Physiology: Respiratory System, Blood, Blood Pressure 🩺👨⚕️🩸
stay cute stay lit stay pumping 🥺🥺
Respiratory Anatomy
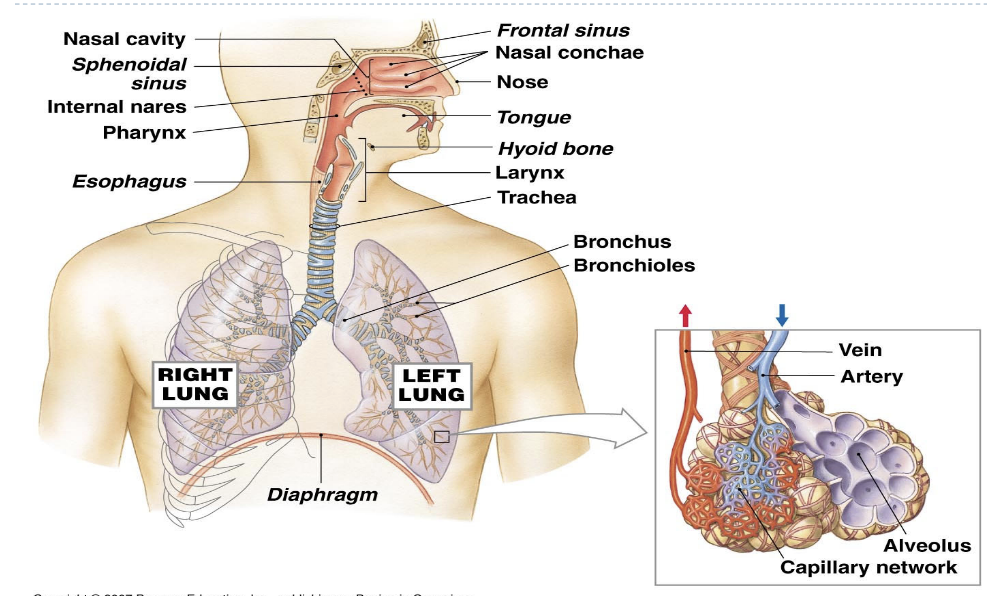
Nasal Cavity
Passageway from external environment to pharynx
Complex network of tunnels, hairs, bones, mucus, and cartilage that benefited breathing:
Function(s):
Nose Hairs - Filters air clean of larger particles
Warms air
Mucus - Traps bacteria from entering lungs
Pharynx (throat) - PHOOD
Chamber shared with digestive system (liquid & food)
Larynx:- LARRY AIR
Separated chamber where only air is designed to travel through
Epiglottis → flap that covers opening to larynx, prevents bolus from going down the respiratory tract
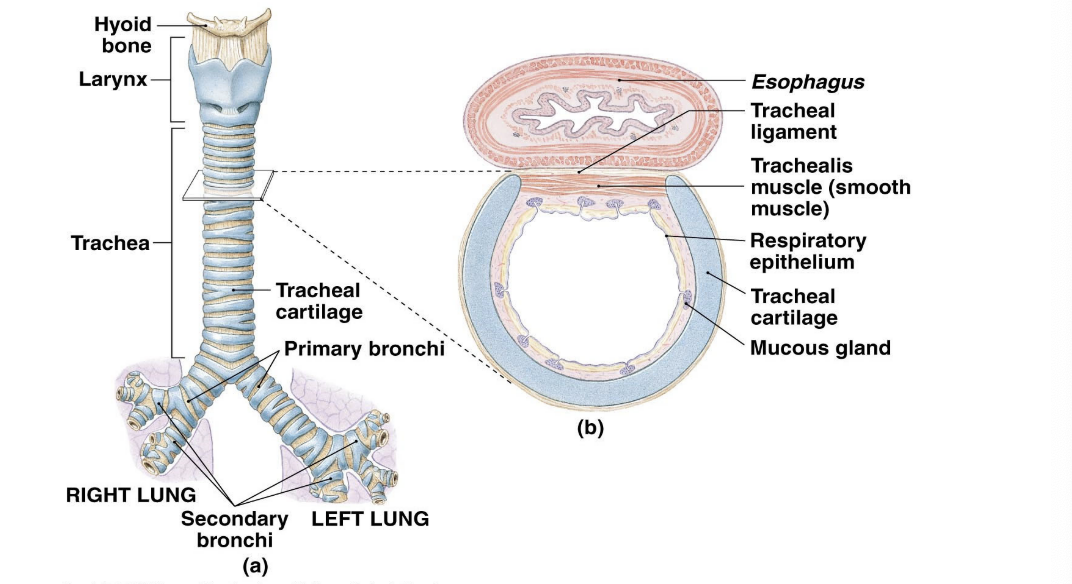
Trachea (windpipe)
Tough flexible tube
C-ring cartilage to prevent overexpansion of the tracheal walls

Bronchi - thiccccccc(C) (bronchus)
Gets smaller as it branches out
Right bronchi larger than left
Divisions:
Primary bronchi (2 total, one right one left)
Secondary: second division entering lung lobes
Tertiary: third division
Bronchiole
Small tubes from division of the bronchi
Serves as regulator of airflow (constricting to result in less, widening resulting in more)
Alveoli
Small sacs at inner surface of lungs
Gas exchange occurs
150 million alveoli per lung
Turbinates
Superior Turbinate
Filters and humidifiers air & sense of smell
Middle Turbinate
Regulates airflow & drains mucus from sinuses
Inferior Turbinate
Regulates airflow
Inflamed Inferior Turbinate
When inflamed, it blocks airflow
Stuffy nose
Facial pressure
Sinus infections
Headaches
Why should one breathe through their nose & not their mouth?
