Topic 13- Reproduction II (Female)
Outcomes:
• compare and contrast female reproductive structures
• sequence oogenesis
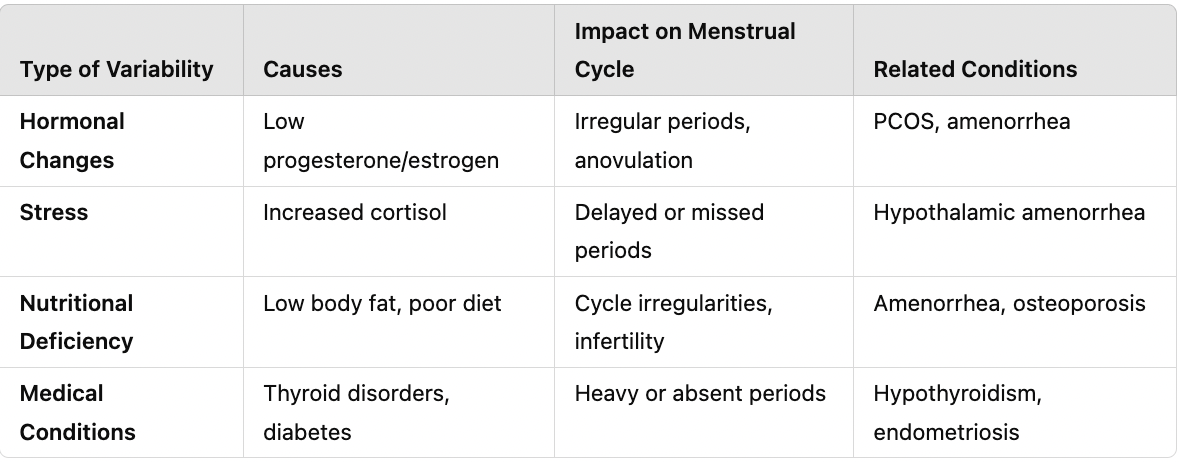
• hypothesize and diagnose the impact of variability on oogenesis
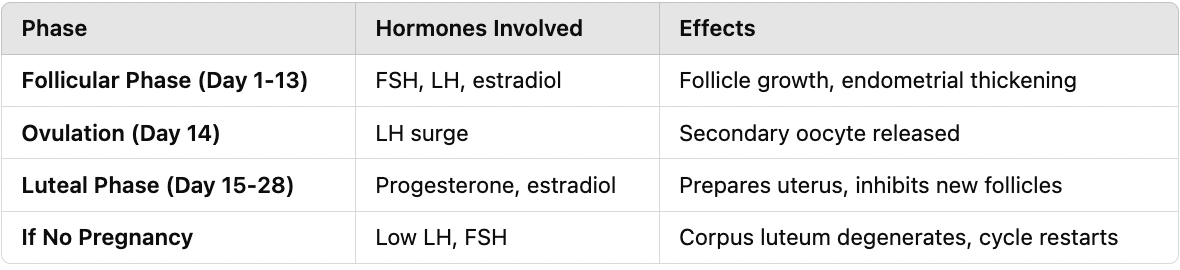
• sequence the menstrual cycle
• hypothesize and diagnose the impact of variability on the menstrual cycle
• sequence female endocrinology
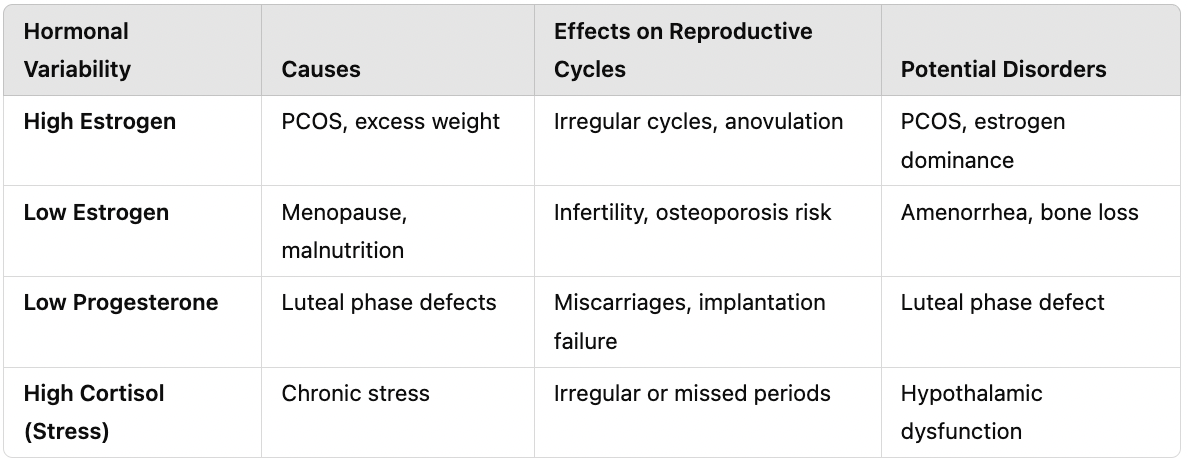
• hypothesize and diagnose the impact of variability on female endocrinology and reproductive cycles
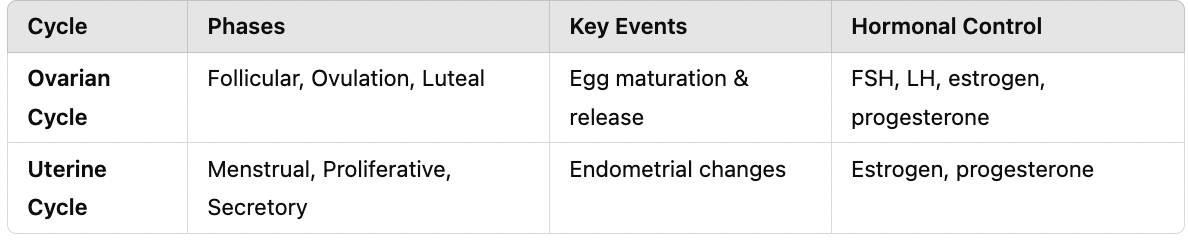
• compare and contrast ovarian and uterine cycles
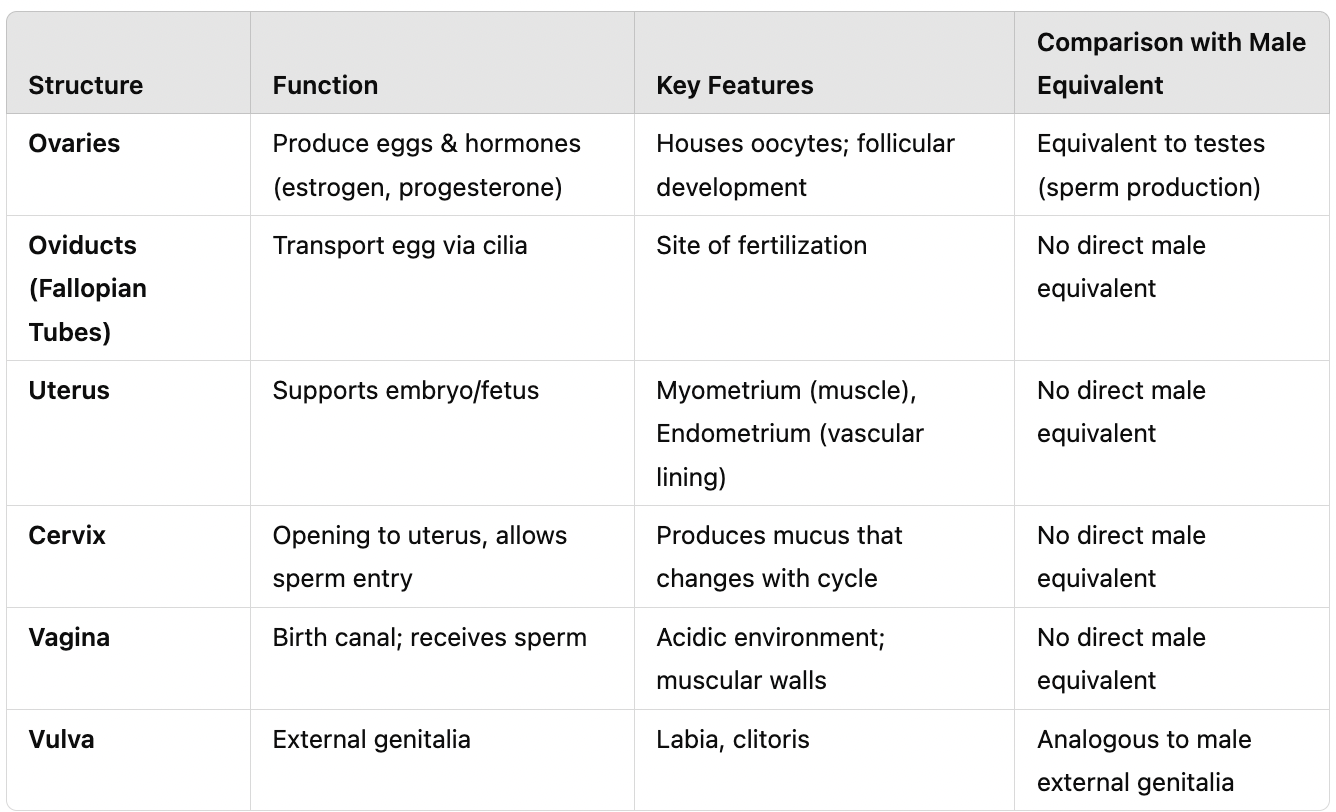
I. Female Reproductive System
A. Functions
Egg production
Receives penis and sperm
Nourishes embryo
Lactation (milk production)
B. Anatomy
Ovary:
Female gonads that house oocytes
Secretes estradiol and progesterone
Follicles:
Structures where eggs mature
Contains multiple developing oocytes
Oocyte:
Cell that undergoes meiosis to form an egg
