Anatomy/Physiology Exam 3
Chapter 17 - Cardiovascular System
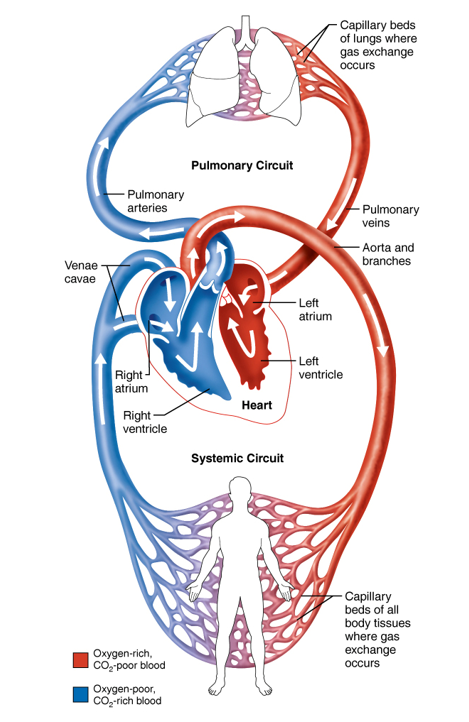
Pulmonary Circuit - Oxygenate blood
Systemic Circuit - Oxygenate body/tissues
Arterial = away from heart, out of ventricles
Venous = towards heart, into atrium
 Heart anatomy:
Heart anatomy:
Tissue layers:
Pericardium - outer covering, fibrous pericardium and parietal layer of pericardium
Epicardium (visceral pericardium) - inner serous membrane, secretes serous fluid into pericardium cavity
Myocardium - heart muscle
Endocardium - connective tissue/inner endothelium of heart
Valves: open and close with pressure differences, segregate atria and ventricles (AV valves) and ventricles and arteries (semilunar valves)
Chordae tendineae - anchor AV leaflets to papillary muscles
Papillary muscles - contract to hold valve closed and prevent backflow from ventricular contraction
insufficiency - valves weak and allow back flow (forces heart to work harder)
stenosis - valves stiffened and misshapen, creates turbulent flow leading to blood clots/strokes, may also need extra pressure/effort to open (strain)
Sounds: “lub-dub” = AV and then semilunar valves closing, murmur caused by stenosis or insufficiency
Coronary circulation - branches off aorta and returns to right atrium (through coronary sinus)
circulation needed because the tissues are too thick in the heart to rely on diffusion from the chambers alone (extend into myocardium)
Cardiac Muscle
Similarities: striated myofibril/sarcomere structure, T-tubules to carry AP to SR, troponin based excitation-contraction coupling
Differences: no fascicle structure, gap junctions, pacemaker, Ca+2 from outside of cell, can be excited or inhibited by ANS
Unique: branched and y-shaped cells, myofibrils irregularly aligned, strictly aerobic respiration
Intercalated discs - gap junctions and desmosomes anchoring neighboring cardiac cells to allow direct AP conduction, behaves as a single coordinated pump
Action Potential
Pacemaker cell - generate depolarization to trigger AP (SA node, AV node/bundle, Purkinje fibers)
Automaticity - heart beats on its own, rhythmically
Pacemaker potential is an unstable, rising “resting” potential due to Na+ entering via F-type sodium channels (open at -60mV, driven by K+, ‘hyperpolarized’) to progressively depolarize to threshold. Main polarization is from T-type (fast) Ca+2 channels (open around -50mV) which then accelerate pacemaker to L-type (slow Ca+2) threshold of -40mV. K+ restores membrane to -60mV
Conducting cells - carry AP quickly from nodes throughout heart, internodal pathway (bundle of His/bundle branches, purkinje fibers)
AP propagation: (1) Sinoatrial (SA) node generates impulse, (2) Depolarization spreads via gap junctions to atrioventricular (AV) node, delayed by 0.1 seconds, atria contract before ventricles, (3) pulse sweeps to AV bundle (only thing that connects atria and ventricles), (4) bundle branches conduct impulse through intraventricular septum to apex, (5) subendocardial conducting network (purkinje fibers) excite ventricles and they contract from the bottom up
