Week 6: Obsessive Compulsive and Related Disorders
Introduction to Obsessive-Compulsive and Related Disorders
Overview of disorders in the DSM-5 section.
Understanding the grouping of these disorders.
Contemporary models, cognitive-behavioral perspective.
Relationship to treatment approaches.
Discussion of controversial issues.
List of Disorders in DSM-5
OCD (Obsessive-Compulsive Disorder).
Body Dysmorphic Disorder.
Hoarding Disorder.
Trichotillomania (Hair-Pulling Disorder).
Excoriation (Skin-Picking) Disorder.
Substance/Medication-Induced Obsessive-Compulsive and Related Disorder.
Obsessive-Compulsive and Related Disorder Due to Another Medical Condition.
Other Specified Obsessive-Compulsive and Related Disorder.
Unspecified Obsessive-Compulsive and Related Disorder.
The lecture will focus on the first five disorders.
The DSM has avenues to cover human experiences that don't quite meet diagnostic criteria such as unspecified obsessive-compulsive and related disorder.
Obsessive-Compulsive Disorder (OCD)
Most familiar disorder in this section.
More exposure in media (films, television, etc.).
DSM-5 Diagnostic Criteria (Distilled)
Experience of obsessions and/or compulsions.
Experiences cause marked distress.
Experiences are time-consuming (over an hour a day) or significantly interfere with functioning and relationships.
Specify level of insight into these experiences (good to absent insight or delusional beliefs).
Question: Why isn't it a psychotic disorder if delusional beliefs are present?
Obsessions
Persistent thoughts, ideas, impulses, or images.
Experienced as intrusive.
Inappropriate to the circumstances.
Cause marked anxiety or distress.
Intrusive thoughts are common, but not always indicative of OCD.
Recognizing these as products of one's own mind is important.
Categories/Types of Obsessions
Fears of contamination (e.g., viruses).
Doubts (e.g., "Did I turn the iron off?").
Order/arrangement obsessions.
Sexual, horrific, violent, or blasphemous imagery.
Aggressive or inappropriate impulses.
Nonsensical thoughts or images.
Compulsions
Repetitive behaviors or mental/cognitive acts.
Examples: hand washing, checking, praying, counting, repeating words.
Goal: to prevent or reduce anxiety.
Examples of Obsession/Compulsion Pairing
Intrusive thought of contamination → compulsive hand washing.
Doubt about shutting the front door → repeated checking.
Pairing of obsession and compulsion may seem logical but can be excessive.
Muscle tensing routine example: intrusive thoughts of family being harmed paired with a muscle tensing routine.
Even with awareness of no logical link, compulsions may still occur due to perceived anxiety reduction.
The goal of treatment is to help the individual stop the routine and hold that anxiety knowing nothing bad will happen.
Common Types of Compulsions
Washing/cleaning.
Checking.
Repeating things.
Ordering.
Mental rituals like counting.
Reassurance seeking.
Compulsive shopping (mentioned but questioned if relevant).
Prevalence of Intrusive Thoughts and Ritualized Behavior
Most people experience intrusive, unwanted thoughts.
Dinner plans during a lecture are an example.
Sometimes thoughts can be pleasant.
More than 50% of the population engages in some level of ritualized behavior (e.g., checking keys before leaving the house).
Not all meet criteria for OCD (distress, time-consuming nature, impact on functioning).
General Population Study
Checking was the most commonly experienced OCD-like symptom.
12-month prevalence rates of OCD are about 1% to 2% (US data, similar in Australia).
No difference in prevalence rates between male and female adults.
Late adolescence, early adulthood is the average age of onset, but childhood onset and later adulthood onset are not unknown.
OCD often follows a fluctuating course, depending on external stressors.
In about 50% of cases, it's chronic.
Childhood Onset
Not everyone with adult OCD reports symptoms in childhood (1/3 to 1/2 do).
Childhood onset OCD is more common in boys than in girls.
Obsessions vs Compulsions
Around 90% experience both obsessions and compulsions.
