Lactation, Milk, and Nutrition
Week 1 January 6
Lecture 1 1-10: outcomes
1. Describe why there is a need for optimal infant and young child feeding all around the world.
Describe the particular problems that developing countries may face in regards to optimal infant and young child feeding.
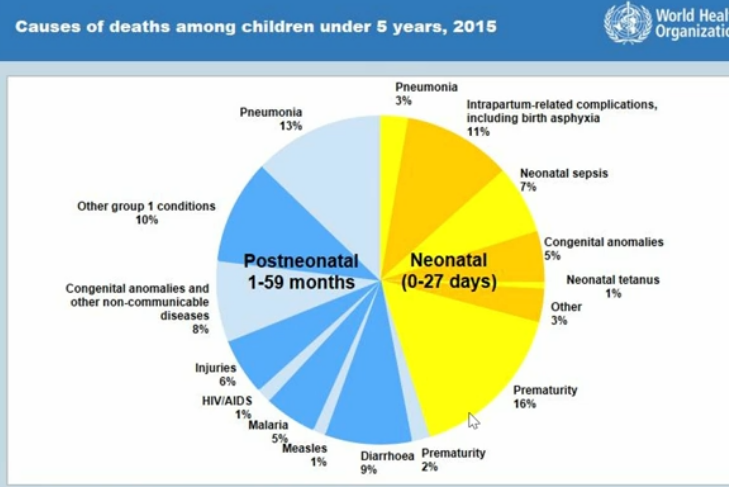
Identify the top FOUR causes of death of children younger than five years of age.
Define the WHO and UNICEF recommended infant and young child feeding practices.
Define exclusive breastfeeding.
Define complementary feeding.
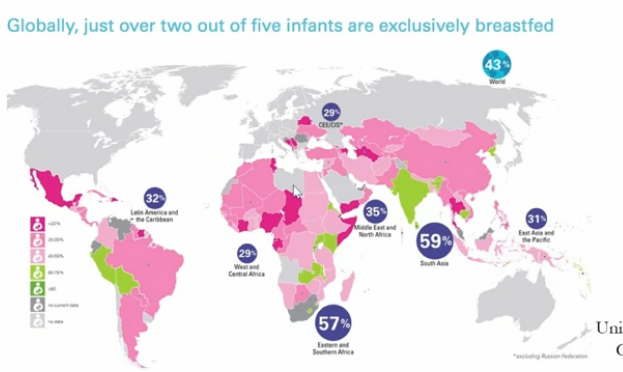
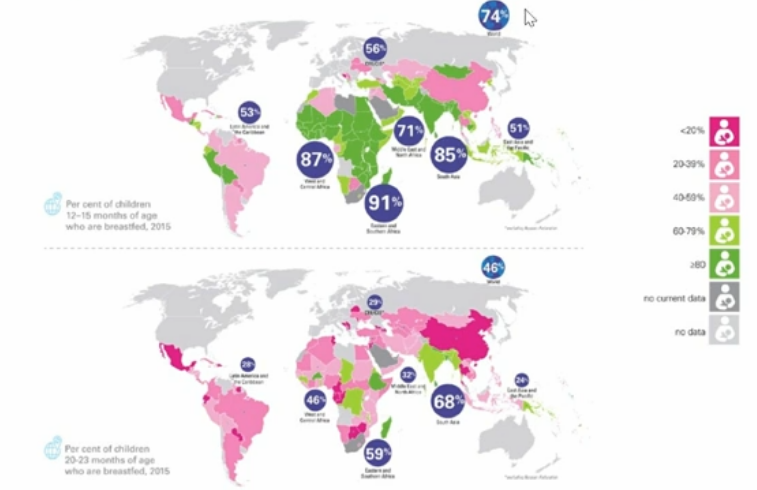
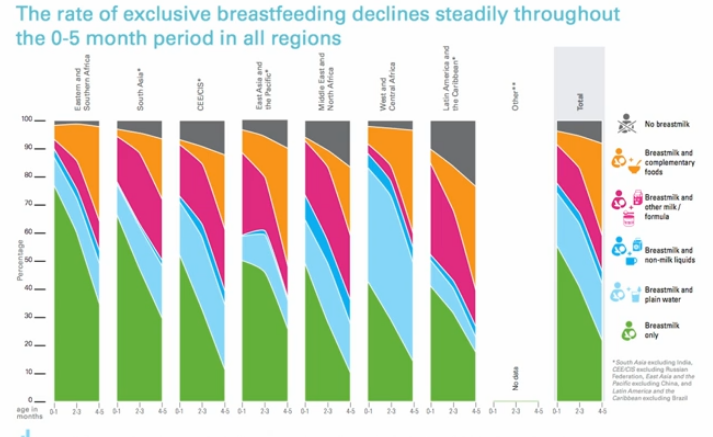
Describe the current global breastfeeding status.
List the conditions which children and mothers may have an increased risk of if breastfeeding does not occur.
Describe the benefits of breastfeeding for the infant and the mother.
Evaluate whether or not a woman may be at an increased risk of becoming pregnant by using the Lactational Amenorrhea Method of birth control.
Describe the socioecological model of breastfeeding support.
List the 8 MDG's and describe how breastfeeding helps to achieve each one.
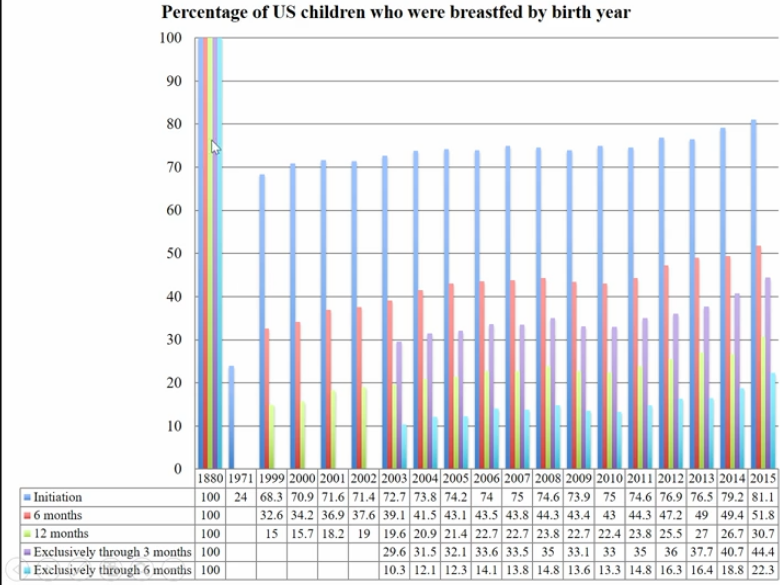
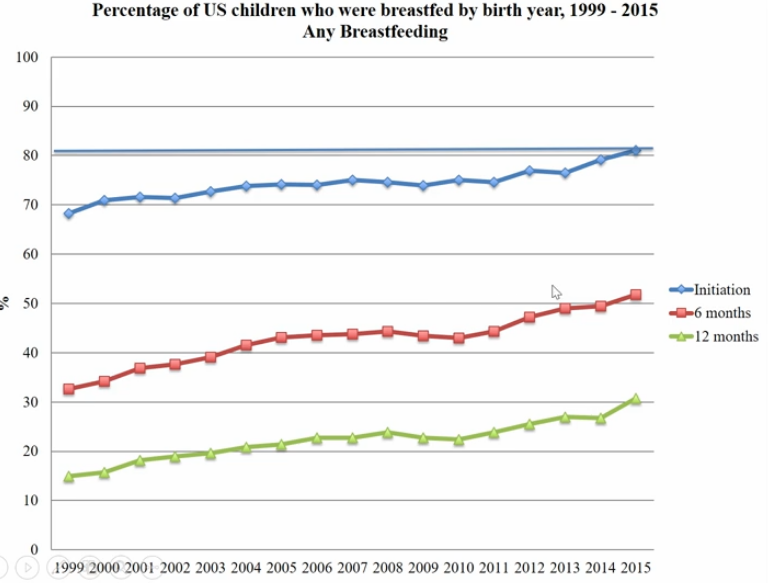
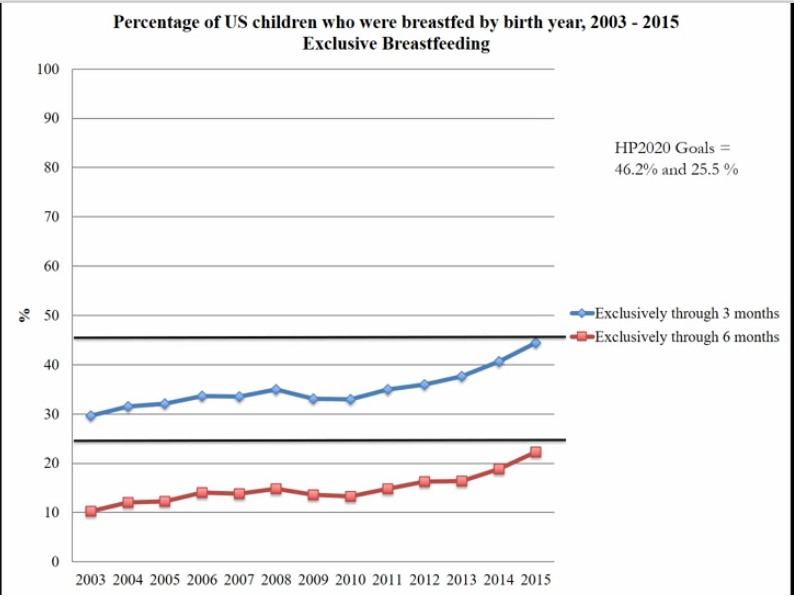
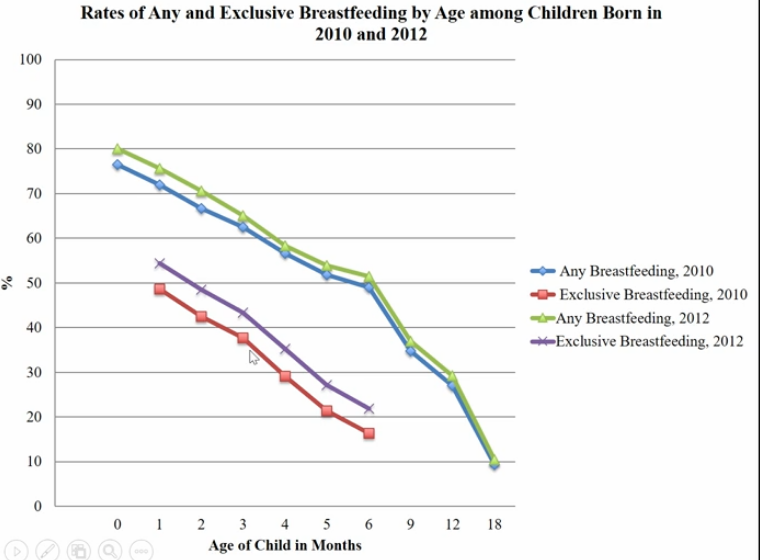
Describe the general breastfeeding trends (you will not be asked specific statistics).
Identify campaigns that are intended to help support breastfeeding.
Describe the economic benefits of breastfeeding.
Describe the mechanisms by which breastfeeding can impact: obesity, cholesterol, type two diabetes, blood pressure, and IQ scores later in life.
Lecture 2 1-12: Why Breastfeed?
optimal infant and young child feeding practices
most effective interventions to improve child health
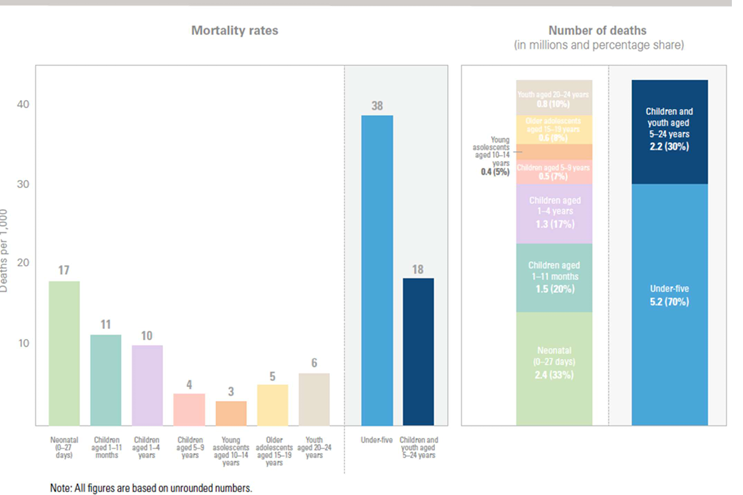
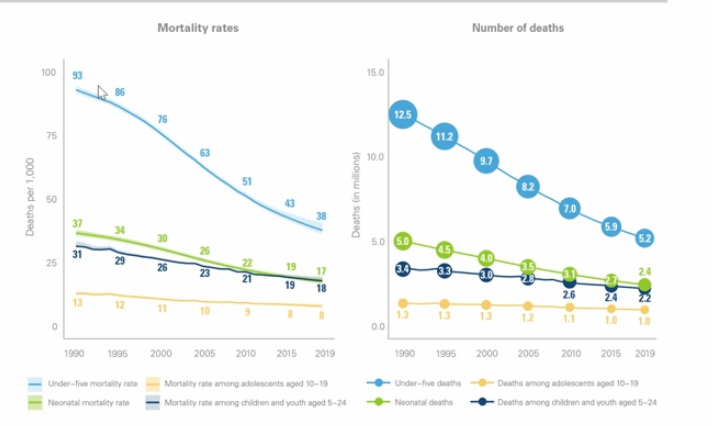
in 2019 an estimated 5.2 million children dies before their fifth birthday (60% decrease from 1990)
¾ of these deaths (3.9 million) occurred in the first year of life
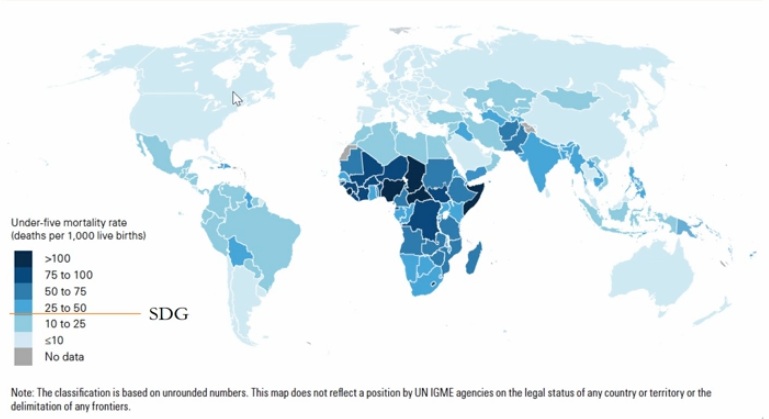
developed countries have lower infant mortality
the US averages around 3 per 1000
NC is about 6 per 1000
What do you think are leading cases of infant mortality
globally the top causes of infant death in 2010 (NIH)
neonatal encephalopathy, or problems with brain function after birth, neonatal encephalopathy usually results from birth trauma or a lack of O2 to baby during birth
infections, especially blood infections
complications of preterm birth
lower respiratory infections ( ie flu or pneumonia)
diarrheal disease
globally (WHO)
infectious disease including pneumonia, diarrhea and malaria along with preterm birth complications, birth asphyxia and trauma and congenital anomalies remain
the most common cause of death in the US in 2011 were the following (NIH)
birth defects
preterm birth and low birth weight
sudden infant death syndrome (SIDS)
pregnancy complications
accidents
the mother’s perspective
exclusive breastfeeding can
delay the return of fertility
accelerate recovery of pre-pregnancy
mothers who breastfeed exclusively and frequently have less that 2% risk of becoming pregnant in the first 6 months postpartum, provided that they still have amenorrhea
need for optimal infant and younf child feeding
under-nutrition is associated with at least 45% of child deaths
about 26% of children <5 years of age in developing countries are stunted and 7.5% wasted
suboptimal breastfeeding in the first year of life, results in
1.4 million deaths and 10% of disease burden in children less than 5 years old
recommended infant and young child feeding practices
WHO and UNICEF’s
exculsive breastfeeding for 6 months
nutritionally adequate and safe complementary feedong start from the age of 6 months with continoued breastfeeding up to 2 years of age or beyond
the child will have more antibodies and calores
feeding definitions
exclusive breastfeeding
an infant receives only breast milk from his or her mother or wet nurse, or expressed breast milk, and no other liquids or solids, not even water, with the exception of oral rehydration solution, drops or syrups consisting of vitamins, minerals supplements or medicines
complementary feeding
the process starting when human milk is no longer sufficient to meet the nutritional requirements of infants
other food and liquids are needed, along with human milk
the target range for complementary feeding is generally taken to be 6-23 months of age
breastfeeding may continue beyond 2 years
what breastfeed for 2 years or beyond
for the child, not breastfeeding association woth increased risk of
diarrehea
pneumonia
ear infections
meningitis
urinary tract infections
asthma
type 1 diabetes
celiac disease
ulcerative colitis
childhood leukemia
obesity in childhood and adolescence
increased risked of heart disease later in life
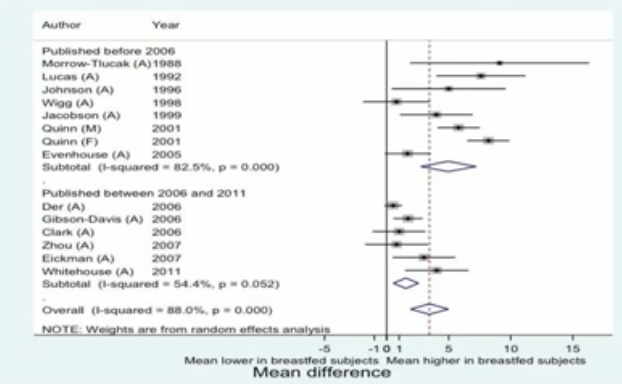
about 4 numbers lower IQ score
for the mother, not breastfeeding her infant is associated with increased risk of
postpartum hemorrhage
breast cancer
ovarian cancer
developing countries
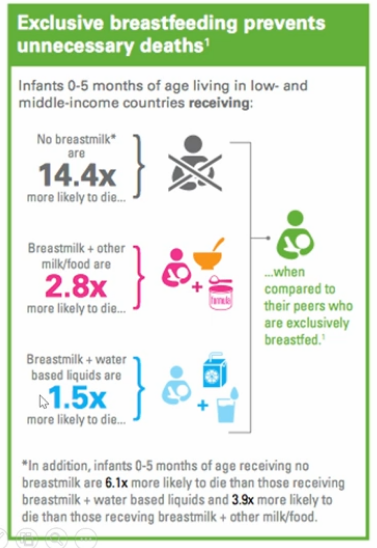
infants not breastfed are 6-10x more likely to die in the first months of life
complementary feeding
stating around 6 months of age the infants begin to require more calories and nutrients than what is provided in milk
if complementary feeding is inadequate
growth may falter
micronutrient deficiencies may increase
especially iron
infectious illness may increase
even with complementary feeding, breastfeeding is a critical souce of nutrients for baby/toddler
breastfeeding provides
up to ½ of infants energy needs up to 1 year of age
up to 1/3 during the second year
high quality nutrients that in complementary foods
immune factors
breastfeeding helps to achieve all millennium development goals
millennium developed goa
developed by UNDP (united nations gloabl development network)
in 2000, 189 nations made a promise to free people fore extreme poverty adn multiple deprivations
eradicate extreme poverty and hunger
breastfeeding reduces early childhood feeding cost
exclusive breastfeeding and continued breastfeeding for 2 years is associated ith reduction in underwight and is an excellent source of high quailty calories for energy
achieve uiveral primary education
breastfeeding and responsive complementary feeding are prerequisites for readiness to learn
breastfeeding and quality complementary foods significantly contribute to cognitive development
could be bc of the fats in the milk that the brain needs to grow and develop
promote gender equality and empower women
breastfeeding is a good equalizes giving every child a fair start on life
most differences in growth between sexes begin as complementary foods are added into the diet, and gender preferences begins to act on feeding decisions
breastfeeding is uniquely a right of women and should be supported by society
more societal constructs to allow women to breastfeed more
reduce child mortality
infant mortality coud be reduced by about 13% with improved breastfeeding practices alone, and about 6% with improved complementary feeding
in addition, about 50-60% of mortality in children < 5 years is secondary to malnutrition
poor breastfeeding practices
inadequate complementary foods and feeding
improved maternal health
the global WHO demands increased attention to support the mothers nutritional and social needs for increased reproductive health and nutritional and pregnancy outcomes
breastfeeding is associated with:
decrease maternal postpartum blood loss, decreased breast cancer, ovarian cancer, endometrial cancer, and the probability of decreased bone loss post-menopause
breast feeding promoted healthy birth spacing
reduced maternal risks of pregnancy too close together
combat HIV/AIDs, malaria, and other diseases
compared with artificial feeding, breastfeeding during the first 6 months by HIV-positive mothers increase HIV-free survival by 32 per 1000 live births
after 6 months, as the age-specific mortality rate and risk of death caused by replacement feeding both decline, replacement feeding appears to be safer
also depends on access to antiviral mediations
low uptake of the virus during exclusive and high uptake during complementary feeding
ensure environmental sustainability
breastfeeding is associated with
decreased milk industry waste pharmaceutical waste, plastics and aluminum tin waste, and excess use of firewood/fossil fuels
develop a global partnership for development
support breastfeeding including
the global strategy for infant and young child feeding
the surgeon general’s call to action to support breastfeeding
socio-ecological model
fosters multisectoral collaboration
builds up the existing partnerships for support of developments
optimal infant feeding has major implications future economic productivity
economic benefits of breastfeeding
reduced health care related expenses
reduced time off to care for sick infant
benefit for employers
lower maternal absenteeism
increased employee loyalty
improved productivity
