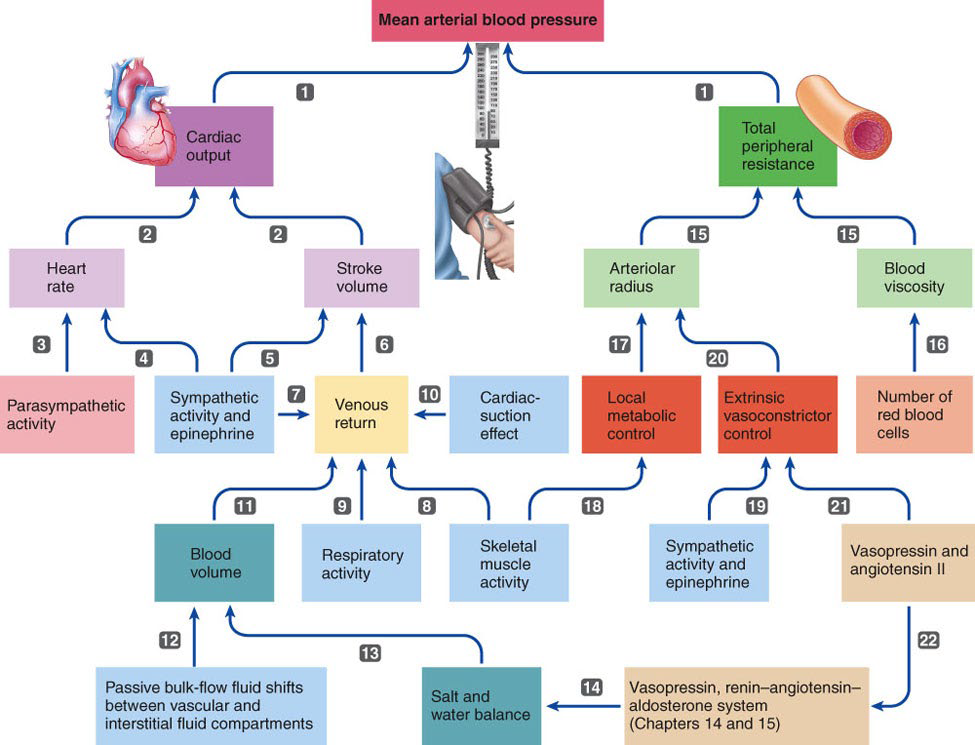
Cardiac Output, Blood Flow, and Blood Pressure Regulation
Cardiac Output (CO)
The volume of blood ejected by the ventricles per 1 minute~5L at rest
↑ with:
Sympathetic stimulation and exercise
Vigorous exercise ↑ CO to 21 L/min for fit person and up to 35 L/min for world class athlete
CO= HR X SV
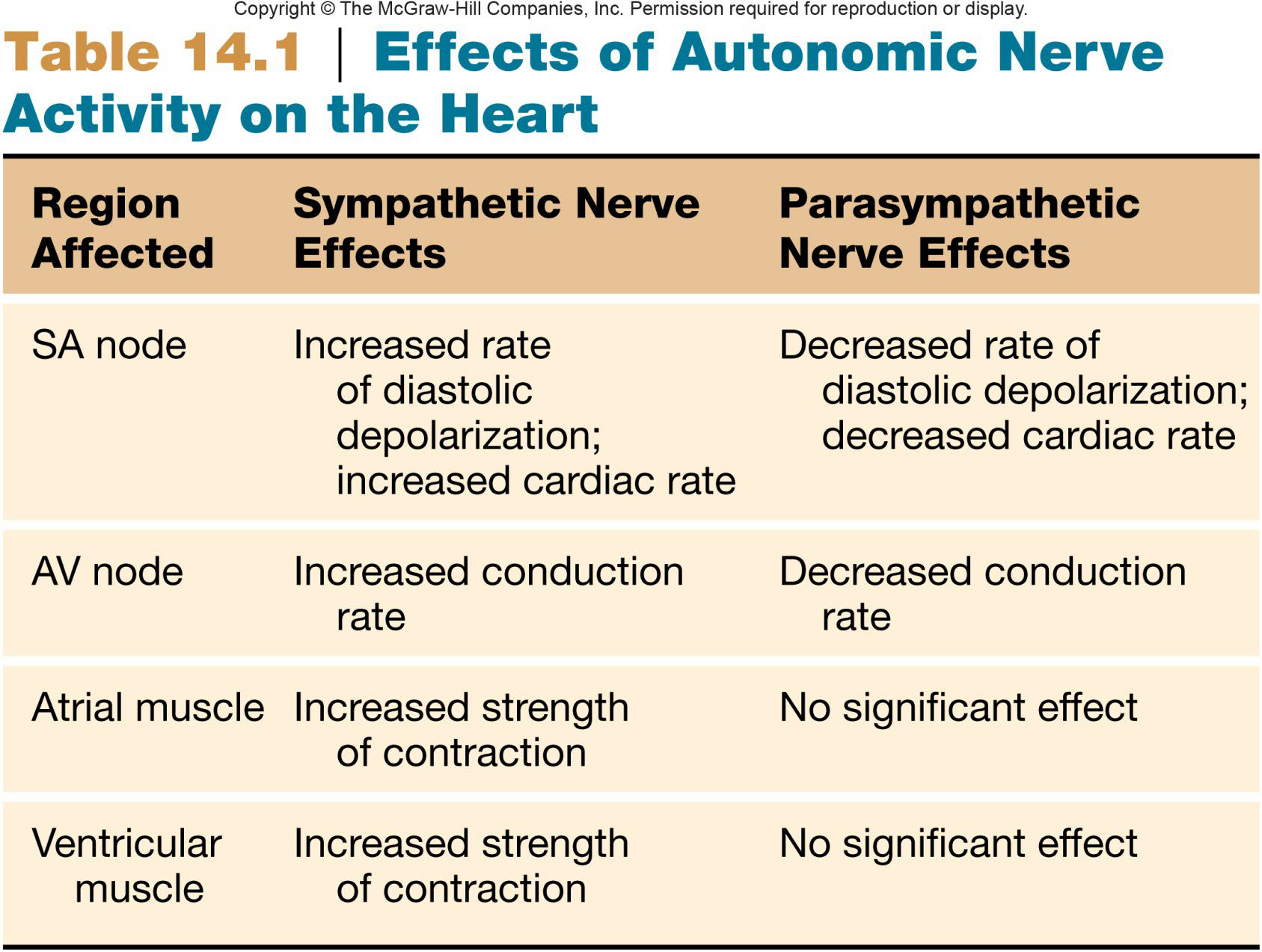
Heart Rate (HR)
Heart rate is the number of heart beats per minute (BPM)
Normal HR at rest:
Adult= 60-100 BPM (average ~70 BPM)
Athlete= 40-60 BPM
Infant= ~120 BPM
HR increase with:
increase metabolic demands
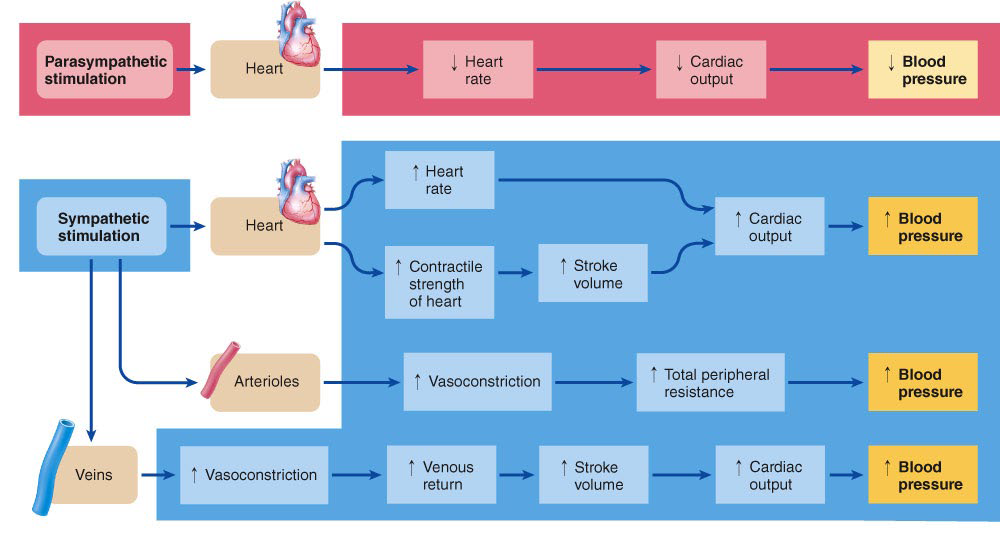
Sympathetic NS activity (NE and/or EPI)
HR decrease with:
Parasympathetic NS activity (Acetylcholine)
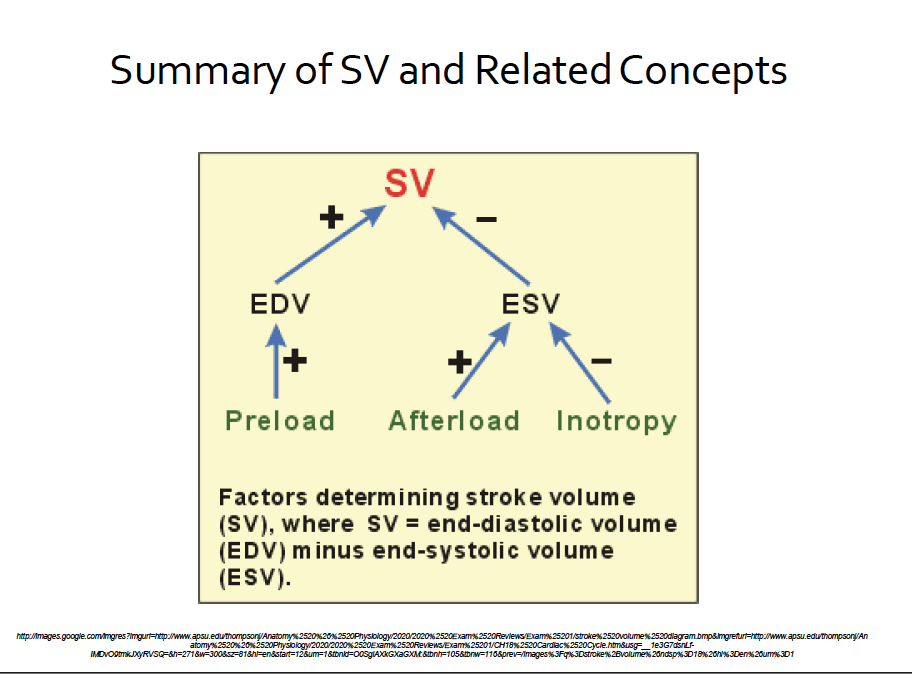
Stroke Volume (SV)
Volume of blood pumped by ventricle/beat (or per systole)
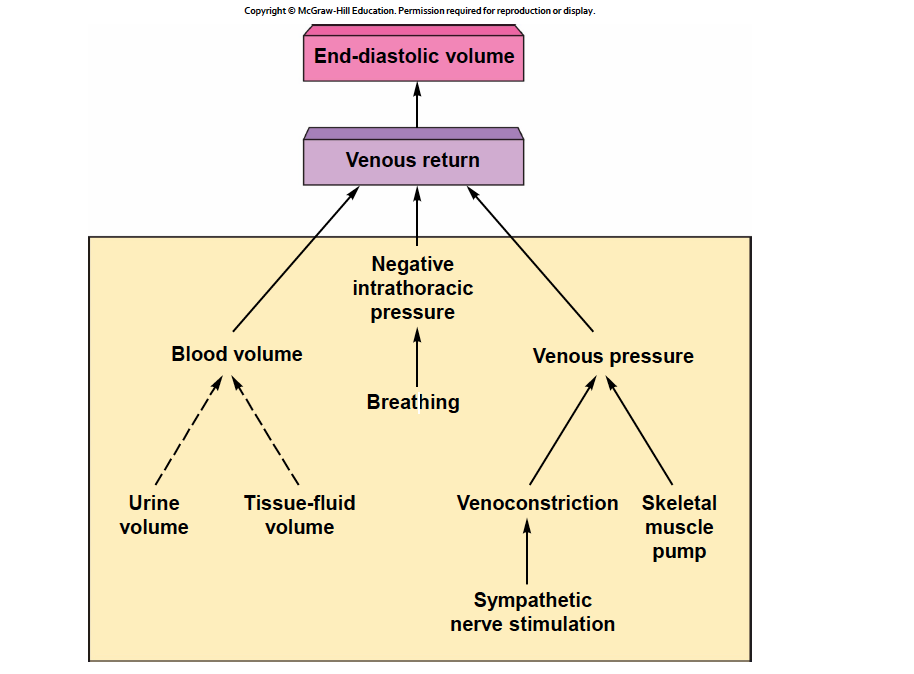
Determined by extent of venous return and by sympathetic activity
SV= EDV- ESV
EDV= end diastolic volume
ESV= end systolic volume
Frank-Starling Law of the Heart
Normal heart pumps during systole most of the blood it receives in diastole

Cardiac Reserve
The maximum percentage that the cardiac output can increase above the resting level.
