Topic 12- Reproduction I (Male)
Outcomes:
• sequence animal reproduction
• compare and contrast types of animal reproduction
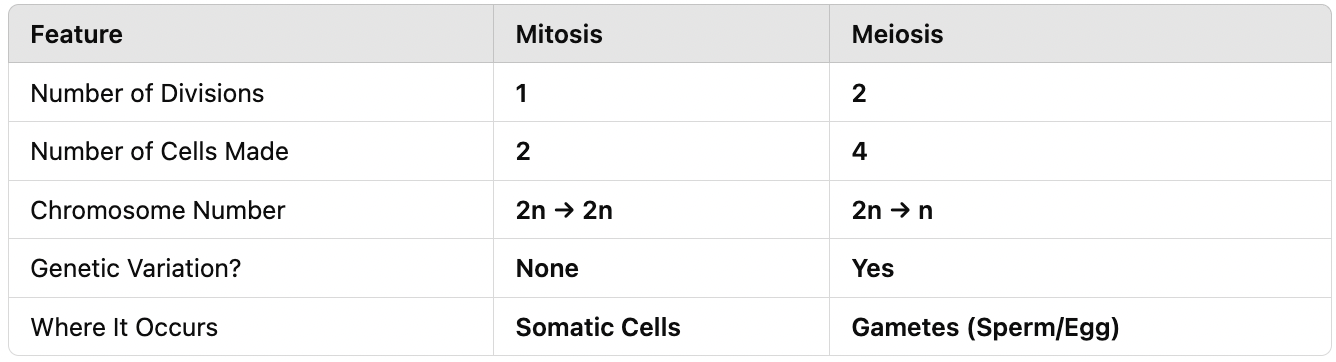
• sequence mitosis and meiosis
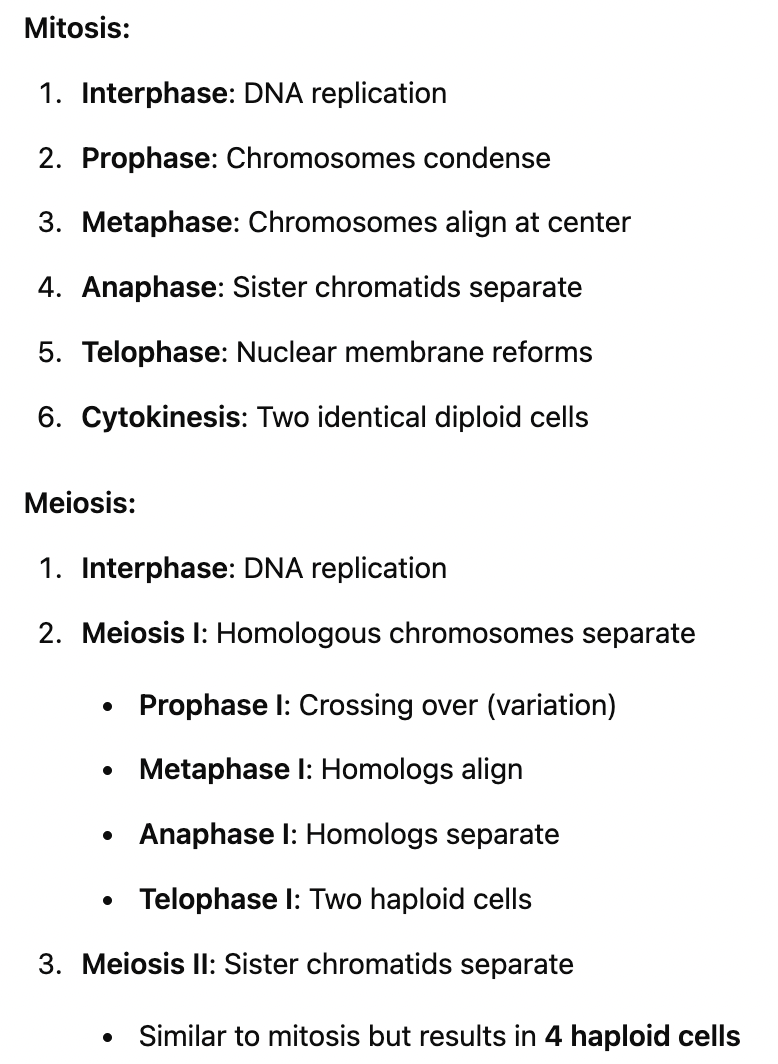
• compare and contrast mitosis and meiosis
• compare and contrast male reproductive structures
• sequence spermatogenesis
• hypothesize and diagnose the impact of variability on spermatogenesis
• sequence male reproductive endocrinology
