Chapter 22: The Respiratory System
Organs and Structures of the Respiratory System
- The conducting zone of the respiratory system includes the organs and structures not directly involved in gas exchange.
- The gas exchange occurs in the respiratory zone.
- The external nose consists of the surface and skeletal structures that result in the outward appearance of the nose and contribute to its numerous functions.
- The root is the region of the nose located between the eyebrows.
- The dorsum nasi is the length of the nose.
- An ala is a cartilaginous structure that forms the lateral side of each naris (plural = nares), or nostril opening.
- The philtrum is the concave surface that connects the apex of the nose to the upper lip.
- The nasal bone is one of a pair of bones that lies under the root and bridge of the nose.
- The alar cartilage consists of the apex of the nose; it surrounds the naris.
- The conchae, meatuses, and paranasal sinuses are lined by respiratory epithelium composed of pseudostratified ciliated columnar epithelium.
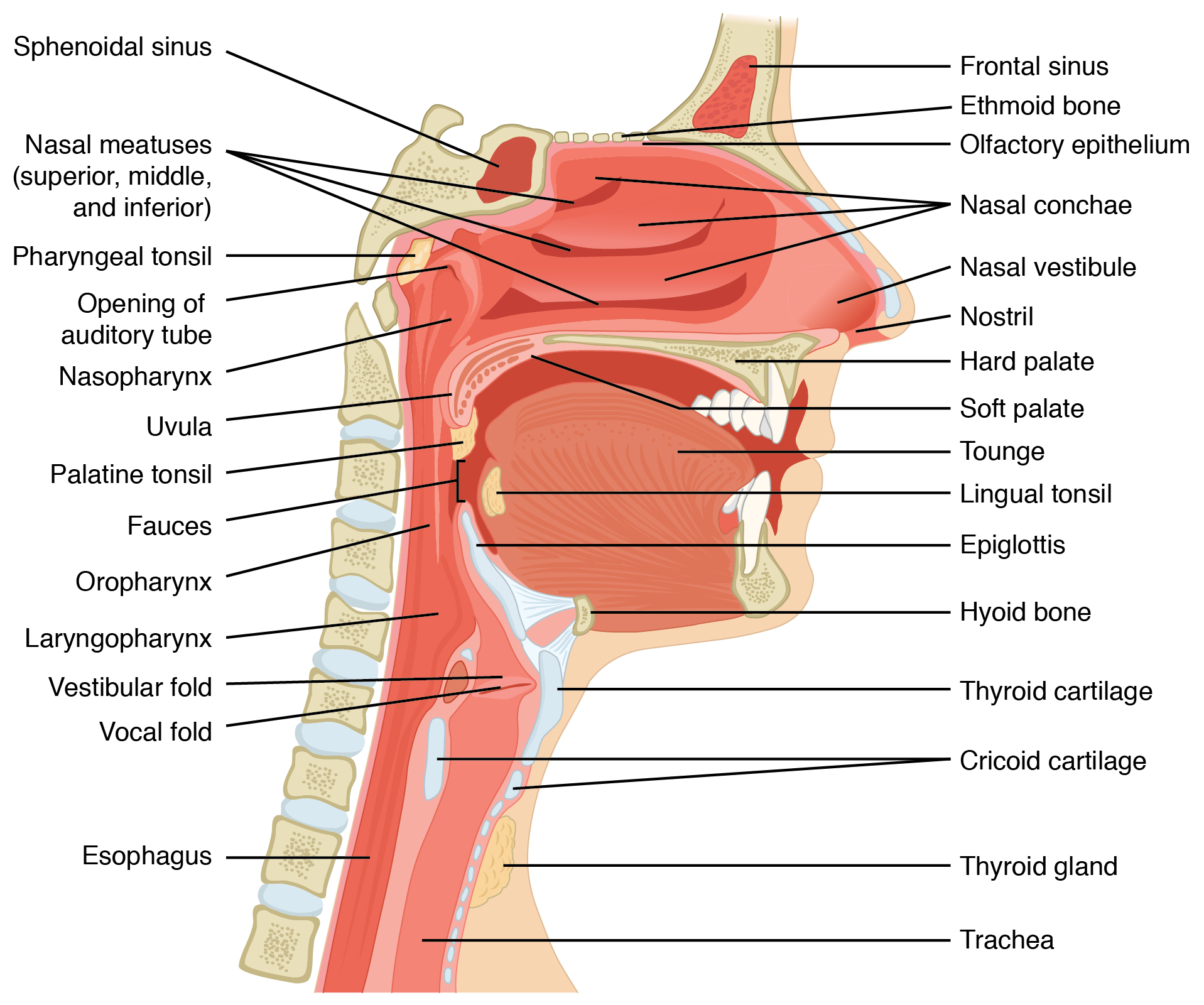
Pharynx
- The pharynx is a tube formed by skeletal muscle and lined by mucous membrane that is continuous with that of the nasal cavities.