Cardiac reserve= COmax- COrest
Factors Affecting Stroke Volume
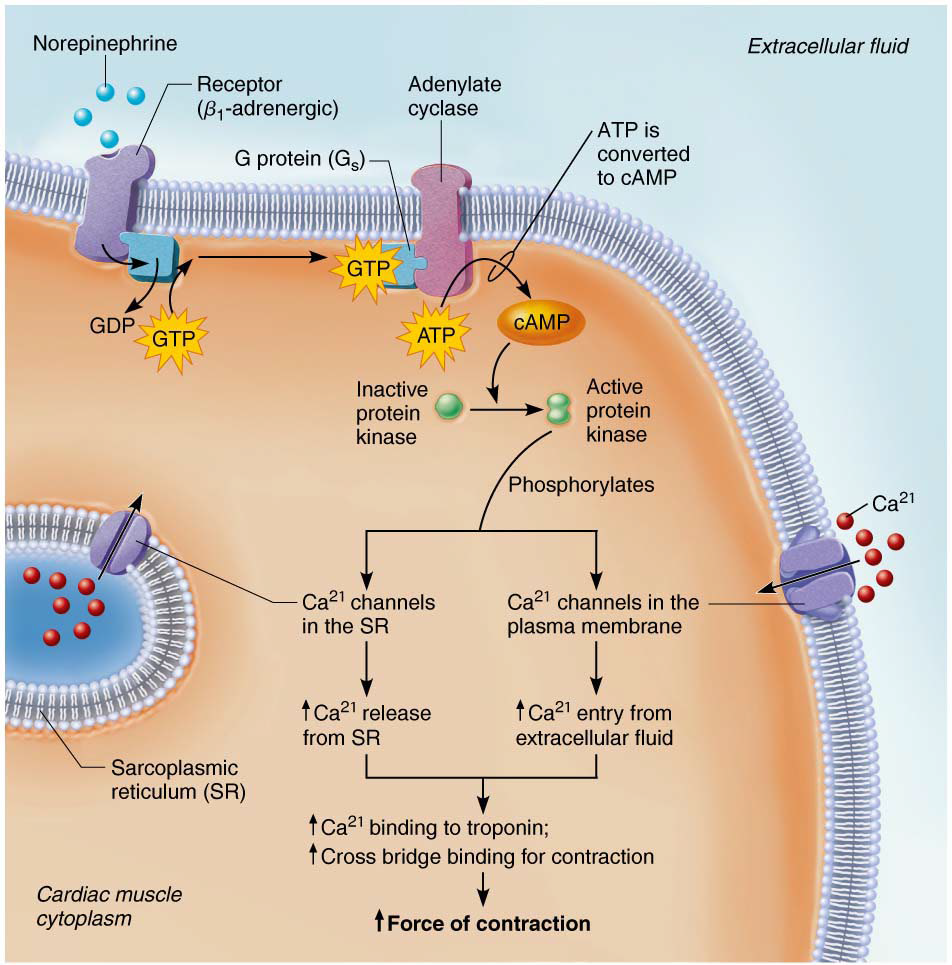
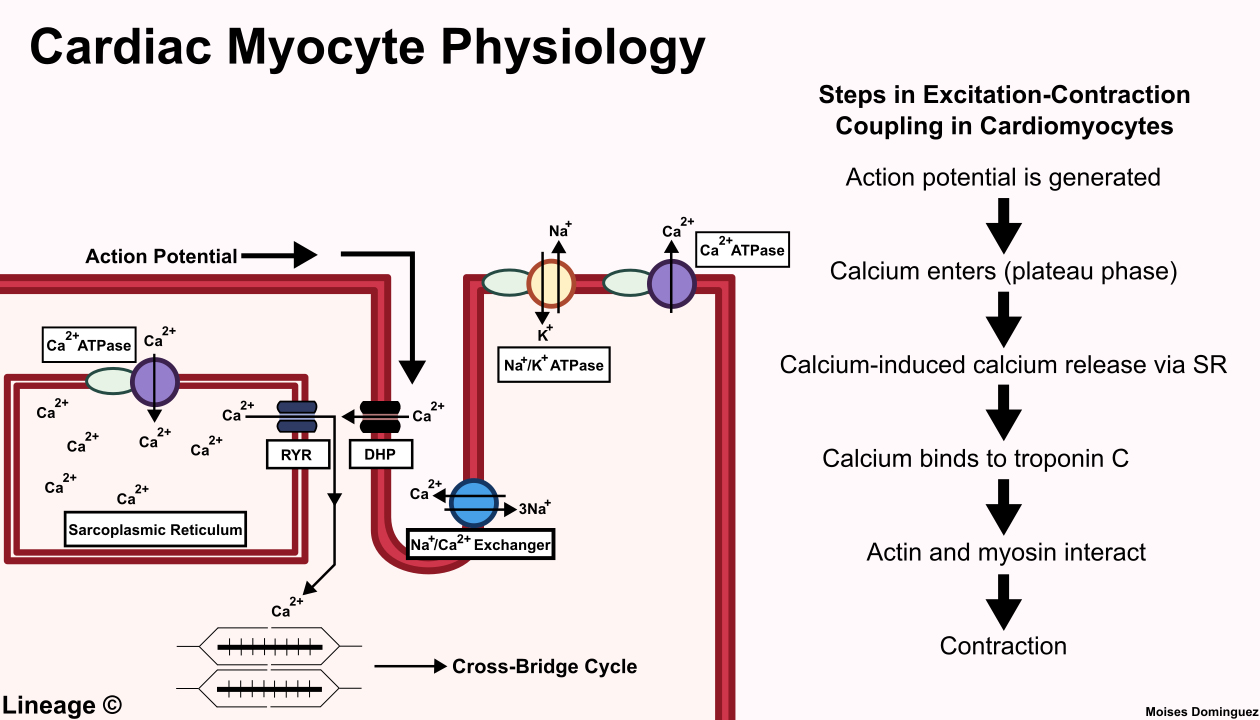
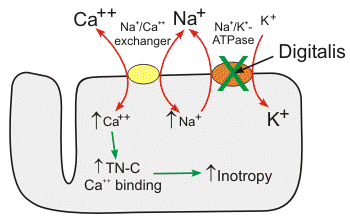
Inotropy= contractility
The ability of the heart muscle to generate force during myocardial ventricular contraction
Positive inotropic agents:↑contractility
Include: Hypercalcemia, Catecholamines, and sympathetic stimulation
Negative inotropic agents:↓contractility
Include:Hypocalcemia, Hyperkalemia, Parasympathetic stimulation
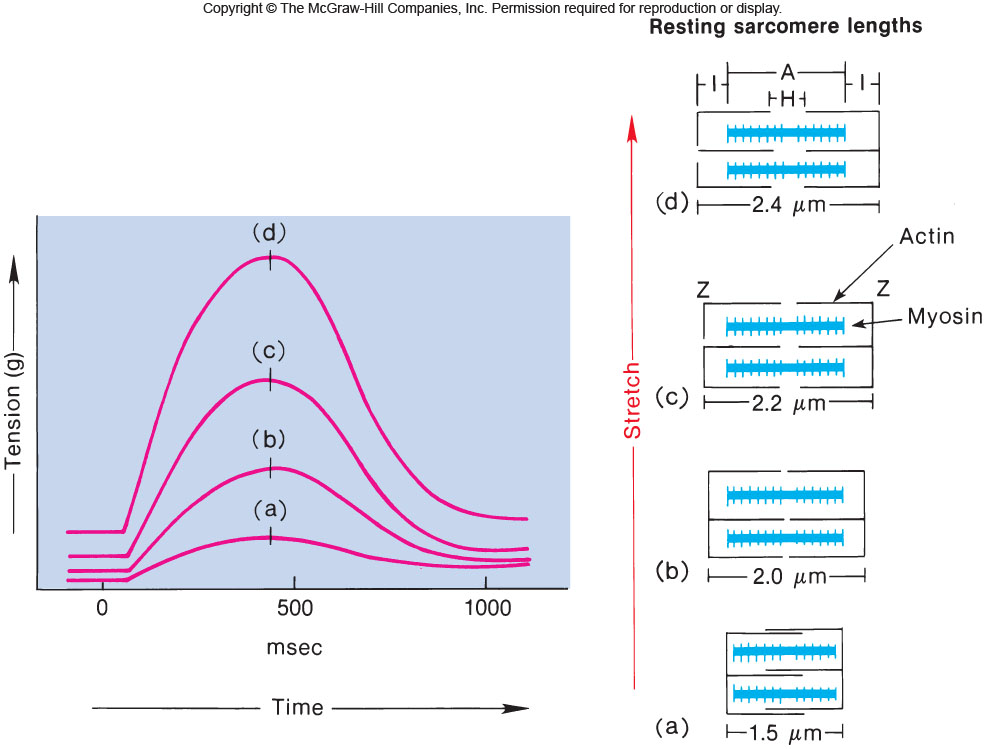
Preload
Amount of tension in the L ventricle immediately before it contracts
↑ preload = ↑force of contraction
Closely related to venous return (VR) → ↑VR → ↑preload
Frank-Starling law of heart - SV∝ EDV
ventricles eject as much blood as they receive
the more they are stretched, the harder they contract
Afterload
The “load” the heart has to push against in order to eject the blood from the ventricles
Blood pressure in the aorta and pulmonary trunk
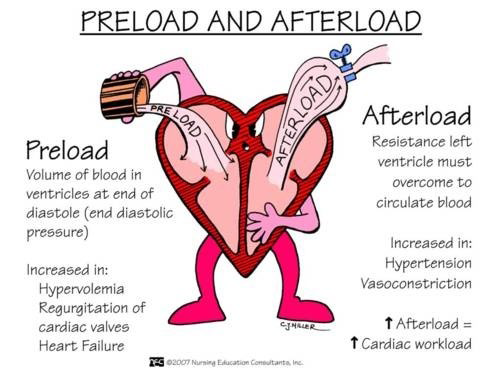
Anrep Effect
Sudden increase in afterload results in an increase in myocardial contractility to compensate → due to increased myocardial stretch
Due to increases Ca2+ entering the cytoplasm through the Na+/Ca2+ exchanger in the T-tubules
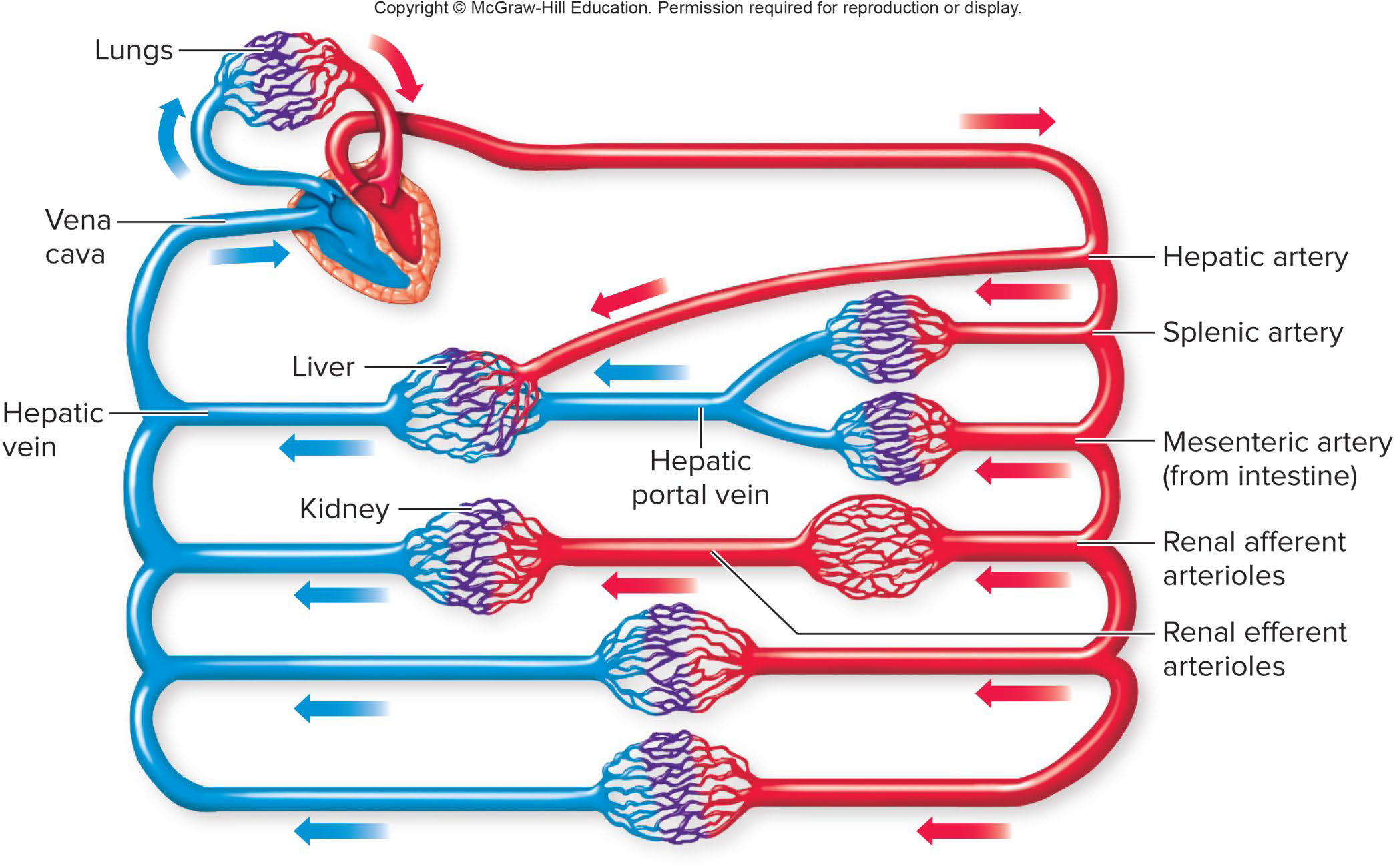
A very important consequence of these events is that the cardiac output of the left ventricle must equal the output of the right ventricle so that the blood flow through both the pulmonary and systemic circulations are equal.