• hypothesize and diagnose the impact of variability on male reproductive endocrinology

I. Introduction to Animal Reproduction
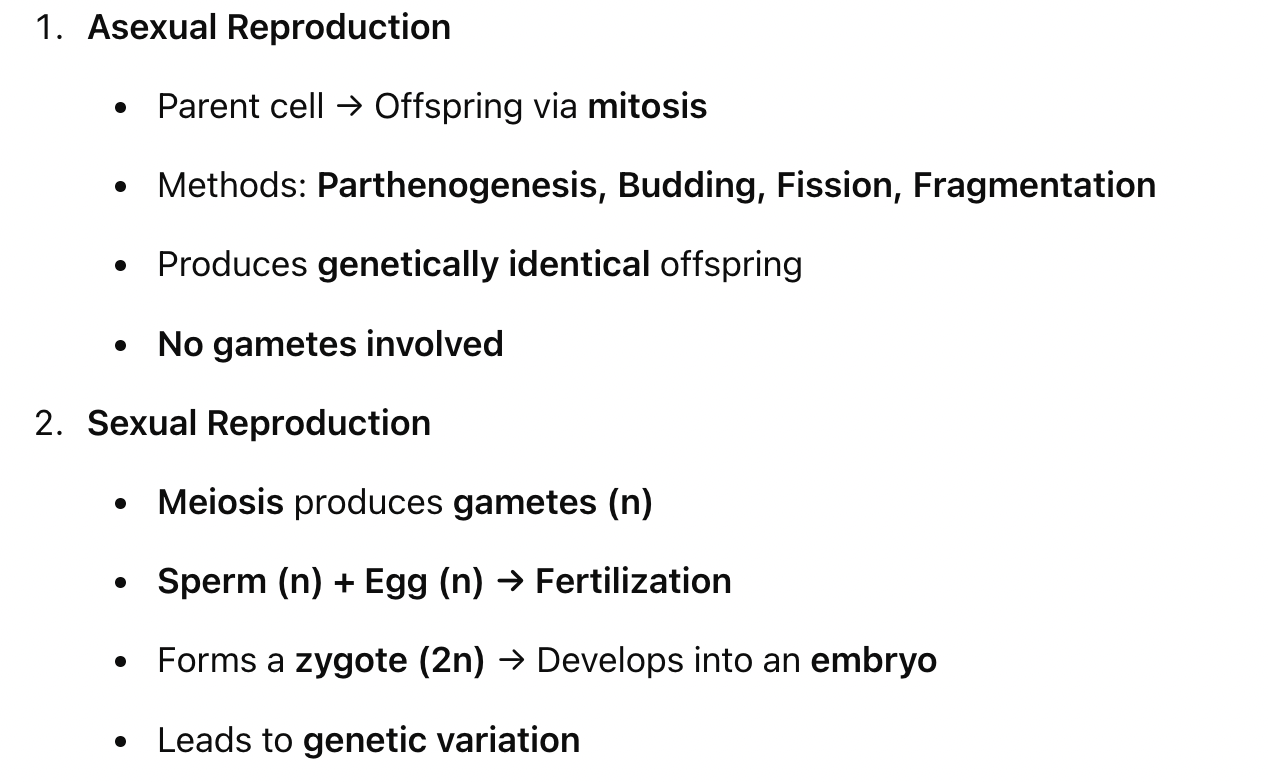
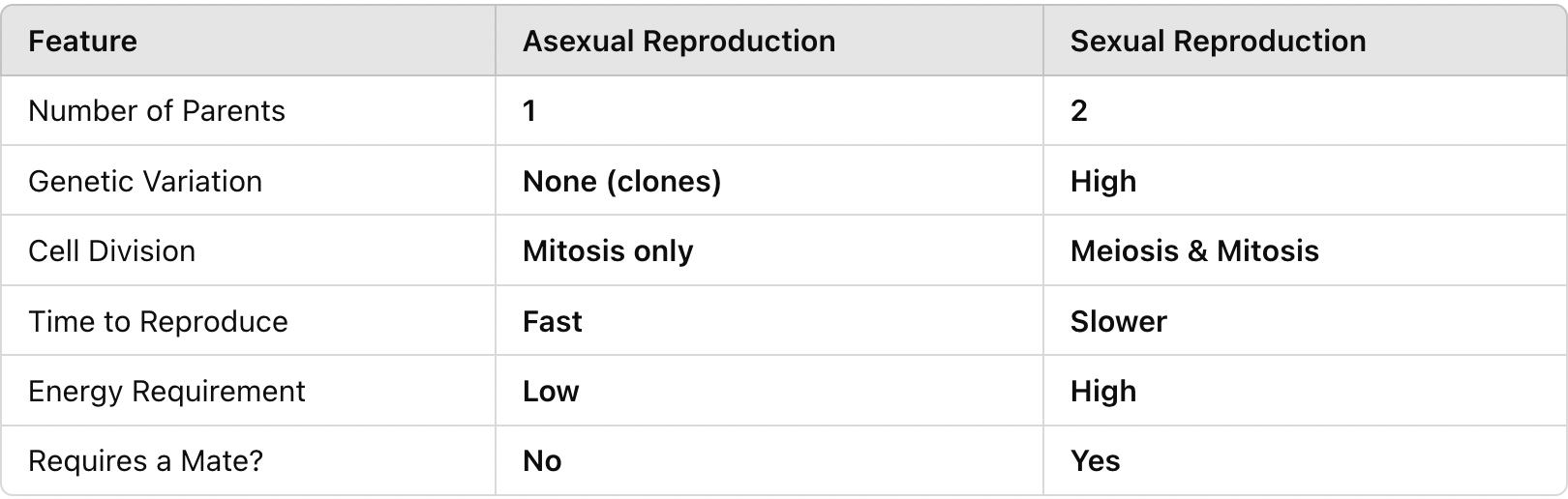
A. Asexual Reproduction
Single parent → 100% of genes passed on.
Mitosis only, no gametes involved.
Mechanisms of Asexual Reproduction
Parthenogenesis:
Diploid eggs develop into an organism without fertilization.
Offspring are genetically identical to the mother.
Budding, fission, fragmentation:
Offspring produced via mitosis.
