CHAPTER 11_Gas Exchange in Humans
1) Features of Gas Exhange
Gas exchange surfaces vary across organisms, adapted to their size and environment. Despite differences, all gas exchange surfaces share common features that maximize gas exchange efficiency:
Large surface area, for fast gas diffusion
Thin walls to minimize diffusion distance → making it shorter
Good ventilation, with air, to maintain diffusion gradient
Good blood supply to sustain high concentration gradients for faster diffusion
2) The breathing System
Nasal Cavity
Trachea
Pleural Cavity (filled with fluid)
Lung
Bronchus
Intercostal muscles
Ribs
Bronchioles → alveoli
Diaphragm
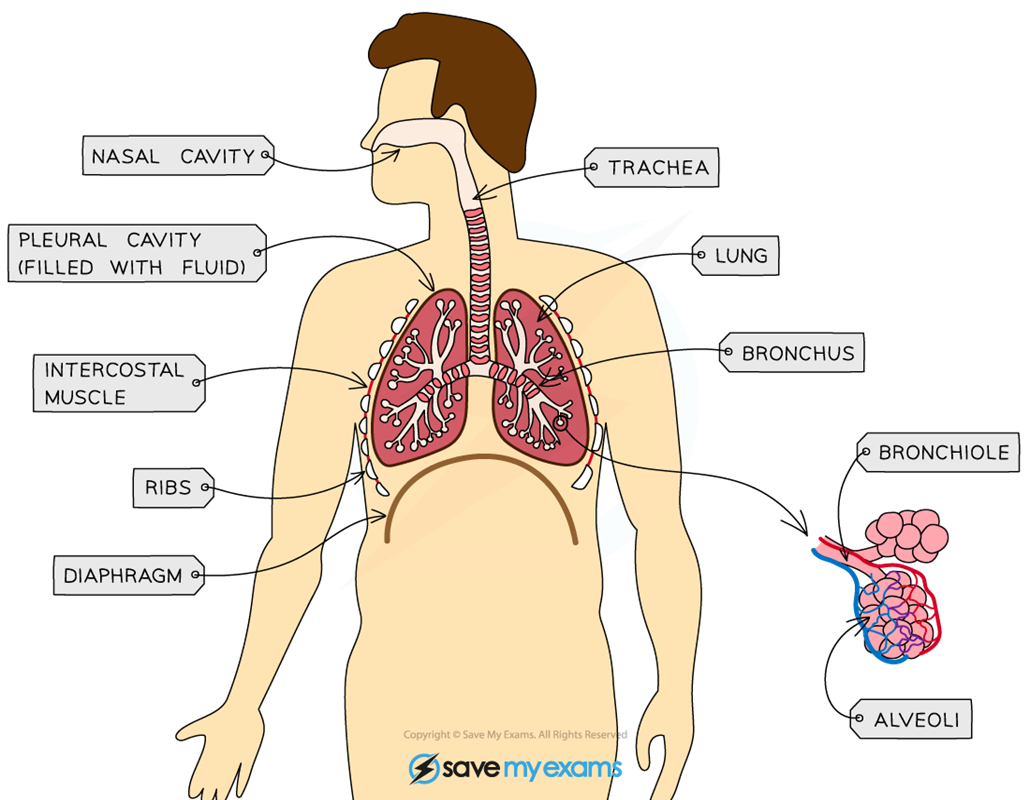
STRUCTURE | DESCRIPTION |
Ribs | Bone structure that protects internal organs such as lungs |
Diaphragm | Sheet of connective tissue & muscle at bottom of thorax that helps change volume of thorax to allow inhalation & exhalation. |
Intercostal muscles | Muscles between ribs which control their movement causing inhalation and exhalation. |
Trachea | Windpipe that connects mouth and nose to lungs |
Larynx | Also known as voice box when air passes across here we are able to make sounds. |
Bronchi (PL) | Large tubes branching off trachea with one bronchus (singular) |
Bronchioles | Bronchi split to form smaller tubes called bronchioles, in lungs, connected to alveoli. |
Alveoli | Tiny air sacs where gas exchange takes place |
3) Investigating differences in Inspired & Expired air
Investigation to inspect differences between inspired and expired air:
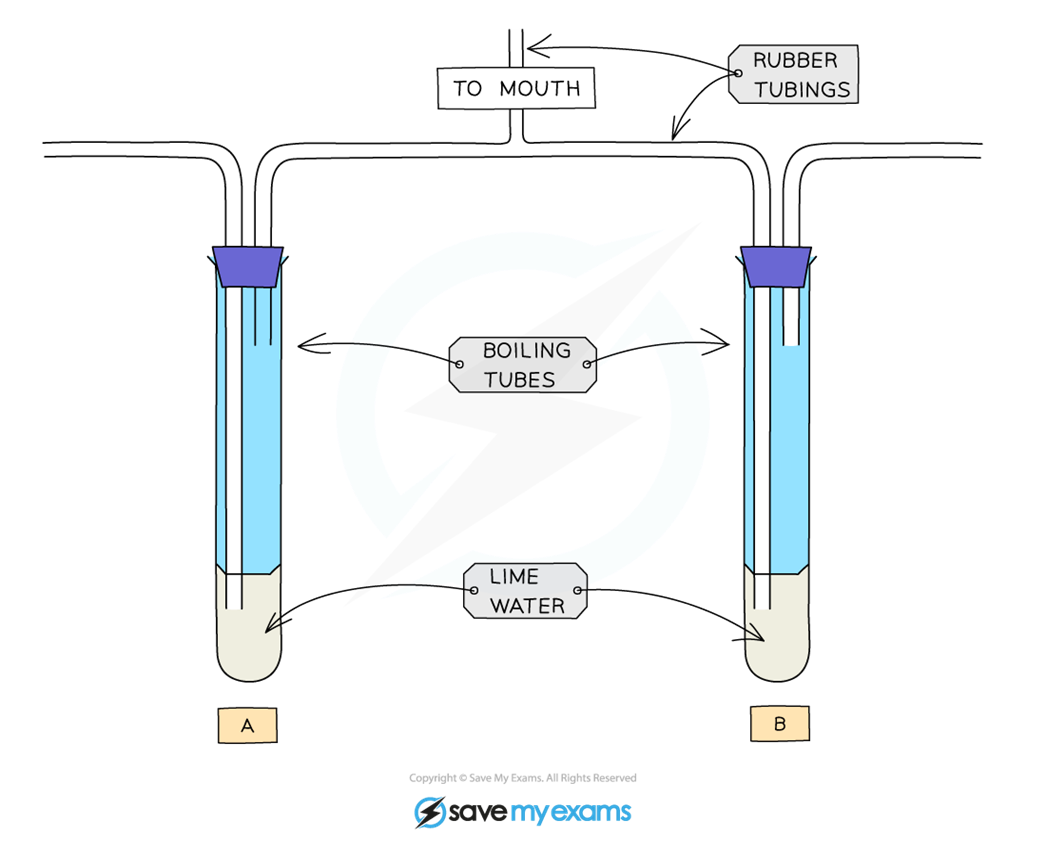
Wehn we breath in, air drowns through the boiling tube A