lower insurance premiums
enhanced public image
health care payers or insurers would benefit savings in:
physician fees
emergency room fees
prescriptions
laboratory procedures
long term health care savings
less chronic diseases
estimates of health care saving
USDA estimates that >$3.6 billion could be saved of rates were increased to levels recommended by US surgeon general
estimate could be higher. only representants savings for ear infections, gastroenteritis, and NEC
if all women participating in WIC breastfed for 1 month, $30 million would be saved
an additional %48 million if 75% of WIC mothers breastfed for 3 months
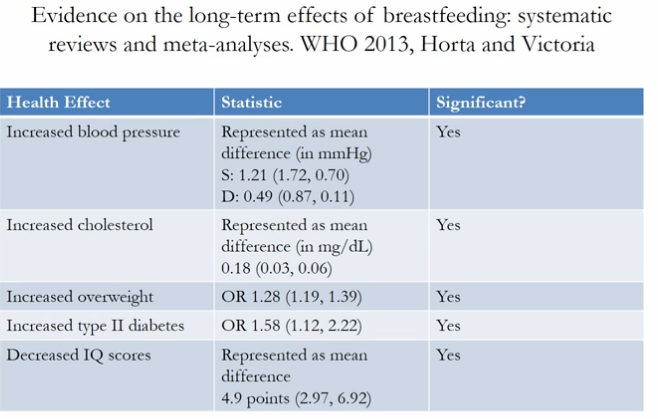
breastfeeding reduces high cholesterol, hypertension and blood pressure, chances of being overweight, type 2 diabetes, and decreased IQ scores
effect pf breastfeeding on obesity later in life: mechanisms
lower protein and energy intake among breastfed
higher protein intake in infancy may increase obesity later
breastfed and formulates infants have different hormonal responses to feeding
formula feeding leads to a greater insulin response
increase fat deposition and increase adipocytes (fat cells)
breastfed infants adapt more readily to new foods such as vegetables
reduces the caloric density of their subsequent diets
effect of breastfeeding on blood pressure later in life: mechanisms
sodium content? - no consensus
fatty acids content of human milk - PUFAS
important structural component of the vascular endothelium
studies are mixed regarding health effects of PUFA added to infant formula - may not act the same
breastfeeding has protective effect on obesity
insulin-like growth factor (IGF-1) is inversely related to blood pressure in adulthood
IGF-1 later in life is positively associated with breastfeeding
IGF-1 programming may lead to lower blood pressure
effects of breastfeeding on cholesterol later in life: mechanisms
cholesterol content is markedly higher in human milk than in most commercially available formulas
high cholesterol intake in infancy may have a long-term programming effect on synthesis if cholesterol by down-regulation of hepatic hydroxymethylglutaryl coenzyme A (HMG- CoA)
HMG- CoA is the rate-limiting enzyme in synthesis of cholesterol from acetate
animal studies show that early exposure to increased levels of cholesterol is associated with decreased blood cholesterol levels at a later age
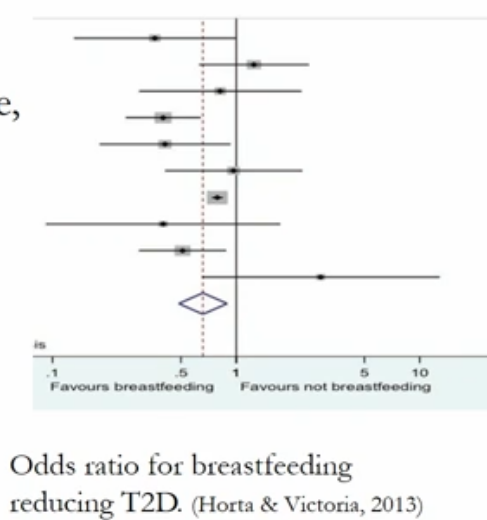
effect of breastfeeding on type 2 diabetes later in life: mechanisms
breastfeeding increases LCPUFAs in skeletal muscle membrane, which decrease fasting glucose
early changes in skeletal muscle membrane may decrease insulin resistance, beta-cell failure, and type 2 diabetes
formula fed infants have higher concentrations of inulin, which may increase the risk of beta-cell fail and type 2 diabetes
adjusting of obesity reduces the strength of the breastfeeding association
effect of breastfeeding on IQ scores later in life: mechanisms
LC-PUFAs are preferentially incorporated into neural cell membranes; structural lipids constitute about 60% of the human brain
docosahexaenoic (DHA) and arachidonic (AA) acids are important for retinal and cortical brain development
breastfeeding enhances the bonding between mother and child, which may contribute to the child’s intellectual development
Week 2 January 14
Learning objectives
Lecture 3 1-17: why drink milk
review: which factors apply to adults and cross species milk consumption
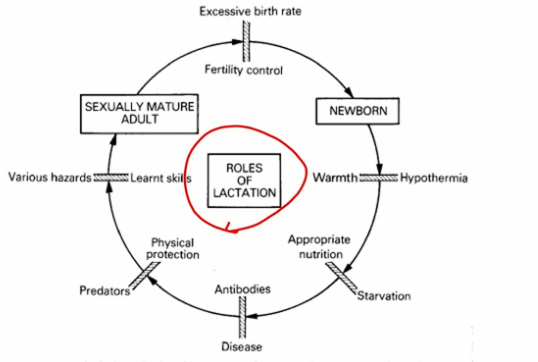
the bonding between the mothers and child through breastfeeding also promotes learned skills
review life cycle
which factors apply to adults and cross species milk consumption and which species
appropriate nutrition (includes proteins, fats, and calories) and preventing appropriate disease (ie bacteria in yogurt and bioactive proteins)
learned skills taking what you know from the dairy industry and applying it to other fields of agriculture and growing food
cows, goat, camel
camel milk can be used for its antidiabetic factors
moose in Siberia
horse and donkey milk is proscribed for Anti disease functions

say that dairy is important to the diet for high quality protein and minerals that might be provided in low income countries
most people in those contries will consume food with high levels of starch
milk can be expensive so milk powder can be used as a substitute
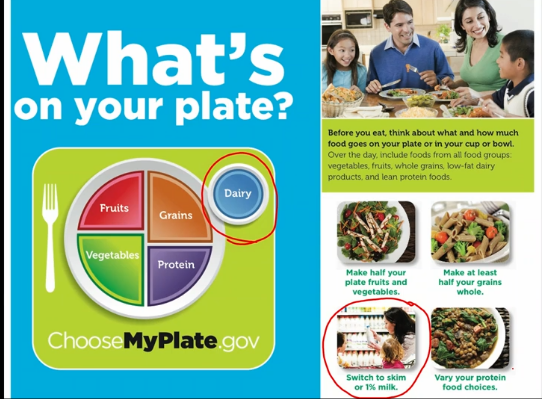
tells people to drink skim or 1% milk because the nutrients are provided and people tend to think milk is a very fatty food
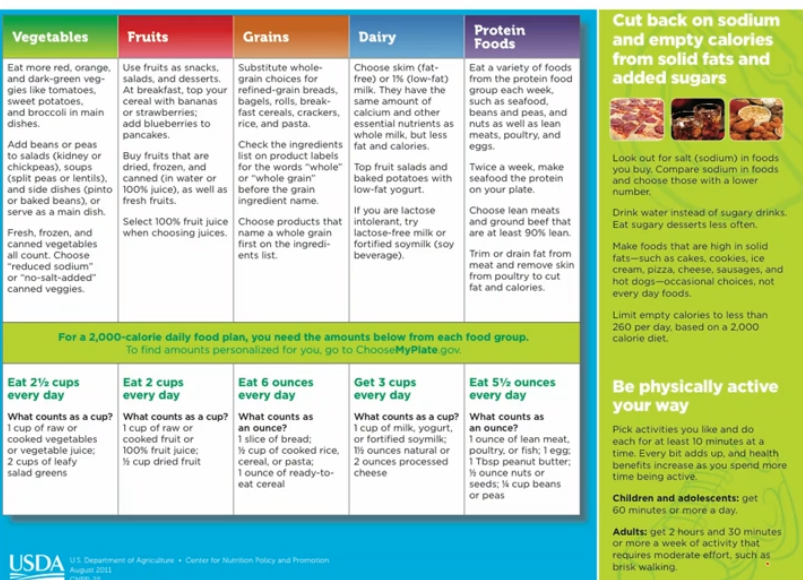
talks about less fat same amount nutrients (tries to stick to the recommended 2000 cal diet)
how to get the 3 cups
top fruit salads and baked potatoes with low-fat yogurt
if lactose intolerant try lactose-free milk or fortified soymilk
health benefit of drinking milk
improved bone health, and may reduce the risk of osteoporosis
important to bone health during childhood and adolescence, when bone mass is being built
associated with a reduced risk of cardiovascular disease and type 2 diabetes and lower blood pressure in adults
nutrients from milk
calcium is used for building bones and teeth and in maintaining bone mass
diets rich in potassium may help to maitain healthy blood pressure
vitamin D functions in the body to maintain proper levels of calcium and phosorous, thereby helping to build and maintain bones
vitamin D is added to millk a lot of time bc cows dont produce that much and people tend to be defficent
RDA (recommended daily allowance) in 3 cups of whole milk
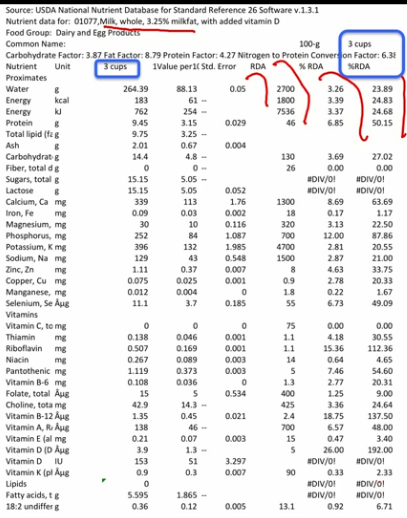
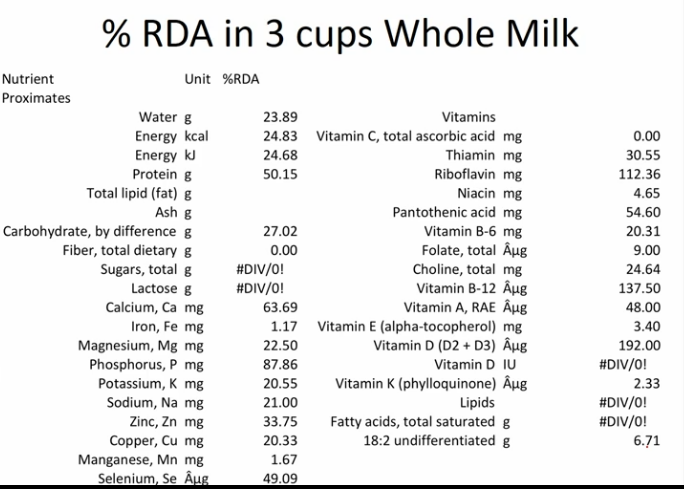
nutrient density is the measure of the amount of beneficial nutrients in a food product in proportion to its energy content, weight or amount of detriment nutrients. it is a way of evaluating the nutrient quality of food by comparing the amount of nutrients consumed in a bite a meal or day
milk is nutrient dense in protein, calcium, phosphorus, zinc, riboflavin vB12), vD
vD is fat soluble so vD added to whole milk will likely enter your body instead of 1% it will prolly be sticking to the sides of the container
what’s special about milk’s nutrition? disease prevention
malnutrition
bioactive components relating to various disease:
rickets, osteomalacia, osteoporosis
metabolic syndrome, obesity, cardiovascular disease, hypertension and type 2 diabetes
oxidative and inflammatory stress
regulate satiety and digestive
satiety: the feeling of fulness and satisfaction after a meal
processes
cancer (Ca, [H,X]AMLET human milk protein) (particularly colon cancer)
dental caried
evolutionary considerations
pre-human 3.2 million years ago were probably omnivores
time of finding Lucy the hominid
walking upright
carying an infant and breastfeeding while moving
cattle depicted in drawings about 30,000 years ago
important part of the culture
do not know if the meat or milk was consumed
domestication of livestock happened about 10,000 years ago
holding animals for their whole life and then breeding them
milk adopted as human food about 6,000 years ago
we know this from artifacts
had traces of milk proteins
History of dairying
animal domestication - milk, meat, blood, hides, wool, muscle power
dairy domestication occurs around the world
species and breed differences
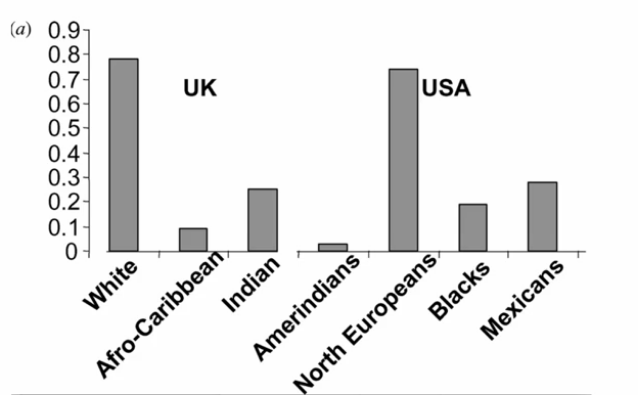
persistent lactasia (lactose digesting capacity. LDC) - mutation in human regulatory sequence (intron) that permits adult lactose utilization
single nucleotide mutation
when the animal is weaned, the genes turn off from being able to digest milk
mutation began in the yt people
dairy domestication occurs around the world - species and breed differences
cattle transported with population migration - animals were wealth, wealth generating
most early Americans and European families held a few cows for family use
had to transport animals on the boats for 1-2 months
milk is perishable commodity - use right away
northern climates favored
seasonal breeding
good bc animals like goats don’t require as much fed but you would have to find another milk source
most milk consumed in the colder months and less in the summer months
urbanization hastens innovation
larger farms, transport, distribution
mechanization: feeding, milking, packaging
sanitation: benefit consumers and animals
developed in the early part of the 20th century to increase shelf life and prevent spoiling
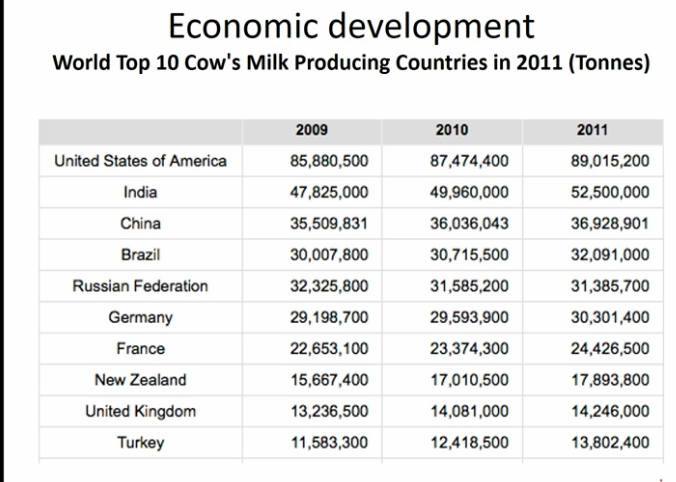
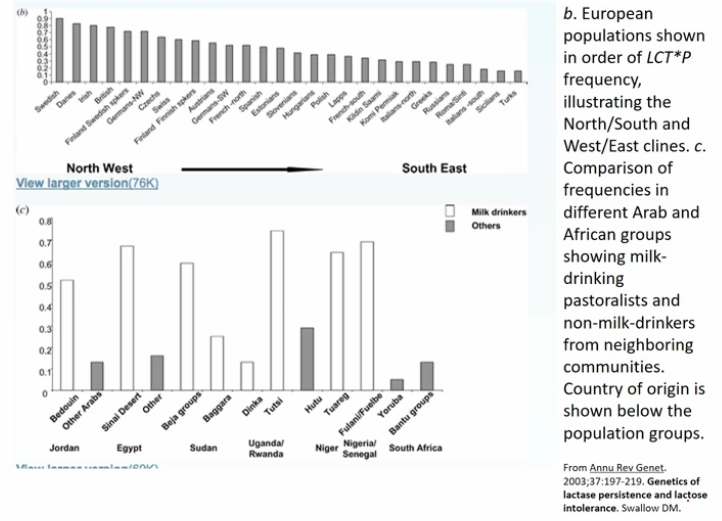
Pakistan is 2nd in total milk production if you add up all the animal’s milk
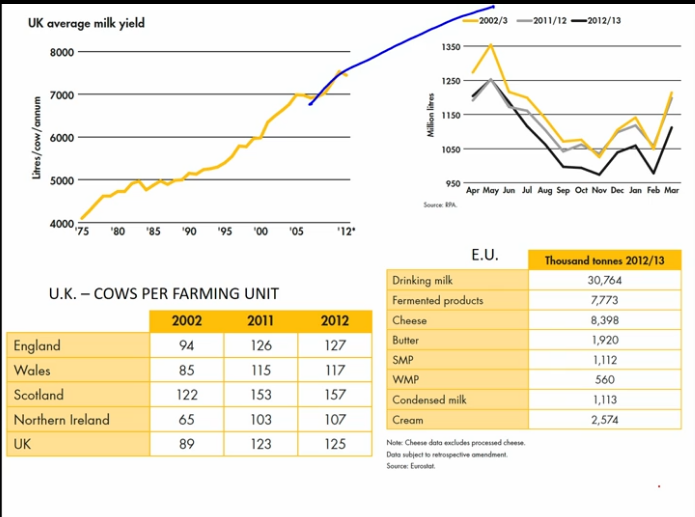
highest production in April and May with the least being in October and November
cows are being rebreed
in January and February milk increase as the cows calve
cows are producing more milk due to better genetics
highest cost of milk is processing
US - milk marketing
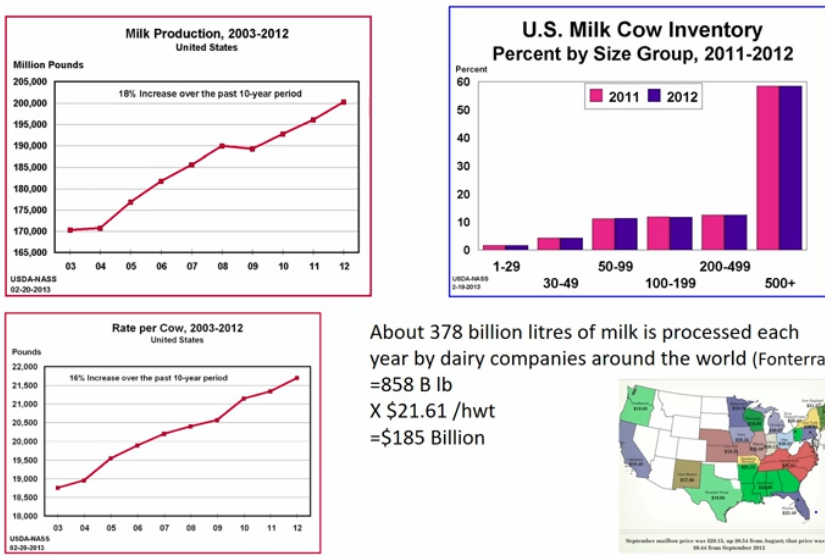
USDA report: US farm numbers continue to decline
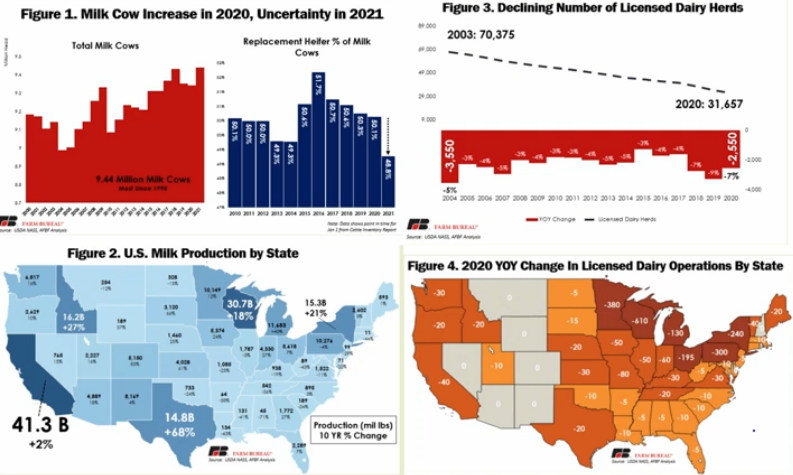
California is the biggest producer - 2% increase; 41.3 billion lb.