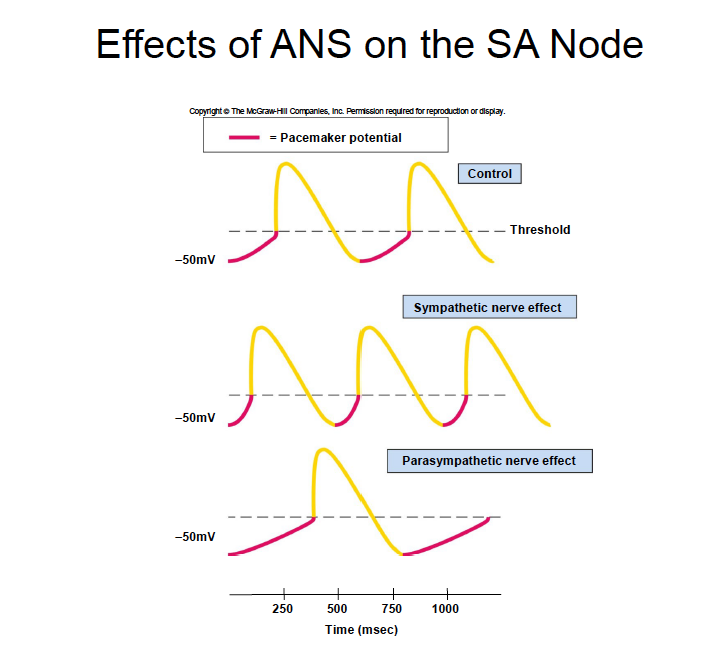
Factors Affecting Heart Rate
Chronotropy= affecting time or rate
Sympathetic system:↑HR → Positive chronotropic effect
Parasympathetic system:↓HR → Negative chronotropic effect
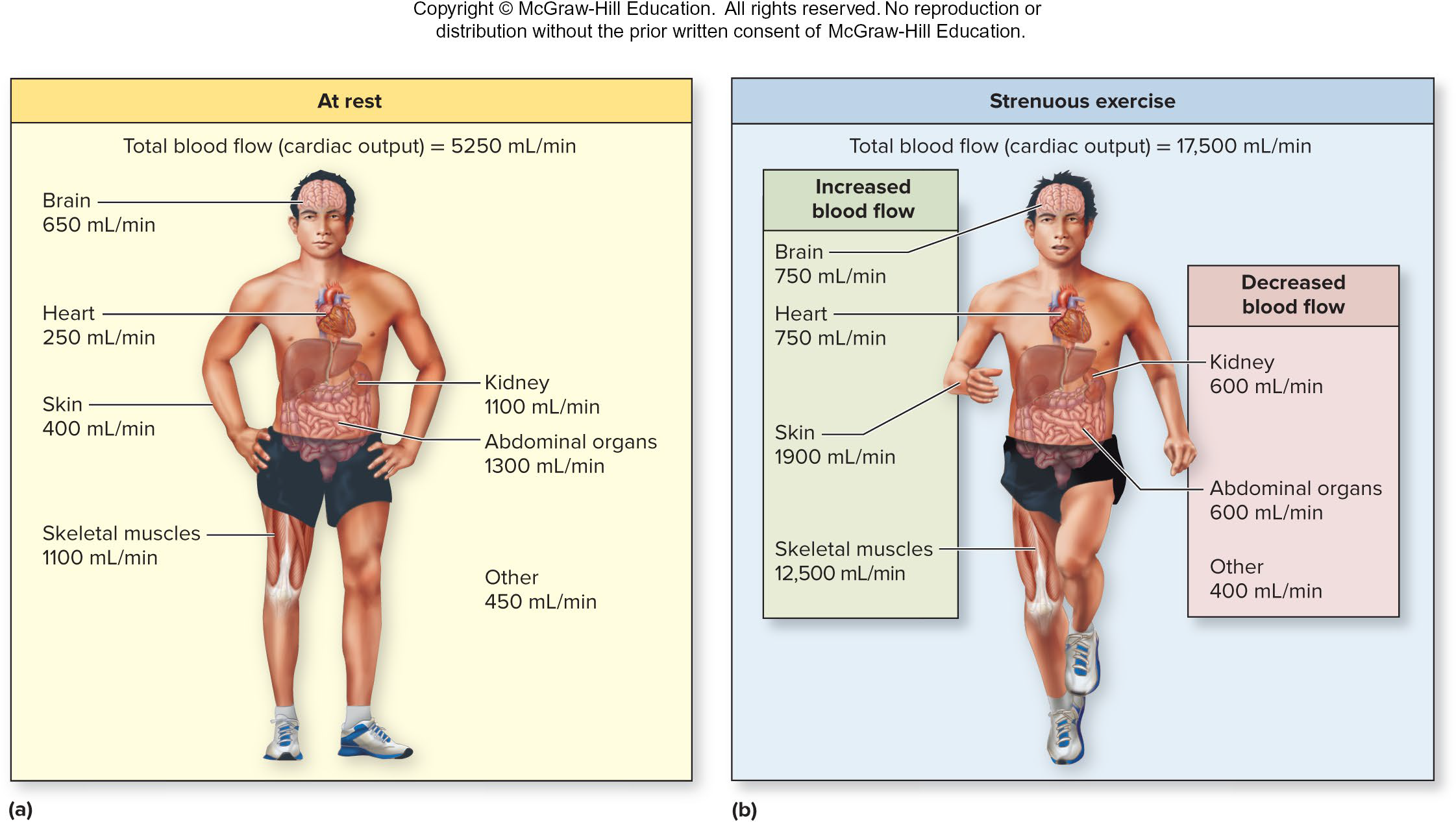
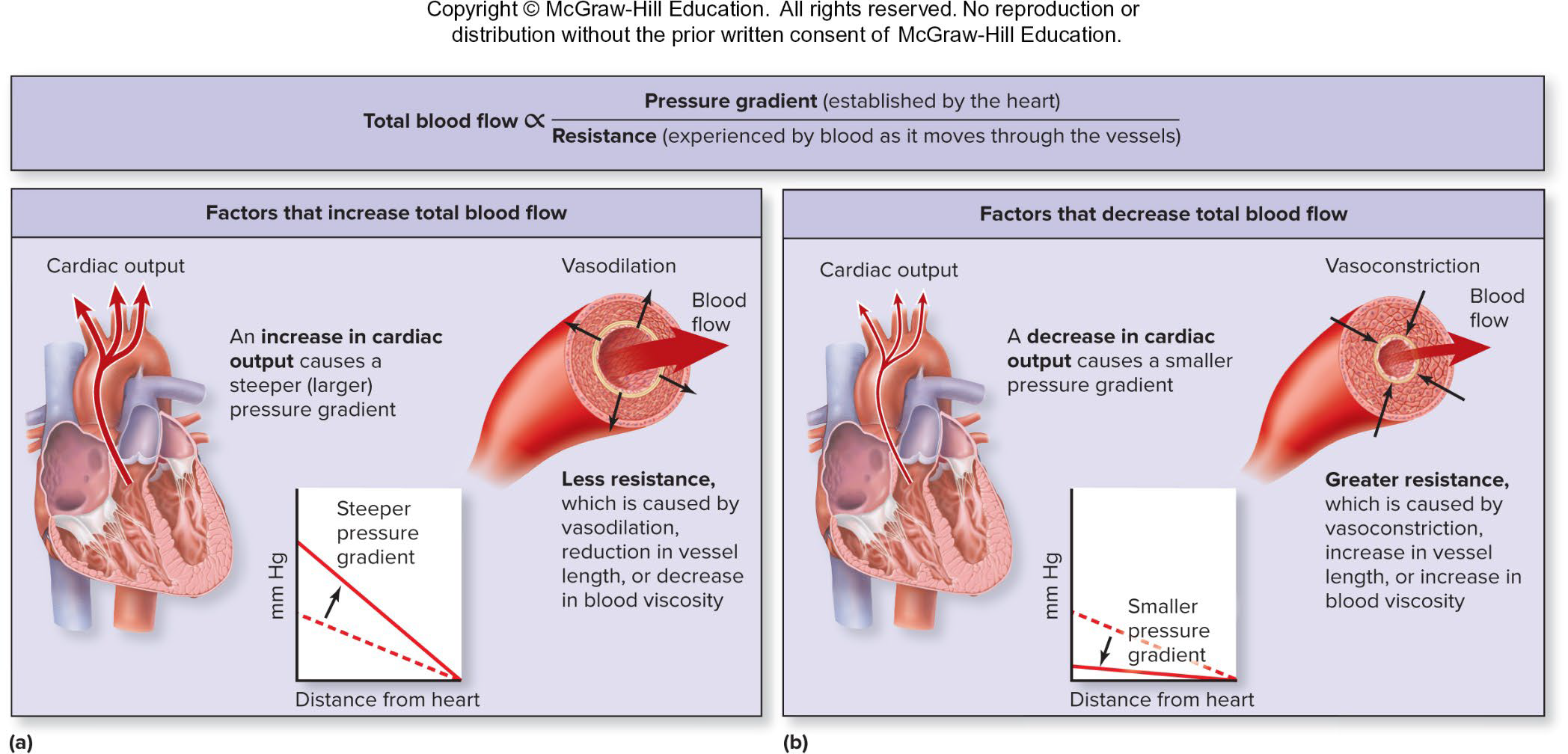
Blood Flow and Perfusion
Perfusion= Amount of blood flowing through an organ, tissue, or blood vessel / time (ml/min)
Blood is constantly reconditioned so composition remains relatively constant
Reconditioning organs receive more blood than needed for metabolic needs:
Digestive organs, kidneys, skin
At rest, blood flow is constant and = CO
Perfusion to other organs is adjusted according to metabolic needs
Ex: during exercise, fight or flight, etc.