When we breath out, air is blown into the boiling tube B
Lime water is clear but becomes cloudy/ milky when carbon dioxide is bubbled through it.
Lime water in boiling tube A remains clear but limewater in boiling tube B becomes cloudy.
→ This shows us that the percentage of CO2 in the exhaled air is higher than in inhaled air.
Differences in Inspired and Expired air
Gas exchange in alveoli changes the composition of air.
Inhaled air has 20-21% oxygen
of which only 4-5% is absorbed
so exhaled air has 16% oxygen
CO2 in inhaled air is 0.04%
exhaled air holds 4% CO2 due to diffusion from the blood
Exhaled air has more water vapour & is warmer than inhaled air
GAS | INSPIRED AIR | EPIRED AIR | additional notes |
Oxygen | 20 - 21% | 16% | only 4-5% is really absorbed into the bloodstream Reason for difference:
|
Carbon dioxide | 0.04% | 4% | CO2 diffuses into the alveoli from the blood Reason for difference:
|
Water Vapour | Less | More | exhaled air is more humid |
Temperature | Cooler | Warmer | exhaled air is warmed by the body |
Nitrogen | 78% | 78% | - |
4) Investigating effects of Physical Activity on Breathing
Exercise increases breathing rate (frequency) & also the depth (amount)
At rest: Count breaths per minute & measure the average chest expansion, over 5 breaths with a tape measure
Exercise for at least 3 minutes
After exercise: repeat the breath count & chest expansion measure again
→ Both will have increased post-exercise
Explaining the Link between Physical Activity
During exercise, breathing rate & depth increases, because muscles need more oxygen for aerobic respiration & to remove CO2.