Wisconsin - 18% increase in milk production; 30.7 billion lb.
Texas - 68% increase in milk production; 14.8 billion lb.
New York -15.38% increase in milk production; 15.3 billion lb.
Idaho - 27% increase in milk production; 16.2 billion lb.
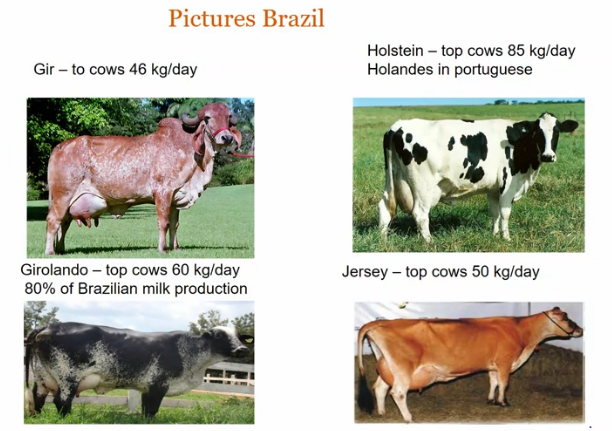
developing countries - appropriate, species, breeds, management
collection from small holder dairies
milk bulking centers
test quality
record payment
breeds
Malawi zebu (Malawi)
people are trying to improve genetics my mixing genes with other breeds like the Holstein
Finnish Friesian (Finland)
Holstein Friesian (Germany and the Netherlands)
milk yield consideration
heat tolerance in tropical developing countries
adequate diets necessary
energy for maintenance (forge)
milk for calf (forage)
extra milk for collection (forage + concentrations)
milk uses
family
vendor sales (immediate money)
coop bulking groups
pasteurization and processing
monthly check
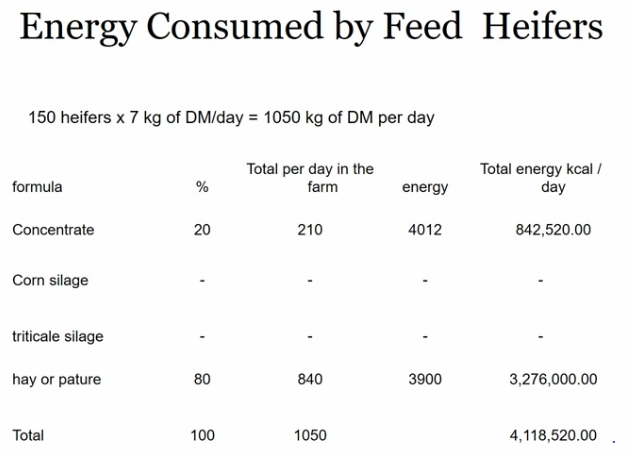
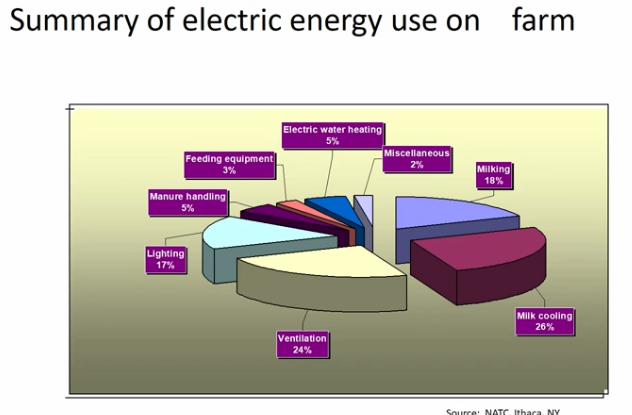
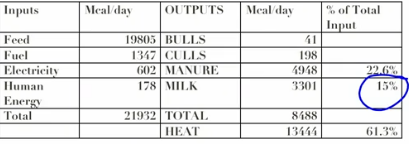
dairy farm energy
energy flux
farm system
how the operation works
Maintenace
storage of milk
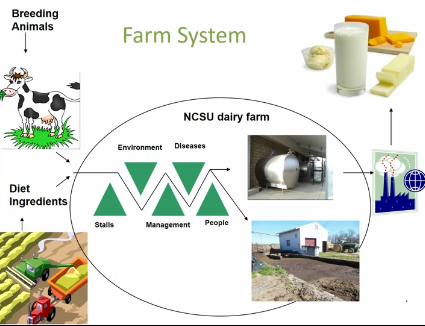
pictures
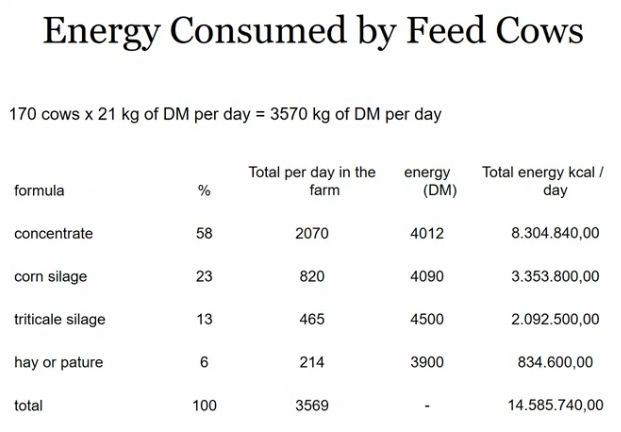
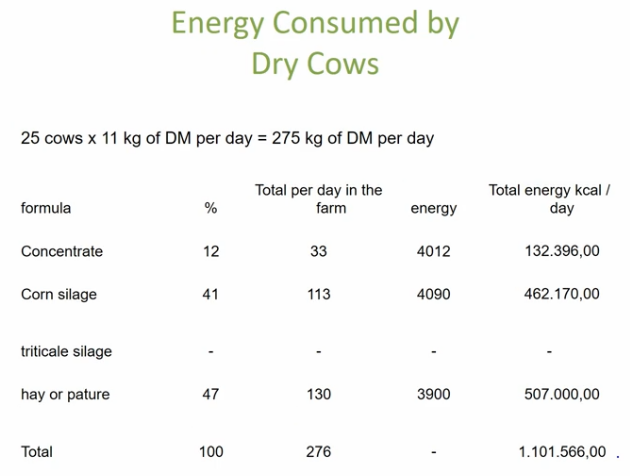
calculation basis
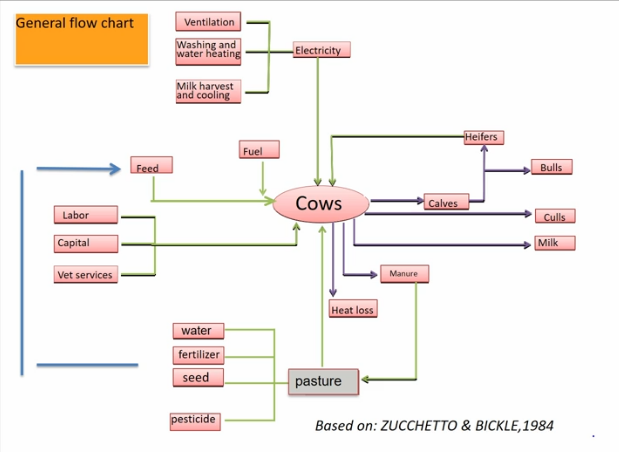
how the energy goes in and out of the dairy farm
electricity, feed, and human components (labor, capital, vet services) are the inputs
calculation basis: NCSU dairy unit
milk production -80 lb./day Holstein + 65 lb./day jersey (average = 75 lb./day)
75 lb./day or 34 kg/day x 625 cal/kg = 21,250 cal/cow/day
160 milking cows x 21 kcal/day = 3360 kcal/day
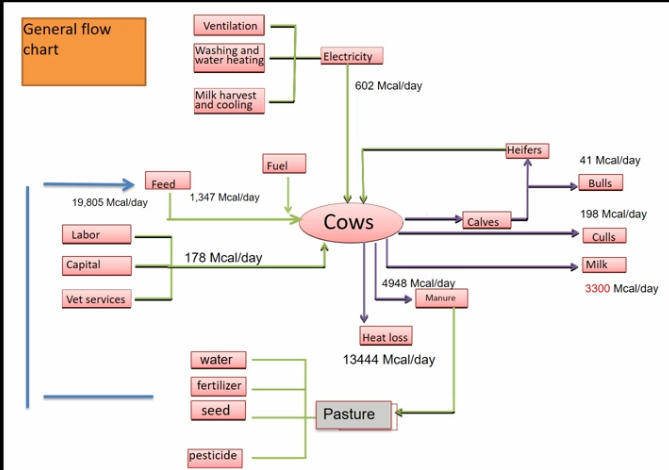
conclusion
system flows mainly from feed to manure and energy loss represents 61% as heat and 23% as manure from total inputs
why drink milk
milk is life sustaining food
milk is rich in essential nutrients
retail milk is sanitary and ha uniform quality
milk taste good to most people
physical and chemical properties allow transportation and processing in massive quantities with minimal labor
much of US and other temperate countries are good for dairy relative to other crops
Lecture 4 1-19: human milk composition and correlation to reducing infant mortality
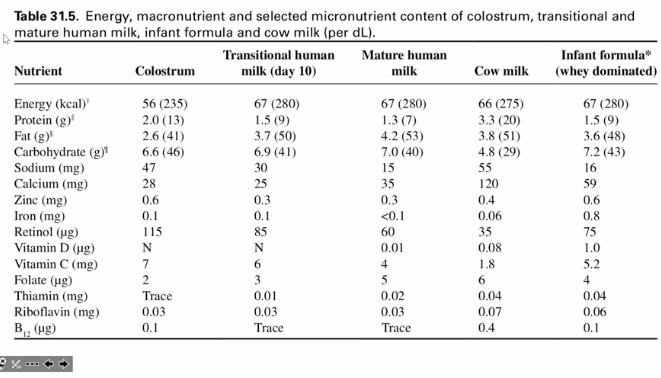
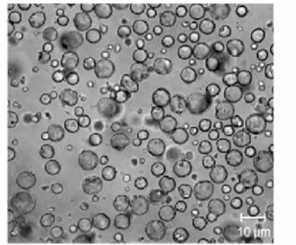
human milk and formula
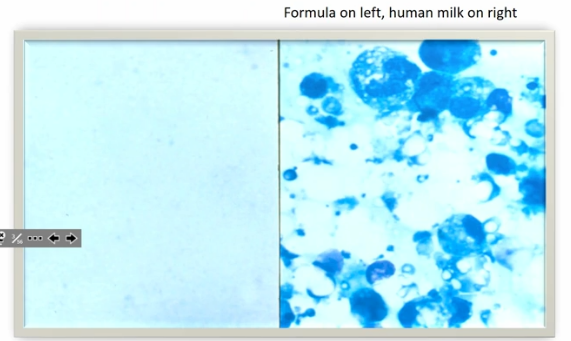
the differences in the microscope pictures are bc of
cellular protein and nucleic acids straining unevenly and darker blue in human milk
white is fat bc fat does not stain
the proteins and nucleic acids are stained
bacteria and cell debris are removed from bovine milk before it is processed into infant formula
processing includes putting the milk through a centrifuge to remove the somatic cells and bacteria
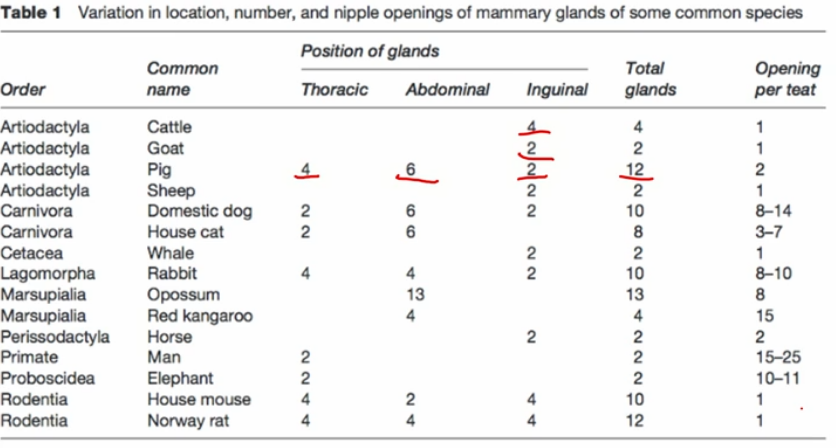
cow’s milk has more minerals
same osmolarity
some people made their formula from cows’ milk
dilute it and then and some sugar or sucrose and some fat
carbs pull water
1940s-1970s
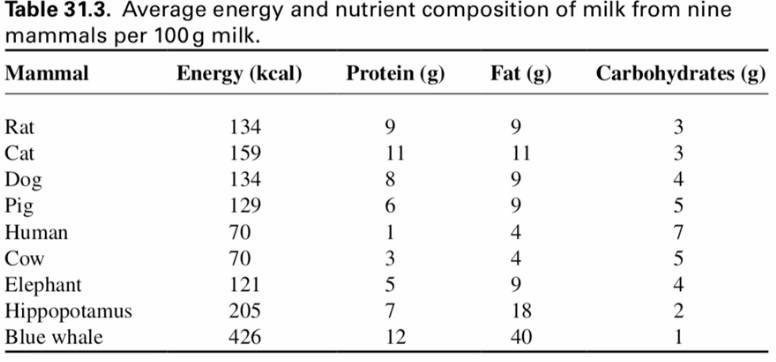
blue whale milk is thick
high casein (protein)
not very osmotic
horse milk is similar to human milk
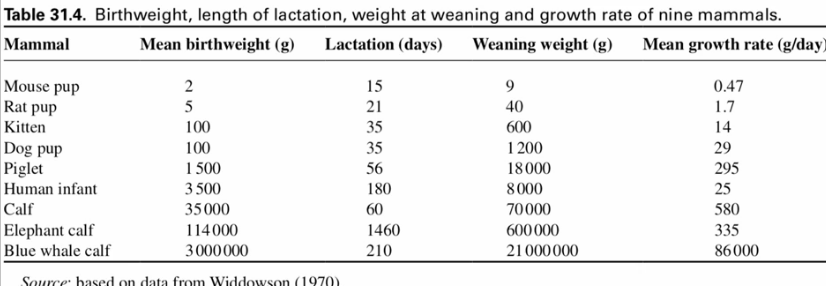
less calories in milk means slower growth rate
humans and horse milk provide all the water an infant needs
protein drops
carbs increase
a big drop in sodium from colostrum → mature milk
helps with water intake
water will follow the sodium
the tight junctions in the infant are still leaky so the sodium leaks from the blood into the cell
more calcium more casein
lipids
largest source of energy in human milk
contributes 40-55% of the total energy
for adults it is less than 30% of the recommend total energy
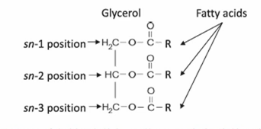
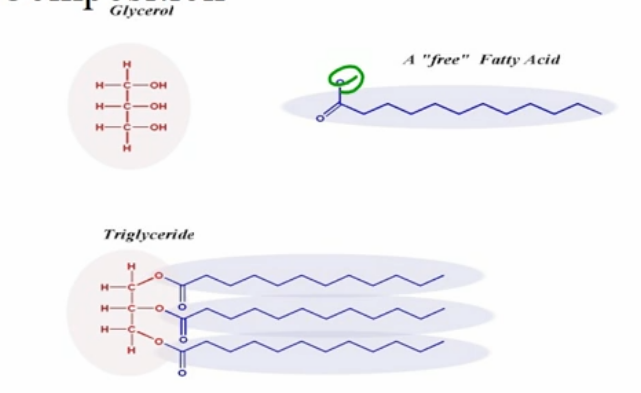
in the form of triglycerides
has an ester bond
cow’s milk has a lot of short - medium carbon side chains (C6-C12)
plants are normally C16-C18
a lot of research is going to see if changing the lipid composition plant vs cow will have an effect on the human body
brain effects also
when C6-C12 is absorbed in the intestines they are small enough to stay within the blood stream
C16-C18 has to be repackaged into triglycerides into chylomicrons to be transported within the bloodstream
contains over 200 fatty acids
oleic acid dominates (C18:1 omega 9)
long-chain PUFAs
short-chain fatty acids
sphingomyelins
functions
allow maximum absorption of fatty soluble nutrients
provide essential fatty acids and polyunsaturated fatty acids
omega 3 and omega 6 are essential
provide cholesterol
plants do not make cholesterol
neonatal cell membrane production needed for growth, brain and retinal development, and bile salt synthesis
linked with cell growth
nervous system myelinization
contains over 200 fatty acids
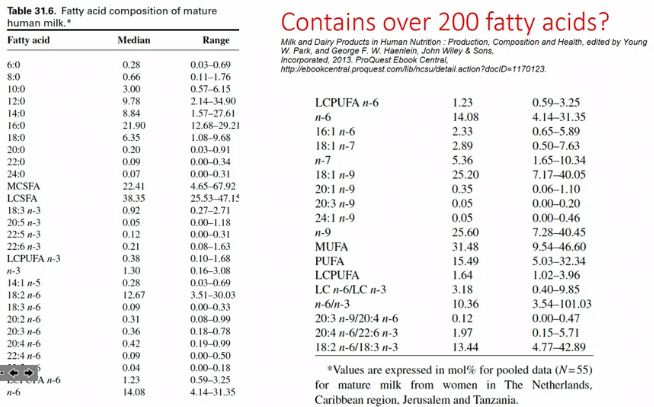
from 6 to 24
different chemical structures if you go from unsaturated (has the double bond) to saturated
monounsaturated fats in the omega 3 position (meaning the double bond is 3 carbons away from the methyl end)
PUFA = polyunsaturated fatty acid
very small amounts of odd chain FA
15 and 17
linoleic acid is an essential omega 6 FA (18:2n-6)
alpha linolenic acid is an essential omega 3 FA (18:3n-3)
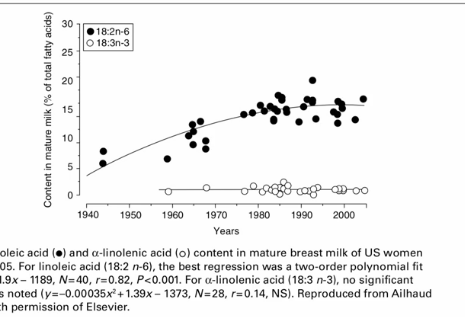
what biological or environmental factors might be responsible for an increase in essential fatty acid composition of human milk samples over the years 1945 to 2005
changes in diets to increase plant oil use in foods and in cooking and less of saturated fat from animals
lard is from pigs
Talo is from cows
human milk lipids are dynamic
fat content is higher in the evening than in the morning
the type of fat consumed
a diet rich in PUFAs will cause an increased percentage of PUFAs in the milk without affecting the total fat content
when fish oil is given during pregnancy, it significantly increases omega-3 FA and IgA as well as other immune factors
the ratio of PU to saturated fats in human milk promotes calcium absorption
calcium absorption is depressed by 4.5 P/S ratio found in bovine milk
human milk lipids have antiviral activity
potent cytolytic effects on intestinal parasites and gram-positive bacteria and yeast
lipids in fresh human milk do not inactivate viruses until storage at 4 C or 23 C due to the release of FFA from milk triglycerides
level of lipoprotein lipase in milk was correlated with he antiviral activity of the milk TG→FFA
antiviral effect is caused by disintegration of viral envelopes by FA
carbohydrates
primary source of calories in human milk
lactose is the predominant carb
easily digested
facilitates calcium absorption
binds with calcium in the disaccharide form
essential for CNS development
reduces osmolarity relative to monosaccharides
more slowly digested than sucrose or maltose
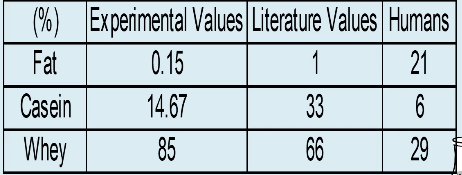
proteins
over 400 proteins in human milk
casein (10-50%)
about 5 different monomers to form casein in cows
human milk has lower amounts of casein than bovine milk
whey (90-50%)
alpha-lactalbumin (helps make lactose)
beta-lactalbumin (not present in humans only cows)
lysozyme
serum albumin
50% in colostrum and 90% in mature milk
enzymes
hormones
IgA (32x higher in human milk than in bovine milk)
IgG
IgM
cytokines
growth factors
anti-inflammatory factors
proteins and AA in human milk have several functions