Some have obsessions with more cognitive or behavioral compulsions.
Some describe compulsions without obsessions.
Terminology
OCD is part of public discourse and diminishes the experience.
Concept creep (clinical language drifts into non-clinical space).
Symptom Types
Aggressive and violent-related symptoms: More likely in women.
Sexual or religious-type symptoms: More likely in men.
Checking is the most commonly experienced type of symptom.
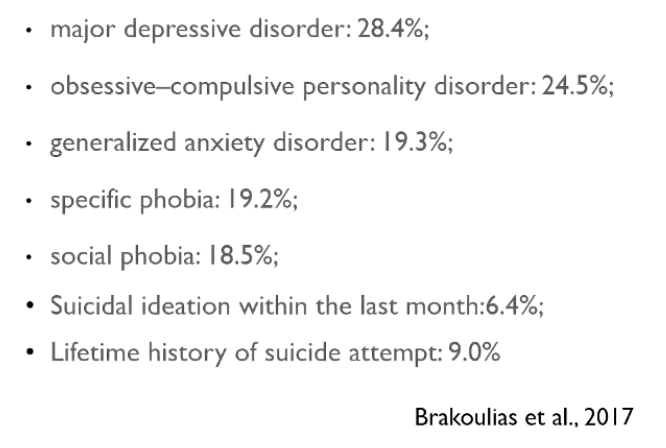
Comorbidity
Comorbidity = experiencing OCD and at least one other diagnosable mental disorder.
Most commonly diagnosed comorbid disorder = major depressive disorder.
Suicidal ideation and history of suicide attempt is not unknown, ten percent concerning rates.
Intrusive thoughts, especially violent imagery can be highly distressing.
Causes of OCD
Multifaceted - Combination of factors.
Learned responses.
Early childhood experiences.
Critical learning incidents > Maladaptive beliefs about responsibility, control.
Family history of OCD is there. some are linked to genes.
Mutations in hSERT gene linked to OCD
Brain structure and function impacted but can't diagnose with MRI.
Serotonin can have involvement, SSRIs can reduce symptoms in short term.
Neurocognitive/neuropsychological functioning deficits (executive functioning, memory), but not diagnostic, standard deviations overlap.
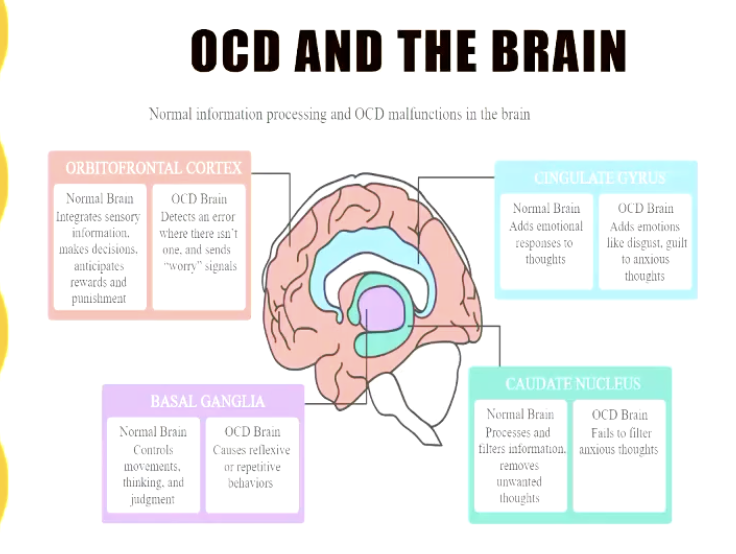
Cognitive behavioral Model for OCD
Developed by Paul Salkoskis. 1985
Premise: INTRUSIVE thoughts are NORMAL.
Place MEANING on these thoughts and ADD additional ATTENTION.
RESPOND and REDUCE intensity -> hyper-vigilant.
Triggering events increase anxiety and compulsions can be a response.
Compulsions WORK in short term, but lead to be hyper-vigilant to intrusive thought again.