The nose acts as a natural filter
It warms up the air you breathe before it goes in your system
More efficient uptake of oxygen
Respiratory Physiology
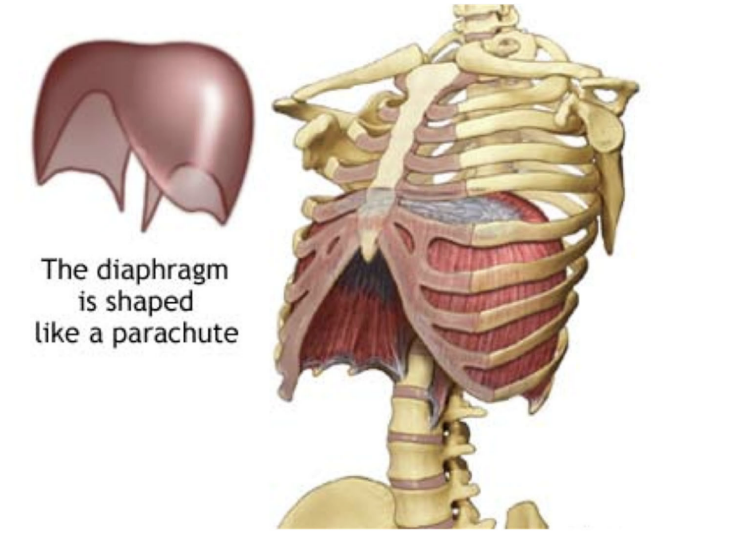
Diaphragm
Muscle at the bottom of the rib cage
Regulates the volume of thoracic cavity (lungs & rib cage area)
LARGER the cavity, the LARGER the lungs
SMALLER the cavity, the SMALLER the lungs
Air moves from high to low
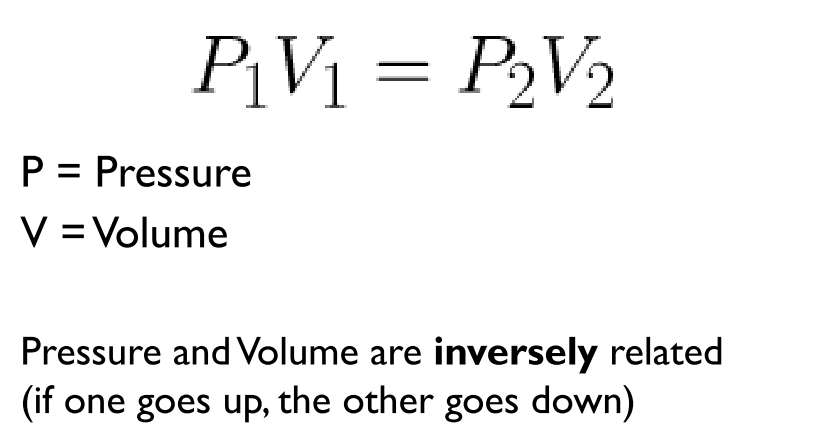
Boyle’s Law
Steps to Air Flow
Volume of the lungs changes →
Pressure in the lungs changes →
Causes pressure inside vs outside to change →
Air moves

Lung Capacity
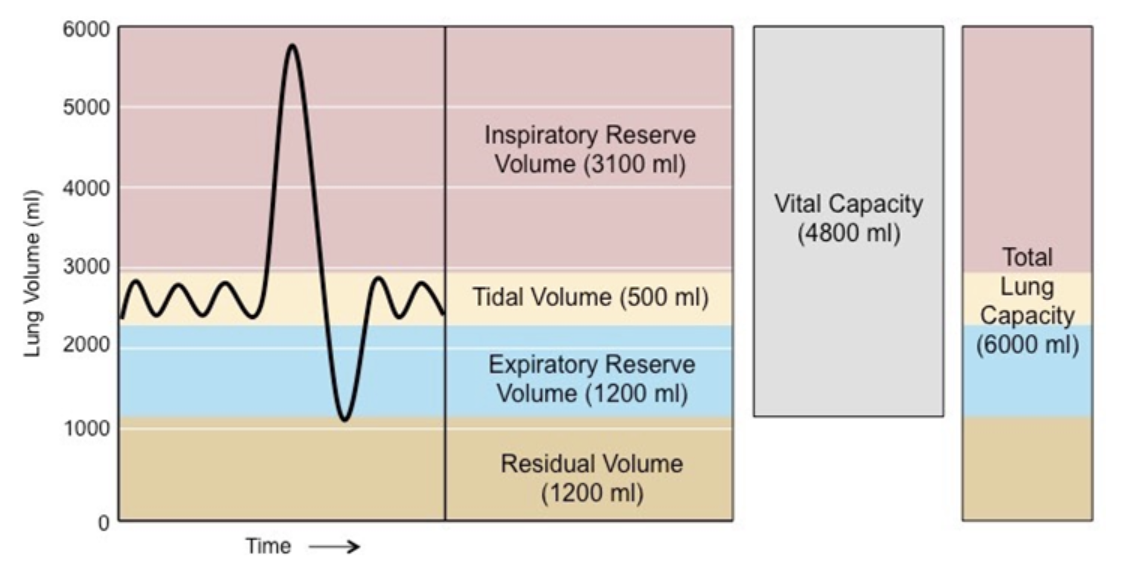
Total Lung Volumes
Males: 6000 ml
Females: 4200 ml
Total Lung Capacity
Maximum volume of air the lungs can hold after a maximal inhalation.
Calculation:
TLC = IRV + TV + ERV + RV
Examples
Balloon that can be fully inflated. The maximum amount of air you can blow into the balloon before it bursts represents the total lung capacity.
Tidal Wave Volume
Standard breath cycle, the volume of air inhaled or exhaled during a normal, quiet breath.
Example
Think of the tides, going in and out comfortably
Inspiratory Reserve Volume (IRV → Mona w/ her IV → from normal to extra inhale)
The extra volume of air that can be inspired with maximal effort
Example
After a normal breath, if you take a deep, forceful breath, the extra air you inhale beyond the normal breath is your inspiratory reserve volume.
Expiratory Reserve Volume (ERV → the ER after choking → from normal to extra exhale)
Max amount of air that can be forcefully exhaled
Example