- The nasopharynx is flanked by the conchae of the nasal cavity, and it serves only as an airway.
- A pharyngeal tonsil, also called an adenoid, is an aggregate of lymphoid reticular tissue similar to a lymph node that lies at the superior portion of the nasopharynx.
- The oropharynx is a passageway for both air and food.
- The laryngopharynx is inferior to the oropharynx and posterior to the larynx.
Larynx
- The larynx is a cartilaginous structure inferior to the laryngopharynx that connects the pharynx to the trachea and helps regulate the volume of air that enters and leaves the lungs.
- The thyroid cartilage is the largest piece of cartilage that makes up the larynx.
- The thyroid cartilage consists of the laryngeal prominence, or “Adam’s apple,” which tends to be more prominent in males.
- The thick cricoid cartilage forms a ring, with a wide posterior region and a thinner anterior region.
- The epiglottis, attached to the thyroid cartilage, is a very flexible piece of elastic cartilage that covers the opening of the trachea.
- The glottis is composed of the vestibular folds, the true vocal cords, and the space between these folds.
- A vestibular fold, or false vocal cord, is one of a pair of folded sections of mucous membrane.
- A true vocal cord is one of the white, membranous folds attached by muscle to the thyroid and arytenoid cartilages of the larynx on their outer edges.
Trachea
- The trachea is formed by 16 to 20 stacked, C-shaped pieces of hyaline cartilage that are connected by dense connective tissue.
- The trachealis muscle and elastic connective tissue together form the fibroelastic membrane, a flexible membrane that closes the posterior surface of the trachea, connecting the C-shaped cartilages.
Bronchial Tree
- The trachea branches into the right and left primary bronchi at the carina.
- A bronchial tree (or respiratory tree) is the collective term used for these multiple-branched bronchi.
- A bronchiole branches from the tertiary bronchi.
Respiratory Zone
- The respiratory zone begins where the terminal bronchioles join a respiratory bronchiole, the smallest type of bronchiole.
Alveoli
- An alveolar duct is a tube composed of smooth muscle and connective tissue, which opens into a cluster of alveoli.
- An alveolus is one of the many small, grape-like sacs that are attached to the alveolar ducts.
- An alveolar sac is a cluster of many individual alveoli that are responsible for gas exchange.
- A type I alveolar cell is a squamous epithelial cell of the alveoli, which constitute up to 97 percent of the alveolar surface area.
- A type II alveolar cell is interspersed among the type I cells and secretes pulmonary surfactant, a substance composed of phospholipids and proteins that reduces the surface tension of the alveoli.
The Lungs
- A major organ of the respiratory system, each lung houses structures of both the conducting and respiratory zones.
- The cardiac notch is an indentation on the surface of the left lung, and it allows space for the heart
- The pulmonary artery is an artery that arises from the pulmonary trunk and carries deoxygenated, arterial blood to the alveoli.
- Once the blood is oxygenated, it drains from the alveoli by way of multiple pulmonary veins, which exit the lungs through the hilum.
- The parasympathetic system causes bronchoconstriction, whereas the sympathetic nervous system stimulates bronchodilation.
- The pulmonary plexus is a region on the lung root formed by the entrance of the nerves at the hilum.
Pleura of the Lungs
- The pleura (plural = pleurae) is a serous membrane that surrounds the lung.
- The visceral pleura is the layer that is superficial to the lungs, and extends into and lines the lung fissures.
- The parietal pleura is the outer layer that connects to the thoracic wall, the mediastinum, and the diaphragm.
- The pleural cavity is the space between the visceral and parietal.
- Pleural fluid is secreted by mesothelial cells from both pleural layers and acts to lubricate their surfaces.
The Process of Breathing
- Pulmonary ventilation is the act of breathing, which can be described as the movement of air into and out of the lungs.
- Atmospheric pressure is the amount of force that is exerted by gases in the air surrounding any given surface, such as the body.
- Intra-alveolar pressure is the pressure of the air within the alveoli, which changes during the different phases of breathing.
- Intrapleural pressure is the pressure of the air within the pleural cavity, between the visceral and parietal pleurae.
- Transpulmonary pressure is the difference between the intrapleural and intra-alveolar pressures, and it determines the size of the lungs.
- Thoracic wall compliance is the ability of the thoracic wall to stretch while under pressure.
Pulmonary Ventilation
- Inspiration is the process that causes air to enter the lungs, and expiration is the process that causes air to leave the lungs
- A respiratory cycle is one sequence of inspiration and expiration.
