceuticals should be placed on inventory shelves or in the refrigerator
storage guidelines available in package inserts or some reference texts
Special Handling of certain pharmaceuticals
Narcotics
must be kept in a locked cabinet
physical inventory required every two years
destruction must be witnessed and documented
INvestigational Drugs
Separate, secure storage area
supplied directly from the manufacturer
not usually labeled with the name and strength
package labeled with the lot number and expiration date
Performing Ongoing Inventory Responsibilities
Rotating Inventory
Place new drug In front and old drug in the back
document the inspection of expired drugs
Checking for drug recalls
recall notice form the wholesaler/ manufacturer will list the drug and lot number will be recalled
Technician pull drugs from the shelves, unit dose carts, crash carts, automated dispensing cabinets
technicians complete and signs a return form to the wholesaler to receive credit from wholesaler
copy of the form kept in the pharmacy
Electronic Hospital Records and Medication Orders
Electronic Health Records allow for easier communication about a patient within a health system
Immediate access to patient’s medical records
Improve documentation
Enhanced coordination of patient care
Intake Records
Upon admission to a hospital, patient interviews about his medication his history by admitting staff or nurse
some pharmacy technicians specialize to identify unknown medications brought from home (home meds)
Patients is given a wrist band
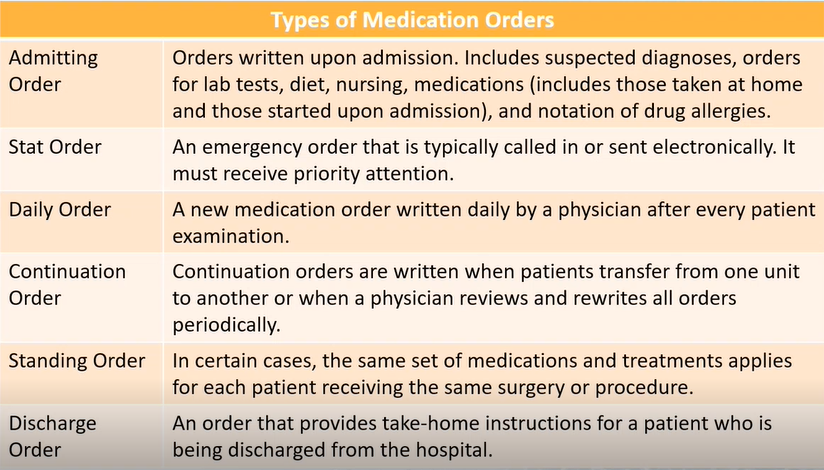
Medication Orders
Ordered by the prescriber for a patient
received electronically, by fax, pneumatic tube, phone, or hand delivery
written in the medical chart
entered by the hospital pharmacist
Computerized Prescriber Order entry
Prescriber directly enters into the electronic health record using a mobile device or laptop
a pharmacist checks and verifies the order
Advantages of CPOE
Efficient medication order completion
allows for prescriber entry off-site
simplifies inventory ordering and posting of patient hospital charger
improved medication safety
reduces transcription errors
includes safeguards that identify duplicate drugs, incorrect doses, and laboratory test results that may affect drug or dose
Handwritten Orders
Input by pharmacist into the pharmacy software
Verified for accuracy by the pharmacist if the pharmacy technician has entered the order
Electronic Medication Administration Record (eMAR)
all electronic record of the administration time of each drug
reduces medication error
increased nurse productivity
Benefits of eMAR
Enhances communication among healthcare team members
reduces medication errors
provides a way to meet documentation guidelines
All information collected using automation must be used in a way that protects patient privacy according to HIPAA
Formular Drugs: Weekend Pass
Patient Order which are needed for a limited time period, outside the hospital
label must contain information required by law in NB community pharmacies (aux. safety caps and directions
patient specific
cannot be taken out of the acudose
INvestigational Drugs
Not approved by the health protection branch for general use by the public
two types of investigation drugs
clinical
SAP drugs (special access program)
Emergency (covid vacc)
Written consent have to be signed by the patient
Technical Duties
Clinical Trials
released by health protection branch of health canada
released to a qualified investigator who is experienced and trained
why: to investigate the safety and the effectiveness of a drug to be evaluated. It is the final stage of human testing
It would be a current drug that is in use but a different form or indication of it
Emergency Status
How are these Drugs different from the Rx drugs