If oxygen demand isn’t met, muscles respire anaerobically, producing lactic acid.
Lactic acid lowers cell pH & can denature enzymes, so it must be removed
→ it’s removed using oxygen: called repaying oxygen depth
The longer it takes for breathing to return to normal, the more lactic acid was made & the greater the oxygen depth.
Mechanism for increasing breathing during exercise
During heavy exercise, respiration in muscle cells increases, producing more Co2 as a by-product
→ this CO2 diffuses out of muscle cells into blood plasma
→ the increase in CO2 lowers blood pH slightly, making it more acidic.
As blood circulates to brain, chemoreceptors in medulla oblongata detects the raised CO2 levels & drops in the pH.
Chemoreceptors are specialized cells that monitor chemical changes like gas levels & pH in the blood.
In response, the brain sends nerve impulses to diaphragm & intercostal muscles, causing them to contract more frequently & forcefully.
This increases both the rate & depth of breathing, improving oxygen intake & CO2 removal to support higher respiration rate in muscles.
5) Identifying Intercostal muscles
Muscles can only pull, not push, so two sets are needed to move the rib cage.
One set pulls the rib cage up: the other pulls it down
like a push and pull factor
External Intercostal muscles are located on the outside of the ribcage
Internal Intercostal muscles are located on the inside of the ribcage
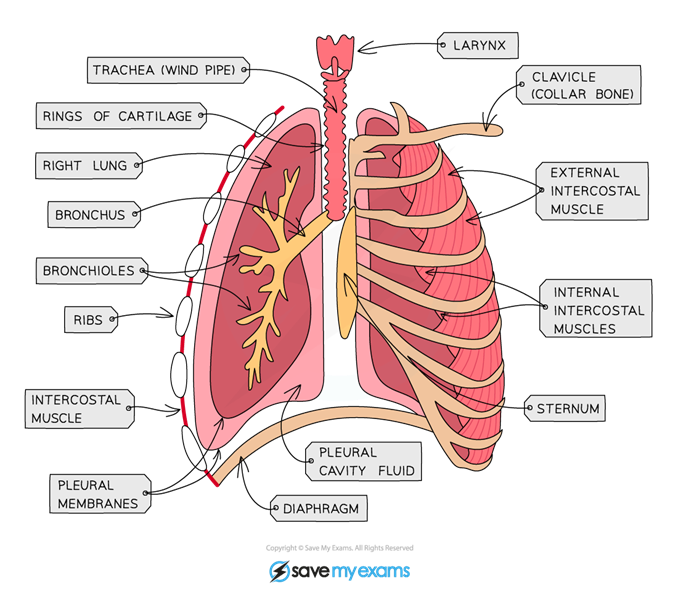
6) Function of Cartilage in Trachea
Rings of cartilage surround the trachea (and also bronchi)
The function of the cartilage is to support the airways & keep them open during breathing.
If they were not present, then the sides could collapse inwards, pressure breathing and the pressure inside the tubes drops.