Self-perpetuating cycle.
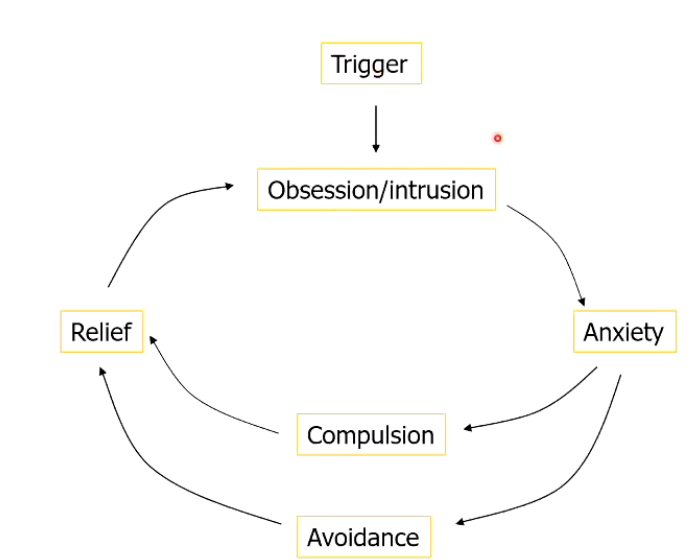
Response to anxiety is avoidance.
Avoid situations that trigger thoughts.
Super effective in short term -> safety behavior.
Cognitive behavioral Model Example
LETTER in the Mail
Worried touched by someone with HIV -> Infection pass to family, hold responsible
Results in anxiety, can't tolerate these thoughts.
So avoid touching things and washing is employed, super effective in the moment.
Over time triggers are not required and hand washing and avoidance occurs left, right and center.
Evaluation of Intrusive Thoughts:
Evaluate if overly important must address.
The thoughts are highly threatening, or something bad will follow.
The person needs to be able to control their thoughts > intolerable.
The thoughts are associated with certain perfection, and it must be certain the bad event will not happen so if not, one must act responsibly.
Must do these actions perfectly, or it could come True, perfection, control are common amongst those with OCD.
COVID-19 Impact
Restrictions > impacts from sanitizer and masks.
Symptom Worsening.
Some cases became the central focus of those with OCD.
Specialty care was effective for those with OCD.
Body Dysmorphic Disorder (BDD)
Diagnostic Criteria
Preoccupation with one or more perceived defects or flaws in physical appearance that are not observable or appear slight to others.
At some point, the individual has performed repetitive behaviors (e.g., mirror checking) or mental acts in response to the appearance concerns.
The preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Previously dysmorphophobia
Features
Preoccupied with perceived defects in physical appearance.
Describing themselves looking like monsters and being hideously ugly.
Focus one area or all of the body on a shift basis.
Intrusive unwanted difficult to control.
Compulsive mirror checking, grooming, reassurance etc.
Muscle dysmorphia, concern body is too small
How common is BDD
Under diagnosed, go to dermatologists and plastic surgeons first.
Often seen amongst patients with cosmetic surgeons, maxillofacial surgeons.
Waxes and Wanes, also impacted by functional status of that individual.
No overall differences from main and female prevalence rates.
Medical assistance to rectify
Males - Genitalia more likely, females comorbid with eating disorders more likely
Impact ranges from moderate to servere>incapacitating, can lead to job and university limitations
BDD can be distressing to others, especially when asked to provider reassurance >shared responsibility
What makes some people so focus and others not, cognitive differences?
There are specific cognitions endorsed by BDD over no BDD?
If the appearance defective then I am worthless is more BDD than normal
Mirrors generate more anxiety compared to someone without BDD.
People are more likely to return or be unhappy with procedures after treatment.
It is important to screen people at Cosmetic surgeons
Culture > Societal influences, eating and muscle dysmorphia can be viewed with different lenses
Social media > increasing focus with increased prevalence to BDD
Hoarding Disorder
Persistant difficulty discarding or parting with possessions regardless of actual value.