Oviducts (Fallopian tubes):
Transport secondary oocyte via cilia
Uterus (Womb):
Myometrium: Smooth muscle that contracts during labor
Endometrium: Lining with blood vessels, glands, and tissues
Cervix:
Narrow opening at the bottom of the uterus
Vagina:
Birth canal
Vulva:
External genitalia
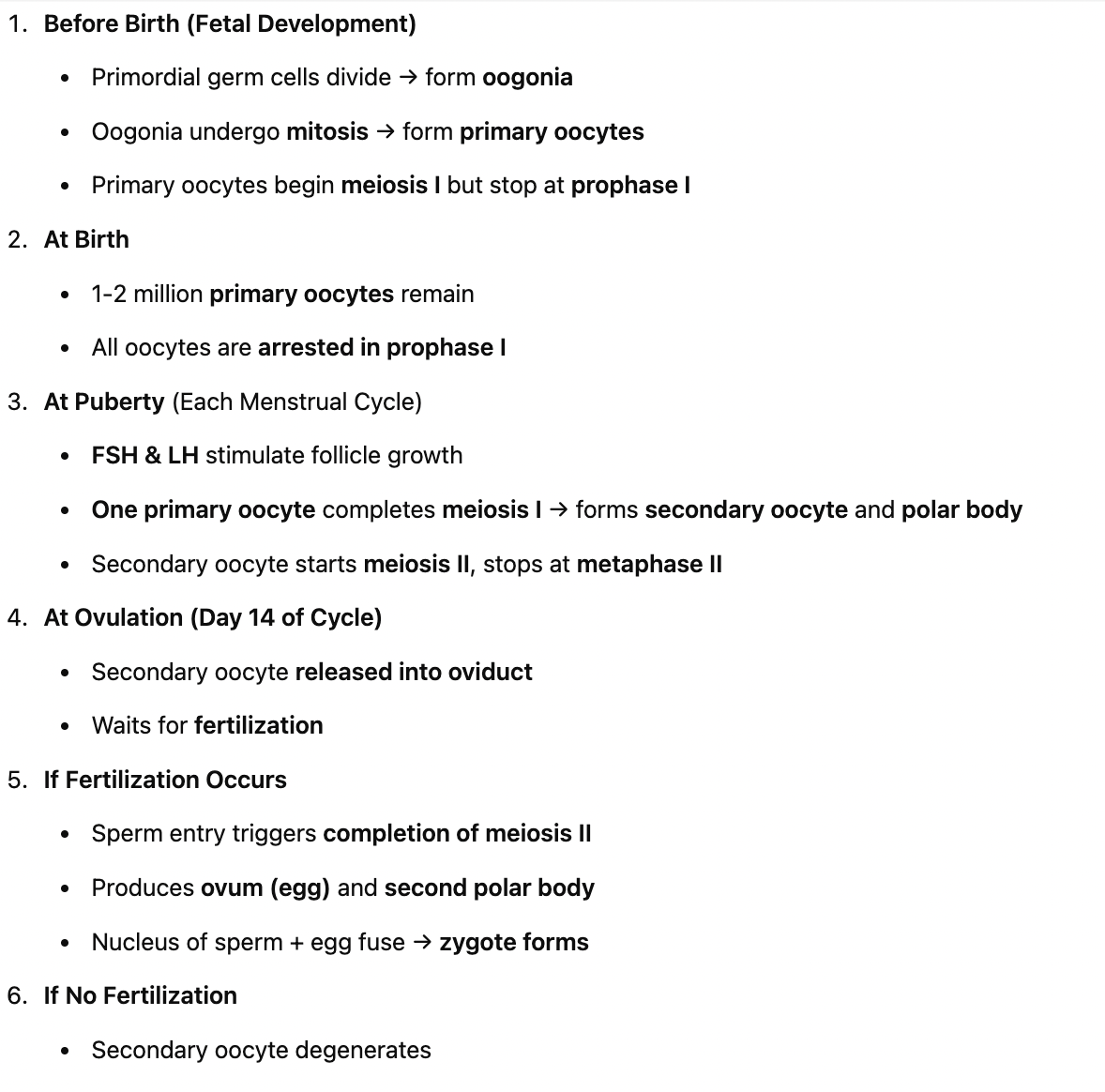
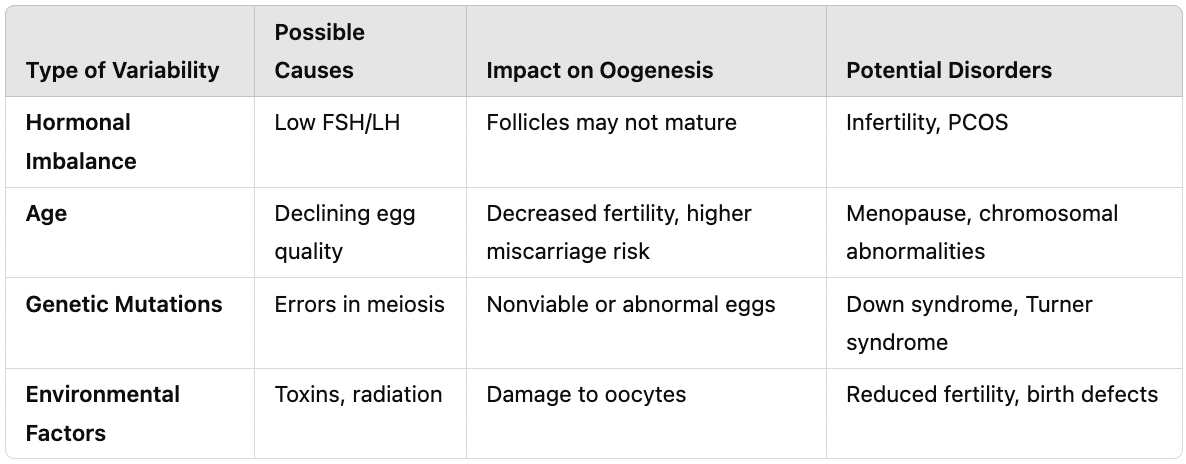
II. Oogenesis (Egg Development)
A. Meiosis Review
2n cell → 4 haploid cells
In oogenesis, only one egg is produced; the others become polar bodies
B. Prior to Puberty
In the embryonic ovary, primordial germ cells divide → form oogonia
Primary oocytes begin meiosis I but stop at prophase I
At birth:
1-2 million primary oocytes exist, but only 200,000 remain at puberty
Each oocyte is housed in a follicle
Follicle cells provide protection
Zona pellucida (glycoprotein layer) surrounds the oocyte
At puberty:
Each month, 6-12 follicles begin to mature, but only one completes development
C. During and After Puberty
At puberty, estrogen levels rise