Advantages of Asexual Reproduction
Rapid reproduction.
No need for a mate.
100% of genes are passed on.
B. Sexual Reproduction
Meiosis → Gametes (n)
Sperm: Small, motile, flagellated.
Egg: Large, non-motile, rich in nutrients.
Fertilization:
Sperm meets egg → Forms a zygote (2n) → Develops into an embryo.
Advantages of Sexual Reproduction
Genetic variation.
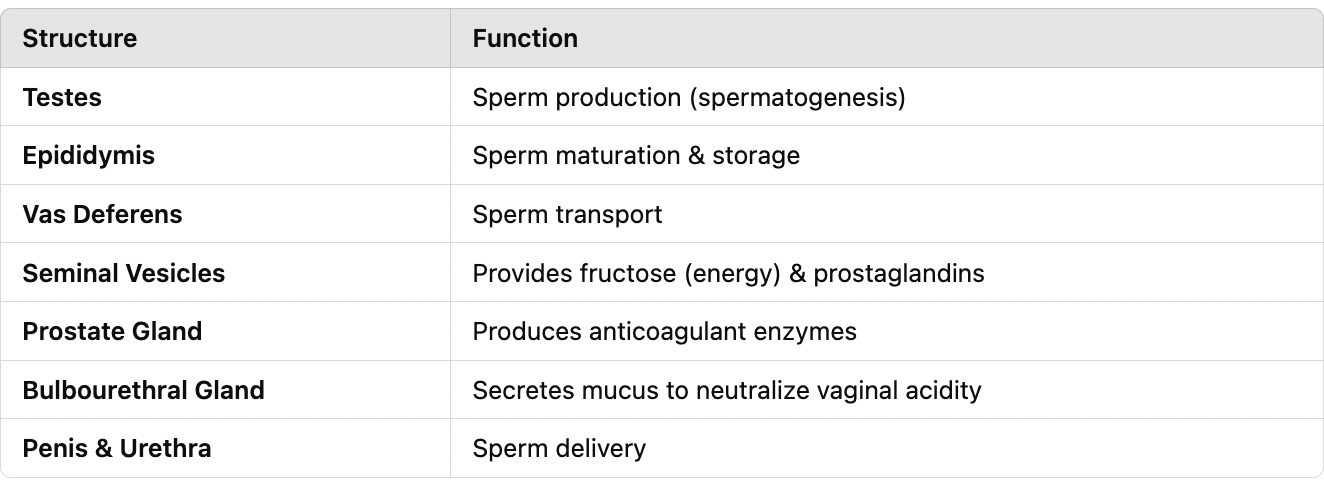
II. Male Reproductive System
A. Introduction
Functions: Produces and delivers sperm.