SA node = 100 bmp intrinsic, ~70 bpm with vagal tone (parasympathetic “break”)
sets normal HR (fastest)
AV node = 50 bpm (backup pacemaker for isolated ventricular contraction)
impulses from SA reach AV before it would reach threshold on its own, AV responds to external stimulation under normal conditions (also a backup)
P fibers = 30 bpm (rescue pacemaker if bundles are blocked)
Ions: slow L-type Ca+2channels maintained a longer depolarized state (200+ ms) to ensure ventricle can contract to reach proper end-systolic volume and AP is as long as the twitch so the heart cannot tetanus (contract without relaxing). This also sets the maximum heart rate around 220 bpm
L-type stays open past the K+ channels to maintain depolarization; eventually they close and K+ can restore potential
Innervation:
SyANS - increase HR through beta-adrenergic receptors by depolarizing pacemaker faster, increase Ca+2 concentration and EC coupling
PaANS - decrese HR through inhibitiory muscarinic cholinergic receptors, hyperpolarizing pacemaker to slow threshold
EKG - medical tool to evaluate heart function based on electrical impulses/timing
P-wave - atrial contraction
QRS complex - atrial relaxation and ventricular contraction
T wave - ventricular relaxation
Cardiac cycle - volume, pressure, electrical changes and EKG, valve actions, sounds
Systole - begins at ventricular contraction, isovolumetric as pressure builds in contracting ventricle; V pressure rises above A pressure and AV valve closes (first heart sound and QRS complex, ventricle contains EDV). V pressure above arterial pressure and semilunar valves open (ventricular ejection, ejection fraction of ventricular blood flows into arteries)
Diastole - begins at ventricular relaxation (T wave), isovolumetric as pressure drops below arteries and semilunar valves close (second sound), ventricle contains ESV. Relaxation continues and blood flows into atria, pressure exceeds ventricular and AV valves open allowing blood into ventricle (80% passive filling dues to pressure gradient). P-wave occurs and atrium contracts to force remaining 20% into ventricle. Atrium relaxes and another QRS complex begins, reenters systolic, cycle continues.
Right vs Left - Pressures in LEFT are greater because the length and resistance of the systemic circuit are greater; left has much more muscle to generate 4x the pressure to move blood (same ventricular capacities)
Diseases
tachycardia - high resting heart rate (over 100)
bradycardia - low resting heart rate; different for athletes (under 40 dangerous)
arrhythmia - failure of coordinated heart rhythm
ectopic focus/extrasystole - competing pacemaker signal (with SA)
premature contractions (PAC or PVC) - an early beat followed by normal with more force than usual
bundle block - AV node or bundle of His are not functioning properly (ventricles fall behind)
pulmonary arrhythmia - normal reflex to change HR based on changing thoracic pressure
fibrillation - lack of coordination and ineffective blood pumping
