Clinical Chem Urinalysis
Urinalysis
- common laboratory test on urine sample
- non-invasive procedure to check for the composition of urine
- to screen, diagnose & monitor a wide range of health conditions/clinical disorders
- urinary tract infection, urologic disorders (e.g., calculi & malignancy), diabetes, kidney & liver diseases
Diagnostic Testing
Physical
- volume
- closely regulated by kidneys
- reflects overall fluid homeostasis
- Polyuria
- urine volume > 2000ml/day
- due to osmotic diuresis in diabetes mellitus, hyperthyroidism & infections
- insufficient secretion of / inability to respond to antidiuretic hormone (ADH)
- lack of hormone aldosterone
- after urination, it burns
- excessive intake / infusion of fluid
- renal diseases where the kidneys fail to concentrate urine
- the use of diuretics, alcohol & caffeine
- Oliguria
- urine volume <500ml/day
- as a consequence of conditions that decrease plasma volume, lead to dehydration, have impaired renal functions
- Anuria
- urine volume <100ml/day for 2-3 days despite high fluid intake
- follows oliguria in shock; acute tubular necrosis caused by exposure to toxic agents
- Colour
- normal: straw to dark-yellow colour
- presence of the pigment urochrome which is produced at a fairly constant rate
- colour intensity indirectly indicates urine concentration & state of hydration
- examine the urine sample under good light against a white background
- if the urine sample stands at room temperature, urochrome will increase & the colour may deepen
- Odour (not routinely reported)
- normal: faintly aromatic odour
- as the urine specimen stands, the odour of ammonia predominates
- unusual odour is indicative of diseases states
- fruity odour: ketonuria resulting from uncontrolled diabetes mellitus
- “mousy” smell: associated with phenylketonuria
- sweet-smelling like maple syrup: maple syrup urine disease
- “fishy” odour: bacterial infection (e.g. urinary tract infection)
- Clarity
- normal: clear or slightly cloudy
- via visual examination
- alkaline urine: precipitation of phosphates, carbonates
- acidic urine: precipitation of urates, uric acid, calcium oxalate
- foamy urine: presence of proteins
- substances that can cause cloudy urine: white blood cells, red blood cells, bacteria, fats
- may indicate inflammation or infection of kidneys, urinary & genital tracts, sexually transmitted diseases, kidney stones, diabetes
- specific gravity
- density of liquid compared with that of a similar volume of distilled water, when both solutions are at the same or similar temperature
- indicate the kidney’s ability to reabsorb water & chemical substances from the glomerular filtrate
- normal: >1.000 (1.002-1.035)
- influenced by the number and size of particles present
- e.g. ↑USG with the presence of large amount of glucose and proteins
- low USG: overhydration, diabetes insipidus, acute tubular necrosis, pyelonephritis
- high USG: dehydration, uncontrolled diabetes mellitus, acute glomerulonepritis, heart & liver failure
- constant fixed USG of 1.010 regardless of fluid intake
- chronic glomerulonephritis with severe renal damage
- loss of urine concentrating ability
- as a preliminary rapid screening of urine concentration
- urine osmolality → more reliable & accurate to evaluate kidney function, particularly the concentrating ability
Chemical
pH
- normal range: 4.5 - 8.0
- reflects the kidneys’ ability to regulate acid-base balance
- through regulation of hydrogen ions excretion
- only reliable when testing on freshly voided specimen
- influenced by diet & medications
Alkaline urine (pH >7.0)
- due to respiratory/metabolic alkalosis, presence of urease-producing bacteria, renal tubular acidosis, urinary tract infection
- promotes calcium-phosphate precipitation
- vegetarian diet, diets high in citrate, drugs i.e., sodium bicarbonate, potassium citrate & acetazolamide
Acidic urine (pH <7.0)
- diabetes mellitus, diabetes ketoacidosis, diarrhea, emphysema
- promotes the formation of uric acid & cystine kidney stones
- high-protein diet, intake of acidic fruits (e.g., cranberries), drugs (e.g., ammonium chloride)
Red blood cells (RBCs)
- normal: negative/<5 RBCs per ml
- Indications:
- tumours/trauma/infections/inflammation in genitourinary tract
- pyelonephritis, lupus nephritis, kidney stones, renal hypertension
- non-renal: hemorrhagic disorder, exposure to toxic chemicals, strenuous exercise
Hematuria
- presence of 3 or more RBCs per high-powered field in 2 of three urine samples
White blood cells (WBCs)
- normal: only a few
- Indications:
- bacterial infection in renal/genitourinary system, i.e., cystitis, pyelonephritis
- other non-infectious inflammatory disorders, e.g., glomerulonephritis & lupus nephritis
- presence of tumours and renal calculi
Pyuria
- excessive amount of WBCs in urine
- \
> 5 WBCs per high-powered field is considered abnormal
- \
Proteins
- normal: only in trace amount (<150 mg/day or 10mg/dL)
- Indications:
- physiological: strenuous exercise, dehydration
- renal diseases/failure: e.g., nephrosis, glomerulonephritis, polycystic kidney disease
- systemic disorders leading to increased level of serum proteins: e.g., multiple myeloma
Proteinuria (Albuminuria)
- elevated proteins in the urine
- ~1/3 of the total urinary proteins is albumin
- other proteins: Tamm-Horsfall mucoproteins (secreted by distal renal tubule), immunogloblin light chains, microglobulin, etc.