Primary oocyte completes meiosis I, forming:
Secondary oocyte (haploid)
First polar body (degenerates)
The secondary oocyte begins meiosis II, stopping at metaphase II → it is ovulated
Ovulation:
Secondary oocyte is released, surrounded by zona pellucida and follicle cells
Moves into the oviduct
Remains in metaphase II until fertilized
D. After Ovulation
In the ovary, the remaining follicle becomes the corpus luteum (temporary endocrine gland)
Corpus luteum secretes estrogens and progesterone
Prepares for pregnancy and prevents another egg from releasing
If no fertilization occurs, the secondary oocyte degenerates
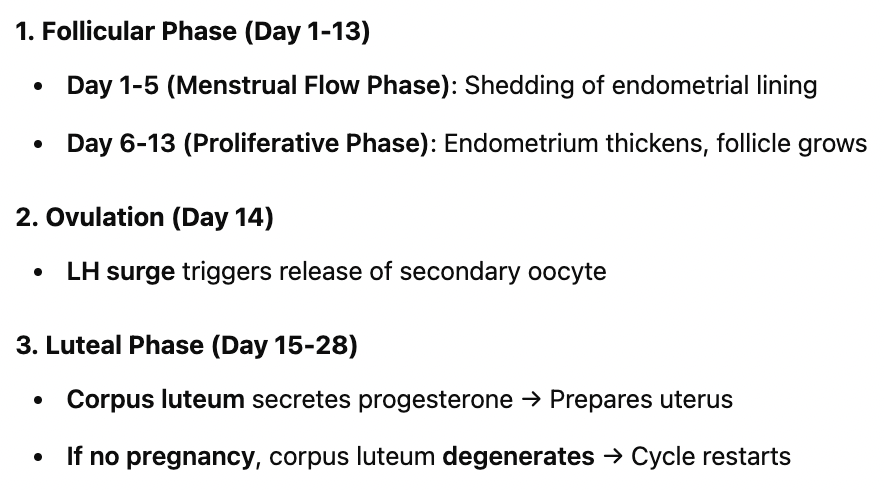
III. Menstrual Cycle
A. Overview
Unique to humans and primates
Controls ovulation and endometrial thickening
Prepares for pregnancy
B. Components of the Menstrual Cycle
Hormonal regulation:
Hypothalamus releases GnRH → stimulates the anterior pituitary
Anterior pituitary releases:
LH (Luteinizing Hormone)
FSH (Follicle-Stimulating Hormone)
28-Day Cycle:
Ovarian Cycle:
Follicular phase → Ovulation → Luteal phase
Uterine Cycle:
Menstrual flow → Proliferative phase → Secretory phase
IV. Female Endocrinology
A. Female Sex Hormones
Ovaries respond to FSH and LH by secreting:
Estrogen (Estradiol)
Secreted by follicle cells and corpus luteum
Stimulates endometrial growth
Develops secondary sex characteristics
Progesterone
Secreted by the corpus luteum
Prepares uterine lining
Maintains pregnancy
Hormonal Regulation:
High estradiol, low progesterone → Stimulates hypothalamus
High estradiol, high progesterone → Inhibits hypothalamus
B. Ovarian Cycle (28 Days)
1. Early Follicular Phase (Day 1-5)
FSH and LH released from anterior pituitary
Follicle cells secrete low estradiol
Negative feedback: Low estradiol & progesterone inhibit the anterior pituitary
2. Late Follicular Phase (Day 5-13)
Follicles grow, increasing estradiol but keeping progesterone low
Positive feedback: High estradiol stimulates the hypothalamus
LH surge occurs on Day 13
3. Ovulation (Day 14)
1 day after LH surge, ovulation occurs
High estradiol, low progesterone → increases GnRH → triggers LH and FSH release
4. Luteal Phase (Day 15-28)
Follicle tissue transforms into the corpus luteum
Secretes progesterone and estradiol
Negative feedback: Inhibits the hypothalamus to prevent another egg release
If no pregnancy occurs:
Low LH and FSH trigger corpus luteum degeneration
Estradiol and progesterone levels drop → Cycle restarts at Day 1
V. Uterine Cycle (Menstrual Cycle)
A. Menstrual Flow Phase (Day 1-5)
Endometrial lining sheds → menstruation begins
New follicles begin to grow
Negative feedback on hypothalamus
B. Proliferative Phase (Day 6-13)
Uterus prepares for embryo implantation
High estradiol levels → Endometrial lining thickens (positive feedback)
Ovulation occurs on Day 14
C. Secretory Phase (Day 15-28)
Corpus luteum secretes high estradiol & progesterone
Endometrial glands secrete nutrients to sustain an early embryo
If no pregnancy occurs:
Hormone levels drop
Endometrial lining disintegrates → Cycle restarts
 Knowt
Knowt