more worrisome in ventricles bc they cannot pump blood
coronary atherosclerosis - buildup of plaque that occludes lumen and limits blood flow (dangerous in small coronary vessels and can cause heart attack)
high blood pressure (150/90) - blood volume mis-management, diastolic number more important
beta blockers - reduce sympathetic tone from epinephrine
ACE inhibitors - block enzymes for ANGII
ARBs - block ANGII receptors
CCbs - Ca+2 channel blockers
myocardial infarction - denial of blood to heart (heart muscles will be damaged and/or die), heart attack
cardiomyopathy - enlargement of heart (ventricles), weakened and flabby ventricles that cannot pump blood effectively
if afterload is too high it will not be able to compensate and leads to heart failure
congestive heart failure - high systemic afterload and excessive ventricular effort results in damage or disfunction and heart too weak to attain effective ESV
sometimes body compensates early on with kidneys and blood volume
left-sided because of the higher pressure (leads to buildup of fluid in lungs due to leakage from pulmonary circuit)
Chapter 18 - Circulatory System
Blood vessels:
Elastic arteries - high pressure, high flow, low resistance, high elasticity (propel blood by expanding and passively contracting with pulses to maintain blood pressure), upper arterial tract
muscular arteries - high pressure, high flow, low resistance, lower elasticity and more muscular activity to modify flow to organs
arterioles - lower pressure, lower flow, higher resistance (high tuning), highest pressure drop (resistance vessels); maintain total peripheral resistance (TPR) and BP by smooth muscle action and small lumen (sympathetic tone controlled)
capillaries - low pressure, low flow, high surface area; filters for blood into (filtration) and out of (reabsorption) the interstitial fluid; diffusion/transport of gases, waste, nutrients, signaling molecules
continuous - strong barrier, pinocytosis fluid movement, most common, forms blood-brain barrier (some intercellular clefts for filtration)
fenestrated - porous barrier, stops most proteins but high bulk fluid movement through fenestrations/clefts, areas of high filtration/reabsorption (kidney, digestive, endocrine)
sinusoid - very porous, allows unrestricted fluid flow through sinunsoids (proteins and cells), bone marrow, liver, adrenal medulla
venules (little veins) - transition structure between capillaries and veins, some functional aspects in reabsorption
veins - low pressure, high flow (low flow RATE), high compliance (low elasticity); low pressure gradient BUT check valves and muscle/respiration-based pumping moves blood to heart, volume reservoir (activity forces blood into circulatory flow to deliver gases/nutrients quicker)
Flow
Systemic - 75% (60% in venules alone, blood reservoir)
Arterial flow at rest: 20% muscles, 25% abdominopelvic organs, 13% brain, 20% kidney
Pulmonary - 12% (5% in capillaries, 8% in heart)
Cardiac output (CO) = stroke volume x BPM
CO of systemic and pulmonary are the same, stroke volume is equal and beats are coordinated