Brain CANNOT tolerate disrupted blood supply:
Completely dependent on oxygen for energy
↓O2 → brain damage in ~5 min
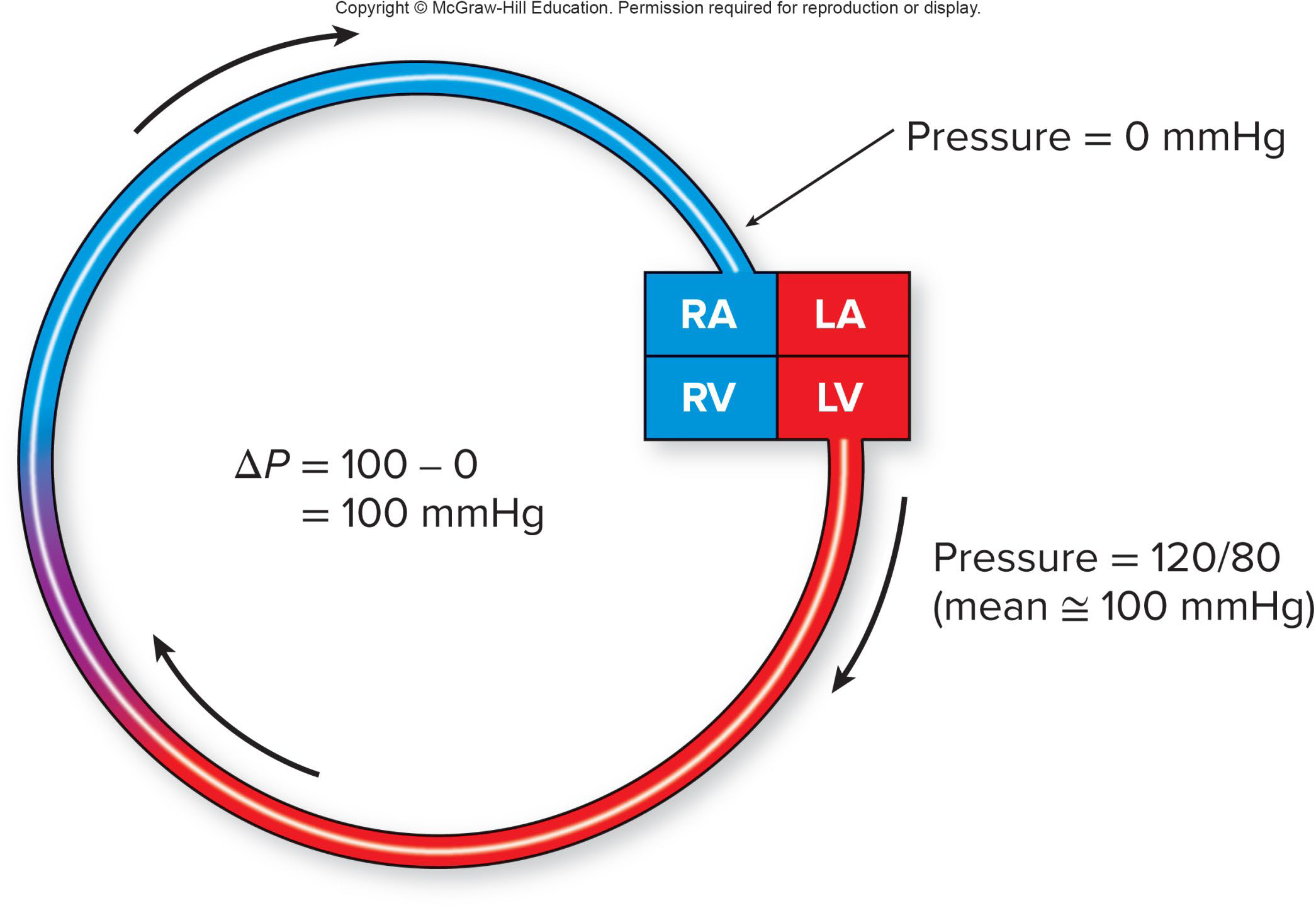
Hemodynamics
2 main variables that govern hemodynamics:
Pressure gradient: Fluid flows down its pressure gradient
Blood will always flow from an area of high pressure to an area of low pressure
Pressure gradient can be adjusted by:
↑ Pressure to overcome resistance → ↑ force of heart contraction
↓ Pressure in the tissue or organ → ↓ Resistance
Resistance: opposes fluid blood flow
Opposition of blood flow through a vessel
Referred to as peripheral resistance (PR) or (TPR)
Depends on 3 things:
Blood viscosity
Vessel length: the longer the vessel→ ↑the resistance
Vessel radius or diameter
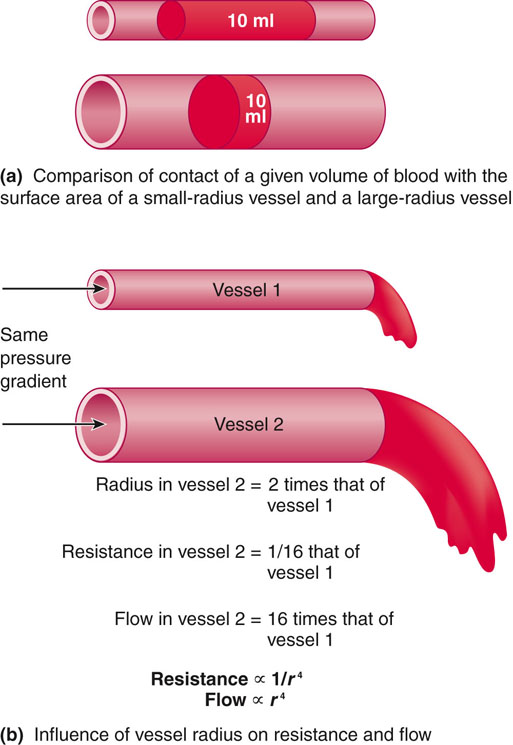
Major determinant= vessel’s radius
Slight change in radius → ↑ change in blood flow
R is proportional to 1/ r4
↓radius or diameter of blood vessel → ↑friction→ ↑↑ R
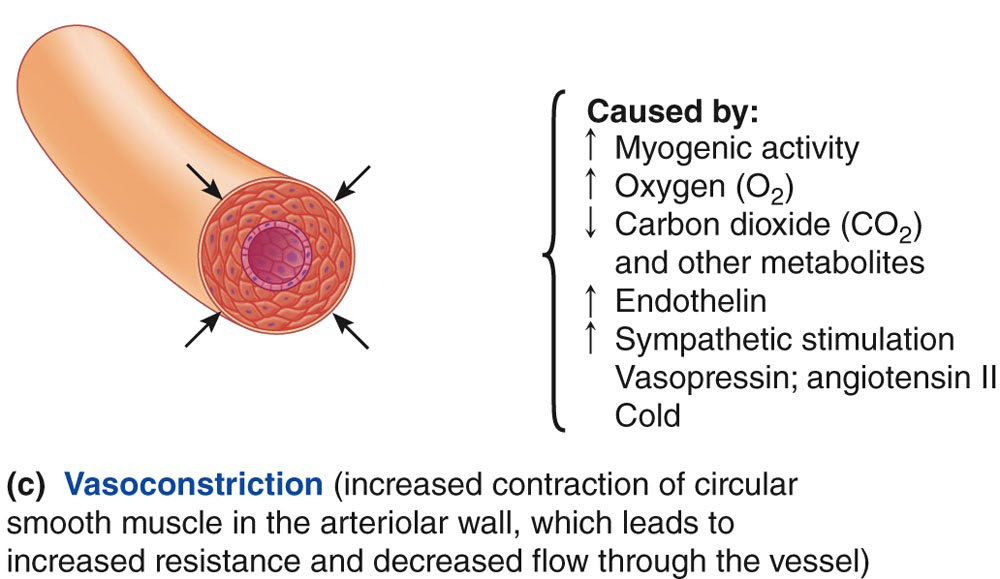
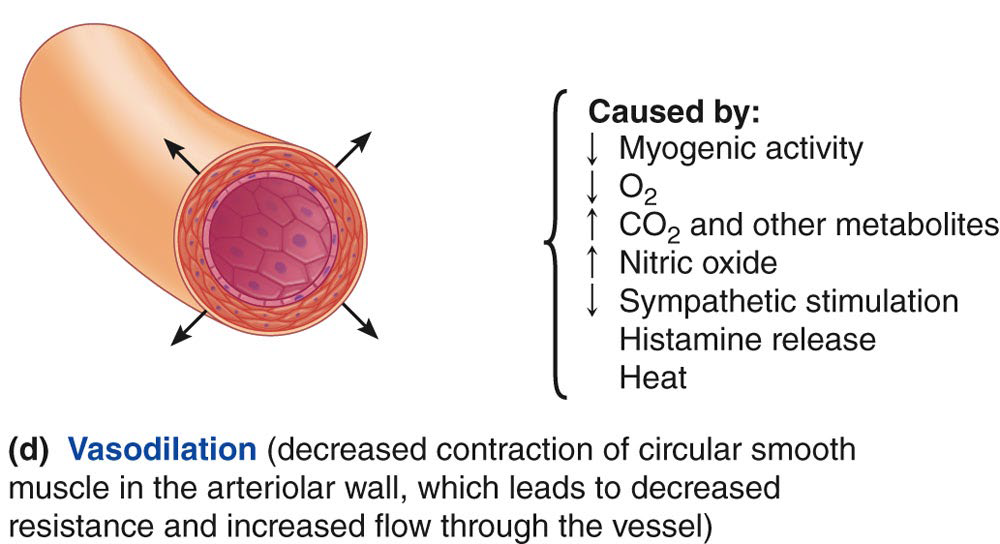
Regulation of Blood Flow
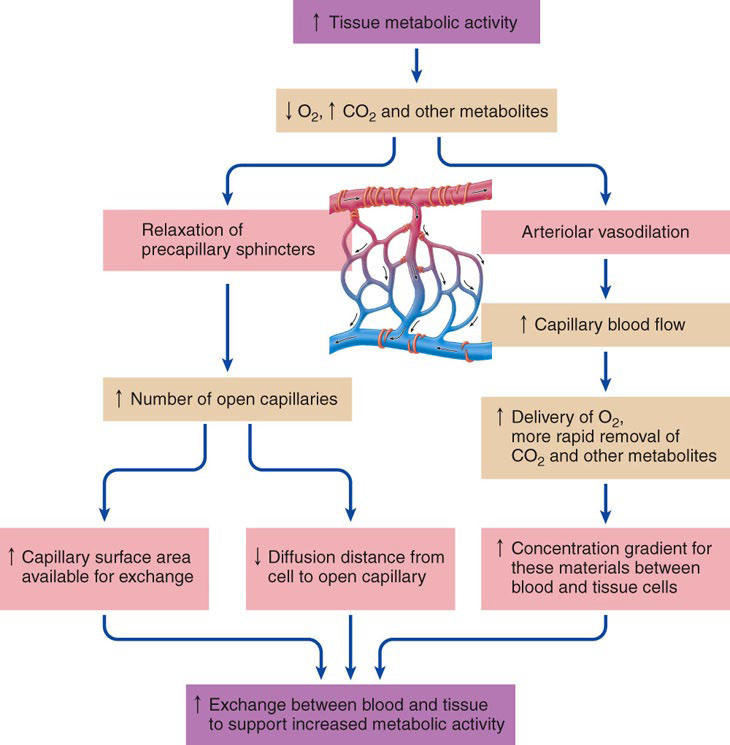
Local Blood Flow Regulation
Blood vessels undergo autoregulation→ vasodilation or vasoconstriction
No involvement from CNS or hormones
Respond to local chemical and physical changes (ex. stretch= Myogenic response)