Glucose
- normal: negative
- Indications:
- diabetes mellitus, Cushing;s syndrome, Fanconi’s syndrome, liver & pancreatic diseases
- rare hereditary metabolic disorders
- gestational diabetes
Glycosuria
- the presence of reducing sugars in urine
Glucosuria
- presence of glucose in urine (most common type of ==GLYCOSURIA==)
Ketones
- normal: negative
- Indications:
- pregnancy, ketogenic diets, compromised nutritional intake
- uncontrolled diabetes mellitus (diabetic ketoacidosis), liver disease, certain forms of glycogen storage disease
Ketonuria
- high level of ketones in the urine
Bilirubin
- normal: negative
- Indications:
- liver dysfunction (due to obstructive jaundice, cirrhosis, viral- or drug-induced hepatitis, hepatotoxic drugs, toxins)
- biliary obstruction
- congenital hyperbilirubinemia
Urobilinogen
- normal: 0.1mg/dL - 1.0 mg/dL or 4mg/day
- Indications:
- ↑in hemolysis, hepatocellular disease (e.g., cirrhosis, hepatitis), severe infection
- ↓in bile duct obstruction, renal insufficiency, with antibiotic use
Leukocyte esterase
- normal: negative
- Indications:
- presence of neutrophils, either due to infection or other inflammatory processes, in urinary tract or kidneys
Nitrites
- normal: negative
- Indications:
- presence of a significant number of bacteria, and a urine culture should be performed
- UTI caused by nitrate reductase positive bacteria
Microscopical
- should be performed among those with persistent hematuria or proteinuria
Cells
red blood cells
- 0-5 cells/high power field
- confirming hematuria following positive dipstick results
- presence of dysmorphic red blood cells is suggestive of glomerular diseases
white blood cells
- 0-5 cells/high-power field (under high-power magnification)
- may also be examined under low-power magnification
- indicative of UTI, but culture is still needed for confirmation
epithelial cells
- increased squamous epithelial cells: originate from vagina, suggestive of contamination
- transitional epithelial cells: normal
- increased renal tubule cells: acute tubular necrosis & renal pathology associated to nephrotoxic agents
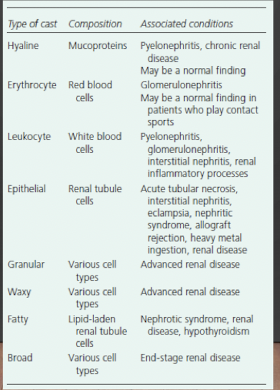
Casts
formed in the lumen of distal convoluted tubules & collecting ducts
via agglutination of protein cells or cellular debris
coagulum consists of Tamm-Horsfall mucoprotein with or without additional elements
prompt testing is mandatory (as it is dissolved in acidic urine within 30min or 10min in alkaline urine)
Crystals
- commonly found in urine; may or may not be pathologic
- supersaturation of solute componentys in urine initiates the crystallization
- acidic urine: calcium oxalate, uric acid & amorphous urate crystals
- alkaline urine: calcium phosphate, amorphous phosphate & ammonium magnesium phosphate crystals
- cystine crystals: abnormal; in those who have cystinuria & kidney stones
- tyrosine & leucine crystals: abnormal; suggestive of severe liver diseases
Bacteria
- absent in urine of normal healthy individuals
- reflects genitourinary tract infection or contamination of external genitalia
Dipstick
- results are available almost immediately
- convenient and cost-effective test to be performed at urgent care facilities, emergency departments, clinics or event at home
Fecal Analysis
- collected in a plastic hat-type receptacle
- should not be contaminated with urine or water
- should include any visible blood, mucus, pus, or parasites
- should be sent to the laboratory within 30-60 mins
Microscopial
Leukocytes
- especially neutrophils and monocytes
- as initial evaluation of diarrhoea of unknown aetiology/cause
Epithelial cells
- large amount indicates intestinal mucosa is irritated
Fats
- in the forms of triglycerides, fatty acids & fatty acid salts
- coupled with staining techniques prior to microscopic examination
- steatorrhea → excess fats in the stool (>60 fat droplets per high-power field)
- due to malabsorption syndromes or deficiency in pancreatic enzymes
- non-pathological: surgical resection of intestines & recent intake of excessive amounts of dietary fats
Meat fibers
- assess the efficiency of digestion
- presence in the stools indicates inadequate proteolysis
- usually correlates positively with steatorrhea
Parasites
- among individuals with intestinal disorders of unknown etiology or history of possible exposure to parasites
- i.e., roundworms, tapeworms, hookworms, & protozoa
- must be transported immediately to the lab
Chemical tests
Occult blood
- most frequently preformed
- to detect carcinoma
- numerous other pathological conditions, e.g., peptic ulcer, gastritis, inflammatory bowel diseases, diverticular diseases, hemmorrhoids, anorectal fissure, etc.
- stool samples are obtained after bowel movement or during rectal examination
- follow meat-free, high-bulk diet for 3 days before testing
- stop taking drugs that might alter the test results
Quantitative fats
- definitive test for excessive fecal fats
- evaluation is performed over 72-hour period
- controlled diet = percentage of solid material
- elevated level indicates intestinal malabsorption or pancreatic insufficiency
Trypsin
- normally not present in stool, except children <2 years old
- absence in children <2 years of age indicates pancreatic deficiency
Carbohydrates
- related to malabsorption disorders, e.g., celiac diseases
- excessive amounts appear in the stool
- evaluation: oral & intravenous (IV) glucose tolerance tests, and compare the results
- carbohydrate malabsorption syndrome
- normal on IV but not on oral glucose tolerance test
Urobilinogen
- rarely assessed on stool sample
- blood and urine samples are more commonly used
- ↓ in liver & biliary tract disorders; ↑in hemolytic anemia
Bile
- absent in faeces of normal adults
- otherwise occurs with diarrhea & hemolytic anemias
Microbiologic
Stool cultures
- evaluate diarrhea of unknown etiology or other systemic infections
- identify pathological types of bacteria
- sampling via rectal swab or during bowel movement
- must not be exposed to air or room temperature more than necessary