Preload - pressure on resting heart from venous return, (left-ventricular end diastolic pressure, LVEDP) leading to stretch on heart
Frank-Starling relationship - increased preload → increased contraction (resting cardiac muscle is shorter than optimal, so when stretched it can provide a larger contraction)
Contractility - strength of contractions at given stretch (controlled extrinsically by SyANS and endocrine system)
Afterload - amount of diastolic pressure on heart by arteries (backpressure against ventricular contraction)
increased by high BP, arteriosclerosis, atherosclerosis/stenosis
heart is adapted to normal pressure, but increased P can cause valve damage (elevated diastolic pressure is more concerning to doctors!)
SV = EDV - ESV
End diastolic volume (EDV) - highest volume of ventricle during cardiac cycle, determined by venous return (but mostly physical activity or SyANS activity)
End systolic volume (ESV) - lowest volume of ventricle during cycle, function of how hard the ventricle is working (contractility) and afterload; altered by SyANS, endocrine and humoral
Flow = difference in pressure / resistance
arterioles have greatest resistance and also easiest to control resistance (diameter) and therefore flow (also manages MAP upstream)
HR and SV changes are not to change MAP but rather provide the flow required (TPR is the main SHORT TERM way to change MAP)
MAP = diastolic pressure + 1/3 pulse pressure
systolic - pressure at peak of ventricular contraction
diastolic - pressure when ventricles are relaxed and filling
pulse pressure - difference between systolic and diastolic
MAP proportional to CO and TPR; changes in HR, SV, CO, vascular tone ALL affect pressure (long-term changes in volume are done by kidney)
Autoregulation - intrinsic control at the tissue level, responds to local nutrient/waste levels, loss of blood flow, skeletal muscle activity, temperature
dilation of local vessels to increase flow to metabolically needy tissues
Active hyperemia - blood flow increases (vasodilation) to muscles when active due to decrease in nutrients and O2 and increase in temperature
Filtration and Reabsorption
20 L/day filtered out of plasma into ISF from arteries and 17 L/day is reabsorbed into plasma on venous side
3 L/day remains in ISF and becomes lymph (unless swelling is occurring); returned to circulation, through lymphatic drainage into subclavian artery
starling forces (hydrostatic [bulk] and osmotic [solute])
hydrostatic pressure - force on wall from fluid
capillary HP - filtration through capillary walls (35 mmHg)
interstitial fluid HP - reabsorption through capillaries (17 mmHg)
colloid osmotic pressure - force opposing HP, large non-diffusible molecules
capillary OP - plasma proteins in blood (25 mmHg ISF to blood)
interstitial fluid OP - (0.1-5 mmHg)
fluid flows out of capillaries at the start (net +10) and back into capillaries at the end (net -8)
Neurological control