nutrition (provides 4 cals per gram)
after digestion and absorption
antimicrobial and immunomodulatory activities
in gut and post absorption of nutrients
example for protein: vB12 binding protein
example for AA: zinc and histidine
vitamins and minerals
vitamins
most vitamins avaliable in sufficient quantities in human milk
cows milk is less diluted and contains the same if not more minerals
vD - supplementation recommended by AAP
vK - present in small amounts in human milk
protection from hemorrhagic disease
minerals
iron - levels in human milk are sufficient to meet the iron requirements of the exclusively breastfed full-term until 6 months of age
most formulas are iron fortified bc bacteria can’t grow without it
harder for absorption
fluoride - in communities with fluoridated drinking water, breastfed babies receive fluoride through their mother’s milk
whats in infant formula
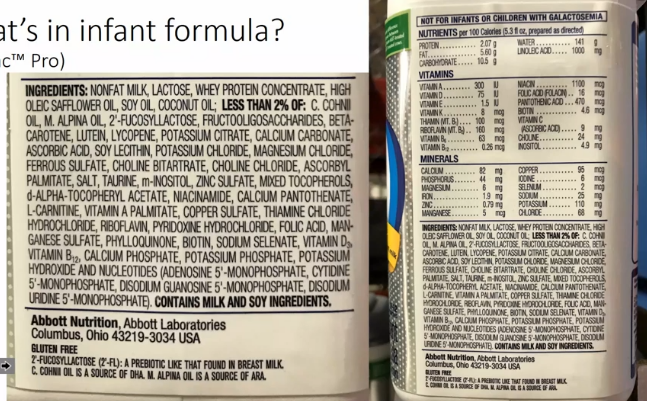
fat free milk, add lactose, add whey, add oleic acids (has omega 6) cohni oil (for DHA) and alpina oil (for arachidonic acid), HMOs (oligosaccharides such as fructooligoaccarides and 2’-fucosyllactose), beta creatine (vA precursor) lutein and lycopene (bioactive nutrients and accumulate in the retina), potassium citrate (for some fat), calcium carbonate ( for calcium), ascorbic acid (vC), soy lecithin (emulsifier for fat), potassium chloride to balance the P:K ratio, magnesium chloride (Mg an essential nutrient), ferrous sulfate (for iron), choline (for phospholipid synthesis and neurotransmitter), ascorbyl palmitate (vC), taurine (AA high in human milk for vision), tocopherols (vE), potassium hydroxide (to balance pH), nucleotides (found in human milk but not bovine milk)
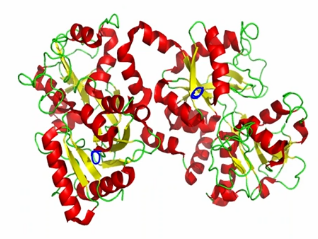
HAMLET: human alpha-lactalbumin made lethal to tumor cells
complex of alpha-lactalbumin and oleic and linoleic acid
can increase the activity of antibiotics against methicillin-resistant staphylococcus aureus (MRSA)
broad anti-tumor activity (does not affect healthy cells)
cells
babies ingest thousands-millions of immune cells from their mothers daily
immune cells increase significantly in milk when the mother baby has an infection
glycoproteins
mucins: protect against infection, regulate cellular signaling, and transcription (glycoprotein that complexes bacteria)
bile salt stimulated lipase (BSSL): aids in lipid digestion and inhibits virus invasion (breaks down the triglycerides and fatty acids)
lactadherin: binds to rotavirus and inhibits its replication; stimulates growth of intestinal epithelial cells
lactoferrin
lactoferrin
iron chelation to assist in iron absorption in the infant and inhibit bacterial iron absorption
modulator of inflammatory and immune responses
protects against tumor growth
aids in one development
the peptides also seem to have an antibacterial agent to them
immune factors
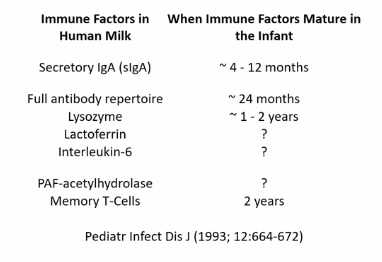
secretory IgA
in the gut and found in human milk
mother is exposed to pathogen → mother makes antibody to pathogen → mother breastfeeds baby → baby ingest antibody → baby is protected from specific pathogen
lysozyme
breaks down the outer cell wall bacteria
human milk contains 3,000x more lysozymes than bovine milk
resistant to break down by acid in the stomach as well as trypsin
adequate amounts reach the intestinal tract
breaks down cell wall of gram positive bacteria
select defense molecules
mucins
inactivates viruses and bacteria
fibronectin
makes phagocytes more aggressive against microbes
helps repair tissues damaged by immune response
bifidus factor
fosters growth of lactobacillus bifidus in gut
gamma-interferon
enhances antimicrobial activity of immune cells
one of the first things to be produced during an immune response
B12 binding protein
reduced amount of B12 available to harmful bacteria
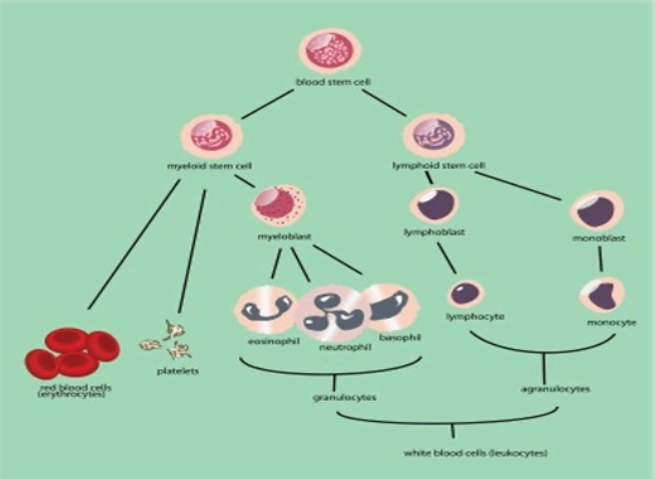
leukocytes (white blood cells)
Phagocytes
b lymphocytes
produce antibodies against specific microbes, especially E. coli
T lymphocytes
kill infected cells directly and mobilize the immune system
lymphocytes
neutrophils
attack and digest bacteria
most abundant in colostrum
macrophages
kill microbes in baby’s gut
produce lysozyme and mobilize the immune system
adiponectin
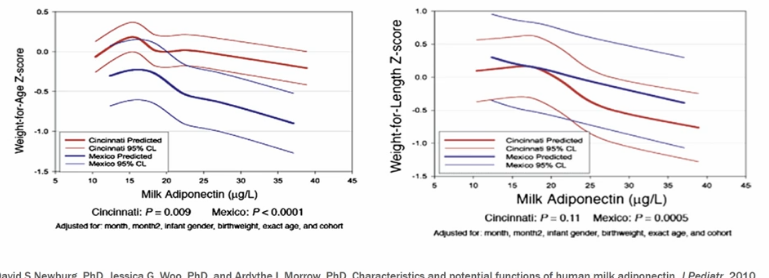
inversely related
more adiponectin less body fat
effects of breastfeeding on blood pressure later in life: mechanisms
FA content of human milk
PUFAs are protective of high blood pressure
breastfeeding has a protective effect on obesity
may then lead to protective effect on blood pressure
adapts to baby’s needs
hindmilk has more fat

stages of human milk

pre-term milk
composition similar to that of colostrum
higher levels of IgA, lactoferrin, and lysozyme
LC-PUFAs are higher and remain higher for the first 6 months in women who deliver preterm
24 calories per ounce
human milk composition changes with individual variation in second year lactation
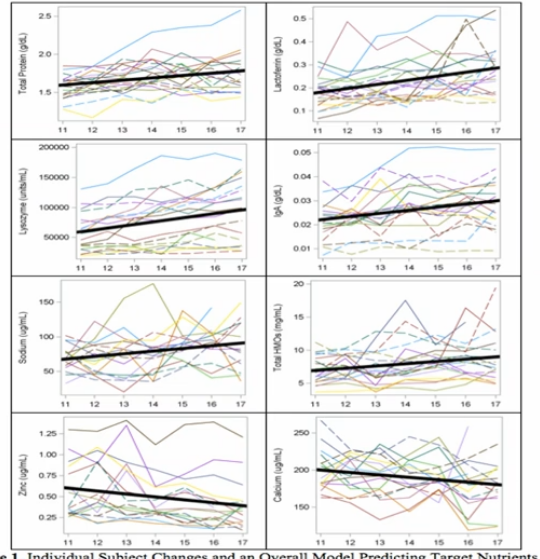
time-associated changes in human milk
time since the last feeding
the more time that has passed since the last feeding, the lower the concentration of fat in the milk
diurnal variation
fat content peaks midmorning
fat content is lowest in the middle of the night
hormones
prolactin
the milk making hormone and the mothering hormone
levels are higher at night
CCK
signal satiation after feeding
melatonin
levels are higher at night
it has a hypnotic effect as well as a relaxing effect on then smooth muscle of the gastrointestinal tract
oxytocin
associated with
lower blood pressure
vasodilation
metabolic
effects
anti-inflammatory properties
Week 3 January 21
learning objectives
Lecture 5 1-24: nutritional components in milk
Article notes from lecture
residential green environments are associated with human milk oligosaccharide diversity and composition
HMO = human milk oligosaccharides
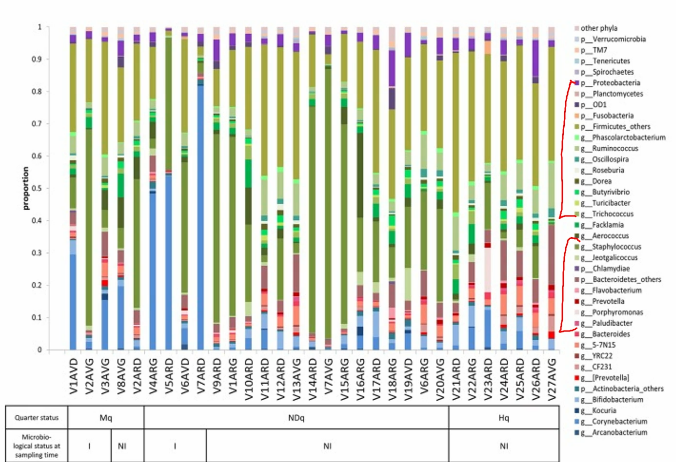
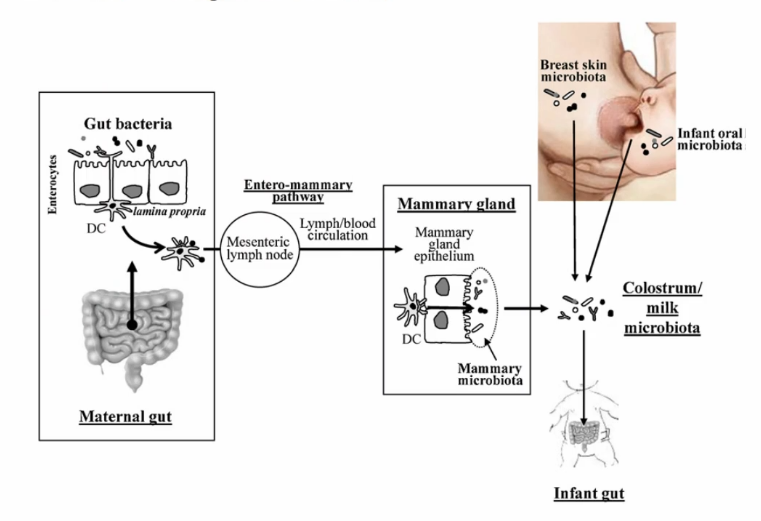
breast milk composition is impacted by the living environment
green environments (with varying levels of environment microbiota) may influence the abundance and composition of microbiota that colonize the maternal skin and respiratory tract leading to changes in the maternal immunity and milk microbiota
green environment may also influence the concentrations of other components in milk such as pollutants which interact with HMOs within milk → changes in HMO diversity and concentration
ie bacteria from trees is different from bacteria on concrete
modifications in HMO composition may further impact infant gut microbiota composition and immunity impacting on risks of several childhood disease
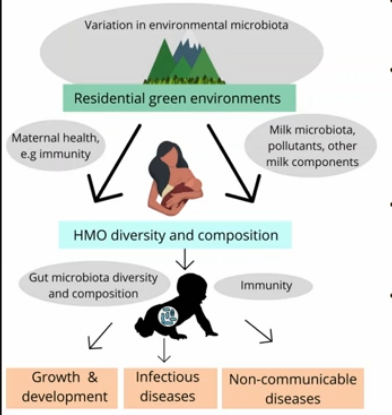
1)greenness (normalized difference vegetation index NDVI)
2) vegetation cover diversity (VCDI)
3) naturalness index (NI)
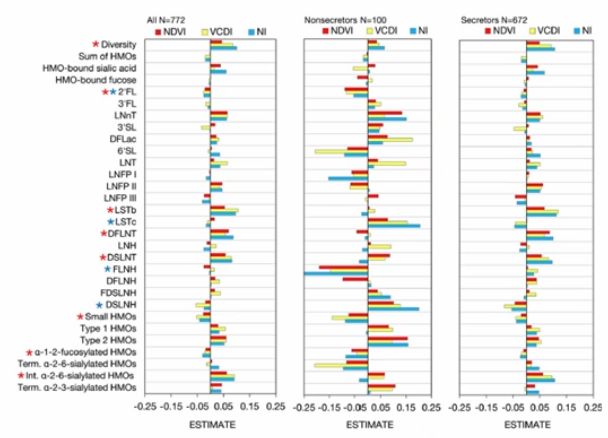
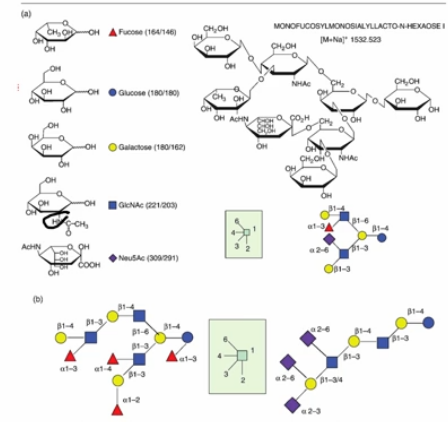
the main HMO secreted is 2-fucosyllactose
nondigestible by the gut
becomes a prebiotic to feed the gut
people make a lot of 2-FL are known as secretors
people who do not produce a lot of 2-FL are Non secretors
the environment affects them more
based on this reading of an infant formula ingredient label in an earlier lecture, what components were identified as additives to account for the difference in the amount of oligosaccharides secreted into milk of cows relative to humans?