Short-term regulation
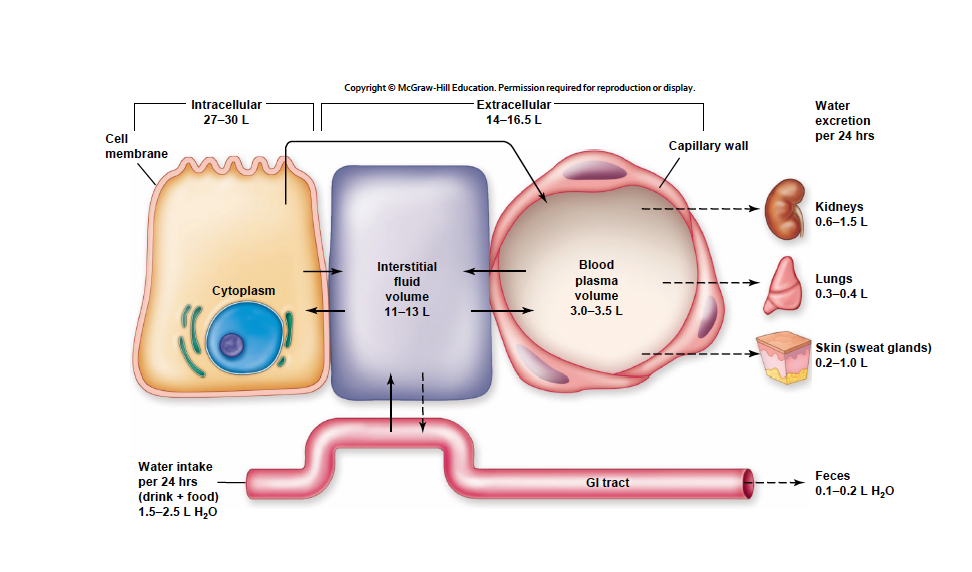
Long-term regulation→ changes in blood volume:Kidneys
Endothelial cell control:
Secrete vasoactive substances:
Nitric Oxide (NO)
Endothelin
Stimulate angiogenesis
Collateral circulation
Modulates capillary permeability
Changing pore size
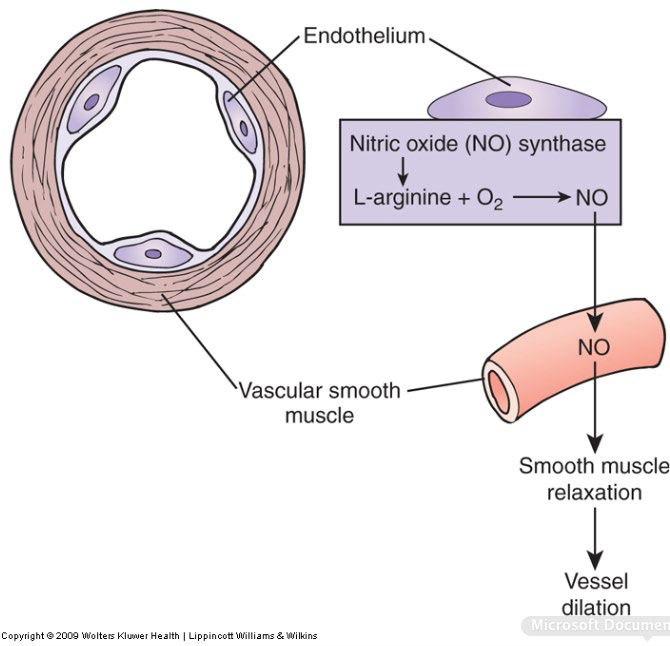
vasoconstriction
vasodilation
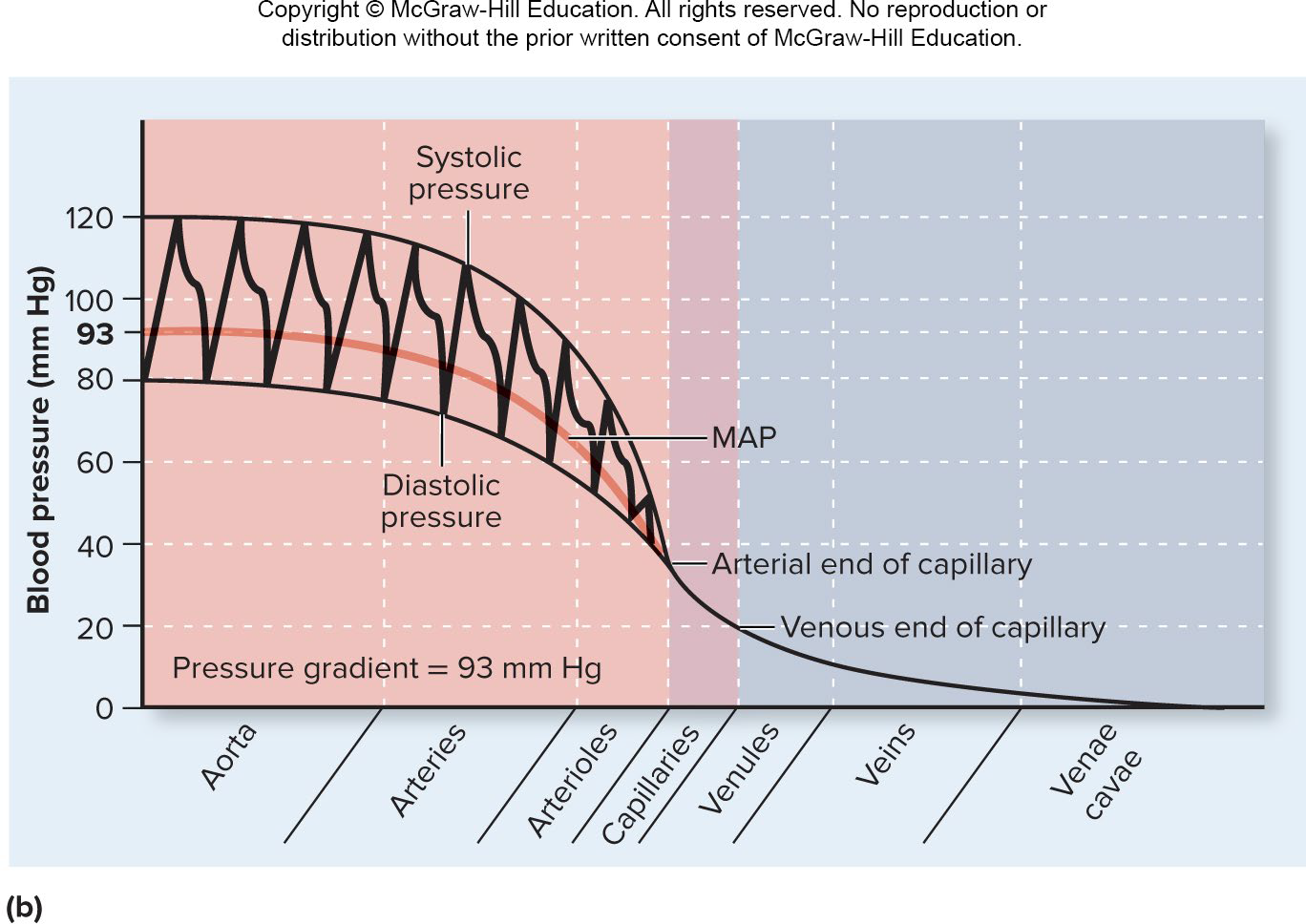
Blood Pressure (BP)
Is highest in the aorta
Declines throughout the length of the circulatory system
The steepest change in blood pressure occurs in the arterioles
Blood Pressure vs Vessel Type
Measured at brachial artery of arm using sphygmomanometer
Systolic pressure:
Peak arterial BP
Taken during ventricular contraction (ventricular systole)
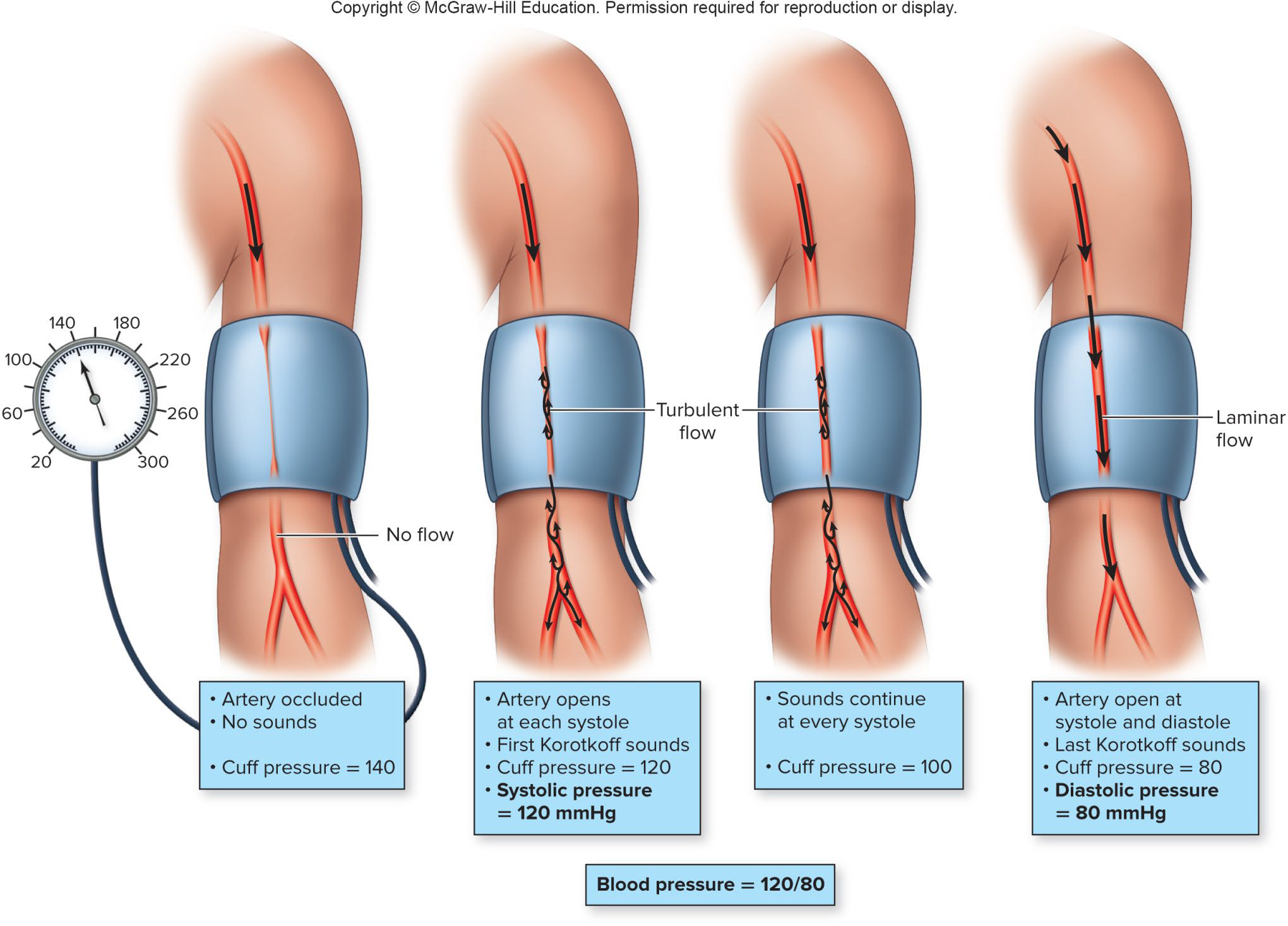
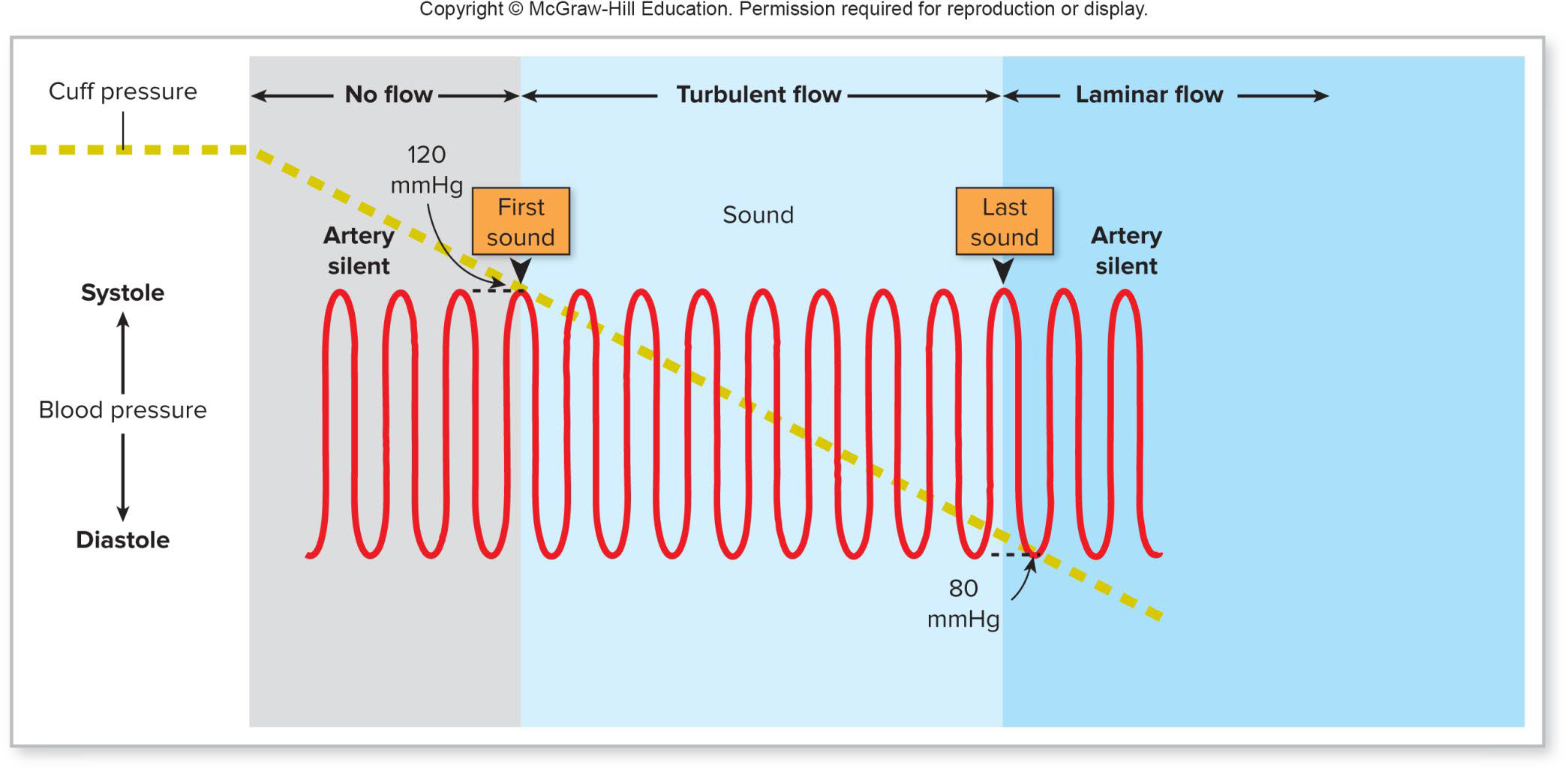
Pulse Pressure
Diastolic pressure: Minimum arterial BP
taken during diastole
Pulse pressure: difference between systolic and diastolic pressures
“Taking the pulse” is a measure of heart rate.
What the health professional feels is increased blood pressure in that artery at systole.
The difference between blood pressure at systole and at diastole is the pulse pressure.
If your blood pressure is 120/80, your pulse pressure is 40 mmHg.