vasomotor tone - constant stimulation by SyANS through maintenance norepinephrine and epinephrine produced by the adrenal medulla (a bit constricted at rest, BP drops at night when SyANS is slowed, high BP is a sign of stress)
baroreceptors - located in carotid sinus and aortic arch to measure BP and report to medullary cardiovascular center
increased pressure → increased Action Potential frequency → increased CV efferent signals → increase SyANS activity → increase HR and SV
only respond to changes in “normal” so it will not affect high resting BP (tolerance)
chemoreceptors - present in carotid sinus and aortic arch (measure pH and O2 levels and brain stem (osmolarity)
changes in gas concentration → increased activity of cardioacceleratory center → regulation of breathing
Endocrine controls
epinephrine - SyANS, accelerates HR, increases SV, increases vasoconstriction, increases BP
mainly to maintain MAP with external conditions and activities
angiotensin II/III - renin-angiotensin-aldosterone system (RAAS)
ANGT to [by renin] ANGI to [by ACE] ANGII to [by ACE2] ANGIII;
ANGII stimulates aldosterone, causes vasoconstriction when BP low;
ANGIII stimulates aldosterone but NOT vasoconstriction
response to low BP or volume, ACE inhibitors are effective anti-hypertensive drugs
vasopressin/ADH - posterior pituitary to affect low BP and/or high osmotic strength
long-term (renal) to reabsorb more water into bloodstream
ONLY way to alter osmotic problems other than thirst (does not move salt)
at high levels it is also a vasoconstrictor, short-term, in conjunction with ANGT (angiotensin)
Long term control: RAAS and kidney
aldosterone - water/mineral balance in body (mineralocorticoid); increases water retention in kidneys by reabsorbing sodium, increases K+ excretion by kidney (high potassium, low sodium, low BP, SyANS and RAAS stimulate aldosterone)
atrial natriuretic peptide (ANP) - produced by heart, stimulated by myocardial stretch in atrium; antagonizes aldosterone and decreases ADH production, generalized vasodilation through renin inhibition
vasopressin/ADH
EPO - produced by kidney in response to low PO2, increases RBC production and oxygen transport capacity
high altitude is a huge trigger here (Olympic training center in CO spgs)
will increase blood viscosity and thus BP/resistance, however most systems balance this out
Diseases
Hypertension - high blood pressure (over 130/90)
risk factors: genetics, stress, obesity/diet, age, smoking
treatments: lifestyle changes (diet, exercise), lowpressors (ACEi, beta-blockers) as vasodilators, diuretics (Lasix) to lower blood volume
Hypotension - not common, but shock is life-threatening (lack of adequate blood flow, 90/60)
hypovolemic - low blood volume (hemorage)
vascular shock - poor circulation due to vasodilation
anaphylactic - widespread vasodilation due to histamine cascade (allergy)
neurogenic - ANS disruption (psychological or “fear” shock)
septic - widespread infection (vasodilation) or DIC (clotting that blocks blood flow)
cardiogenic - heart problems and cannot sustain BP (heart attack or failure)
Chapter 21 - Respiratory system
Ventilation and Pressures