2’-fucosyllactose and fructooligosaccharides
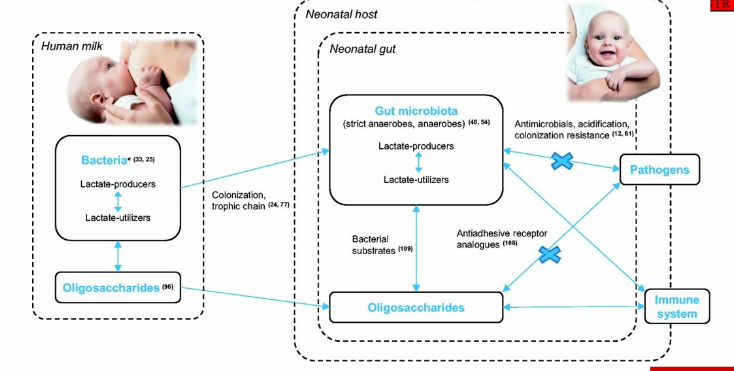
oligosaccharides
serve as a prebiotic for development of friendly gut bacteria
binds pathogens and prevents them from binding to the gut
third most abundant ingredient in human milk
made up of fucose, galactose, hexose, glucose, sucrose, galactose
lots of binding sites
whats in human milk
HMO are food for freindly bacteria like bifidobacterium infantis. shorter chain HMOs in particular are almost entirely consumed by this microbe
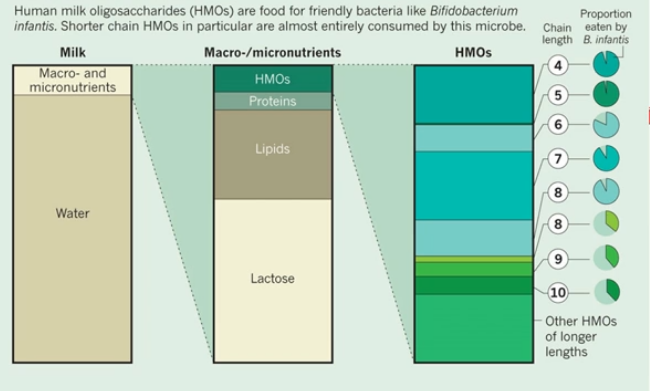
prebiotic
non-digestible food ingredients that stimulate the growth and activity of designated species of beneficial bacteria
HMOs
probiotic
living organism which when administered in adequate amounts confers a health benefit on the host
breast milk bacteria
human milk has significantly more oligosaccharides than other species milk
breast milk microbiome
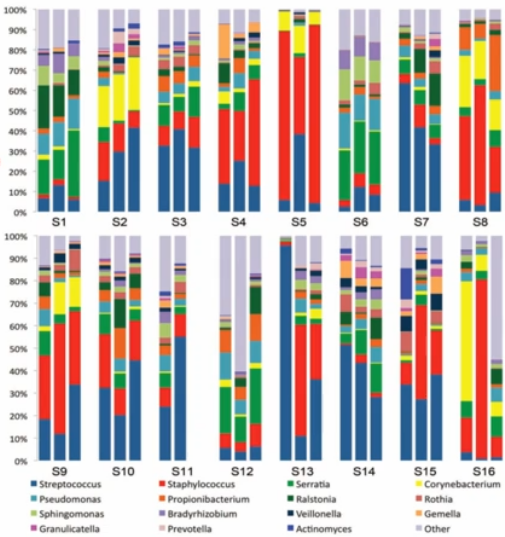
hundreds of bacterial species
varies greatly between individuals
composition changes over the course of lactation and is affected by obesity and mode of infant delivery
probiotic action
human milk is a source of beneficial bacteria that can colonize the infant gut
nutritional role of the normal infant gut microbiome
HMOs and milk from primates have an effect on the nutrition of the infant, the infant is having an effect on the growth of the microorganism, and the microorganisms have an effect of what nutrients are available in the infant’s gut
where does vB12 come from?
vB12 synthesis
comes from mostly animal products bc mammals can’t produce it → comes from microorganisms
beef has a lot of B12 because they are ruminants
important for DNA replication, red blood cell formation, and development and normal function CNS
number of genes involved in B12 synthesis within microbiome increases with age
where does folic acid come from?
folate synthesis (vB9)
involved in DNA replication and repair and erythropoiesis
microbiome may synthesize a pool of folate that represents around 63% of adequate intake level for infants less than 5 months of age
found in foliage
in plants it is attached with complex with glutamic acid
bacteria probably produce the form with polyglutamate
animals will eat their own feces to ingest and absorb more B12 and folic acid
which class of organisms that is contained in human foods is able to synthesize the vitamin folate
bacteria
plants
fungi
what is the class of organisms that is principally responsible for synthesis of the vB12 that is a needed component of the human diet
bacteria
health associations with microbiome dysbiosis
childhood obesity
necrotizing enterocolitis (NEC)
the degradation of the gastrointestinal tract due to bacteria
common in premature babies
one of the leading causes of death in premature babies
intestinal bowel disorder (IBD)
Crohn’s disease
lecture
topics
composition: proteins, lactose, lipids, minerals, vitamins, enzymes
factors affecting composition: species breed, feed, stage of lactation
physical and chemical properties: density freezing point, color, pH, acidity, flavor
bacteria
somatic cells and microorganisms: lactobacilli, history, significance in cultured products
milk fraction terms
plasma: milk - fat (skim milk)
serum: plasma - casein micelles (whey) are taken out
plasma minus the coagulatable proteins
solids-non-fat (SNF): protein, lactose, minerals, acids, enzymes, vitamins
it is the total solids content minus the fat content
total milk solids: fat + SNF
86% in bovine
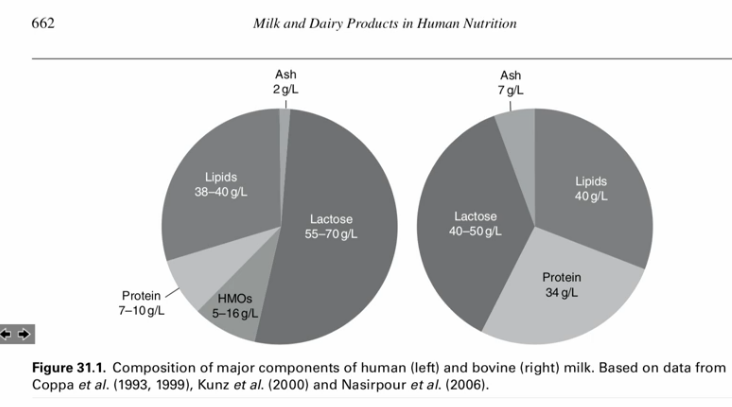
composition tables
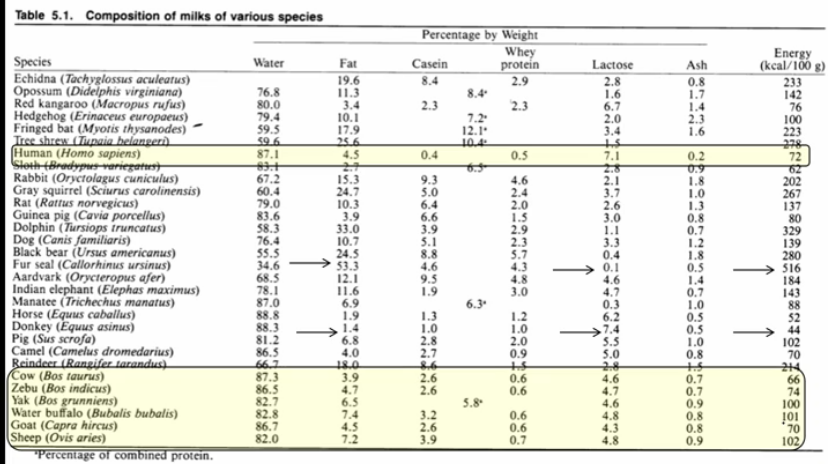
human is about 4.5% fat
87.1% water
casein is 0.4%
whey is 0.5%
lactose is 7.1%
ash is 0.2%
energy (kcal/100g) is 72
high lactose low ash
cow (bos taurus)
87.3% water
3.9% fat
2.6% casein
.6% whey
4.6% lactose
0.7% ash
energy (kcal/100g) is 66
low lactose high ash
ash is made of the minerals, vitamins and electrolytes
composition of bovine milk
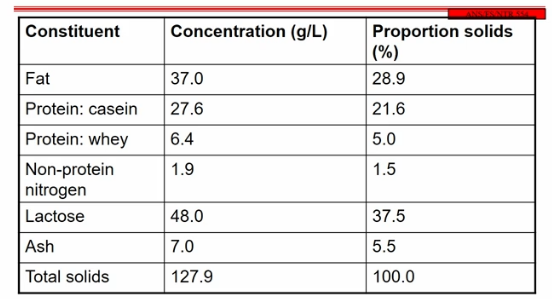
casein is 80% of the protein in the milk and whey is 20% in bovine
in humans is 80% whey and 20% casein
non-protein nitrogen is from urea, nucleotides, small nitrogen molecule containing molecules
N in protein makes up 17-18%
the conversion factor is 6.38 in milk
whereas in most food its 6.25
this is because of the different composition of casein compared to most proteins
lactose
most abundant of milk solids
made up of galactose and glucose
beta 1-4 glycosidic bond
disaccharide and cannot cross the cell membrane of the alveoli
hydrolases break the glycosidic bond in the gut
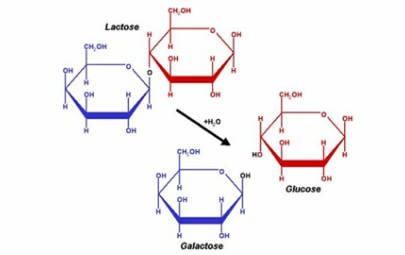
lactose hydrolysis increases sweetness in milk
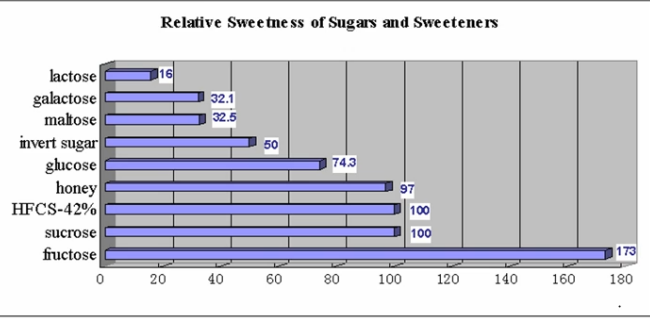
the more hydrolase the more it breaks down lactose into galactose and glucose
milk proteins
casein and whey
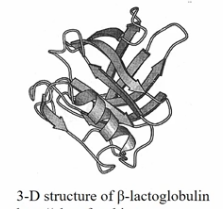
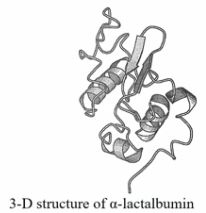
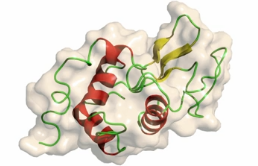
whey
alpha helix
beta barrel is used as a binding site
any molecules like lipids, vitamins will bind here because the beta barrel is hydrophobic
a-lactalbumin binds calcium, zinc, and manganese
important to form lactose
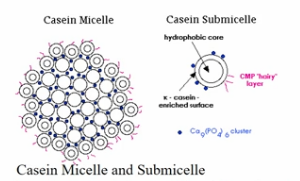
casein
the inside of the casein submicelle is a hydrophobic core
has alpha and beta casein
the outside layer of the is called kappa casein or k-casein
glycoprotein
helps to form a micelle
the micelle keeps the protein suspended in the milk at regular pH
when the pH is changed the micelles with come together
happens in the stomach
that’s how you get milk curds
lysozyme
breaks down the other cell wall bacteria
human milk contains 3,000x more lysozyme than bovine milk
resistant to break down by acid in the stomach as well as trypsin
adequate amounts reach the intestinal tract
a lot in human not so much in bovine milk
beta-lactoglobulin is really resistant to digestion and alpha-lactalbumin is easier to digest
predominant proteins in human and bovine milk
bovine has more casein that human
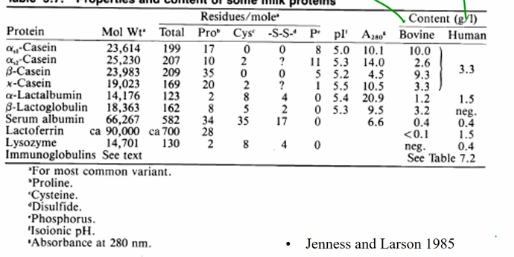
barely any lactoferrin in bovine
cystine makes disulfide binds to form alpha helixes
human milk tends to have beta-casein
milk proteins-reactions
destabilization of the casein micelles
change in pH
the isoelectric point (pI) of milk is around 4.5
so below 4.5 the casein will be protonated and lose its negative charge
as a result, it destabilizes the kappa casein and makes the micelles come together making curds
proteolysis (rennin)
glycomacropeptide
enzyme used to destabilize kappa casein and allows the milk to curd
originally got rennin from calf stomachs but now it is made synthetically
lipids
fat soluble vitamins
saturated FA
butyric acid, SCFA, VFAs
trans FA, CLA, rumenic acid
is a cis/trans isomerization in the rumin when fed linoleic acid (PUFA from soy oils)
reduces the double and then the double bond can reform
when the rumen forms TFA they are healthy
not found in human milk
can have anti caner properties
sterols
essential fatty acids
milk fat
milk fat globule
protein membrane
rupture of FGM (fat globule molecule)
density (fat is less dense than water)
in milk at the store the milk goes into a centrifuge and is homogenized
the bigger fat globs are broken up into smaller ones and coated by casein
in raw milk the bigger globs are lighter that water will float to the top and make a cream fraction
composition
most is made from triglycerides
back bone is glycerol
combined with a free fatty acid
combined with an ester bond
synthesized from within the cell
the mammary gland can synthesize its own triglyceride like in adipose tissue and in the gut
the 2 positions in the carbon tends to polyunsaturated fat and long chain fatty
the short chain FA tend to form on the outside
saturated and unsaturated fatty acids
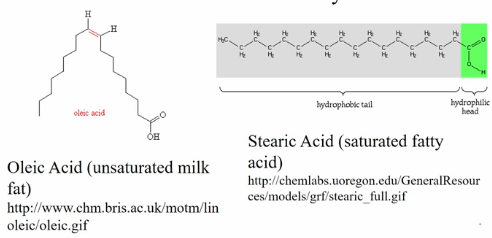
one double is in the cis so that that the Carbon and Hydrogen stay in the same side
stearic acid the saturated form of an 18 carbon FA
principal fatty acids in milk fat
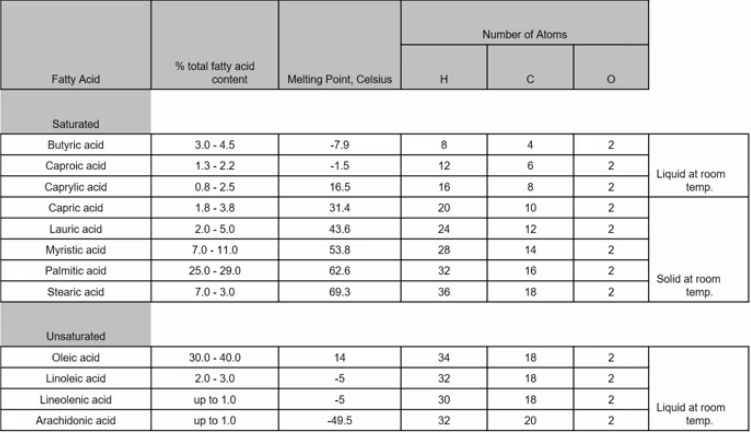
the fatty acids are named based on their length
short chains are made from acetic acid
mammary glands tend to synthesize medium and short chain fatty acids
neither human nor bovine can produce the polyunsaturated fats
linoleic, linolenic (can make DHA from linolenic) and arachidonic acid (from linoleic)
milk fat chemistry
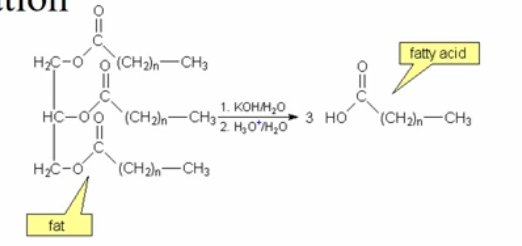
hydrolysis
some bacteria will do hydrolysis of the milk fat
oxidation
the double bonds and the carbonyl group can be oxidized
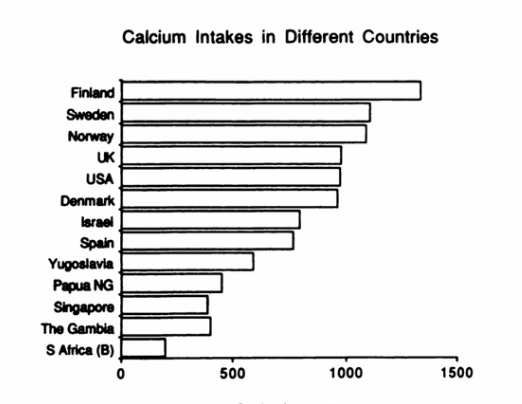
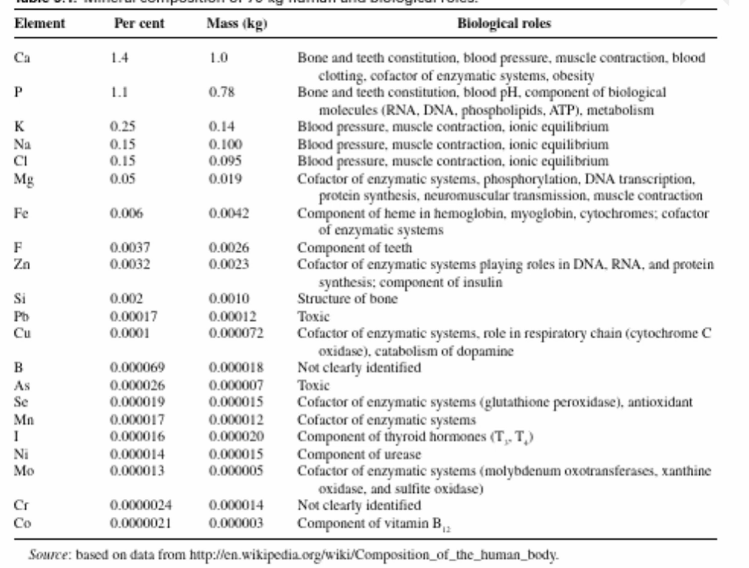
macrominerals
calcium, phosphorus (P), magnesium (Mg), potassium (K), sodium (Na), chlorine (Cl), sulfur (S)
health effects of Ca
osteoporosis
hypertension
dental caries
cancer
trace elements
high = iodine (I), manganese (Mn), selenium (Se) chromium (Cr)
low = iron (Fe), selenium (Se)
regulated (Fe, Cu, Zn) vs unregulated (Se, I)
vitamins
minerals
calcium: functions in the mineralization of bones and teeth, muscle contraction and relaxation, nerve functioning, and blood clotting
iron: carries oxygen as part of hemoglobin in blood or myoglobin in muscles, and it is required for cellular energy metabolism