not available in canada but are approved by some health protection branch somewhere else
who gives permission to use these drugs
Health Canada
who can order these drugs
Doctors or Pharmacist a form has to be filled out why they want this drug then it has to be approved by health canada
these drug are not for general use
Released to a specific doctor, patient and use
Investigational Drugs Consent
required before administration of the drug
written consent by the patient or power of attorney
part of the permanent health record and a copy is given to the patient
INvestigational Drugs Records
investigation drugs must be stored separately from the other drugs in the pharmacy
pharmacy department is responsible for
separate storage and dispensing
records must be accurate, complete,and up to date
Specialty Carts
is a tray put on a cart
Emergency Box
OR cart
ER Cart
Crash Cart for all codes
All contain medications, pertinent to their area, in forms/ packaging that is quick and easy to administer in critical situations
technicians responsibilities
•Meds include seizures, anaphylactic reaction, respiratory and cardiac arrest meds
On all nursing units
Back-up in night cabinet
Immediately replaced when used extra in pharmacy when open in morning for immediate replacement
Secured with a one-time use padlock if broken must be rechecked and re-sealed
Typically uses pull tabs or sealed bags
Unit3-20 sample of order for potassium may need to get from night cabinet
Page 21 usage record
Page 22 chart of how nc gets replenished
Page 23-27 sample emergency box and list and chart of how replenishment is done
Inventory approved by P&T
Use prefilled syringes whenever possible for time
Inventory list in box indicates quantity, strength, packaging and name of drug in alphabetical order all injectables
Most often code is cardiac arrest
Most commonly used drugs are sodium bicarbonate, lidocaine, atropine and epinephrine
Must be in date sticker on outside with the earliest item to expiry
BPMH Medication Reconciliation
Medication Reconciliation
PROCESS INTENDED TO PREVENT MEDICATION ERRORS AT TRANSITION POINTS IN PATIENT CARE
Errors result of failure in communication about medications, especially at vulnerable transition points.
Transition points
Admission
Discharge
transfer between care settings
CREATING MOST COMPLETE AND ACCURATE LIST OF ALL MEDIATIONS A PATIENT IS CURRENTLY TAKING
USING THIS LIST WHEN WRITING MEDICATION ORDERS
COMPARING THE LIST AND THE MEDIATION ORDERS
PATIENT SAFETY INITIATIVE IN CANADA
50 % OF PATIENTS HAVE AT LEAST 1 UNINTENTIONAL MEDICATION DISCREPANCY IN HOSPITAL ADMISSION ORDERS
HIGH INCIDENT WHEN TRANSFERRED FROM INTENSIVE CARE TO A WARD SETTING
TRANSFER BETWEEN LONG-TERM CARE AND ACUTE CARE
DISCHARGE FROM HOSPITAL
Post-hospital medication discrepancies increase the risk of readmission within 30 days
Discrepancies that exist at admission but remain unresolved can create confusion
Medication reconciliation program can reduce time that physicians, nurses and pharmacists spend sorting out the medication problems at the transition of care
component of seamless care initiative in 1998
One of six targeted interventions in Safer Healthcare Now!
Unintentional Discrepancy
Ordered a grey thong instead of grey pants
Forgot to reorder your belt
Undocumented Intentional Discrepancy
Blue a better color for you so substituted in place of red shirt but nobody was told
Intentional Discrepancy
Everyone told you that you had the legs for a dress so we replaced your pants
Medrec Background
MEDICATION RECONCILIATION
IS A REQUIRED ORGANIZATIONAL PRACTICE (ROP) FOR ALL HOSPITALS IN CANADA
IS A VERY IMPORTANT PATIENT SAFETY INITIATIVE AND IMPACTS OUR PATIENTS THROUGHOUT THEIR HOSPITAL STAY, FROM ADMISSION TO DISCHARGE.
