The Immune System
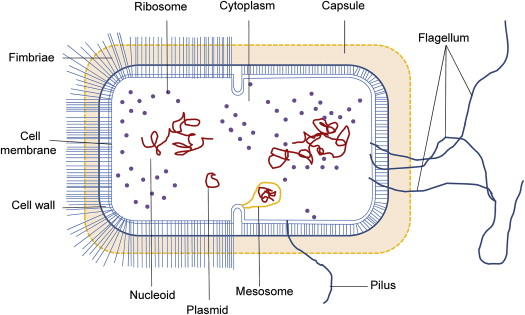

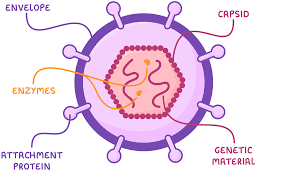
Pathogen
An enemy cell that causes damage/illness to the human body. Takes nutrients and produce toxins.
Antibodies
Clump (agglutinate) pathogens together by attaching them to their complementary antigens. This makes it easier for WBCs to phagocytosise; makes it more obvious to phagocytes (acts as a marker). The pathogens are unable to move.
They prevent pathogens from functioning / reproducing
1 antibody = 2 binding sites
Antibodies can attach to toxins to neutralise the toxin

Physical Barriers
Skin
Prevents invasion by microorganisms
Normal flora compete for microenvironments more effectively than pathogens
Produce nutrients
Resistance to colonisation by pathogens
Mucous Membrane
Found in lining of mouth, nose, vagina, eyelids
Coated with secretions that fight microorganisms
Tears
Lysozyme
Attach bacteria
Protect eyes from infection
Airways
Filter out particles in the air that are inhaled
Coated in mucus
Microbes in the air because stuck to the mucus
Cilia
Sweeps mucus up the airways; away from lungs
Digestive Tract
Stomach acid
Pancreatic enzymes
Bile
Intestinal secretions
They all either kill bacteria or stop them from multiplying
Urinary Tract
When bladder empties, it flushes out the bacteria that reach it.
Vagina
Acidic: Prevents harmful bacteria from growing
Ear Wax
Trap and preventing dust from entering ear from entering and damage the ear
Sweat
Contain antimicrobial peptides; help immune system ward off bacteria or fungi
WBC - Phagocytes
Macrophage
Moves around to remove dead cells and foreign bodies
Produce inflammatory molecules (cytokines) that activate other cells
Displays antigen and presents it to B & T Lymphocytes so that they can attack the particular pathogen
Neutrophils
Most abundant type of WBC.
Attracted to site of infection by cytokines and other microbial chemicals released by macrophages
Chemotaxis
Move towards chemical products from bacteria
Phagocytosis
Phagocytes attach themselves to the antigens of the bacteria
The phagocytes engulf the bacteria to form a phagosome
Lysosome move towards the phagosome and fuse with it
Hydrolytic enzymes released by lysosome breakdown bacteria
Soluble products from breakdown of pathogen are dissolved into the cytoplasm of the phagocyte
Antigens from the pathogen are displayed on phagocyte cell membrane
WBC - Lymphocytes
Each lymphocyte is specific and complementary against a particular antigen.
They have receptors on the outside of the cell surface membrane
Activated when they encounter their complementary antigen either on the pathogen itself or just floating about in the body.
Activation causes “clonal expansion”
Activated lymphocyte makes copies of itself through mitosis
T Cells
Helper T Cells
Capable of helping B cells divide; release cytokines to stimulate B cells to develop
Killer T Cells
Capable of killing infected cells by releasing cytotoxins (perforin)
Regulatory T Cells
Regulate immune cells (stops them from causing damage to your own cells)
Memory T Cells
Helps the response become faster when the same antigen is detected in the body again. When the same antigen is detected again, these cells trigger a quicker and stronger response by rapidly differentiating into active T cells, enabling the immune system to combat the pathogen more efficiently than during the first exposure.
B Cells
Plasma Cells
Antibody secreting cell
Memory B Cells
Readily stimulated to form plasma cells if re-exposed to the antigen at a later date
Immunity
Having correct antibodies available quickly to kill a pathogen BEFORE getting symptoms
Active Immunity
Your B Cells make the antibodies
Natural Immunity
Lymphocytes naturally make their own antibodies when pathogens invade the body
Artificial Immunity
Using vaccinations with antigens / weak form of a pathogen to stimulate antibody production
Passive Immunity
You are given the antibodies
Natural
Antibodies pass through breast milk/through placenta from mother to baby
Artificial
Antitoxins / Antibodies are injected into individuals
Active Immunity Key Facts
Exposure to antigen is needed
Takes time for protection to be developed
Long-Term protection
Memory Cells are produced
Passive Immunity Key Facts
Exposure to antigen is not needed
Protection is immediate
Short-Term protection
Memory Cells are not produced
Monoclonal Antibodies
Immunization: Mice (or other suitable animals) are immunized with an antigen that you want to produce antibodies against. This stimulates their immune system to produce specific B cells that respond to the antigen.
Cell Fusion: Spleen cells from the immunized mouse (which produce antibodies) are fused with myeloma cells (cancerous cells that can divide indefinitely) using a fusion agent such as polyethylene glycol (PEG). This results in hybridoma cells that have qualities of both cell types.
Cloning: The positive hybridomas that produce the desired antibodies are cloned to create many identical cells. This ensures a uniform antibody production.
Harvesting and Purification: The antibodies produced by the cloned hybridoma cells are harvested from the culture medium and purified to remove other proteins and components, resulting in a concentrated solution of monoclonal antibodies.
Can be used for a
Pregnancy Test
Show the location of cancer cells
Identify blood clots
Cancer Treatment
Negatives of Monoclonal Antibodies
Expensive ; Have side-effects ; long time to make them
ELISA TEST
Sample Addition: The biological sample (e.g., blood serum) is added to the wells. If the target antibodies are present in the sample, they will bind to the coated antigen to form immune complexes.
Detection Antibody Addition: A secondary antibody that is specific to the target antibodies and is usually conjugated with an enzyme or a marker is added to the wells. This detection antibody will bind to the target antibodies, forming a sandwich complex.
Substrate Addition and Measurement: A substrate that reacts with the enzyme linked to the detection antibody is added. A color change or fluorescence occurs, which is then measured. The intensity of the signal is proportional to the amount of target antibodies in the sample.
 Knowt
Knowt