Pathology of the Kidneys and UUT Part 4 Flashcards
Urolithiasis
Definition: Commonly known as kidney stones.
Mechanism: Concentrated urine leads to higher amounts of minerals and acid salts sticking together, forming calculi.
Symptoms: Severe pain, potential obstruction distal to calculi.
Treatment: Increased hydration; lithotripsy may be needed for larger or obstructed calculi.
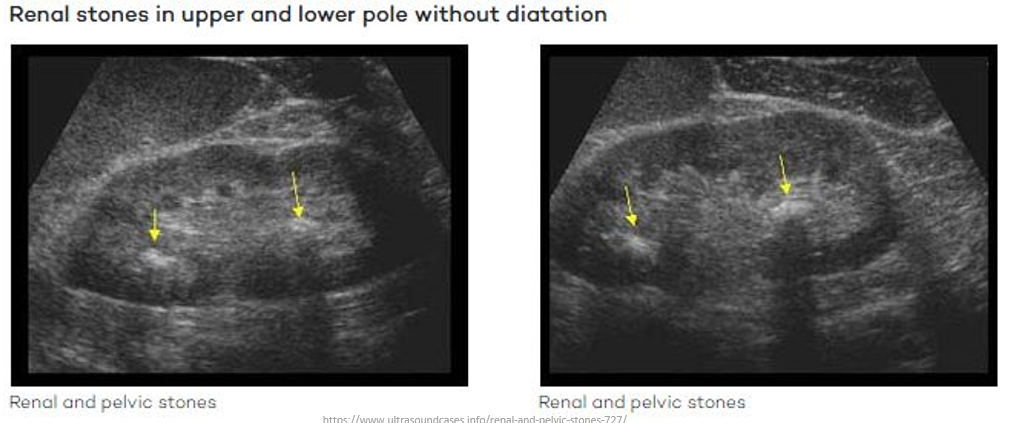
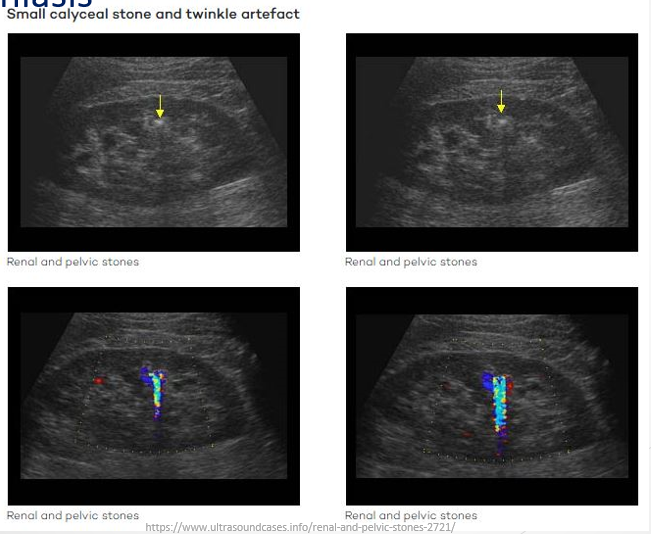
Sonographic Presentation:
Very echogenic with posterior shadowing.
Tiny renal and ureteric stones can utilize the twinkle artifact in sonography.
Variants observed: small calyceal stones, stones in the renal pelvis (both with and without renal dilation).