Respiratory Volumes and Capacities
- Respiratory volume is the term used for various volumes of air moved by or associated with the lungs at a given point in the respiratory cycle.
- Tidal volume (TV) is the amount of air that normally enters the lungs during quiet breathing, which is about 500 milliliters.
- Expiratory reserve volume (ERV) is the amount of air you can forcefully exhale past a normal tidal expiration, up to 1200 milliliters for men.
- Inspiratory reserve volume (IRV) is produced by a deep inhalation, past a tidal inspiration.
- Residual volume (RV) is the air left in the lungs if you exhale as much air as possible.
- Vital capacity (VC) is the amount of air a person can move into or out of his or her lungs, and is the sum of all of the volumes except residual volume (TV, ERV, and IRV), which is between 4000 and 5000 milliliters.
- Inspiratory capacity (IC) is the maximum amount of air that can be inhaled past a normal tidal expiration, is the sum of the tidal volume and inspiratory reserve volume.
Respiratory Rate and Control of Ventilation
- The respiratory rate is the total number of breaths, or respiratory cycles, that occur each minute.
- The medulla oblongata contains the dorsal respiratory group (DRG) and the ventral respiratory group (VRG).
- The apneustic center is a double cluster of neuronal cell bodies that stimulate neurons in the DRG, controlling the depth of inspiration, particularly for deep breathing.
- The pneumotaxic center is a network of neurons that inhibits the activity of neurons in the DRG, allowing relaxation after inspiration, and thus controlling the overall rate.
Factors That Affect the Rate and Depth of Respiration
- A central chemoreceptor is one of the specialized receptors that are located in the brain and brainstem, whereas a peripheral chemoreceptor is one of the specialized receptors located in the carotid arteries and aortic arch.
Gas Laws and Air Composition
- Partial pressure (Px) is the pressure of a single type of gas in a mixture of gases.
- Total pressure is the sum of all the partial pressures of a gaseous mixture.
- Dalton’s law describes the behavior of nonreactive gases in a gaseous mixture and states that a specific gas type in a mixture exerts its own pressure; thus, the total pressure exerted by a mixture of gases is the sum of the partial pressures of the gases in the mixture.
- Henry’s law describes the behavior of gases when they come into contact with a liquid, such as blood.
- Ventilation is the movement of air into and out of the lungs, and perfusion is the flow of blood in the pulmonary capillaries.
- External respiration occurs as a function of partial pressure differences in oxygen and carbon dioxide between the alveoli and the blood in the pulmonary capillaries.
- Internal respiration is gas exchange that occurs at the level of body tissues.
Transport of Gases
- The following reversible chemical reaction describes the production of the final product, oxyhemoglobin (Hb–O2), which is formed when oxygen binds to hemoglobin.
- An oxygen–hemoglobin dissociation curve is a graph that describes the relationship of partial pressure to the binding of oxygen to heme and its subsequent dissociation from heme.
- The Bohr effect is a phenomenon that arises from the relationship between pH and oxygen’s affinity for hemoglobin: A lower, more acidic pH promotes oxygen dissociation from hemoglobin. In contrast, a higher, or more basic, pH inhibits oxygen dissociation from hemoglobin.
Carbaminohemoglobin
- Carbon dioxide does not bind to iron as oxygen does; instead, carbon dioxide binds amino acid moieties on the globin portions of hemoglobin to form carbaminohemoglobin, which forms when hemoglobin and carbon dioxide bind.
- The Haldane effect is a phenomenon that arises from the relationship between the partial pressure of oxygen and the affinity of hemoglobin for carbon dioxide.
- Hemoglobin that is saturated with oxygen does not readily bind carbon dioxide.
Modifications in Respiratory Functions
- Hyperpnea is an increased depth and rate of ventilation to meet an increase in oxygen demand as might be seen in exercise or disease, particularly diseases that target the respiratory or digestive tracts.
- Hyperventilation is an increased ventilation rate that is independent of the cellular oxygen needs and leads to abnormally low blood carbon dioxide levels and high (alkaline) blood pH.
- Acute mountain sickness (AMS), or altitude sickness, is a condition that results from acute exposure to high altitudes due to a low partial pressure of oxygen at high altitudes.
- Acclimatization is the process of adjustment that the respiratory system makes due to chronic exposure to a high altitude.
Embryonic Development of the Respiratory System
- An olfactory pit is one of a pair of structures that will enlarge to become the nasal cavity. At about this same time, the lung bud forms.
- The lung bud is a dome-shaped structure composed of tissue that bulges from the foregut.
- The foregut is endoderm just inferior to the pharyngeal pouches.
- The laryngotracheal bud is a structure that forms from the longitudinal extension of the lung bud as development progresses.
- A bronchial bud is one of a pair of structures that will eventually become the bronchi and all other lower respiratory structures.