magnesium: a factor involved in bone mineralization, the building of protein, enzyme action, normal muscular function, transmission of nerve impulses, proper immune function and maintenance of teeth
phosphorus: involved with mineralization of bones and teeth, it is important in genetic material, in cell membranes as phospholipids, in energy transfer, and in buffering systems
potassium: facilitates reactions, including the making of protein. it is involved in the maintenance of fluid and electrolyte balance, the support of cell integrity, the transmission of nerve impulses, and the contraction of muscles, including the heart
zinc: associated with hormones, it is needed for many enzymes (around 200), it is involved in making genetic material and proteins, immune cell activation, transport of vitamin A, taste perception, wound healing, making of sperm, and normal fetal development
mineral constitutes in milk
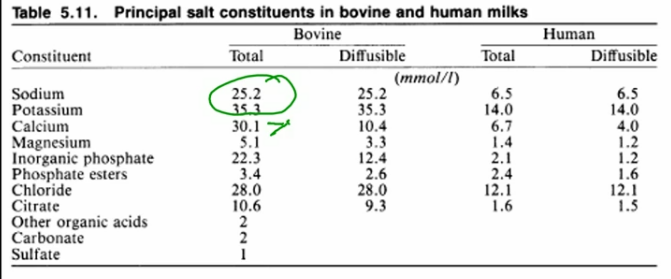
only a third of calcium is free ionized calcium and diffusible
typically bound to casein in cows
and citric acid in humans
in humans the highest is potassium and all of it is diffusible
Lecture 6 1-26: nutritional components in milk pt 2
topics
composition: proteins, lactose, lipids, minerals, vitamins, enzymes etc.
factors affecting composition: species breed, feed, stage of lactation
physical and chemical properties: density, freezing point, color, pH, acidity, flavor
bacteria
somatic cells and microorganisms - lactobacilli, history, significance in cultured products
calcium partitioning in bovine milk
introduction: milk
bovine total calcium 1120 mg/L
skim milk (99%)
casein is 66%
whey is 32%
alpha-lactalbumin (.15%)
lipid (1%)
human total calcium 280 mg/L
skim milk (36%)
casein 6%
whey 29%
alpha-lactalbumin (1%)
lipid 16-26%
sample used
sample 1: whole milk from NCSU dairy plant
sample 2: skim milk from NCSU plant
sample 3: ultracentrifuge skim milk at 100,000 x g for 60 mins
supernatant ultrafiltered in centrifuge overnight
collect sweet whey using a pipette
casein is in a clump at the bottom
ultrafiltration of supernatant
but it in a filter
the top is proteins
the bottom is diffusible proteins of the whey
procedure: preparation of samples
sample 4: centrifuge whole milk at 5,000 x g for 10 minutes
chill on ice to solidify fat
remove fat with a spatula
collect the skim milk fraction by pipette
procedure: preparation of samples
sample 5: pH of skim milk reduced to 4.6 using 1 N HCl
centrifuge at 5,000 x g for 10 min
collect acid whey using pipette
brings the casein down and forms acid whey
calcium values (experimental and literature)
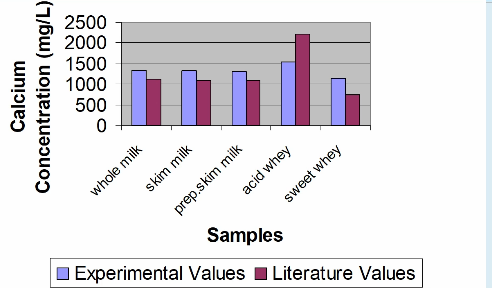
the acid displaces the calcium from the micelles, and it goes into the whey fraction
calcium distribution in fat, whey, and casein fractions
conclusion
milk components fractionate in different physical fractions
fat
cells
casein (suspended solids because of negative charge on the outside)
whey (water-soluble substances)
acid whey contained about one and half times more calcium than sweet whey
lactation and diet quality
lactations rigorous demands require a mother to intake enough energy and nutrients for maintaining homeostasis and synthesizing nutrient-rich milk for her offspring
poor quality diets may lead to poor milk quality and decreased milk yield
but diet differences do not always lead to milk composition changes
soluble milk components have multiple chemical forms
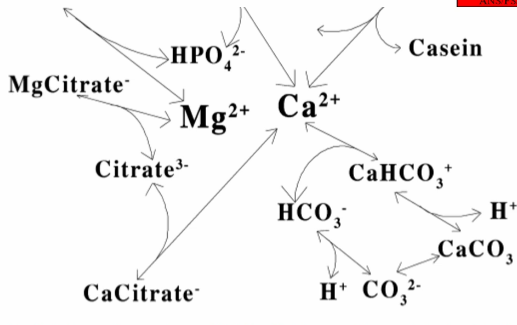
calcium will interact with anything negative in the milk
when calcium binds to something and makes it a neutral molecule it will no longer be soluble
citrate is a high in the negative fraction
the amount of citrate in the milk effect how much calcium is in the ion state and available for the carbonate fraction
by adding CO2 you can change the concentration of carbonate or bicarbonate
by changing the pH it will change the ratio of carbonate and bicarbonate
higher pH makes more carbonate
pulls calcium out and displaces the calcium in the calcium citrate form
magnesium and zinc can displace calcium
zinc can bind to the casein also
we can measure the free calcium, citrate, carbonate and pH to figure out where the calcium is
calcium secretion into milk
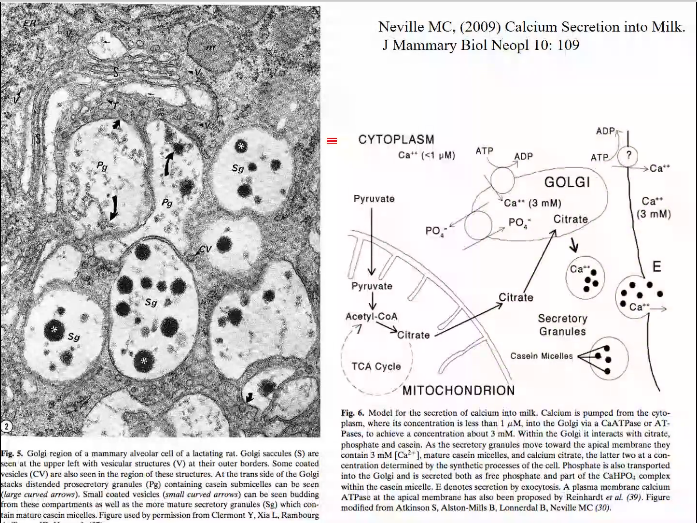
citrate is coming from the mitochondrial energy production and the citric acid cycle
TCA cycle
citrate is diffusible out of the mammary gland
specifically, out of the mitochondria and into the mammary gland in cows
in humans we use citrate as a carrier for acetyl CoA for a breakdown of fats in the cytosol
the remaining carbon portion of citrate after 2 carbons come off back into the mitochondria
cows can because they don’t have the enzyme
this is why cows have a higher concentration of citrate in their milk
the citrate diffuses into the Golgi apparatus to form casein and lactose
forms tiny casein particles in the secretory cells in the mammary
the calcium allows the casein molecules to be attracted to each other forming casein micelles
dependent on free calcium
minor components and micronutrients
non-protien nitrogen
nucleotides
nucleic acids in nucleosomes (particle of nucleic acid inside the cell; once it leaves the cell its called an exosome)
urea
free AA
enzymes
lipoprotein lipase
breaks down fat in milk
if you let milk sit the more free fatty acids there will be
lactoperoxidase
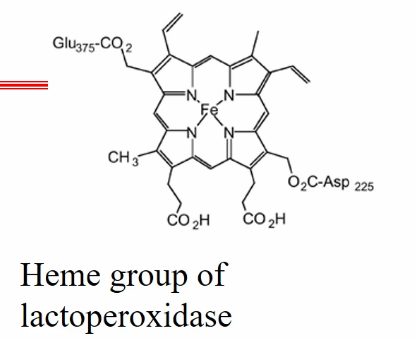
xanthine oxidase
can take unsaturated long chain fatty acid and oxidize them
alkaline phosphatase
changes the phosphorylation in proteins
casein is highly phosphorylated
exosomes: found in human milk
exosomes are membrane-bound extracellular vesicles (EVs) that are produced in the endosomal compartment of most eukaryotic cells
the multivesicular body (MVB) is an endosome with intraluminal vesicles (ILVs) that bud inward into the endosomal lumen. if the MVB fuses with the cell surface (the plasma membrane), these IVLs are released as exosomes
exosomes may transfer maternal DNA to the infant
could be a form of communication
small portion of DNA in a vesicle
portion of minerals in milk
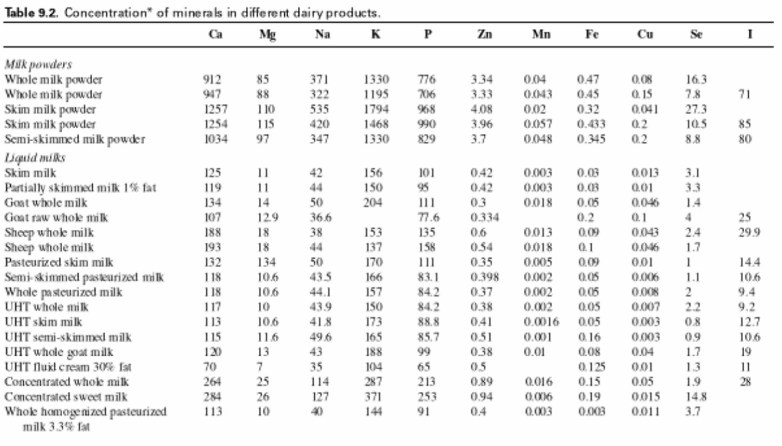
UHT = ultra-high temperature
processing and pasteurization
calcium is the highest and the zinc
Biological roles for minerals
vitamins
fat soluble vitamins
vitamins A, D, and E
water soluble vitamins
vitamins C, B1, B2, B6, B12, pantothenic acid (B5), niacin (B3), biotin (B7), folic acid (B9)
vitamin concentrations in different species
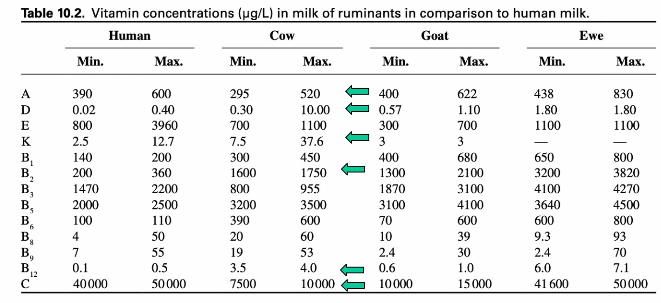
beta-creatine is found in plants and can be converted into vA and enter the fat fraction of the milk
making skim milk would significantly decrease vA and vD because the fat fraction is removed
if the cow is given hay during winter the dairy producer will add vA
also, if the cow is kept indoors then the milk will be deficient in vD
vD will be added to the milk
vK is needed for blood clotting
if low vK it is injected into human babies
cows tend to have high B complex vitamins
functions of vitamins in milk
vA: prevents eye problems, promotes a healthy immune system, is essential for the growth and development of cells, mucous, skin, bone and tooth health, reproduction and immunity
vD: strengthens bones because it helps the body absorb bone-building calcium
vE: an antioxidant and helps protect cells form damage. it functions in stabilization of cell membranes, support of immune function, protection of polyunsaturated fatty acids, and normal nerve development
vC: aka ascorbic acid; needed to form collagen, a tissue that helps to hold cells together. it is an antioxidant, it restores vE to its active form, it helped to synthesize hormones, it supports immune cell function, and helps in absorption of iron
thiamin aka B1: part of a coenzyme needed in energy metabolism. it also supports a normal appetite and nervous system function
riboflavin aka B2: part of a coenzyme needed in energy metabolism. it also supports normal vision and skin health
vB6 aka pyridoxine: part of a coenzyme needed in AA and FA metabolism. it helps to convert tryptophan niacin and to serotonin, and it helps make red blood cells
vB12: part of coenzymes needed to make red blood cells, and it important for nerve cell function
folate aka B9, folic acid, folacin: part of a coenzyme needed for synthesis of red blood cells. it is also needed to make DNA
niacin B3: part of coenzymes needed in energy metabolism. it helps maintain healthy skin and is important for nerve function
pantothenic acid: part of a coenzyme needed in energy metabolism
biotin: cofactor for several enzymes needed in energy metabolism, fat synthesis, AA metabolism, glycogen synthesis
factors affecting composition
breed
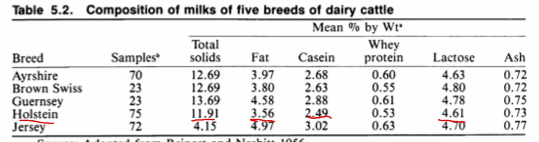
Holsteins make more but less
jerseys make more fats, and casein
diet and season
stage of lactation
stages of lactation changes in competition of bovine milk
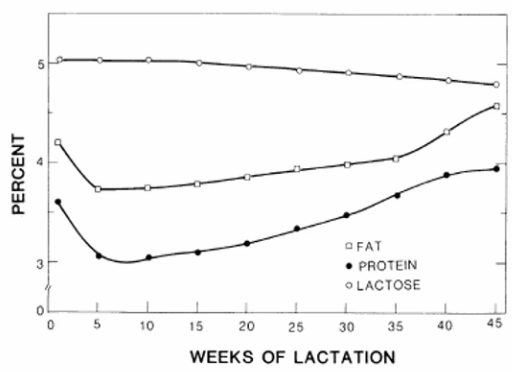
at first the milk is concentrated
lower protein and higher fat
later is more protein and less fat
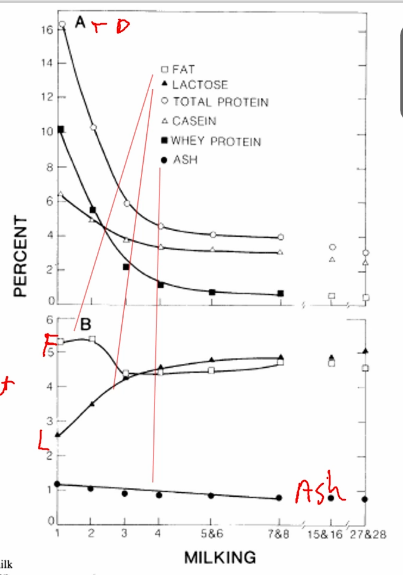
in colostrum not that much lactose so not that much water and concentrated