Medullary Sponge Kidney
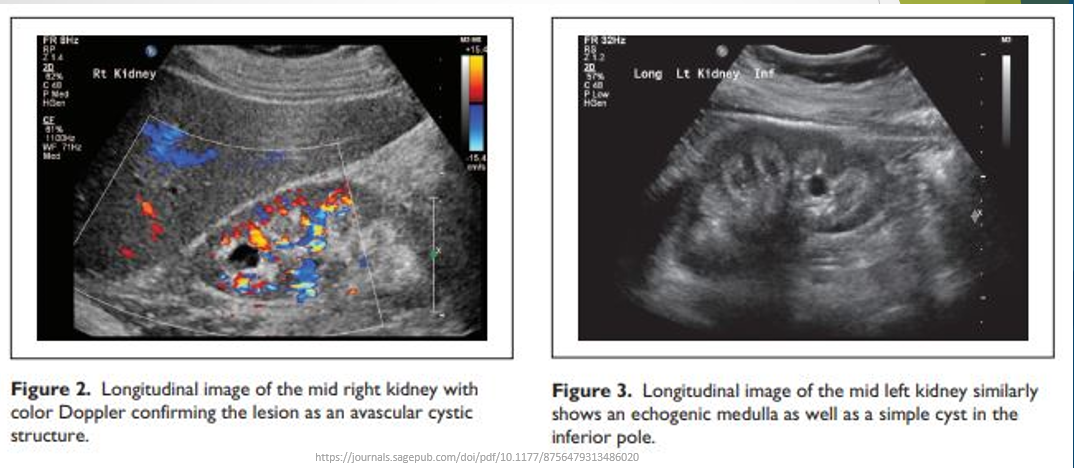
Definition: A congenital, rare, benign condition.
Characteristics: Involves dilatation of collecting tubules in renal papillae, leading to sponge-like cavitary regions in one or both kidneys; echogenic medullary pyramids.
Associated Conditions: May contain nephrocalcinosis.
Nephrocalcinosis
Definition: Increased calcium levels in the kidney.
Causes:
Hypercalcaemia due to hyperparathyroidism,
Certain medications,
Sarcoidosis,
Tuberculosis of the kidney,
AIDS-related infections,
Vitamin D toxicity.
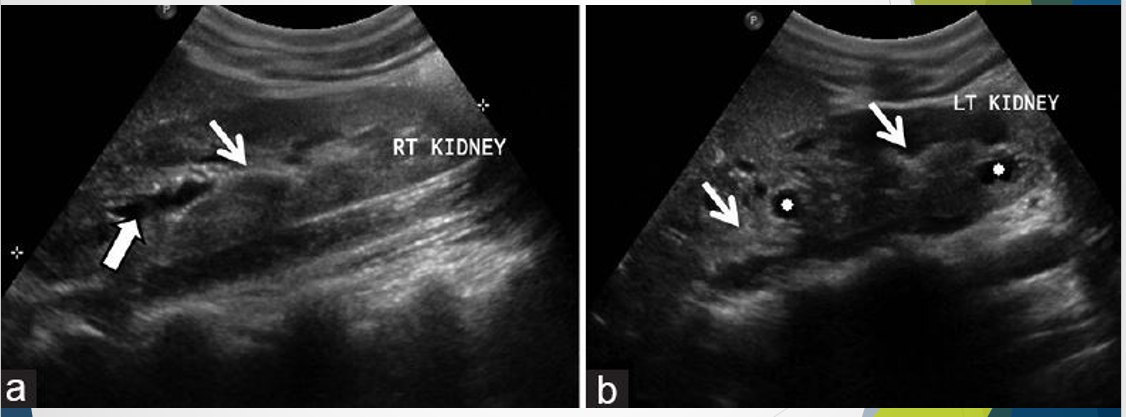
Sonographic Presentation: Calcifications primarily in the medullary pyramids with posterior shadowing dependent on the amount of calcification.