Sperm pathway ("SEVEn UP"):
Seminiferous tubules (testes) → Epididymis → Vas deferens → Ejaculatory duct → Urethra → Penis → Exit from body.
B. Testes
Male gonads located in the scrotum.
Seminiferous tubules:
Site of spermatogenesis (sperm production via meiosis).
Types of Cells in Seminiferous Tubules
Spermatocytes: Undergo meiosis.
Sertoli cells:
Support sperm development.
Secrete inhibin (regulates FSH for sperm count control).
Secrete androgen-binding protein (ABP) (binds & transports testosterone).
Negative feedback mechanism.
Leydig cells:
Located between seminiferous tubules.
Produce testosterone.
C. Epididymis
Coiled duct in testes responsible for:
Sperm transport.
Sperm maturation (takes ~3 weeks).
Sperm storage.
D. Scrotum
Surrounds testes and epididymis.
Functions:
Cooling (1-2°C below body temperature).
Increases sperm longevity.
E. Penis
Function: Delivers sperm to the female reproductive tract.
Internal Structure
Urethra: Runs through the middle, pathway for sperm and urine.
Erectile tissue:
Three parallel columns.
Engorge with blood during an erection.
Erection Mechanism
Sexual stimulation → Nitric oxide (NO) released from endothelial cells.
Smooth muscle relaxation → Arteries dilate and veins compress → Increased blood flow → Erection.
F. Accessory Glands
Produce semen (fluid that carries sperm).
Seminal Vesicles (~60% of semen volume)
Secretes into vas deferens.
Contains:
Fructose (energy for sperm).
Prostaglandins (stimulate uterine contractions to help sperm reach the egg).
Prostate Gland
Secretes into urethra.
Produces:
Anticoagulant enzyme (prevents semen clotting).
Citrate (nutrient for sperm).
Bulbourethral Glands (Cowper’s glands)
2 glands, one on each side of the urethra.
Secretes:
Mucus (lubricates and neutralizes vaginal acidity).
Some sperm can be caught in this secretion.
G. Sperm Pathway
Sexual stimulation → NO release → Erectile tissue engorges.
Sperm leaves epididymis → Enters vas deferens.
Vas deferens loops over the bladder → Passes by seminal vesicles.
Path becomes the ejaculatory duct → Passes through prostate gland.
Ejaculatory duct meets urethra → Passes by Bulbourethral glands.
Sperm exits through the urethra and is ejaculated out of the penis.