Pulse pressure is a reflection of stroke volume
Mean Arterial Pressure (MAP)
Average pressure driving blood forward into tissues throughout cardiac cycle
MAP (or BP) = CO x TPR
Numerically calculated as: diastolic pressure + 1/3 pulse pressure
Arterial Blood Pressure
Dependent on two factors:
Elasticity of blood vessels closest to the heart → compliance
A vein is 24 times more compliant than its corresponding artery.
Volume of blood forced into them/time
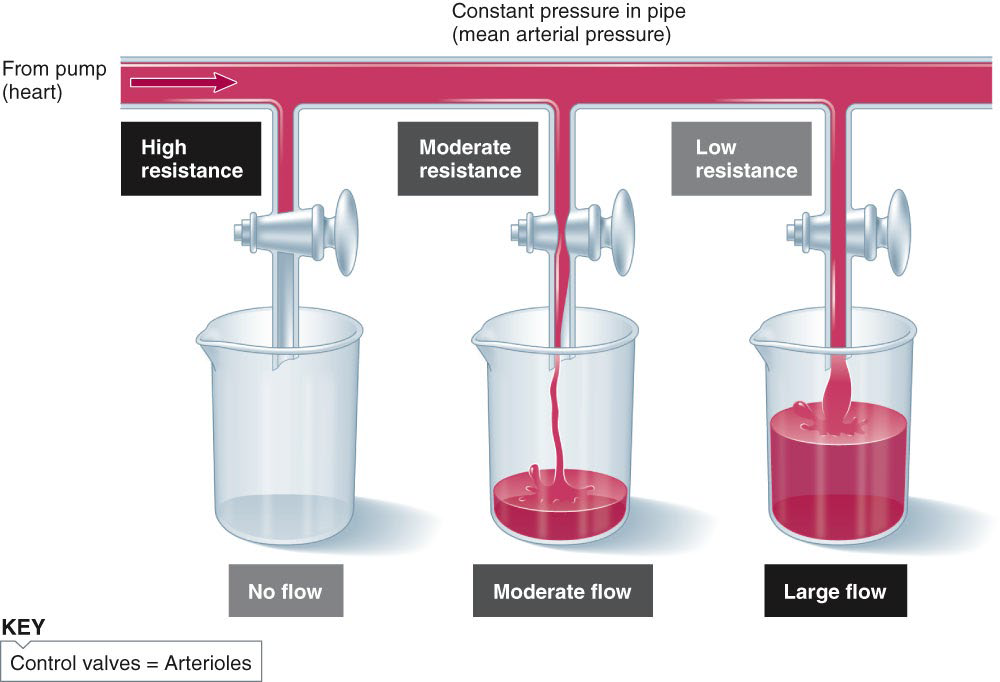
Arterioles = Major Determinants of TPR (resistance)
Arterioles are the major determinants of TPR
Mechanisms involved in adjusting arteriolar resistance:
Vasoconstriction: ↓vessel lumen size = ↑resistance
Vasodilation: ↑ vessel lumen size = ↓ resistance
Capillary Blood Pressure
Capillary BP ranges from 20 to 40 mm Hg
Desirable because ↑ BP would rupture fragile, thin-walled capillaries
Sufficient to force filtrate out into interstitial space and distribute nutrients, gases, and hormones between blood and tissues
Regulation of Blood Pressure
Essential for homeostasis
Requires:
Cooperation of the heart, blood vessels, and kidneys
Supervision of the brain
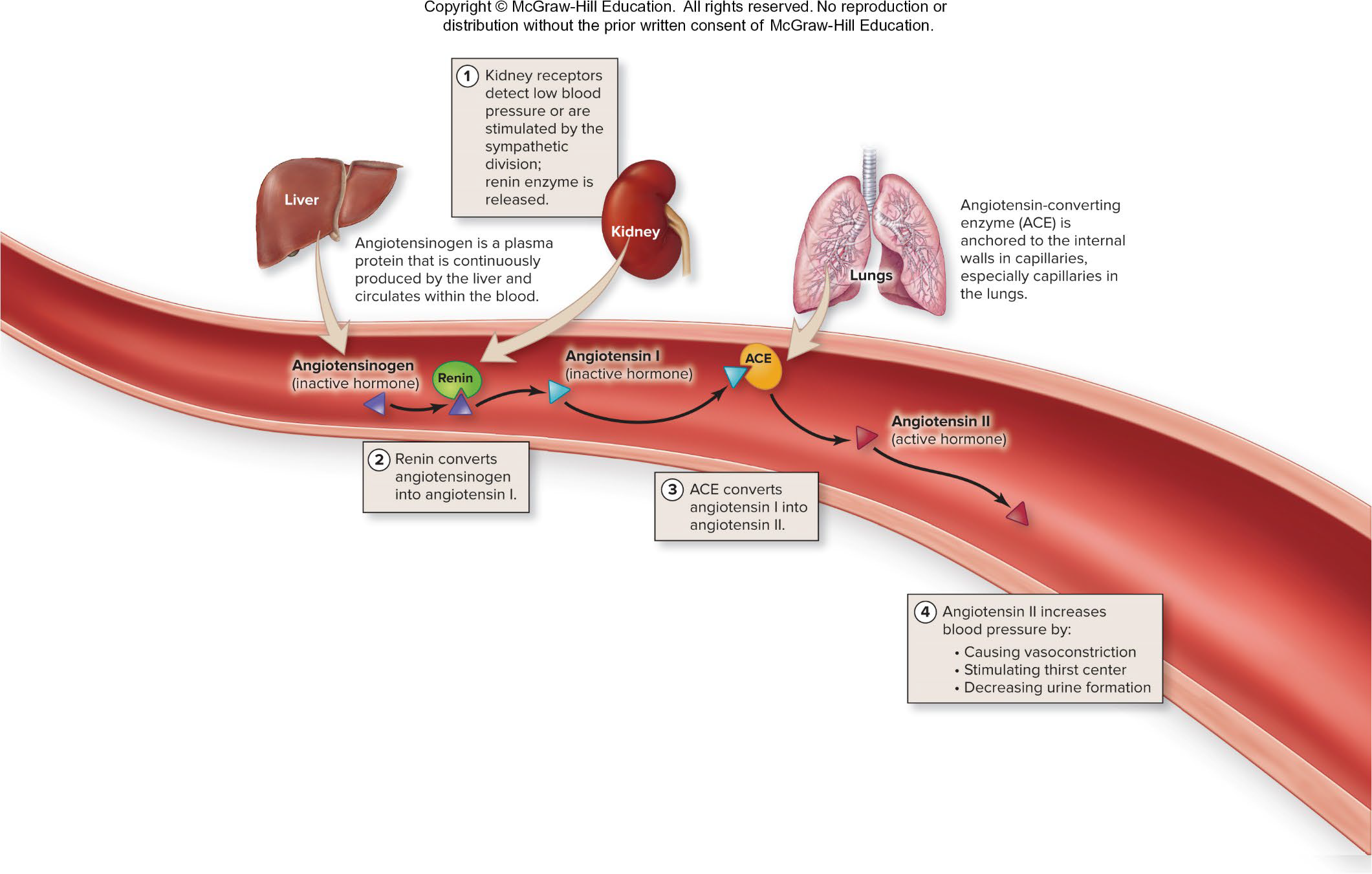