Nephrocalcinosis vs staghorn renal stone - staghorn stll has medullae on top i.e. still visible whereas as the medullae are filled with nephrocalcinosis in medullary sponge kidney


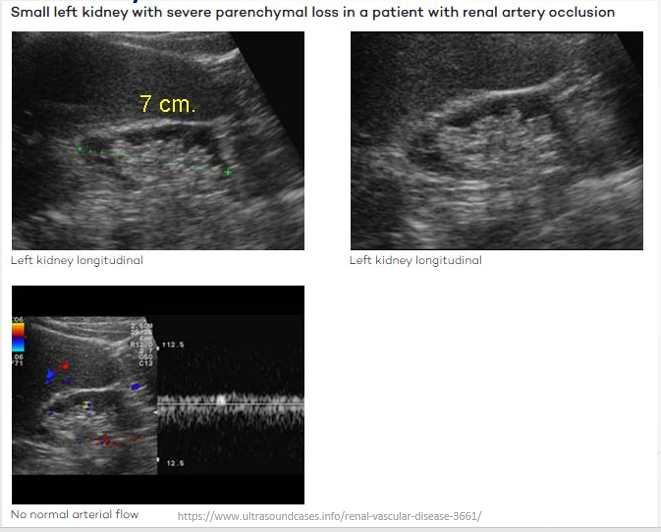
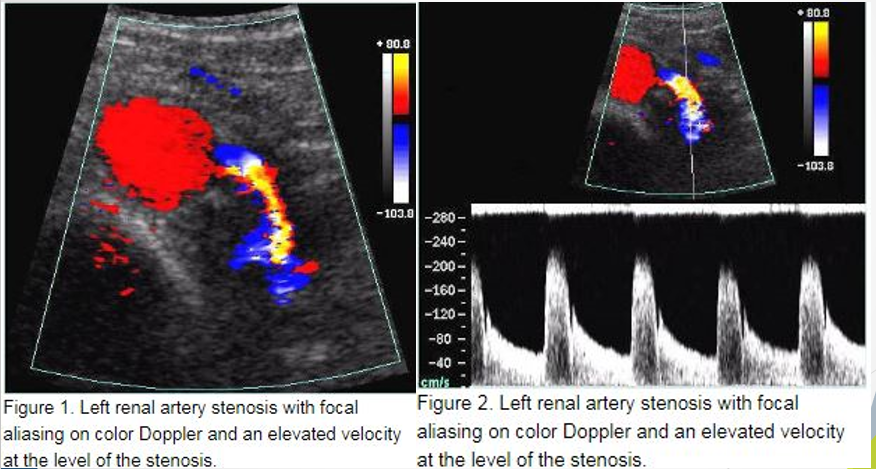
Renal Artery Stenosis (RAS)
Definition: Narrowing of the renal artery, leading to renovascular hypertension.
Causes:
Atherosclerosis (at origin),
Fibromuscular dysplasia (distally).
Clinical Presentation: Hypertension that cannot be controlled my medication
Sonographic Indicators: Stenosis visible on colour Doppler; smaller kidney on affected side; smaller parenchyma
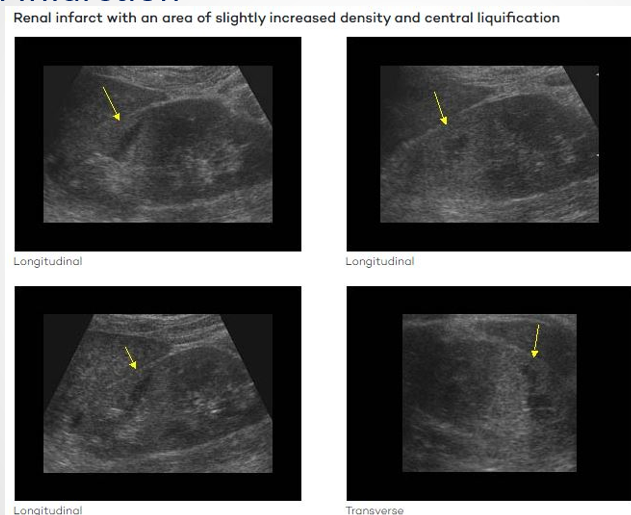
Renal Infarction
Definition: Area of the kidney with no blood flow due to thromboemboli or thrombus.
Variability: Can affect the entire kidney or just a partial area (wedge defect).