NEEDS TO BE A PRIORITY IN OUR QUALITY IMPROVEMENT PLANS FOR EACH NURSING UNIT
IT IS A FORMAL PROCESS COMPARING:
A PATIENT’S ACCURATE AND COMPREHENSIVE MEDICATION HISTORY (BPMH) AND
MEDICATIONS PRESCRIBED AT ADMISSION, TRANSFER AND DISCHARGE
Why is it important
TRANSITIONS FROM ONE HEALTHCARE SETTING TO ANOTHER CAN LEAD TO ERRORS IN PATIENT’S MEDICATION REGIMENS
THESE ERRORS CAN POTENTIALLY LEAD TO:
ADVERSE EVENTS
PROLONGED HOSPITAL STAYS
RE-ADMISSIONS BACK TO HOSPITAL
Transition of Care
TRANSITIONS OR TRANSFERS BETWEEN INTERFACES OF CARE CAN INCLUDE PATIENTS MOVING BETWEEN:
UNITS IN THE SAME HOSPITAL
ICU TO GENERAL WARD
ORHTOPEDICS TO CARDIOLOGY
ONE HEALTHCARE FACILITY TO ANOTHER
HOSPITAL TO HOSPITAL
HOSPITAL TO REHAB
ONE HEALTHCARE SECTOR TO ANOTHER
LONG TERM CARE TO HOSPITAL
HOSPITAL TO COMMUNITY
Why is there a Problem
A REVIEW OF PUBLISHED ARTICLES FOUND THAT 10-67% OF PATIENTS HAD AT LEAST ONE PRESCRIPTION MEDICATION HISTORY ERROR AT THE TIME OF HOSPITAL ADMISSION
WHEN NON-PRESCRIPTION MEDICATIONS WERE INCLUDED THE FREQUENCY OF ERRORS WAS 25-83%
What are the Discrepancies
EX: UNINTENTIONAL DISCREPANCIES
COMMON TYPES OF MEDICATION DISCREPANCIES:
**OMISSION:**
HOME MED NOT LISTED
HOME MED NOT ORDERED
DISCHARGE MED NOT INCLUDED IN INSTRUCTIONS
COMMISSION
DISCONTINUED MED IS LISTED OR ORDERED
THERAPEUTIC DUPLICATION DUE TO FORMULARY SUBSTITUTION
DOUBLE-DOSING VIA TWO ROUTES (IV AND PO)
DESCRIPTION
DOSE TIME MISSED
DOSE INAPPROPRIATE
EXTRA DOSE GIVEN
DIFFERENT FREQUENCY
Where is MEDREC Done
Hospitals within 24 hours
Ambulatory Visits
day surgery, various clinics
Community pharmacy
Long term care homes
home Care
Admission: The goal reconciliation of admission is to ensure medication there is a conscious decision on the part of the patient's prescriber to continue, discontinue or modify the medication regimen that a patient has been taking at home.
Compare BPMH vs. AMO (Admission medication orders)
identify and resolve discrepancies
Transfer: The goal of transfer medication the patient was receiving on the reconciliation is to consider not only what transferring unit but also any medications they were taking at home that may be appropriate to continue, restart, discontinue or modify.
Compare BPMH vs. MAR (Medication Administration Record
identify and resolve discrepancies
Discharge: The goal of discharge medication reconciliation is to reconcile the medications the patient is taking prior to admission and those initiated in hospital, with the medications they should be taking post-discharge to ensure all changes are intentional and that discrepancies are resolved prior to discharge.