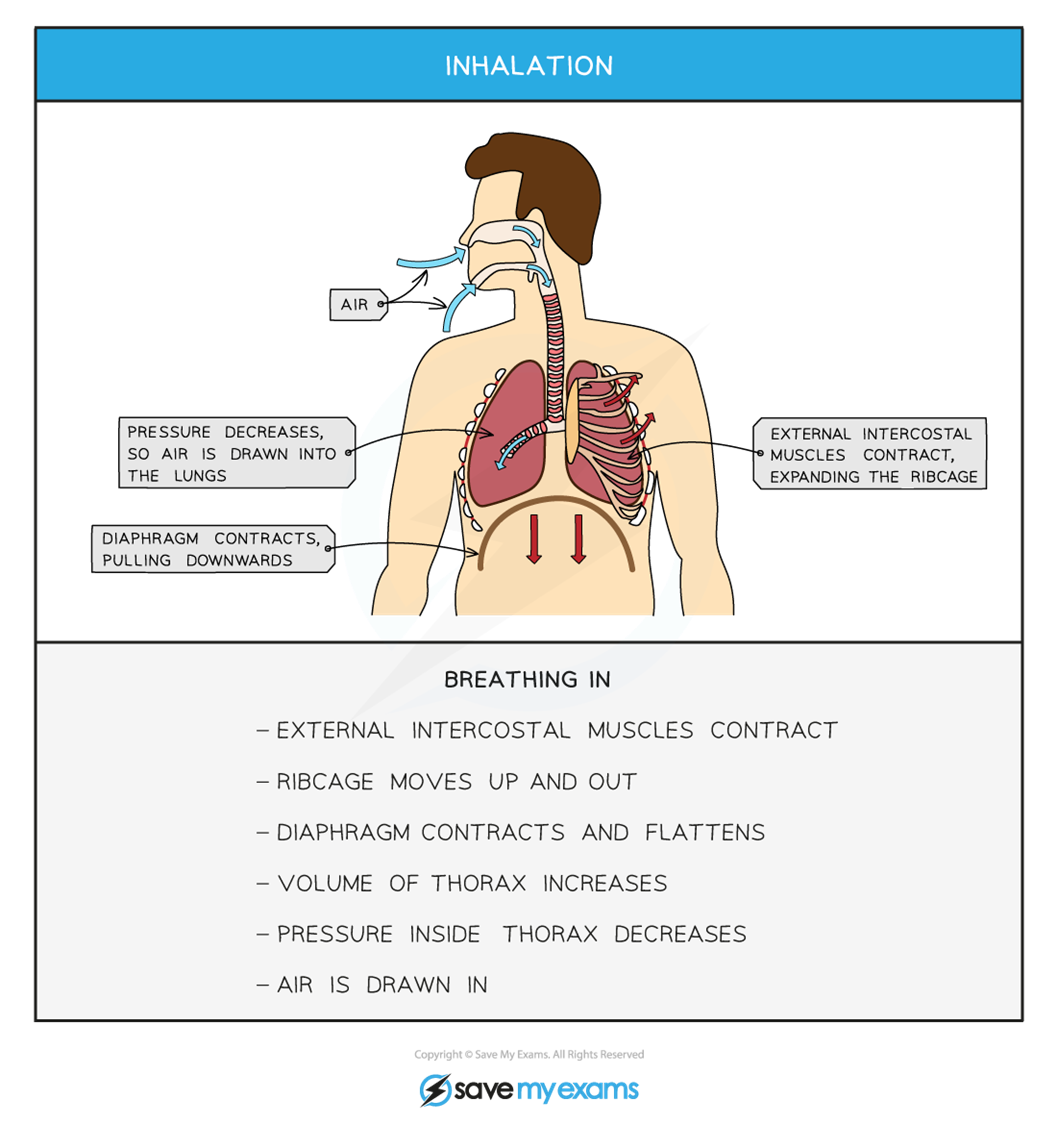
7) Volume & Pressure changes in the Lungs
The Diaphragm, a thin muscle separating chest and abdomen, controls lung ventilation:
A → Inhalation: Diaphragm contacts and flattens
I. Thorax volume increases
II. Air pressure inside the lungs drops
III. Air is drawn in
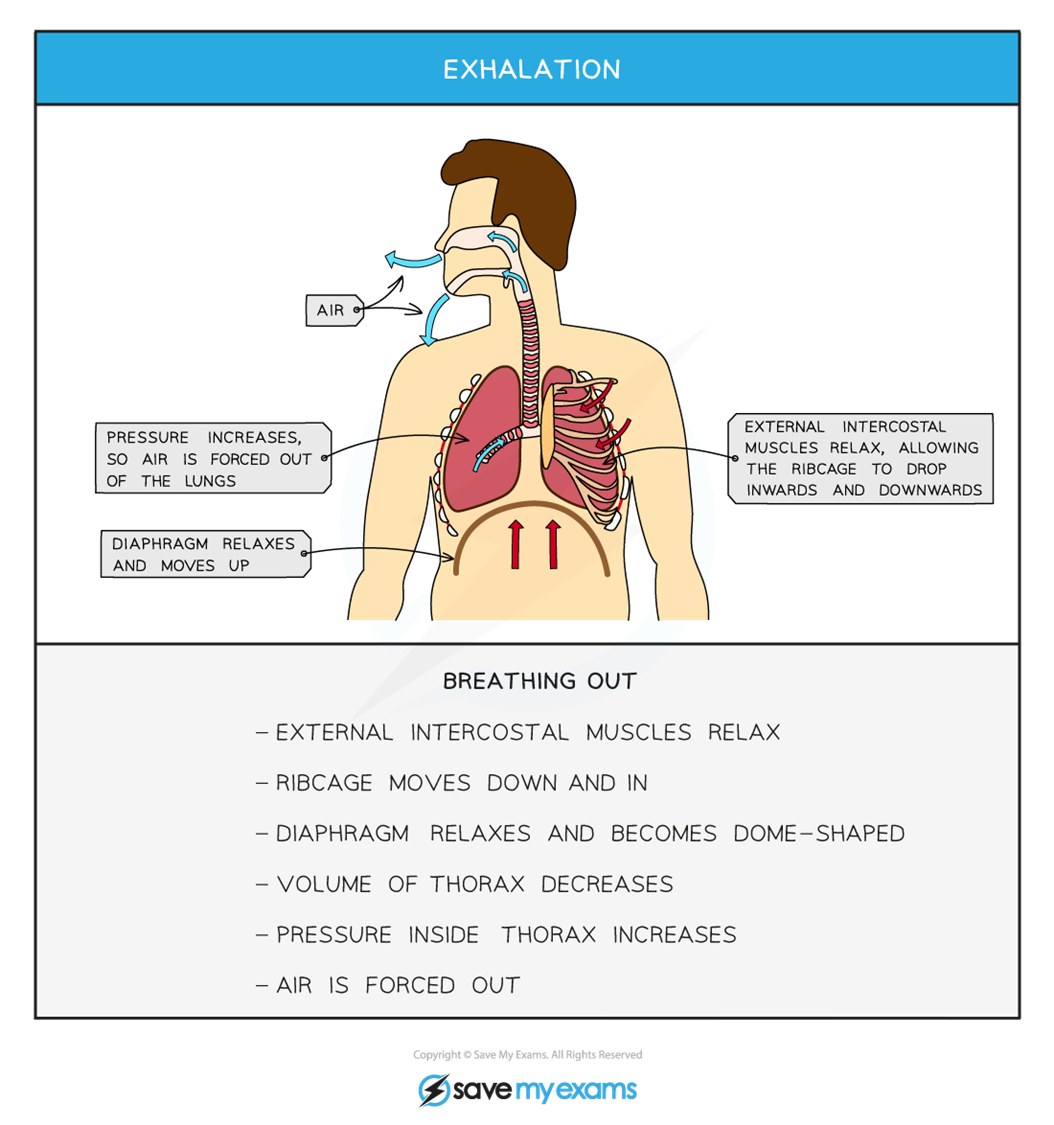
B → Exhalation: Diaphragm relaxes
I. Thorax volume decreases
II. Air pressure rises
III. Air is forced out
Intercostal muscles work as antagonistic pairs
A → External intercostals: contract during inhalation (ribs go up and out)
I. Thorax volume goes up
II. Pressure inside decreases
III. Air goes in
→ they relax during exhalation (ribs go down and in)
I. Thorax Volume decreases
II. Pressure inside increases
III. Air goes out
B → Internal Intercostals: help during forced exhalation (e.g. during exercise) by pulling ribs further down and in
I. Thorax Volume decreases even more
II. Air goes out faster
→ this removes excess CO2 & increases gas exchange
INHALATION:
External intercostal muscles contract
Ribcage moves up & out
Diaphragm contracts & flattens
Volume of thorax increases
Pressure inside thorax decreases
Air is drawn in
EXHALATION:
External Intercostal muscles relax
Ribcage moves down & in
Diaphragm relaxes & becomes dome-shaped
Volume of thorax decreases
Pressure inside the thorax increases
Air is forced out
Forced exhalation:
Internal intercostal muscles contract
Pulls ribcage further downwards & more inwards.
