ACLE
Acute Cutaneous Lupus Erythematosus (ACLE) Study Notes
Key Points
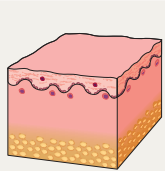
Definition: ACLE is a subtype of cutaneous lupus erythematosus characterized by transient lesions, often exacerbated by sun exposure.
Clinical Presentation:
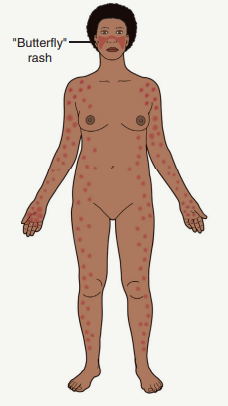
Malar Erythema: Also known as ‘butterfly rash’, the most common feature.
Lesions are usually transient and may resolve without scarring, though dyspigmentation can result.
May occur alongside oral ulcers and is frequently linked with active systemic lupus erythematosus (SLE).
Associated with anti-dsDNA antibodies and lupus nephritis.
Epidemiology
No specific epidemiological data available solely for ACLE.
SLE is more prevalent in women, particularly during childbearing years, and notably in African-American women who develop the disease earlier.
Pathogenesis
Genetic and Environmental Factors: Interaction crucial in the development of cutaneous LE, including ACLE.
Environmental Triggers:
Ultraviolet Radiation (UVR): a significant inducer of apoptosis, causing translocation of cellular and nuclear antigens.
Increases keratinocyte production of SSA/Ro52 and type I interferons (IFNs).
Cytokine Production:
Proinflammatory cytokines including TNF, IL-1, IFN-γ, HMGB1, and IL-18 are stimulated by UVR.
Enhanced IFN secretion occurs due to multiple binding interactions with immune receptors.
Cascade of Immune Response: Involves dendritic cell activation, IFN release, T cell activation, and chemokine production leading to lichenoid tissue reaction.
Rash Description and Clinical Features
Malar Erythema:
Can present with varying severity from mild erythema to pronounced edema.
Associated features can include telangiectasias, erosions, dyspigmentation, and epidermal atrophy.

Duration and Location
Lesion Duration: Ranges from hours to several weeks.
Common Locations:
Primarily affects the face, especially the malar region, while often sparing the nasolabial folds.
Can also spread to the hands avoiding the knuckles.
Oral ulcerations frequently occur.
Association with SLE: Active systemic disease often correlates with ACLE.
Rowell Syndrome: May present with erythema multiforme-like lesions in lupus patients. Rare severe presentations can resemble toxic epidermal necrolysis.
Diagnostic Criteria
Per 2019 EULAR/ACR classification, acute cutaneous lupus is a clinical criterion with a weight of 2.
The 2012 SLICC classification recognizes several types of rashes characteristic of lupus as diagnostic criteria.
Diagnosis and Investigations
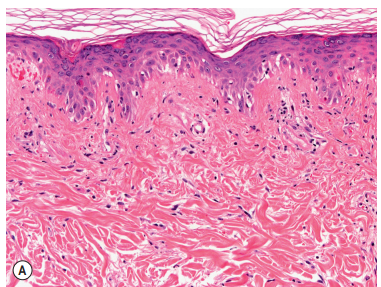
Lesional Biopsy:
Histopathology: Shows mild interface dermatitis with vacuolization of basal keratinocytes and sparse superficial lymphoid infiltrates.
Direct immunofluorescence may reveal granular deposits of IgG and/or IgM in lesions.
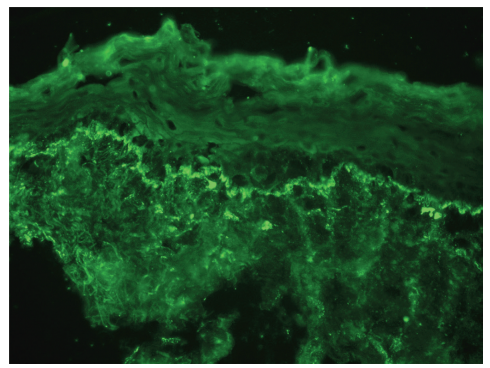
Systemic Evaluation: Important to assess if systemic lupus is present, utilizing patient history, physical exams, and specific lab tests (e.g., ANA profile, urinalysis, CBC).
Differential Diagnosis
Conditions to consider:
Rosacea (including corticosteroid-induced)
Seborrheic dermatitis
Sunburn
Drug-induced photosensitivity
Dermatomyositis
Erysipelas
Pemphigus types
Various dermatitis forms (atopic, contact)
Treatment/Management
Topical Therapy: Corticosteroids are pivotal for symptom management.
Systemic Therapy: Antimalarials like hydroxychloroquine are the gold standard.
Adjunctive Therapy: Emphasis on sun protection and smoking cessation.
Complications
Possible complications include:
Dyspigmentation.
Progression to systemic lupus erythematosus (SLE).
In very rare cases, severe reactions resembling toxic epidermal necrolysis can occur.
Additional Notes
The presence of telangiectasias, erosions, dyspigmentation, and epidermal atrophy aids in differentiating ACLE's malar erythema from other facial rashes.
Note that the three main types of cutaneous LE (ACLE, SCLE, DLE) can coexist in patients.