Compare BPMH vs. MAR (Medication Administration Record + new medications started upon discharge
identify and resolve discrepancies
MEDREC MODELS
Proactive Model: Areas with planned admissions pre admission clinic (bomb done prior to physician writing orders. Used before surgery in pra admission clinics)
when bpmh is done before admission medication orders are written
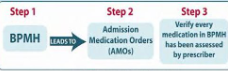
Retro active model: High volumes of admissions - considered inefficient as it creates more work as orders are already written before the BPMH is taken
When thw BPMH is done after the admission medication orders are written

Hybrid Model: bit of both
When both models coexist
happens when
short staffed
complex patients with extensive med histories
incomplete information availible to complete a BPMH prior to admission order
Ideally BPMH should be done within 24 hours of
admission
what is BPMH: A BEST POSSIBLE MEDICATION HISTORY IS A HISTORY CREATED USING:
A SYSTEMATIC PROCESS OF INTERVIEWING THE PATIENT OR THEIR CAREGIVER
**A REVIEW OF AT LEAST TWO RELIABLE SOURCES OF INFORMATION TO OBTAIN AND VERIFY ALL OF A PATIENT’S MEDICATION USE. BOTH PRESCRIBED AND OVER THE COUNTER MEDICATIONS (OTC)**
COMPLETE DOCUMENTATION OF ALL THE MEDICATIONS INCLUDING NAME, DOSE, ROUTE AND FREQUENCY
Why is it important to identify all patient home meds both otc and rx
MEDICATIONS SHOULD BE ASSESSED FOR ALL CONDITIONS
STOPPING SOME MEDICATIONS ABRUPTLY CAN CAUSE WITHDRAW L SYMPTOMS
IDENTIFY IF A MEDICATION IS THE CAUSE OF THE ILLNESS OR WORSENING OF SYMPTOMS
CONSIDER POTENTIAL DRUG INTERACTIONS
SOME MEDICATIONS CANNOT BE TAKEN BEFORE OR AFTER CERTAIN PROCEDURES OR SURGERIES
COMMUNICATE TO THE CIRCLE OF CARE A COMPLETE LIST OF ALL MEDICATIONS ON DISCHARGE FROM HOSPITAL
Where are BPMH’s Done
AT ADMISSION TO HOSPITAL:
IN EMERG
PRE-ADMISSION CLINICS
WITHIN UNITS OF THE HOSPITAL
LONG-TERM CARE UNIT
AMBULATORY CLINICS
HOME CARE
COMMUNITY PHARMACY (MED REVIEW)
AT POINTS OF TRANSFER, WHEN PATIENT MOVES FROM ONE CARE SETTING TO ANOTHER
Where are BPMH’s Documented
WHETHER IT IS PAPER-BASED OR ELECTRONIC FORMAT, THE BPMH SHOULD BE DOCUMENTED IN A HIGHLY VISIBLE DESIGNATED LOCATION FOR ALL HEALTHCARE PROFESSIONAL TO ACCESS
USUALLY IN THE PATIENTS CHART (ELECTRONIC OR PAPER)
When should BPMH’s be completed
ASAP
ideally within 24 hrs of admission
being done before the physician writes thea admission orders
why
to prevent med errors
Anyone can do a BPMH with the proper training
How to do a BPMH
MEDICATION INFORMATION FROM MULTIPLE SOURCES
6 MONTH MEDICATION HISTORY FROM PROVINCIAL DIS OR CALL COMMUNITY PHARMACY TO GET THEIR 6 MONTH MEDICATION HISTORY
MEDICATION VIALS
HOSPITAL DISCHARGE SUMMARY
NURSING HOME MAR
AND INTERVIEW PATIENT OR CAREGIVER
IDENTIFY AND RESOLVE DIFFERENCES BETWEEN THE SOURCES OF INFORMATION
TALK AND LISTEN TO PATIENT/FAMILY/CAREGIVER
ASK FOR A CURRENT MEDICATION LIST (THEY MAY HAVE ONE WITH THEM)
ASK OPEN ENDED QUESTIONS
ASK SPECIFICALLY ABOUT SPECIAL TYPES OF MEDICATIONS (PUFFERS, EYEDROPS, CREAMS, PATCHES, ETC.)