Vasoactive Chemicals: Vasoconstrictors
Epinephrine
Norepinephrine
Angiotensin I and angiotensin II***
Serotonin
Vasopressin (ADH)
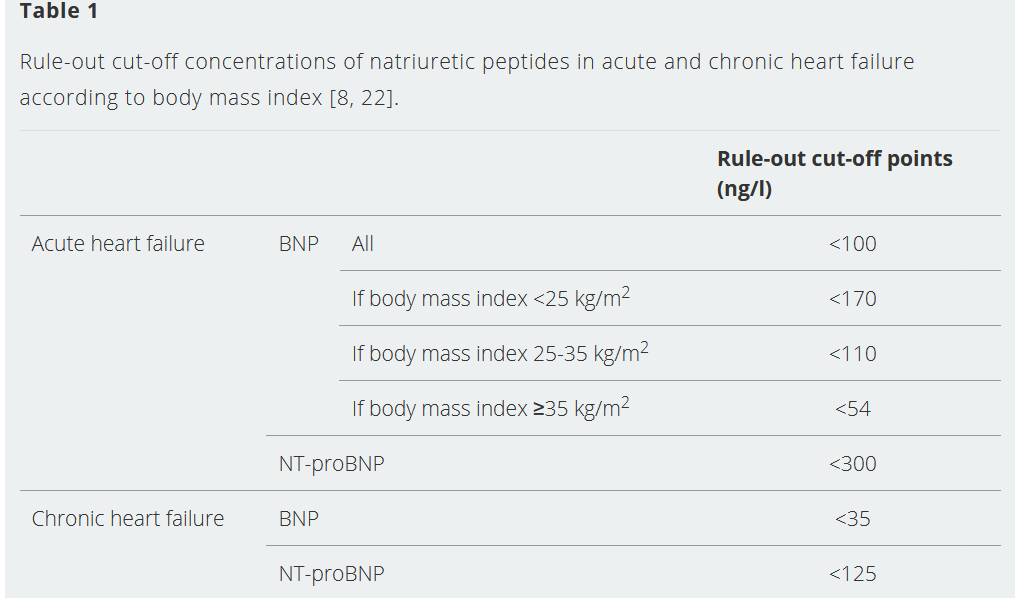
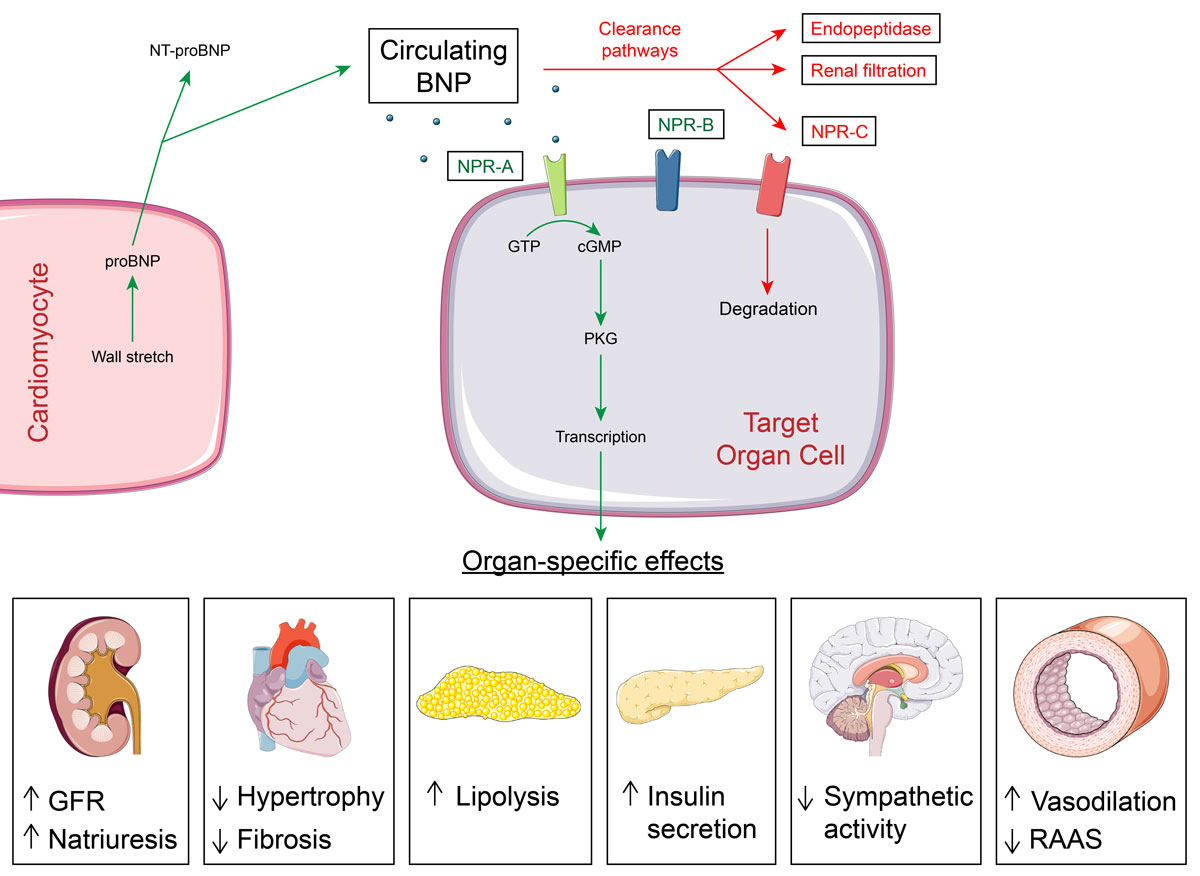
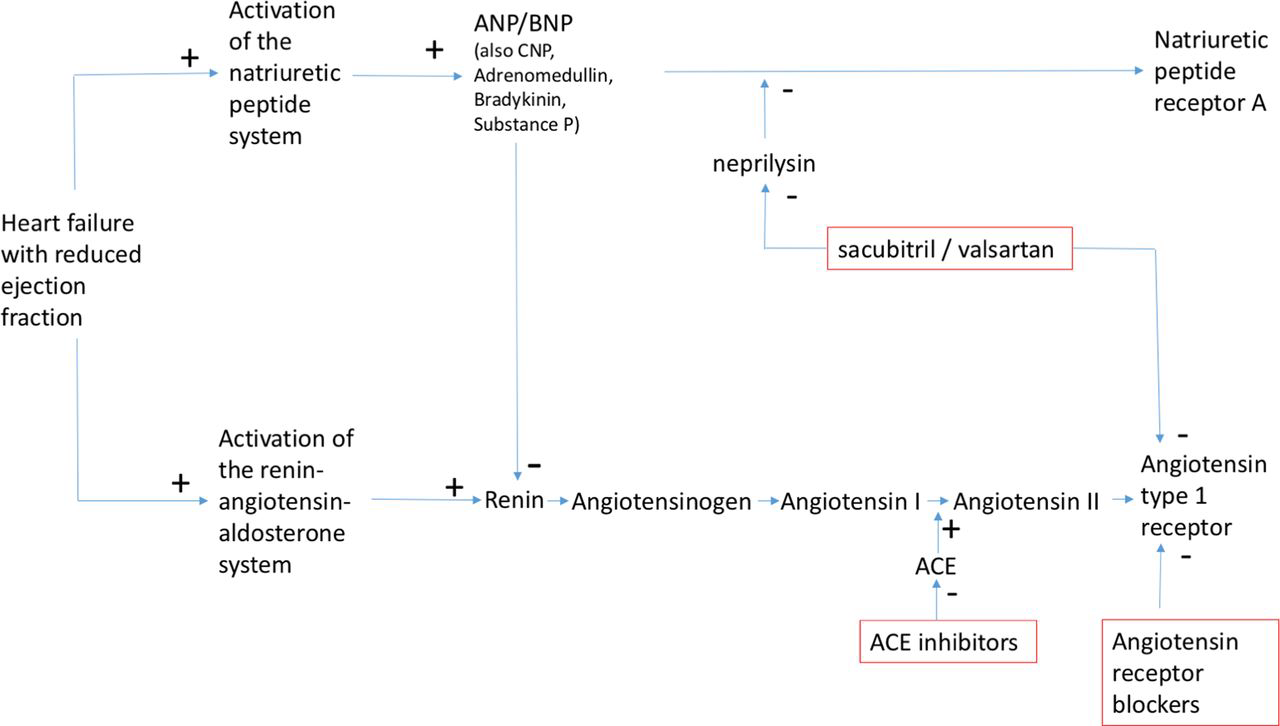
B-type natriuretic peptide (BNP)
Released by the ventricles in response to volume expansion and pressure overload
Also, NT-proB-type Natriuretic Peptide
Helps the body compensate in congestive heart failure
Blood test is diagnostic for heart failure
Effects of Natriuretic Peptides
Downregulate the effects of the Sympathetic NS and the RAAS
Sodium and water excretion via the kidneys
decreasing peripheral vascular resistance by causing smooth muscle relaxation
May inhibit cardiac growth and hypertrophy
Vasoactive Chemicals: Vasodilators
Histamine
Bradykinin
Prostacyclin (PGI2)
NO
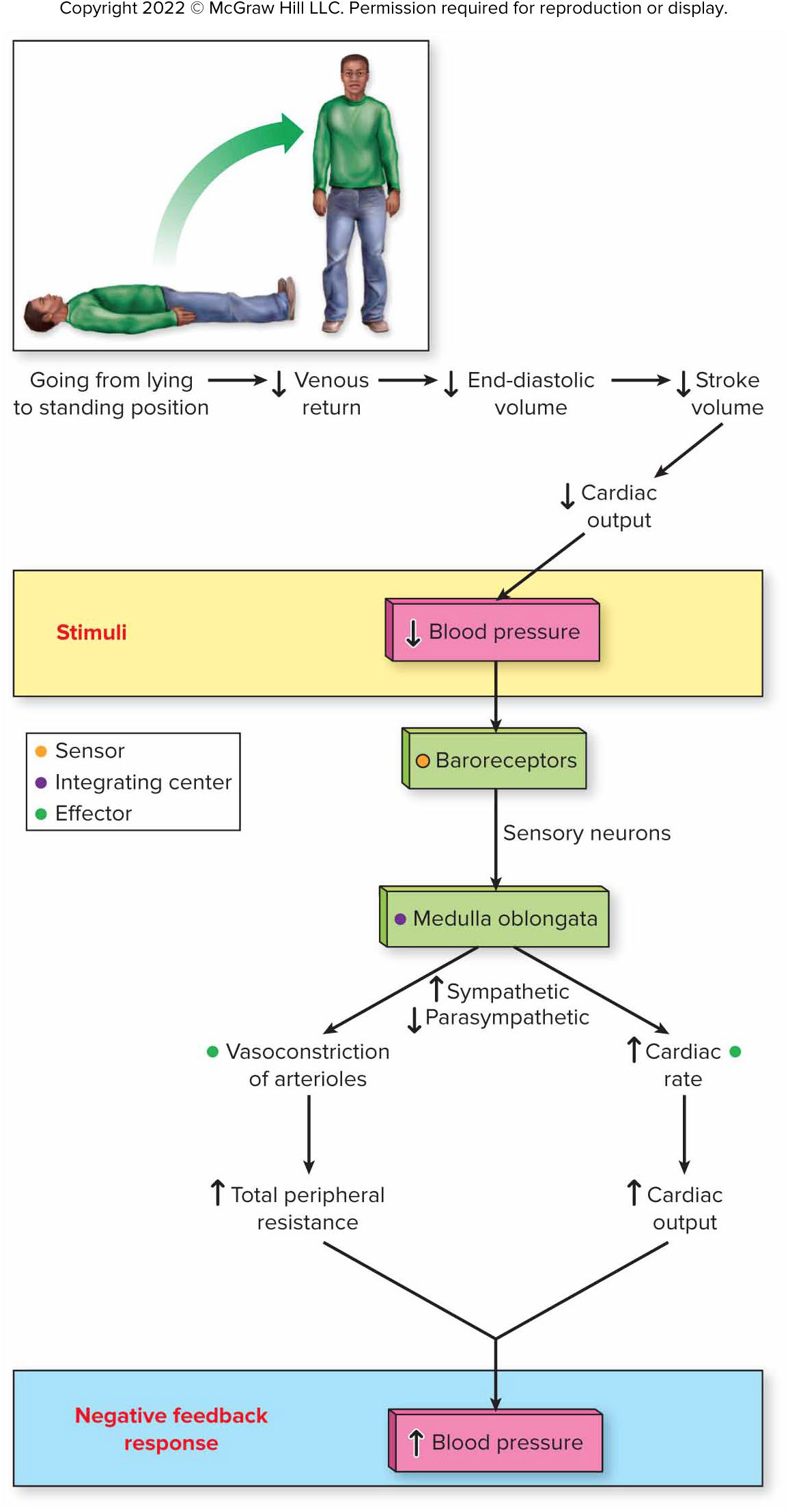
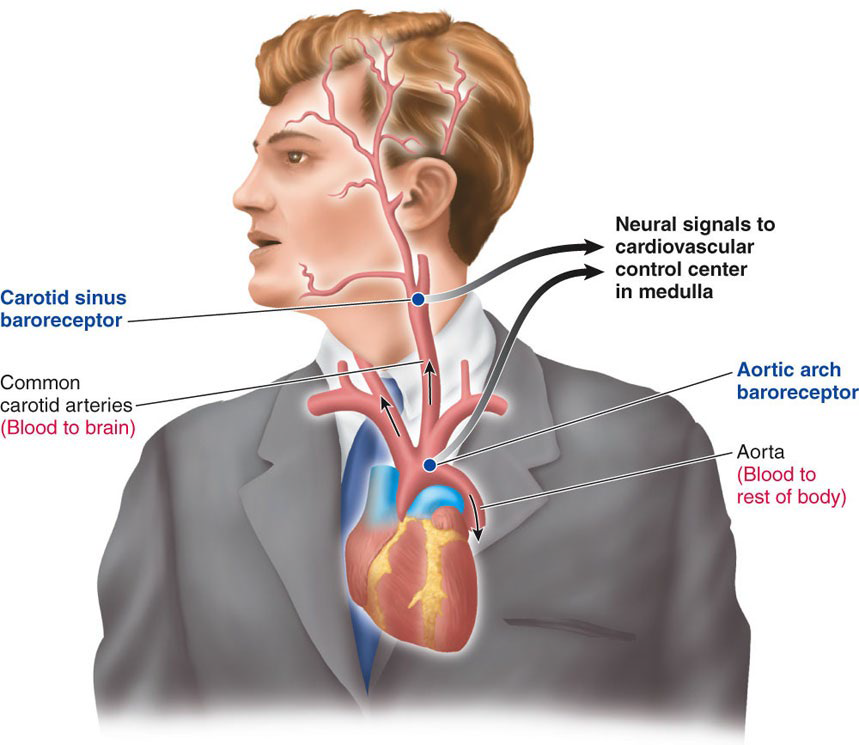
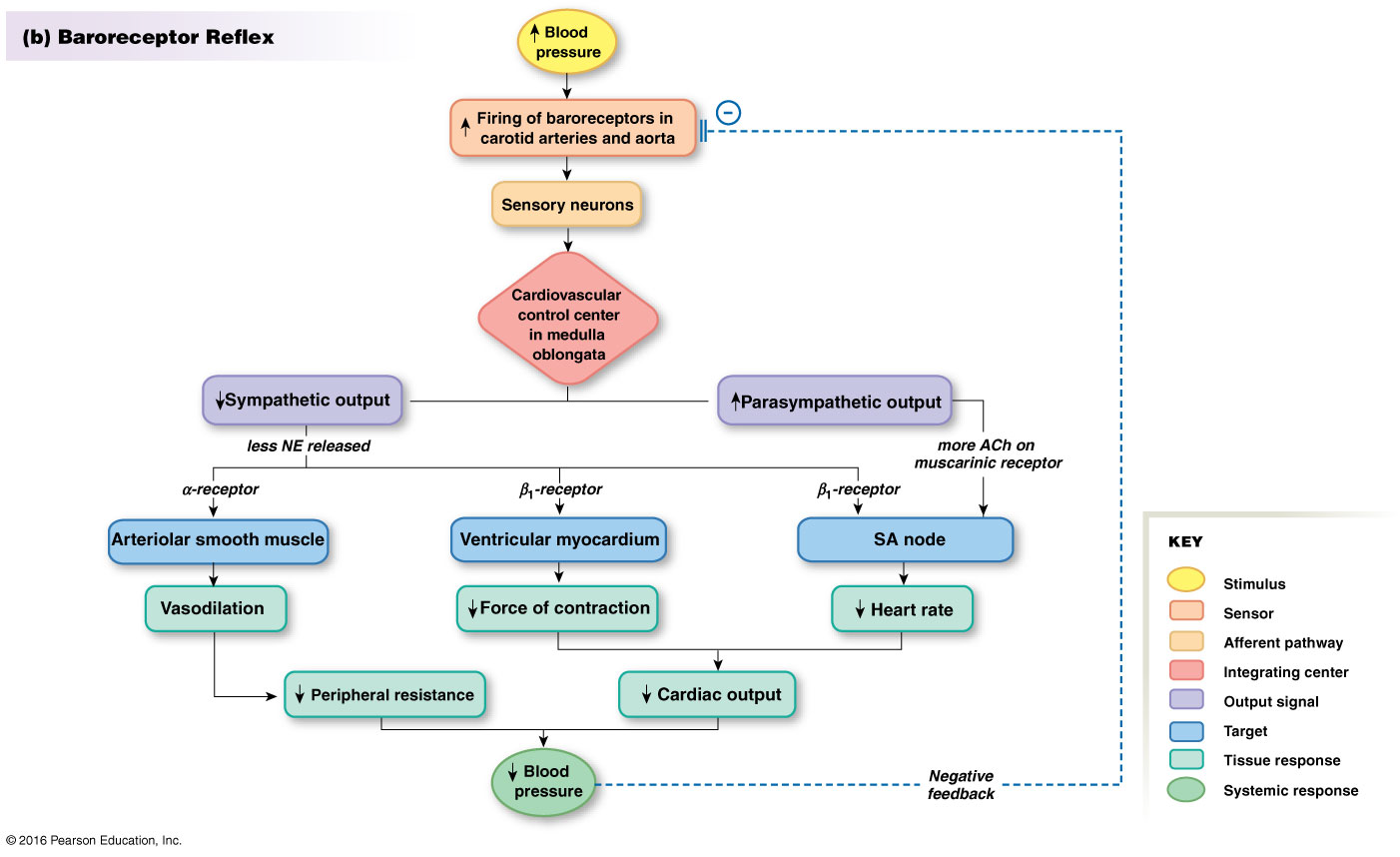
Control Centers for Cardiovascular Function and Blood Pressure Regulation
ANS Control Centers in Medulla Oblongata= Cardiovascular Center
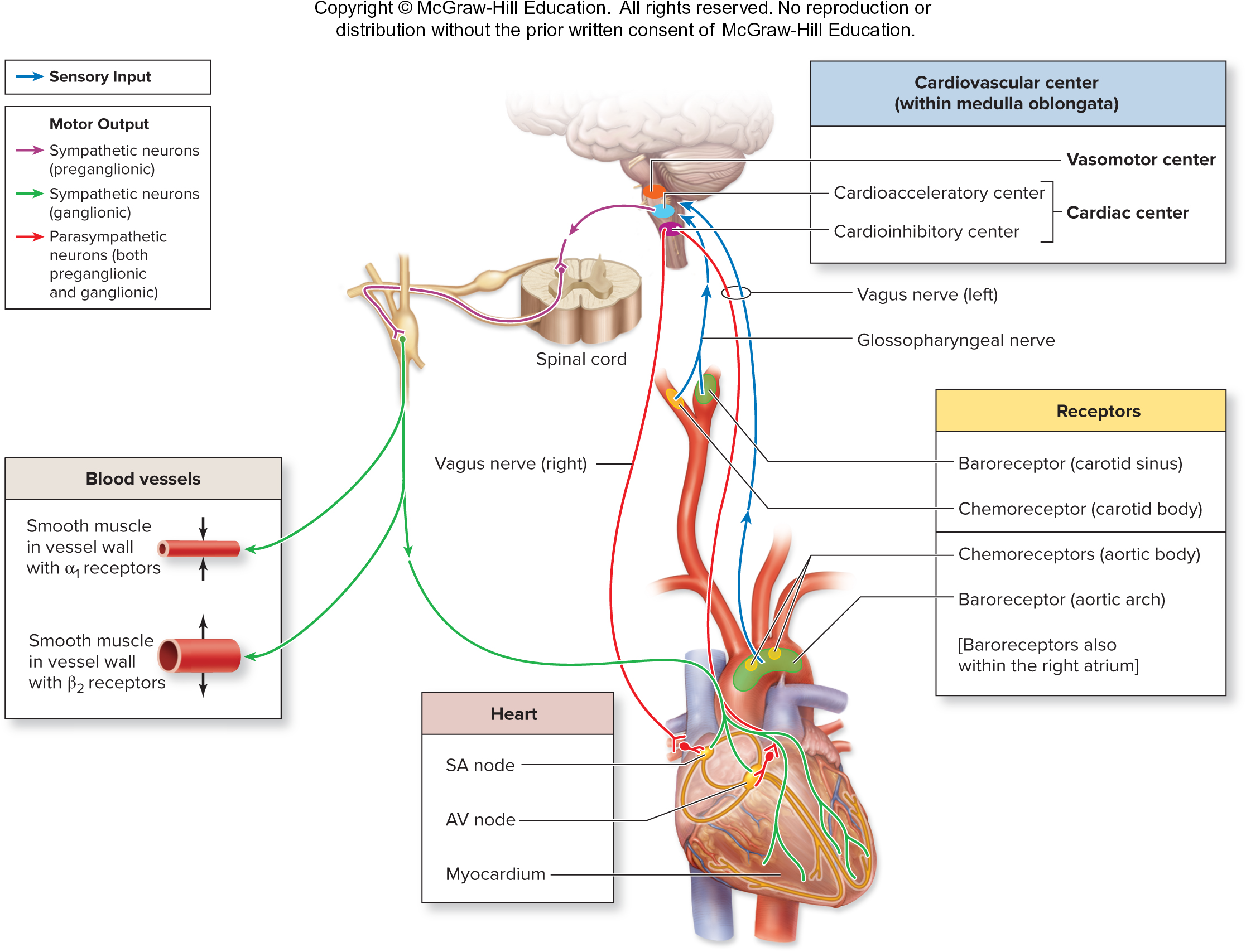
Vasomotor Center
The integrating center for 3 reflexes:
Baroreceptor reflex