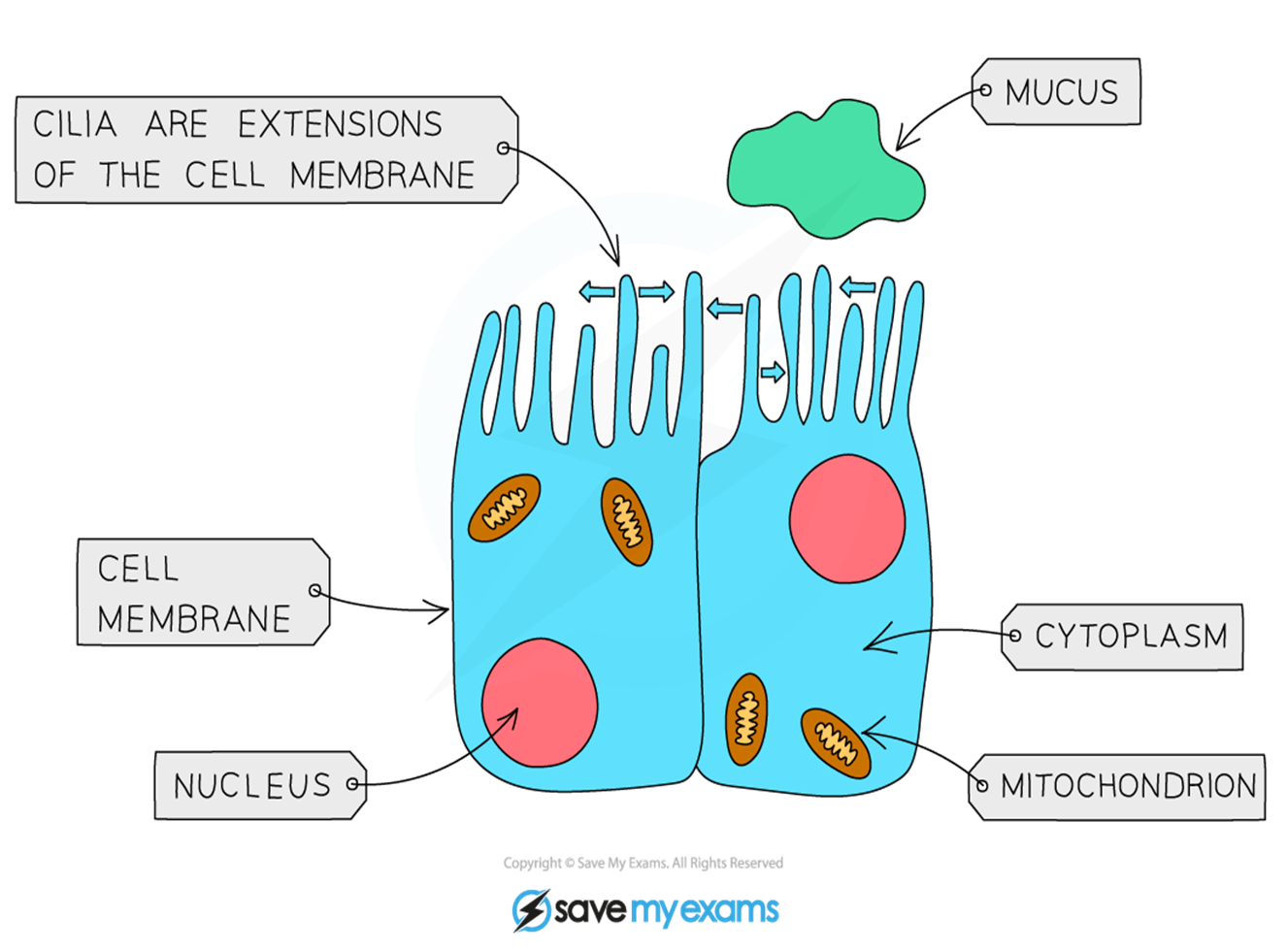
8) Protecting the Breathing System
The airways to lungs are lined with ciliated epithelial cells that have tiny hair-like structures called cilia.
These Cilia beat to push mucus up towards the nose & throat, where it can be removed.
Goblet cells (named after their cup shape) produce the mucus.
The mucus traps dust, pathogens & particles, preventing them from reaching & damaging the lungs.