DEVELOP A “TEMPLATE”
CONSIDER ALTERNATE WAYS TO CONVEY THE SAME MESSAGE (EX. BRAND VS GENERIC NAMES)
CONSIDER CURRENT AND ACTUAL MEDICATION USE
TRY NOT TO USE MEDICAL LANGUAGE
CONSIDER THE UNIQUE SITUATION OF THE PATIENT (EX. LANGUAGE, BARRIERS, COGNITION LEVEL, ACUITY OF ILLNESS ETC.)
Interview
INTRODUCTION
ALLERGY INFORMATION
COMMUNITY PHARMACY INFORMATION
CURRENT AND ACTUAL MEDICATION USE
REGULAR MEDICATION USE (OTC’S)
AS NEEDED MEDICATION USE
**ALL MEDICATIONS: INHALERS, OTC’S, NASAL SPRAYS, VITAMINS, HERBALS, CREAMS, CLINICAL TRIALS, PHYSICIAN SAMPLES, ETC.**
Ask “How do you take your medication?”
sources of information
REVIEW WITH MULTIPLE SOURCES OF INFORMATION
PATIENT/FAMILY/CAREGIVER
MEDICATION VIALS
BLISTER PACKS
DIS HISTORY OR COMMUNITY PHARMACY HISTORY
PATIENT’S OWN MEDICATION LIST
DISCHARGE ORDERS FROM OTHER FACILITY
MAR – MEDICATION ADMINISTRATION RECORD
FAMILY DOCTOR
HOME CARE MEDICATION LIST
NOT ALL SOURCES OF INFORMATION ARE CREATED EQUALLY
START WITH THE MOST RECENT SOURCES OF INFORMATION
KNOW THE LIMITATIONS OF YOUR SOURCES
NO SOURCE OF INFORMATION WILL TELL YOU EVERYTHING THAT YOU WILL NEED TO KNOW; BE SURE TO INVOLVE AND INTERVIEW THE PATIENT AND ASK THE RIGHT QUESTIONS
Patient/Family
PATIENT’S RECALL OF INFORMATION HISTORY CAN BE DIMINISHED DURING ACUTE/STRESSFUL TIME
SOLUTION: VERIFY WHEN PATIENT IS NO LONGER IN DISTRESS; CONFIRM WITH A SECONDARY SOURCE
POOR PERCEPTION OF WHAT A MEDICATION IS
SOLUTION: EFFECTIVE PROMPTING OR PROBING QUESTIONS
PATIENT MAY NOT KNOW THE NAME OR NUMBER OF THEIR COMMUNITY PHARMACY
SOLUTION: DIS SYSTEM
MEDICATION USE VS HOW THE MEDICATION WAS PRESCRIBED
SOLUTION: FOCUS ON “MEDICATION USE”; SEEK CLARIFICATION (FROM OTHER COMMUNITY PHARMACIES, PRIMARY CARE PHYSICIANS, FAMILY MEMBERS, CAREGIVERS)
COMMUNICATION BARRIERS
LANGUAGE: NON-ENGLISH SPEAKING CLIENTS
PATIENT’S LEVEL OF CONSCIOUSNESS/COGNITIVE ABILITY
SOLUTION: FAMILY MEMBERS/CAREGIVERS, INTERPRETERS, OTHER SOURCES OF INFORMATION
Medication Vials
USE THE “SHOW AND TELL” METHOD
CHECK THE PATIENT’S NAME ON THE VIAL
CHECK THE DATE ON THE VIAL
OPEN THE VIALS AND MAKE SURE WHAT IS IN THE VIAL MATCHES THE LABEL
ASK THE PATIENT HOW THEY ARE TAKING THE MEDICATION AND COMPARE IT TO THE INSTRUCTIONS ON THE VIAL
“TELL ME HOW YOU TAKE/USE THESE”
Patients own medication list
CONFIRM THE DATE IT WAS LAST UPDATED
DETERMINE WHO WROTE THE LIST
CONFIRM IF THE DIRECTIONS WRITTEN ARE HOW THE MEDICATIONS WERE PRESCRIBED OR HOW THE PATIENT ACTUALLY TAKES THE MEDICATIONS
DETERMINE IF PATIENT IS TAKING ANYTHING ELSE (RX, PRNS, OTC, HERBALS, VITAMINS, ETC)
Blister PAcks
CHECK THE PATIENT’S NAME ON THE BLISTER PACK
CHECK THE DATE ON THE BLISTER PACK – DETERMINE IF ANY CHANGES HAVE BEEN MADE TO THE PATIENT’S MEDICATIONS SINCE THE BLISTER PACK HAS BEEN FILLED
DO NOT ASSUME PATIENT IS TAKING ALL OF THE MEDICATIONS IN THE BLISTER PACK
ASK ABOUT MEDICATIONS THAT CANNOT FIT INSIDE THE PACK, EX. PUFFERS, PATCHES, EYE/EAR DRO
PS, FRIDGE ITEMS, ETC.