immunoglobins are high in the whey fraction
more whey than casein at first
milk fat
changes in milk fat characteristics
dietary manipulation
if you feed cow a lot of polyunsaturated fats then the milk will have a higher concentration of PUFA but it will not change the volume of milk produced
seasonal changes
seasonal and dietary changed in FA composition of human and bovine milk fat
when the person is synthesising fats it will be a short chain like 16:0
when the fat is in the diet longer chains are made like 18:1 and 18:2+3
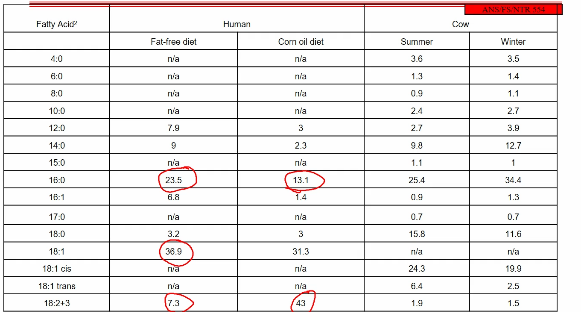
cows make more steric acid in the summer
cows will have more shorter chain FA in the winter because they are making it not getting it in their diet
physical and chemical properties
density
more or less fat
freezing point
early or late milk
depends on potassium, sodium, and lactase will cause a decrease on freezing point
pH
the balance between phosphate and sodium and calcium
titratable acidity
depends on uncharged proteins and inorganic acids
flavor
density of various fluid dairy products as a function of fats and solids-not-fat composition
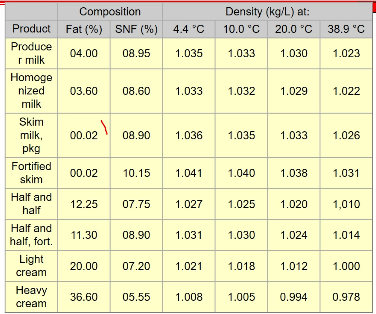
density decreases as fat increases
somatic cells and microorganisms
immune and epithelial cells from cow’s body
include lymphocytes, macrophages to protect the animal against bacteria
the epithelial cells sluff off as the milk is made
find the most at the beginning and end of lactation cycle
lactobacilli
evolved with milk
will form lactic acid and cause casein to be protonated
history
significance in cultured products
i.e. cheese and yogurt
bacteria
pathogenic
can cause souring in pasteurization
natural flora
affect shelf life and milk quality
original source of cultured dairy products
milk bacteria
bacteria in milk were traditionally though as contaminants from the outside as the milk was collected
bacteria is actually already there
mutualistic milk microorganisms may be dependent on coevolving with their mammalian host to thrive in milk
in raw milk some microbes are acid and bile resistant
different bacteria from cows’ milk
lactation and co-evolution between milk microbiota and mammals
diet and gut microbiome
diet can play a role on gut microbial diversity in mother and offspring
maternal impacts of milk
understanding milk microbiota
research emphasis on human milk oligosaccharides and its exclusion impacts with offspring development
milk of earliest mammals may be vulnerable to microbial proliferation because they were secreted onto skin versus nipples
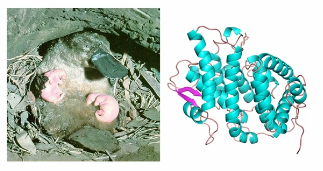
monotreme (platypus and echidna) = lactate of from armpits
that protein is known to be antibiotic in the platypus
bacteria would thrive in platypus milk
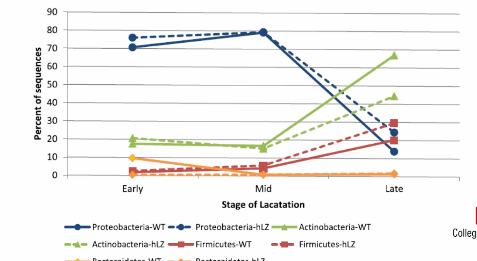
major phyla of raw and transgenic goat milk
transgenic goats expressing human lysozyme had decreased relative abundance of Actinobacteria compared to wild-type goats by late lactation, but most bacterial phyla were relatively unaffected by this antibiotic
Week 4 January 27
learning objectives
lecture 7 1-31: mammary embryology and comparative anatomy: lactation, milk, and nutrition
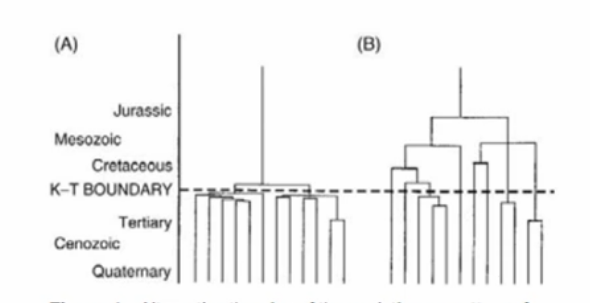
mammals where did we come from
mammals evolved from reptiles
one thought was because of the meteorite right outside the Yucatan peninsula (in the Caribbeans) during Paleozoic period
looking at the fossil records there was a shift in mammals and reptiles
happened between the cretaceous period and the Triassic period
though have been a global drop in temp, reduced plant growth, dust in the air
the dinosaurs could not regulate their temperature and many survived on plants
mammals
the classic classification is the lineic structure
looks at fossil records and compare it to other animals
looks at bone structure
and where the soft tissue has to be
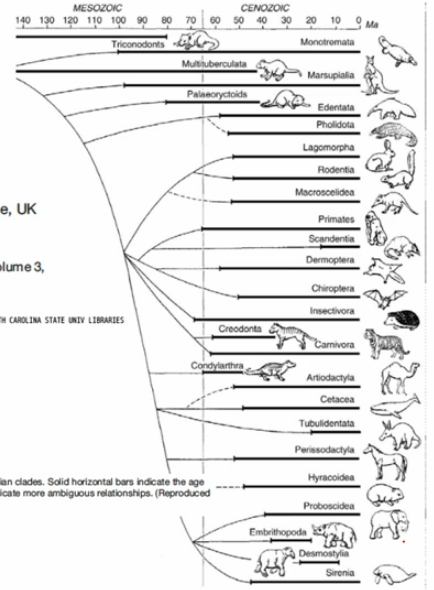
eutherian mammals give live birth and secrete milk
primates are more closely related to bats than rodents
Artiodactyla are the 2-hooved animals
cows, pigs, camels
ruminants related to hippos
lactation is a function of mammals (monotremes, marsupial, and eutherian)
mammary gland probably evolved form a sweat gland
why the abdomen though
that’s where the offspring typically sit
what other characteristics are unique to mammals that may have influenced the classification of animals
hair, live birth in offspring, and inner ear bones, homeotherms, more complex brain function, milk production, one bone in the lower jaw
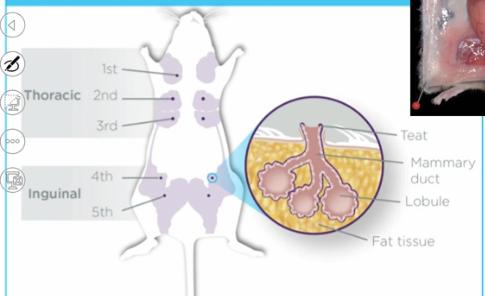
how do mammary structures and functions differ among mammals?
number of mammary glands
number of openings in the teat canals
placement of mammary glands
composition of the milk
milk storage within the gland to allow once per day or very frequent nursing
feeding from the mother creates bonds and induces socialization
why can’t a cow get breast cancer
a cow’s mammary system is not on its breast but abdomen
r-species or k-species
r- is large litter, multiple teats and mammary glands, normally don’t have as great of a survival rate, rapid growth
i.e. rabbits and mice
k- single or twins, have a greater chance of survival, requires more care from mother
i.e. elephants and whales
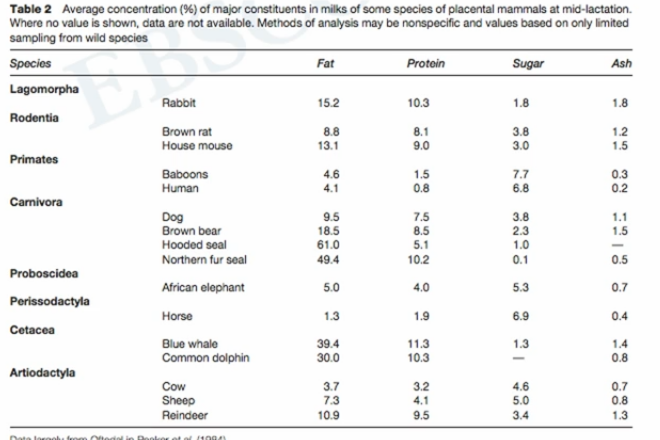
fat and protein tend to be high in the rapid reproducing animals and aquatic animals
anatomy
mammary development in embryo
in the mouse at day 10 the tissue will fold on itself
by day 12.5 there is a thickening of the cells on the skin forming 2 layers of epithelial cells
by day 15.5 a sprout forms
by day 18.5 branching happens in different layers: muscle and fat
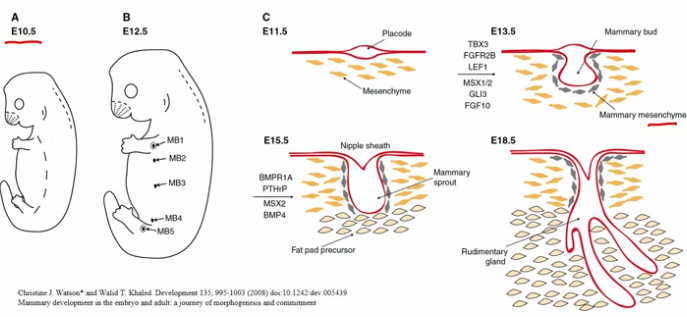
human fetal mammary growth
5 weeks: breast development noticeable in the embryo at 5 weeks of gestation
6 weeks: two milk lines are present, extending from the armpits to the inner thighs
8 weeks: lower milk lines disappear by several weeks
20-32 weeks: upper milk lines develop and form milk ducts by 20-32 weeks gestation
35 weeks: at the end of gestation, duct form openings in the nipples below the skin’s surface
38 weeks: before birth the nipples push outward and become level with skin
growth factors establish mammary epithelial and nipple cells
PTHrP and BMP signaling mammary bud outgrowth and nipple formation. PTHrP, which is secreted from mammary epithelial cells of the mammary bud, increases BMPR1A expression in the mammary mesenchymal cells (purple), which now responds to BMP4. this triggers epithelial outgrowth, elevates MSX2 expression, and inhibits hair follicle formation within the nipple sheath.
human mammary growth and development
mammogenesis
state of mammary gland from the onset of puberty and throughout pregnancy, when it develops to a functioning state
lactogenesis
during the last trimester of pregnancy, when milk synthesis and secretion is established
galactopoiesis
establishment of mature milk and throughout lactation
involution
occurs at the end of lactation, with the slowly returning to its pre-pregnant state
apoptosis when the tissue regresses
mouse adult:
a schematic of stages (A-F) of mammary gland development in the adult mouse, from pre-puberty through to pregnancy, lactation, and involution
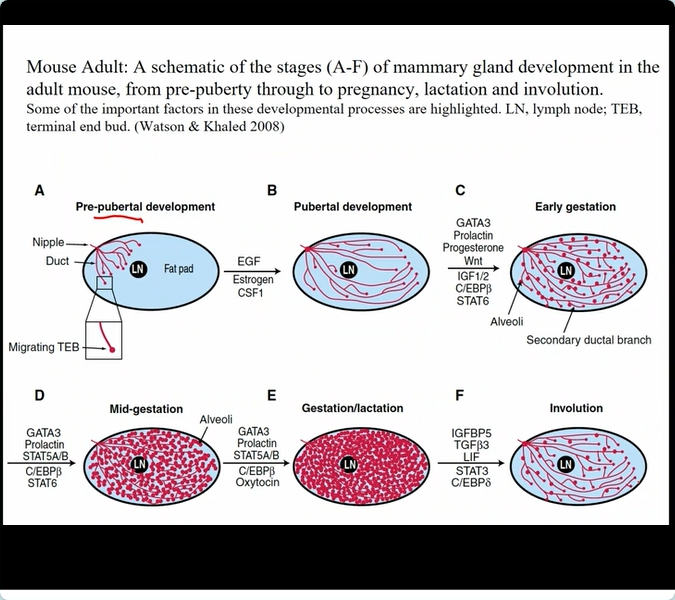
mouse mammary growth and development
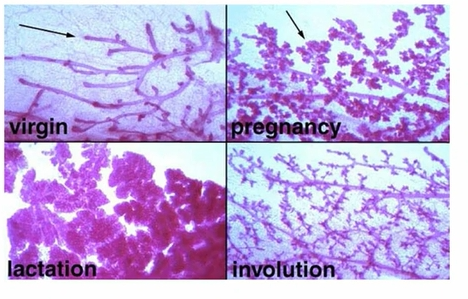
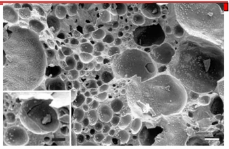
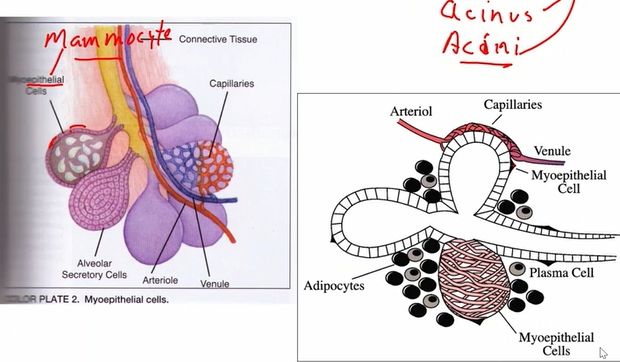
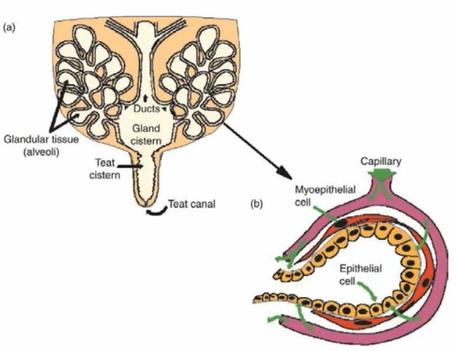
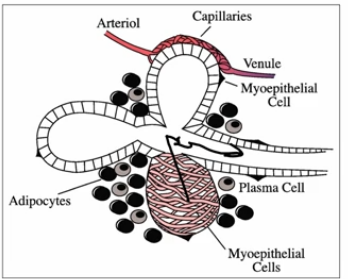
milk producing tissue: alveoli
alveoli = alveolus
acinus = acini
single layer of epithelial cells surrounds the duct aka the mammocyte
capillaries also surround the alveoli
alveoli cells are called secretory cells
milk is held until oxytocin comes along from the pituitary gland
causes the myoepithelial to contract
also has fat cells = adipocytes
and plasma cells for the immune system and antibody production
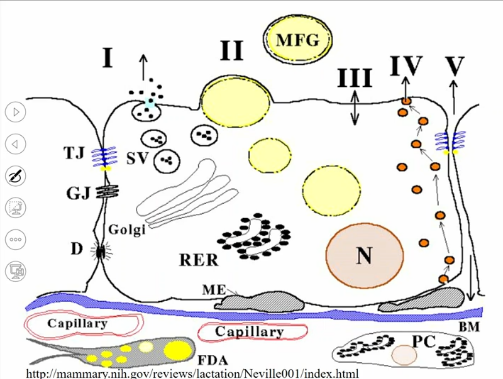
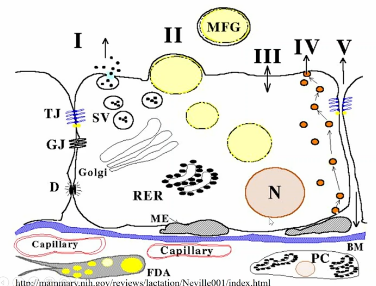
alveoli up close
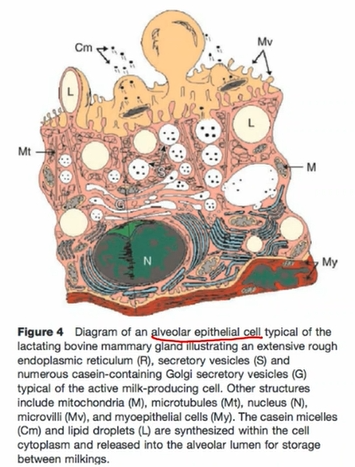
the Golgi apparatus makes secretory vesicles which is the beginning of milk
mammary gland anatomy
lobules to lobes
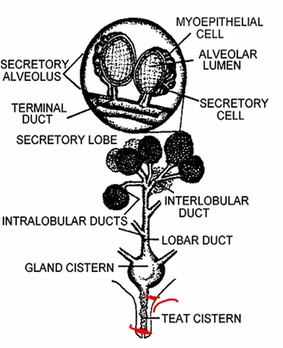
connective tissue and support
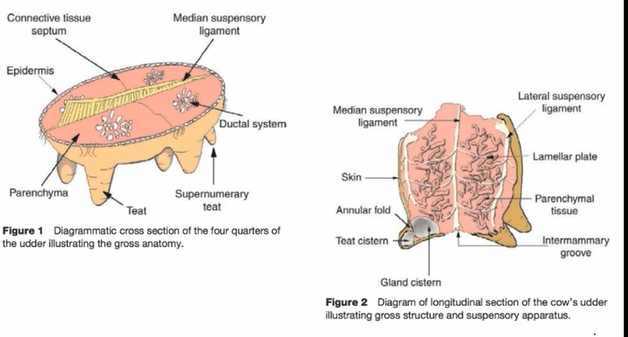
the secretory tissue is called the parenchyma
the mammary gland has a lot of blood flow
dense connective tissue
supernumerary teat is an extra abnormal teat
lateral suspensory ligament is a belly band, and the median is long wise of the cow
if the median ligament degrades in a cow as the get older it will be harder to milk because the teats will go to the side
the cow may be culled
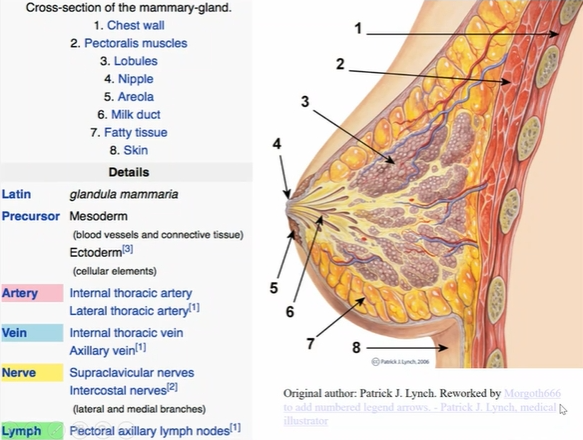
anatomy of the human breast
each breast is an individual exocrine gland that functions and develops independently to extract materials from the blood and convert them into milk
each lobe has its own opening through the skin of the nipple

lobes are separated by connective tissue
advantages of spreading mammary glands
allows multiple offspring to nurse at the same time
why do we not consume dairy products from mammals that aren’t cows?