Distress linked to discarding them and need to save > accumulate.
Accumulate possessions and this clutter can take over the house or rooms.
Can be unlivable or the person is resistant to discarding objects.
Hoarding can cause distress, sometimes with impact on the family, and they recognize it as problematic.
Hoarding the impairment on the functioning of the individual.
It became a standalone disorder with DSM 5, previously OCD.
Estimates 2-6 %, more common older adults. Some have varying levels of insight.
Affects more males
Females show up more often.
Adults are older than young adults.
Linked to needing control over possessions, concern over memory.
Possessions have human qualities can generate meaning (bread bag clip).
Bottle tops, newspapers, electronic information can hoard, all trigger people.
Is the hoarding behaviour something learned from child, genetics or the environment. It can be familial
Creates lots of fire danger and the possibility of people not being able to evacuate or get to safety.
Can be very disruptive and ruptures in functioning and relationships.
A variant that keeps animals, sometimes the people want non-conditional animals so there are positives. Everyone suffers with animal hoarding.
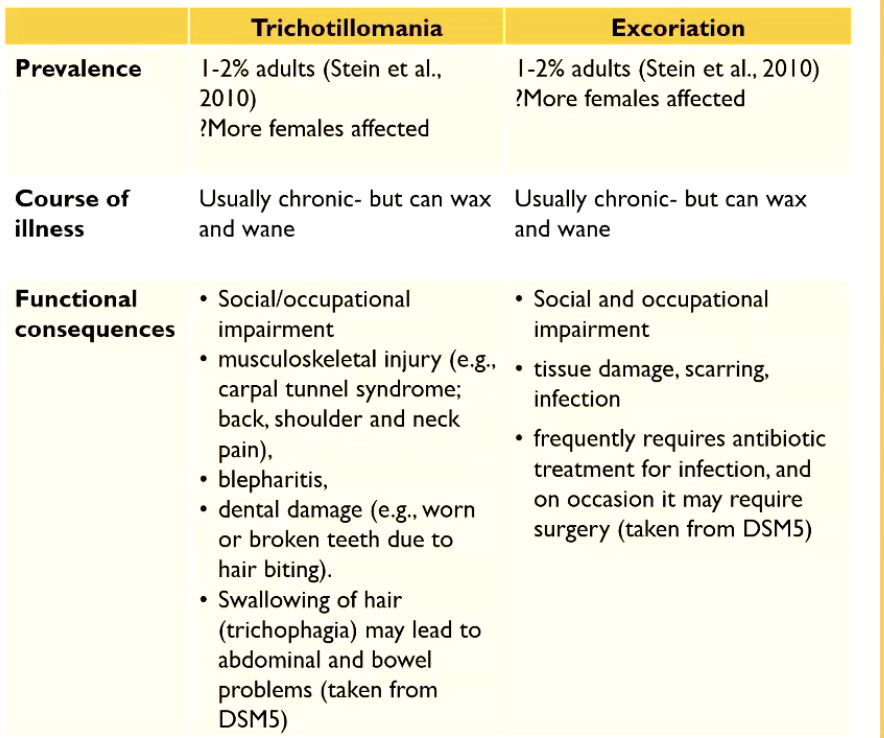
Trichotillomania and Excoriation
Trichotillomania means hair pulling.
Pull their hair out and create lots of bald spots.
They feel that they can't stop the hair pulling.
Causes distress and limitations on their functions.
Hair on the head is most common, but can apply to eyelashes or eyebrows.
They will also camouflage and hide what happened> hats or sleeves.
It is not a good thing as they will inflame this, and it hurts the person pulling them.
Skin picking excoriation, picking the skin and not being able to stop to their skin.
Trying to camouflage it as the hair pulling above.
Very similar behavior.
Research into these is light.
Wax and Wane is not super studied, however impacts the world.
People participate because they can participate easily.
It can: Alleviate pain, it can relieve or generate boredom or trigger + feelings> translate state.
Can be a tension release strategy is useful to highlight.