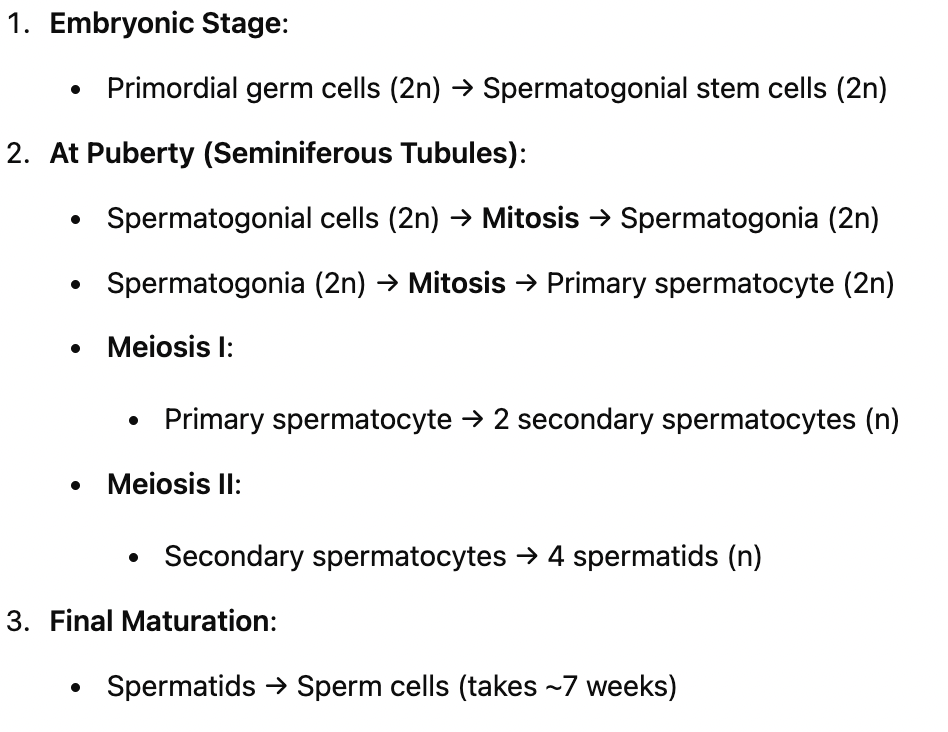
III. Spermatogenesis (Meiosis)
A. Process of Spermatogenesis
Occurs throughout adult lifetime.
Takes place in the testes.
Regulated by hormones.
Developmental Stages
Embryonic Stage:
Primordial germ cells (2n) → Differentiate into spermatogonial stem cells (2n).
At Puberty (In seminiferous tubules/testes):
Spermatogonial cells (2n) undergo mitosis → Produce spermatogonia (2n).
Spermatogonia (2n) undergo mitosis → Forms 1 primary spermatocyte (2n) & 1 spermatogonia cell (2n).
Primary spermatocyte (2n) undergoes meiosis:
Meiosis I → 2 secondary spermatocytes (n).
Meiosis II → 4 spermatids (n).
Spermatids differentiate into mature sperm cells (spermatozoa).
B. Structure of a Sperm Cell
Takes ~7 weeks to mature.
Only the nucleus enters the egg during fertilization.
Parts of the Sperm Cell
Head:
Contains DNA (nucleus).
Acrosome: Contains enzymes to penetrate the egg.
Midpiece:
Contains mitochondria (produces ATP for motility).
Tail:
Flagellum (propels the sperm).
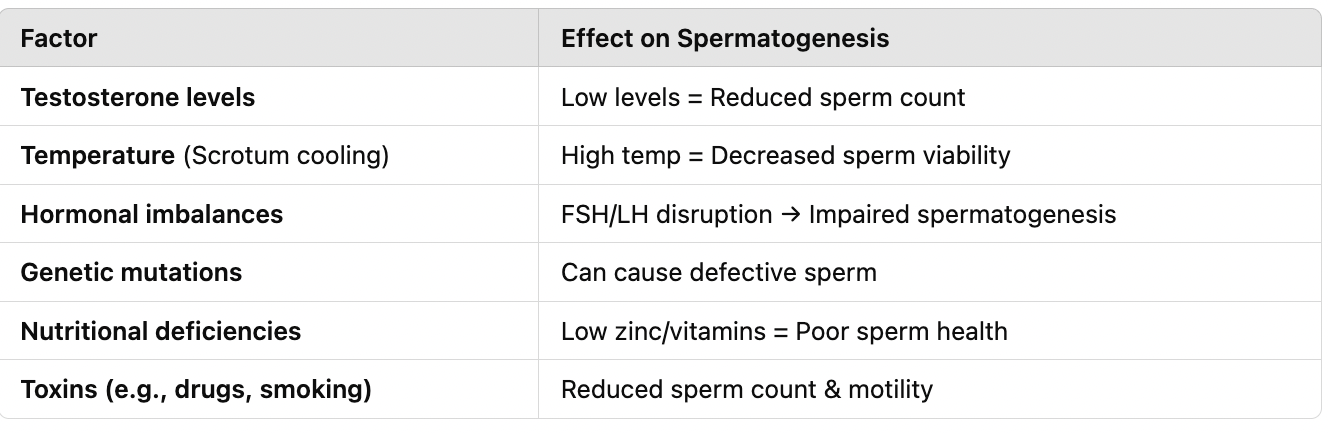
IV. Male Endocrinology
A. Androgens (Male Sex Hormones)
Testosterone:
Supports spermatogenesis.