ASK ABOUT PRN MEDICATIONS
Discharge medication list
CHECK THE DATE ON THE LIST
DETERMINE IF IT IS AN ACTUAL LIST OF ALL MEDICATIONS THE PATIENT IS TO BE TAKING OR IF IT IS ONLY A “PRESCRIPTION”
DISCHARGE PRESCRIPTIONS – MAY ONLY INCLUDE “NEW” OR “CHANGED” MEDS
THE ATTENDING PHYSICIAN MAY ASSUME THAT THE PATIENT SHOULD CONTINUE EVERYTHING THE PATIENT WAS TAKING PRIOR TO ADMISSION WITHOUT DOCUMENTING AT DISCHARGE
BE CAREGUL OF “AUTO-SUB” MEDICATIONS (DUPLICATIONS OF MEDS)
CONFIRM WITH THE PATIENT IF THEY ARE TAKING ANY OTHER MEDICATIONS
CONFIRM IF THEY ARE TAKING THE MEDICATIONS DIFFERENTLY THAN PRESCRIBED
CONFIRM IF ANY CHANGES HAVE OCCURRED SINCE DISCHARGE
CALL COMMUNITY PHARMACY TO CONFIRM IF ANY OTHER ADDITIONAL MEDICATIONS
MAR-Medication Administration Record
LOOK CAN VARY BETWEEN INSTITUTIONS
CHECK THE LAST DOSE ADMINISTERED
BE AWARE
HELD/HOLD MEDICATIONS
CHANGES IN DOSE
DISCONTINUED MEDICATIONS
family physician
IF NO OTHER SOURCE AVAILABLE – CALL FAMILY PHYSICIAN
LIST MAY BE OUT OF DATE DEPENDING ON LAST VISIT
LIST MAY NOT INCLUDE
PRESCRIPTION MEDICATIONS ORDERED BY OTHER PHYSICIANS (SPECIALISTS, DENTISTS, ETC.)
OTC’S, VITAMINS, HERBALS, ETC.
What if sources do not match
IDENTIFY THE DISCREPANCIES
ONLY ONE OF THEM IS ACTUALLY HAPPENING
CLARIFY WITH THE PATIENT DURING THE BPMH INTERVIEW WHAT IS BEING TAKEN
FIND OUT AS MUCH AS YOU CAN FROM THE SOURCES OF INFORMATION, CALL PHARMACY, START-STOP DATES – INVESTIGATE FURTHER.