Differential Diagnosis: May mimic pyelonephritis or renal tumours.
Symptoms: Pain accompanied by nausea, vomiting, fever, hypertension.
How to differentiate between renal infarction and pyelonephritis - ask the patient if they have had a recent UTI
Obstructive Nephropathy
Definition: Renal changes due to blockage of urinary flow leading to swelling (hydronephrosis).
Causes:
Calculi (renal or bladder),
Benign prostatic hypertrophy,
Tumors (primary or secondary),
Scar tissue in ureters or urethra.
Sonographic Signs: Hydronephrosis (uni- or bilateral), altered renal arterial hemodynamic, thinning of renal parenchyma over the long-term.

Renal Transplantation
Indication: Performed when a person’s own kidneys can no longer filter blood (end-stage kidney disease).
Surgical Details: Usually utilizes the donor's left kidney; recipient's kidneys typically remain in position unless causing complications.
Sonography Requests Include: Depend on the age of the transplant for evaluation; look for size, vascular issues, leaks, or hematomas.
DON’T PUSH HARD - sitting in pelvus on patient so don’t have protection of ribs and abdominal muscles
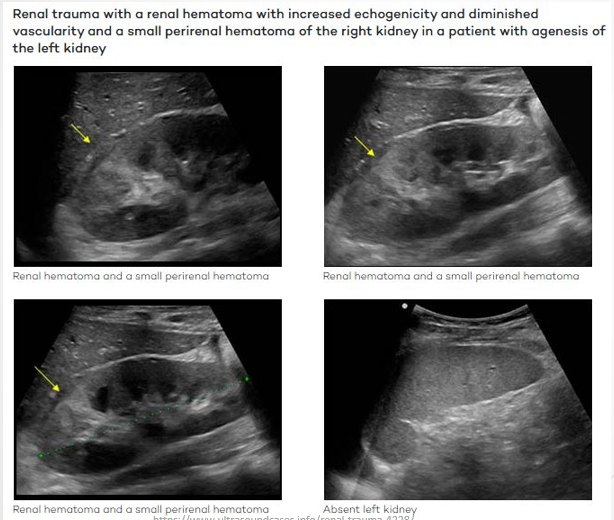
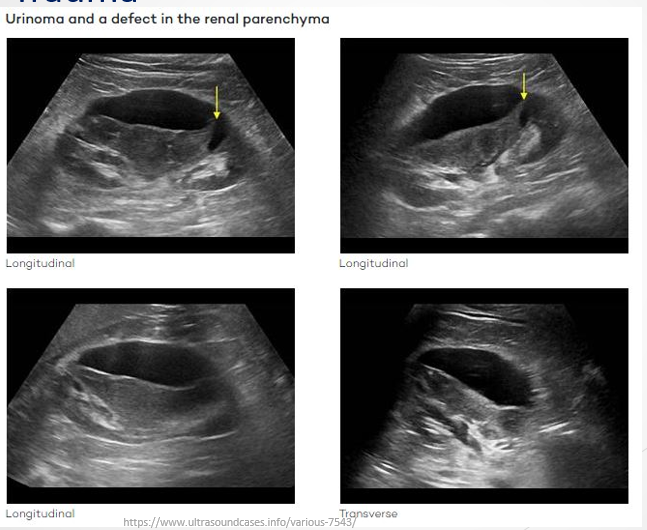
Renal Trauma
Complications: Can lead to laceration of the kidney, hematomas (perirenal or intra-kidney), and urinomas.
Imaging Findings: Evidence of lacerations; increase in echogenicity around hematomas, lack of blood flow in hematomas.
Lacerations will cause trauma so ask patient if they’ve have had recent trauma to differentiate from tumours
Review
Understanding and describing renal pathologies using sonographic terminology is essential, including differential diagnoses.
Key differentiation between nephrocalcinosis and staghorn calculus involves understanding their sonographic features.