Triggers puberty & secondary sex characteristics.
Low levels → Infertility (< 15 million sperm/ml).
All chordates have a hypothalamus and pituitary gland for hormonal regulation.
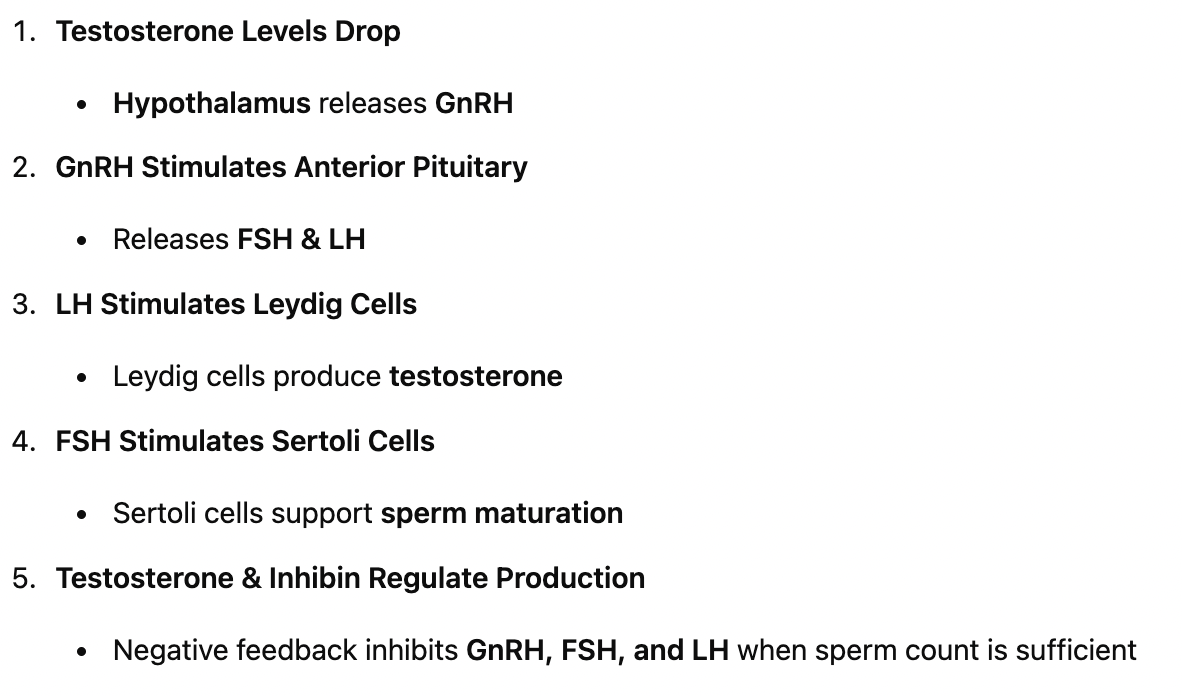
B. Hormonal Signaling Pathways
Testosterone levels drop → Hypothalamus secretes GnRH (Gonadotropin-releasing hormone).
GnRH signals the anterior pituitary → Releases FSH & LH.
Roles of FSH & LH
FSH (Follicle-Stimulating Hormone):
Stimulates Sertoli cells → Supports sperm maturation.
LH (Luteinizing Hormone):
Stimulates Leydig cells → Produces testosterone.