DOCUMENT DISCREPANCIES
CLEARLY RELAY THE INFO TO THE PHARMACIST, WHO CAN THEN RELAY TO PRESCRIBER SO THAT AN INFORMED DECISION CAN BE MADE
Considerations
IF ACTUAL MEDICATION USE VS HOW THE MEDICATION WAS PRESCRIBED
NOTE ACTUAL MEDICATION USE ON THE BPMH
DOCUMENT OR RELAY THE DISCREPANCY(IES) TO THE PHARMACIST
CLINICAL DECISIONS WILL BE MADE BASED ON THE BPMH, WHICH CAN LEAD DIRECTLY TO MEDICATION ORDERS
Helpful Tips
Dose Concideations
ALWAYS CONFIRM/VERIFY MOST RECENT INSULIN DOSE AS IT CAN CHANGE FREQUENTLY
FOR PARTIAL TABLETS, THE EXACT DOSE NEEDS TO BE CLEAR
FOR PARTIAL TABLETS RECORD THE AMOUNT TAKEN (IN MG) PER DOSE
BEWARE OF ATYPICAL DOSING FOR CERTAIN MEDICATIONS SUCH AS WARFARIN, FENTANYL PATCHES, AND DEPOT – INJECTIONS, ETC
EX. WARFARIN 2 MG ON SUN/TUES/THURS/ SAT; AND WARFARIN 4 MG ON MON/WED/FRI
DOCUMENT WHICH DOSE THEY TOOK YESTERDAY OR THE DAY OF ADMISSION (IF POSSIBLE)
BEWARE OF MEDICATIONS THAT ARE IN MCG VS MG
FOR LIQUID SUSPENSIONS – RECORD THE CONCENTRATION OF THE LIQUID AND THE TOTAL NUMBER OF MG TAKEN
CERTAIN MEDICATIONS (E.G. SINEMET) HAVE TO BE DOSE/TAKEN AT EXACT TIMES – TAKE NOTE OF THE EXACT TIME(S) THAT THE PATIENT TAKES EACH DOSE
DO NOT USE DANGEROUS ABBREVIATIONS
PAY PARTICULAR ATTENTION TO “HIGH ALERT” MEDICATIONS (E.G., ANTICOAGULANTS, INSULINS, OPIOIDS, METHOTREXATE)
ENSURE THE PROPER FORMULATION OF THE MEDICATION IS DOCUMENTED, ESPECIALLY LONG ACTING VS. SHORT ACTING. (E.G., CR, XR, ER, LA)
BE AWARE OF COMBINATION PRODUCTS (E.G. DIOVAN-HCT, COVERSYL PLUS, VIMOVO, ETC.) – RECORD BOTH GENERIC MEDICATION NAMES AND DOSES – ADD BRAND NAME IF ITS GOING TO GIVE CLARITY BUT MUST HAVE THE GENERIC AS WELL
DON’T FORGET ABOUT INJECTABLES (COMMONLY MISSED DRUGS: VITAMIN B12 INJECTION, METHOTREXATE, PSYCHOTORPICS)
FOR BISPHOSPHONATES (E.G. ALENDRONATE, RISEDRONATE) DOCUMENT THE SPECIFIC DAY OF THE WEEK THEY ARE TAKEN
Scope of Practice
ALWAYS BE MINDFUL OF WORKING WITHIN YOUR SCOPE OF PRACTICE
UNDERSTAND WHEN TO REFER TO A PHARMACIST, NURSE OR PHYSICIAN:
IF A PATIENT ASKS QUESTIONS ABOUT:
WHY THEY ARE TAKING CERTAIN MEDICATIONS
DRUG INTERACTIONS
THERAPEUTIC/CLINICAL-RELATED QUESTIONS
THEIR HEALTH STATUS
WHAT THE PLAN IS FOR THEM WHILE THEY ARE IN HOSPITAL
Refer to a Pharmacist
IF A MEDICATION IS COMPLETELY UNFAMILIAR TO YOU AND YOU CAN’T FIND ANY INFORMATION ON IT
IF YOU CANNOT RESOLVE THE DIFFERENCES BETWEEN TWO DIFFERENT SOURCES OF THE PATIENT’S MEDICATION INFORMATION
OR AT ANY TIME WHEN YOU ARE UNSURE OF HOW TO HANDLE A PARTICULAR QUESTION OR SITUATION
 Knowt
Knowt