their lactation cycles it too short
the mammary tissue is located in one spot in the cow
have a machine that goes all down their body
other mammals do not like being milked and will not let down the milk
they are not bred to be milked at a parlor
in sows to get milk scientist will have to inject them with oxytocin to have a milk let down response
udder support system
lactating cow: 25kg milk
45kg tissue
70 kg held by suspensory ligament system
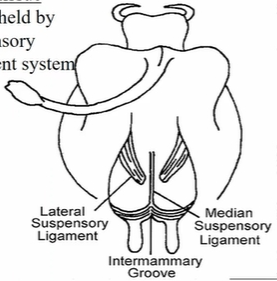
supportive tissue in the human
connective tissue
cooper’s ligaments provide a framework to support and attach the breast to the overlying skin and underlying fibrous tissue enclosing the muscles
subcutaneous fatty tissues
nerves
blood and lymph
beluga on the go - a litter would be a disadvantage
glandular tissue
glandular tissue transforms material in the blood and creates nutrients for the milk
functional part of the breast that produces and transports milk
parenchyma (secretory tissue and lobe)
functional parts of the breast
composed of smaller individual glands or lobuli
areola
the pigmented, circular area surrounding the nipple
the size and color vary from woman to woman
during puberty, menstruation, and pregnancy, it enlarges, and pigmentation increases
it partially covers underlying milk ducts
acts like the gland cistern with milk storage
nipple
circular smooth muscle fibers
closing mechanism for milk ducts
nipple pores
the ductule openings at the end of the nipple
teat
has one duct opening known as the streak canal or teat canal
keratin plug is formed to prevent bacteria from entering before the streak canal closes
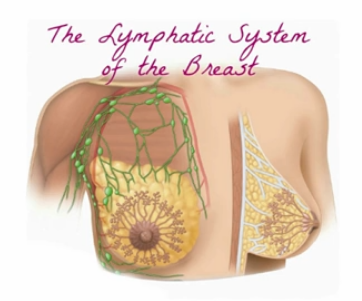
lecture 8 2-2: mammary embryology and comparative anatomy pt 2: blood, lymph, and nerves, allow milk synthesis and secretion
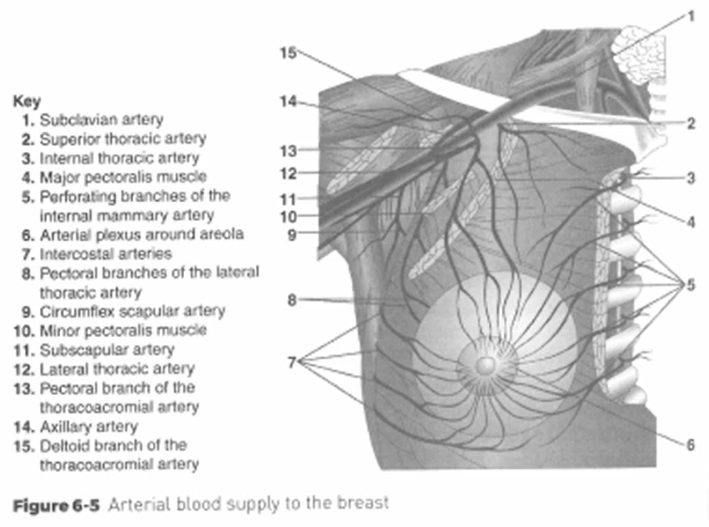
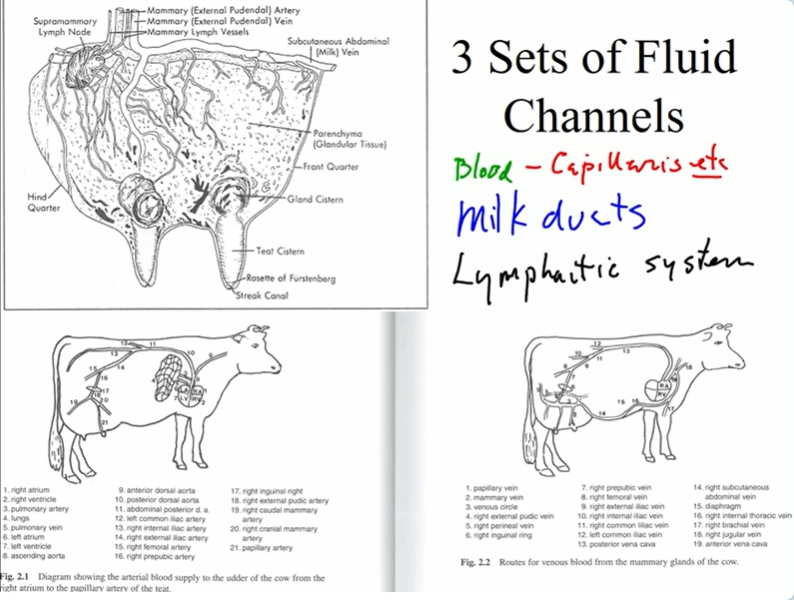
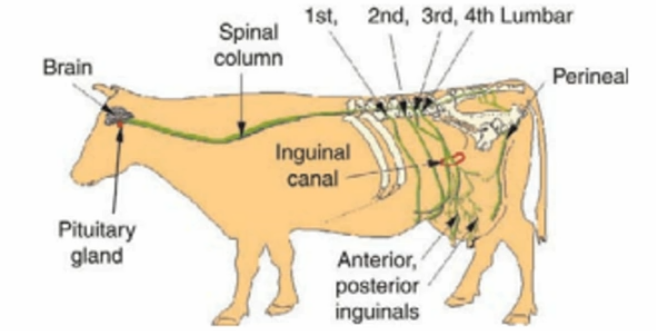
bovine vascular system - arteries
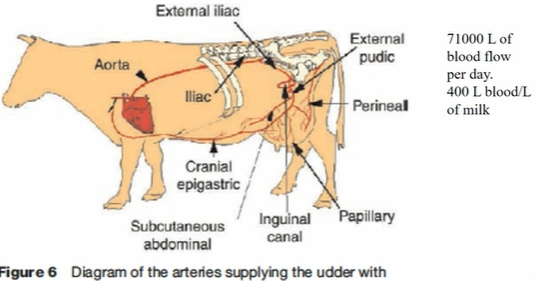
the blood supply branches mostly from the dorsal aorta → inguinal canal
another branch from the aorta is the cranial epigastric artery which also supplies the mammary tissue
the perineal feeds the back
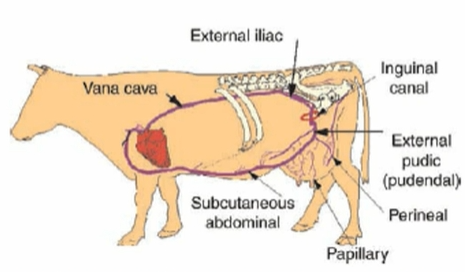
bovine vascular system - veins
most of the blood goes back through the subcutaneous abdominal vein
heart → arteries → arterioles → capillaries → venules → veins → heart
high pressure in the artery capillaries
forces nutrient into the tissues
mammary blood supply in humans
most of the blood comes from the subclavian artery
bovine lymphatic system
is a secondary return system from the mammary gland
large enough for bacteria to get through
for anything that is too large to flow through the endothelial cell wall
human lymph system
complex network of capillaries, thin vessels, valves, ducts, nodes, and organs
lymph is a thin, yellowish fluid
lymph nodes function as filters in the lymph vessels to trap bacteria
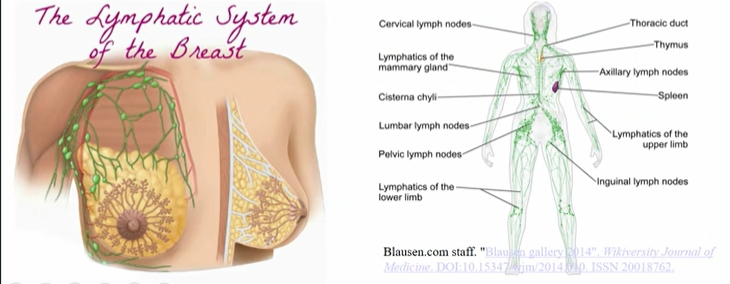
present throughout the body
spleen is connected to the lymph system
relationship between lymph, engorgement, and mastitis
if inadequate draining pressure will be built up in the breast
milk in the ducts → decrease flow of blood and lymph → fluids accumulate (edema) → risk of infection increases → mastitis
if you press down the dent will stay because of no blood flow
engorgement is the initial milk secretion
mammary cytology
mammocytes are known as lactocytes
engorgement might happen if the myoepithelial is not developed or is not strong enough to push out the milk
the lactocytes go from a flat squamous shape to a cuboidal shape as the start to produce proteins
the buildup of colostrum can cause engorgements
the plasma cells are producing immunoglobins
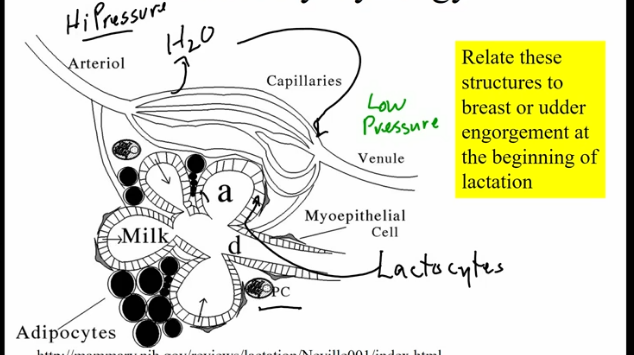
pressure from heart and osmotic pressure of the proteins
arteriol- → capillaries → venule out
collagen is a supportive tissue around the epithelial cells
allows for space when the alveoli expand
more pressure make fluid go out
which spaces at the cellular level are responsible for swelling and edema during tissue engorgement?
Extracellular fluid increases
Alveoli may reach capacity storing milk or colostrum
what are the tube systems in the breast
milk ducts
lymphatic system
blood, capillary, vascular system
responsive to nitric oxide
fluid channels
therapeutic breast massage in lactation for the management of engorgement, plugged ducts, and mastitis
focused gentle massage toward the axillae (near the armpit and is where most of the lymph node are)
alternating gentle massage and hand expression
nerve supply, what are the functions?
nerves on human mammary gland
sensory fibers innervate the smooth muscle in the nipples and blood vessels
3rd, 4th,5th, and 6th intercostal nerves
extensive innervation of the nipple and areola
most comes from the 4th intercostal nerve
innervation composed of both autonomic nerves and sensory nerves

neuro-endocrine reflex during suckling
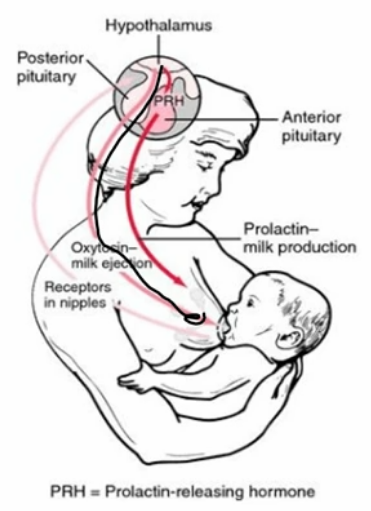
hypothalamus → PP releases oxy → oxy caused myoepithelial smooth muscle contraction
nursing also causes the release of prolactin releasing hormone from the hypothalamus → through portal vein system into the AP → PRH makes the AP release prolactin → prolactin cause milk production and synthesis
A primary function of innervation of the mammary gland is to being the milk let down response
neuroendocrine reflex
capillaries deliver hormones to the alveoli
myoepithelial cells contract when exposed to oxytocin
squeezing effect on the lobule, forcing milk down the ducts
myoepithelial cells multiply and increase in size during pregnancy and lactation
mammary gland study
understand terms used in the lecture and reading
define each in the context of it use and the concept that a term is trying to describe
Lecture 8: mechanisms of milk secretions: introduction
History and research tools
Palade and pancreatic acinar cells
dissolved away all the connective tissues to learn about the mechanism of the pancreas
same technique was used for the secretory cells
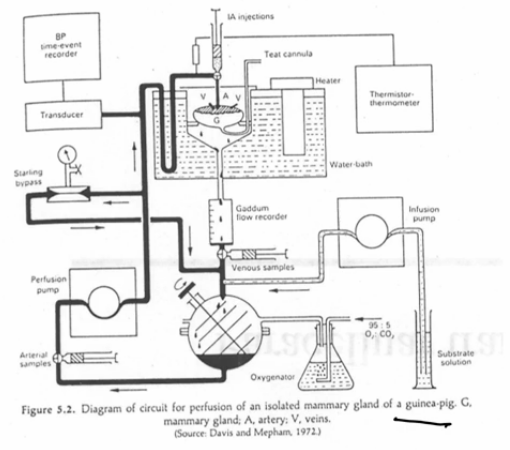
Linzell and Peaker - transplanted goat udder; isolated perfused udder
worked at the Hanner institute in Scotland in the 1950s-70s
also did perfusion studies
Isolated mammary tissue slices
isolated acini; grind and find cell distribution
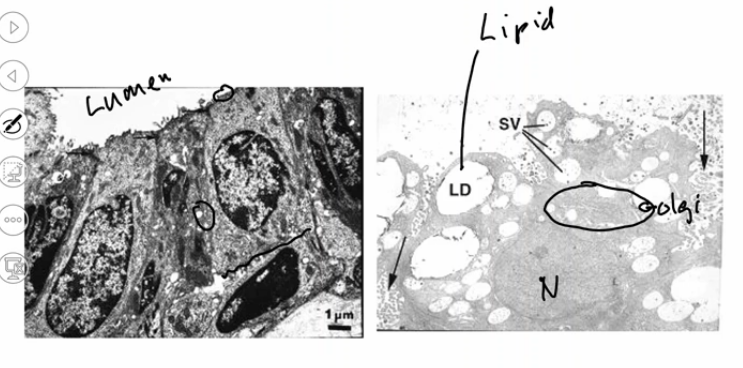
electron microscopy
cell culture and electrophysiology
mouse mammary
isolated perfused mammary gland model
used to see what is in the secretory glands
see what is coming in and out while lactating
collects extracellular fluid from the gland
infusion pump to add nutrients
and oxygen pump
will operate a couple of hours after the mammary tissue have been extracted
electron microscopy
see high resolution of tissues
the lipid droplets will end up as holes because they are washed out when the cells are fixed
the secretory vesicles get bigger as they get closer to the cell membrane
this is happening because of osmotic pressures
water will follow the lactose
cell culture model system
breast tissue (reduction mammoplasty or mastectomy) → chop and digest (collagenase/hyaluronidase) → culture organoids → heterogeneous epithelial cells and fibroblasts (differential trypsinization) → epithelial cells → selection → homogenous epithelial cells → cell senesce
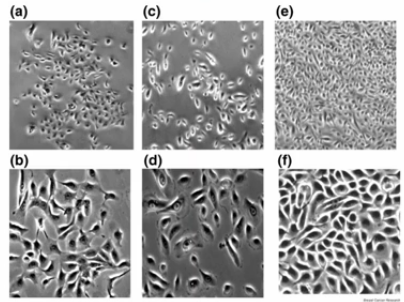
bovine mammary epithelial cell cultures for study if mammary gland function
cells grow to confluence
domes lift off culture dish - tight junctions
no 2-d milk syntheis
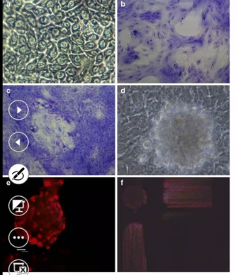
the circle spots in picture d and others are where the cells are not touching the culture plate and are polar
this means that the cells are secreting something down and the pressure is pushing the cells up
to wish they are making lactose
probably secreting ions and the water is following
five pathways for milk secretion
Golgi/ secretory vesicle pathway
lipid secretion
eccrine secretions of water and minerals
transcytosis
paracellular transport
Week 5 February 3
Lecture 9: Milk secretion mechanism
name one type of cell contained in mammary tissue that is not a lactocyte, (mammocyte), or mammary epithelial cell:
fibroblast, macrophage, lymphocyte, erythrocyte, myoepithelial cell, bacteria
isolated perfuesed mamary gland models
blood supply is replaced with artificle blood supply
have to put in oxygen and nutrients maintain body temperature
have to maintain transductor (pressure control)
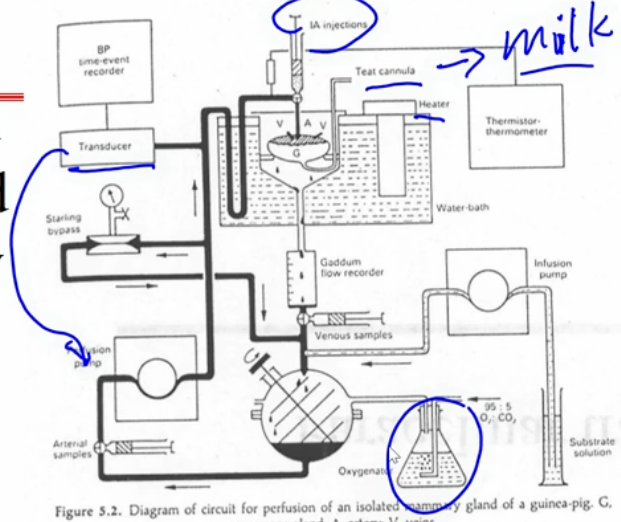
what goes in sample through the arterial port
what come out sample through the venous port
measure what is captured in the milk
operates on the Fick principle
the concentration that goes in the profuse fluid x flow in = concentration coming out x flow (the flow is flow of milk + the flow of venous)
 Knowt
Knowt