Ventilation = breathing, exchanging air outside the body with air inside lungs
driven by muscle contraction (diaphragm and intercostal muscles) that create pressure differences (works due to vacuum seal of pleural membranes)
intrapleural negative pressure (seal) changes pressure on lung wall and thus lung volume
Inhalation - contraction of diaphragm (lowers) and external intercostals (raises)
forced inhalation - engages inspiratory reserve volume (use of scalenes)
Exhalation - relaxation of diaphragm (raises) and contraction of internal intercostals (lowers)
forced expiration - engages expiratory reserve volume (use of abdominals)
Boyle’s Law: P1V1 = P2V2
F = DP/R (DP= difference between atm and lung pressure, R determined by radius of bronchi)
Characteristics of respiration
compliance - extent of stretchiness (measured in DV/DP)
determined by health of tissue and alveolar surface tension
lung surfactant - biological detergent to disrupt surface tension in alveoli which would otherwise exert so much force that the lung collapses (keeps them open)
anatomical dead space - amount of air in conducting airways that cannot undergo gas exchange (150/500 mL is dead space)
alveolar dead space - alveoli that get air but not effective blood flow to exchange gases
V/Q balancing eliminates airflow to these alveoli
Respiration
Respiration = gas exchange between air and blood or blood and tissues (requires dissolution and diffusion)
dissolution - amount of CO2 and O2 in the blood, measured as partial pressures
Dalton’s law = sum of partial pressures = atm pressure
Henry’s law = gas dissolved in liquid related to Pgas
Pressure gradient - drive diffusion
Thickness (permeability) and surface area - greater SA = faster diffusion (40x SA of skin)
Gas solubilities - O2 is faster but CO2 is more soluble
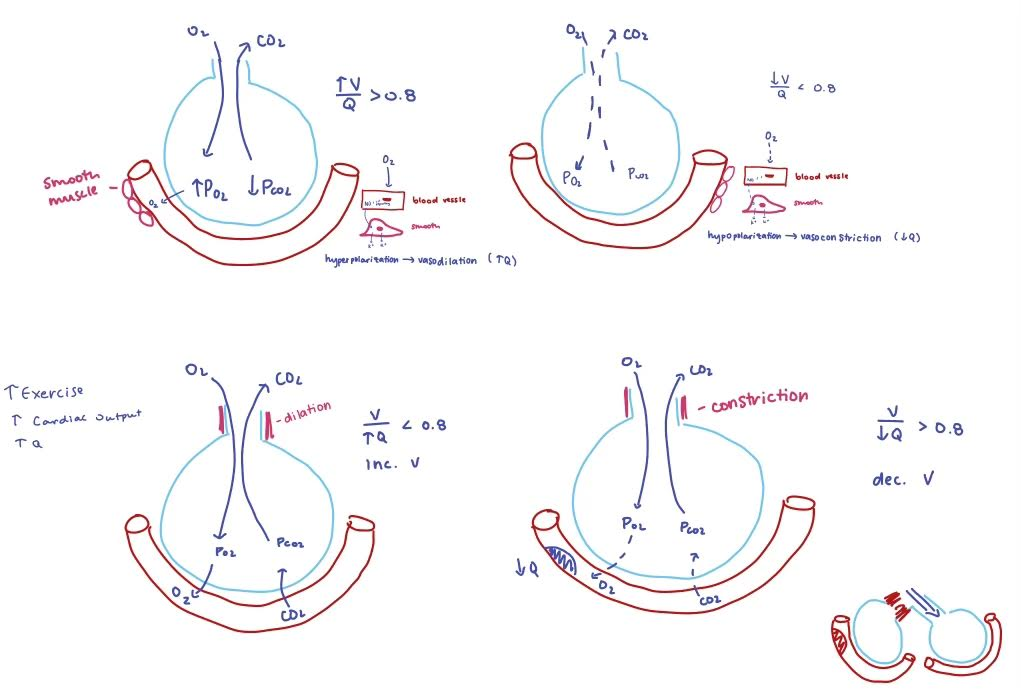
V/Q coupling - control of each variable to balance air and blood flow (~0.8, not 1 due to gravity)
V=alveolar ventilation rate (AVR)
change in ventilation → change in perfusion (controlled by PO2)
Q=perfusion (cardiac output, CO)
change in perfusion → change in ventilation (controlled by PCO2)
internal respiration - tissue exchange of gasses with bloodstream (systemic capillaries)
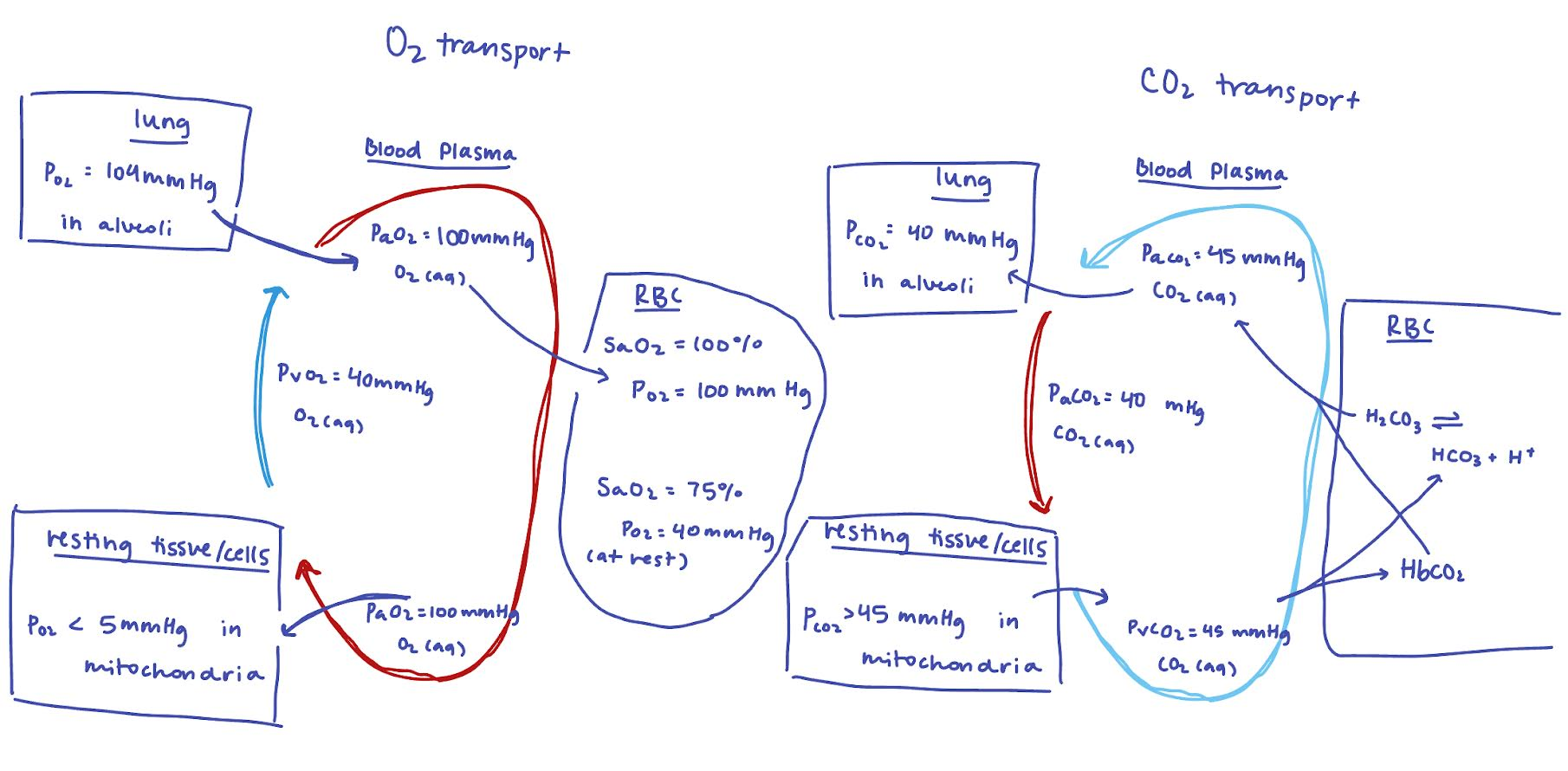
Oxygen transport
1.5% dissolved in plasma (100 mmHg in arterial blood, 40 mmHg in venous)
98.5% bound to hemoglobin (4 O2/molecule, 98% saturated at 100 mmHg)
25% unloaded at rest
80% unloaded under metabolic demand (decreased O2 and increased CO2/decreased pH)
Bohr effect decreases O2 affinity with decreasing pH
CO2 transport
10% dissolved in plasma
70% converted to HCO3 (bicarbonate buffer system)
partial pressures do not change as much as O2 due to the buffer system
20% bound to hemoglobin as carbamate (bound to amino group)
Haldane effect decreases how much CO2 can bind when higher O2 binding
Innervation
Medulla and pons - three centers to control unconscious breathing
ventral respiratory group (VRG) - contractile stimuli to inspiratory and expiratory muscles in an oscillating pattern