Stretch-sensitive receptors
Monitor blood pressure
Important in short-term regulation of BP
Postural changes
Baroreceptors adapt to chronic high or low BP → NOT useful for long-term BP regulation
Reflex Tachycardia
Chemoreceptor reflex
Located in:
Carotid artery
Aortic artery
Sensitive to:
↓O2 or ↑CO2
↑H+
Main function: ↑respiration
Also ↑BP via activation of vasomotor center
Medullary ischemic reflex
Automatic response to a drop in perfusion of the brain
Medulla oblongata monitors its own blood supply
↑Sympathetic stimulation to the heart and blood vessels →
↑ HR and force of contraction
Widespread vasoconstriction
↑BP and restores normal perfusion to the brain
Other Control Centers
Other brain centers can affect vasomotor center
Hypothalamus: Temperature regulation
Cortical regions: Stress, anger, arousal can also ↑BP
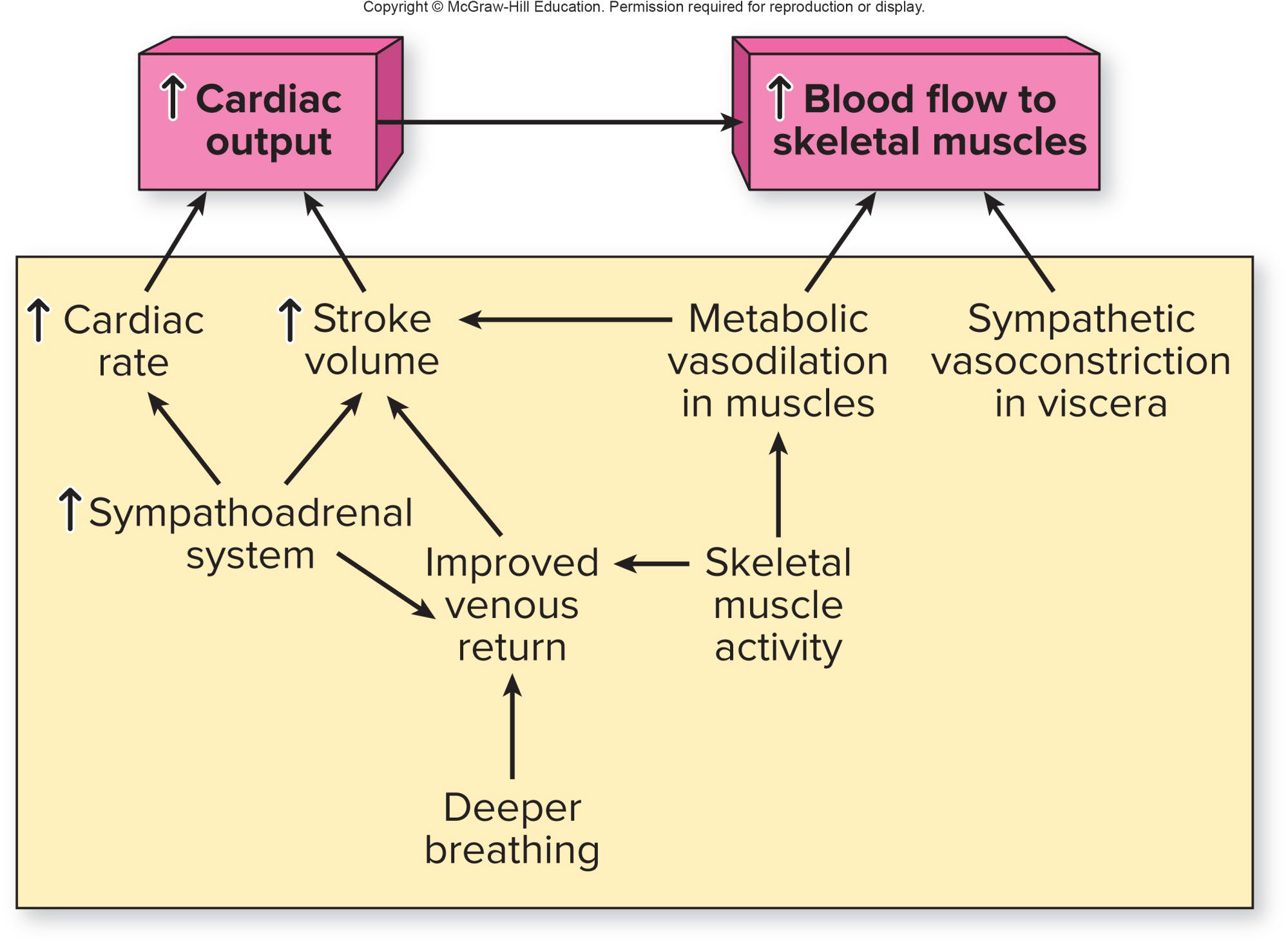
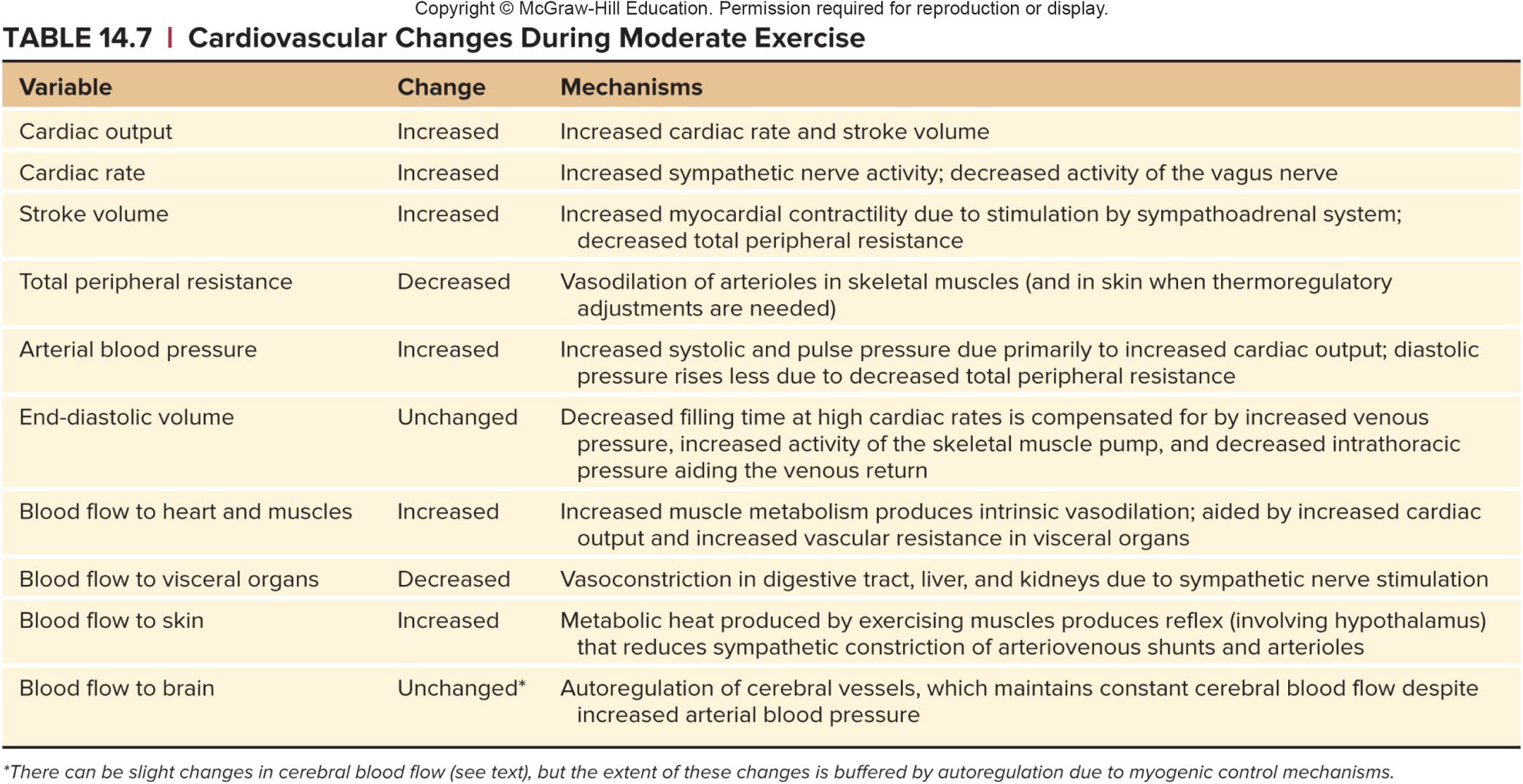
Cardiovascular Effects of Exercise
↑Perfusion to working muscle
Accomplished by:
Heart beats faster and stronger
↑BP
↓TPR
Blood is removed from venous reservoirs
Blood is redistributed so that more goes to active tissues
Cortex → Medulla → Vasomotor center → Activates sympathetic stimulation