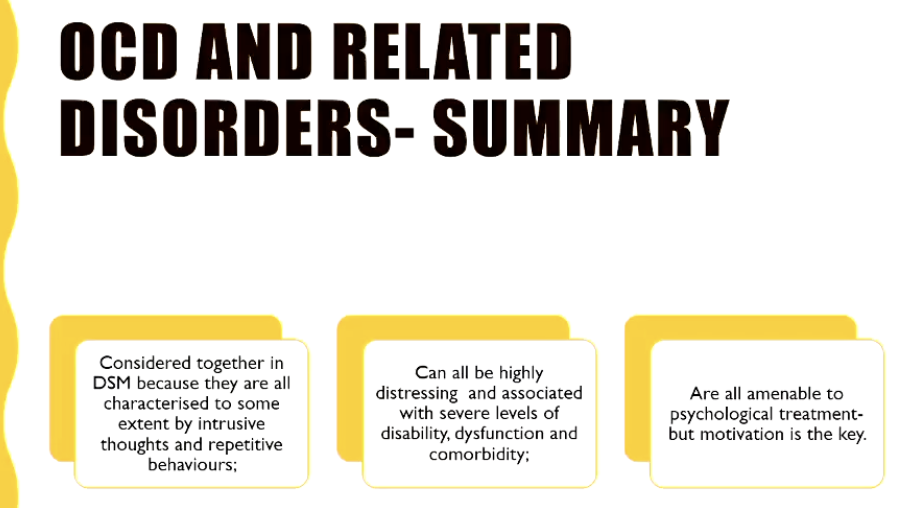
Conclusion
All disorders have the intrusive thoughts as a central theme.
DSM brought them together as they are all linked through intrusive nature, compulsions.
Treatments come from the same psychological perspective.
EXPOSURE therapy + prevent compulsion is the key>
Involves learning new associationsFeared stimulus = dangerous and intolerable
Feared stimuli = safe and tolerable
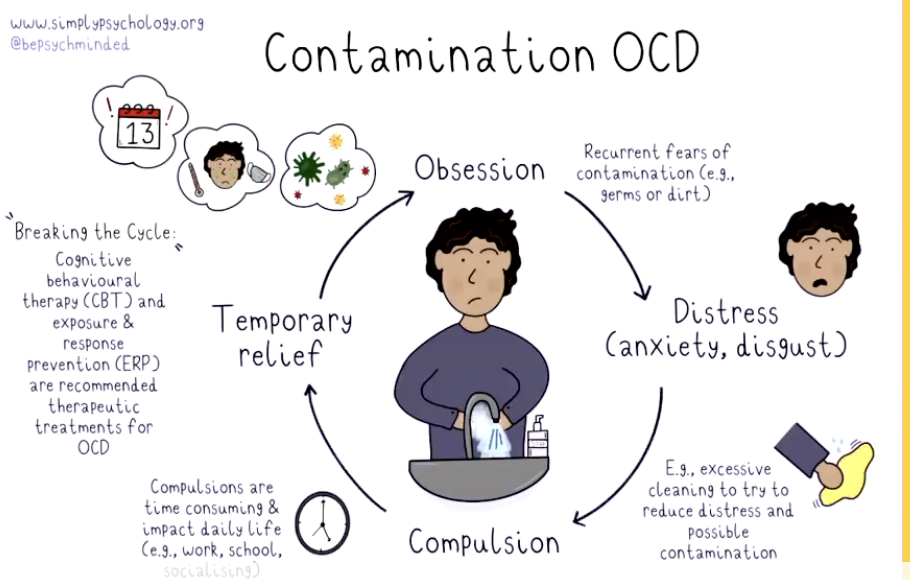
That anxiety is associated prevent actions and change.
Someone with OCD is afraid of x, clean, fear a stimulus is INtolerable or dangerous create new associations in this scenario.
IN VIVO exposure works here, and the new associations are not helpful actions.
Patient needs to learn and not make the same decisions again as they did again