pre-Botzinger complex = first respiratory pacemaker discovered
dorsal respiratory group (DRG) - integration of chemoreceptors and stretch receptors to modulate VRG
pontine respiratory group (PRG) - smooths out transitions and also voluntary activities (deep breathing and vocalization)
hypothalamus - integrates strong emotion and pain to respiratory responses
cerebral cortex - voluntary control over respiration (hold breath)
can be overridden when CO2 accumulates
hering-breuer reflex - stretch receptors to prevent over-inflation of lungs
Diseases
atelectasis (collapsed lung)- damage to lung tissue or chest wall has broken vacuum seal of pleurae so there is no pressure gradient; air in thorax means no breathing (shrinks like balloon)
pneumothorax - air in pleural cavity, no pressure gradient, pulled out with tubes
Infant Respiratory distress syndrome (IRDS) - babies don’t produce enough surfactant and have trouble inflating alveoli
fibrosis - damage/scarring of lung tissue stiffens wall and reduces compliance
asthma - brachioconstriction limits airflow significantly
pneumonia - fluid accumulated in alveoli, preventing air from entering respiratory spaces
hypoxia - lack of oxygen in the tissues of the body (must drop below 60% in plasma before it becomes a major respiratory drive)
anemic - not enough RBC or Hb
ischemic - blockage in blood flow (heart attack)
histotoxic - body can’t use oxygen even if it’s available (cyanide)
hypoxemic - respiratory distress
CO poisoning - competitive inhibitor of O2 binding to Hb
hypercapnia - excessive CO2 in blood
chemoreceptor reflexes are sensitive to CO2 and alter ventilation to compensate (O2 sensors are less sensitive, mainly backup for CO2 sensors)
hyperventilation - CO2 exchange > CO2 metabolism
excessive ventilation, O2 affinity increases (not released) and it is not released when needed
hypoventilation - CO2 exchange < CO2 metabolism
not enough ventilation, blood is acidic, will also result in low O2
Chronic Obstructive Pulmonary Disease (COPD) - irreversible decrease in ability to force air out of lungs
emphysema - destruction of alveolar walls, loss of elasticity, increase in compliance, loss of effective respiration (leads to increased strain on right side of heard)
chronic bronchitis - inflammation, mucus, narrow bronchi (resistance to outflow of air, leading to hypoventilation causing an oxygen-dependent respiratory drive
Altitude sickness
body overreacts to changes in O2, fatigue, shortness of breath, nausea, headache (over 8000 ft)
Acclimation is possible over time
low PO2 in air → low PO2 in blood → increased O2 and CO2 chemoreceptors → stimulation respiration, BPG increases and more O2 is released by Hb
low O2 in kidney stimulates EPO to produce more RBC (compensate for low PO2)
SARS-CoV-2
spike proteins bind to ACE2 and enters the cell (prominent in heart and lung tissues)
not the mechanism for damage, simply the key into the cell; explains the localization in these tissues
infection-driven inflammation and immune activities → damaging interstitial pneumonia