After a normal breath, if you forcefully blow out as much air as you can, the extra air you exhale beyond the normal breath is your expiratory reserve volume.
Vital Capacity (VC → PVC Pipe → blow in deep and out deep)
The maximum volume of air that can be exhaled after a maximum inhalation.
Calculation:
VC = IRV + TV + ERV
Example
Imagine taking a deep breath and then forcefully blowing out as much air as you can. The total amount of air you exhale is your vital capacity.
Residual Volume (RV → an RV car being looted → remaining thing in the RV → remaing breath after exhalation)
The volume of air that remains in the lungs after a maximum forceful exhalation.
Example
Even after a forceful exhale, some air remains in your lungs. This remaining air is the residual volume.
Minimal Volume (MOST MINI VOLUME)
Component of the residual volume
Smallest possible volume of air remaining in the lungs before collapse
Blood
4 components of blood
Plasma (55%)
Yellowish STICKYYYYY fluid
Made of mostly water and proteins
Carries HEAT energy
Carries dissolved materials like glucose, AA’s, vitamins, minerals, salts
Provides immune defense
Red Blood Cells (45%)
Transporter cells
Concave shaped
NO nucleus or mitochondria
Life span of 4 months, recycled by LIVER & SPLEEN
5 million RBCS
Rich in hemoglobin
Protein that allows binding of Oxygen
Iron helps oxygen binding
ANEMIA is lack of properly functioning RBCs, typically due to hemoglobin deficiency
White Blood Cells (<1%)
Phagocytes or Lymphocytes
Possess a nucleus
Feed pathogens via Phagocytosis
Produce antibodies/use cell mediation
Platelets (<1%)
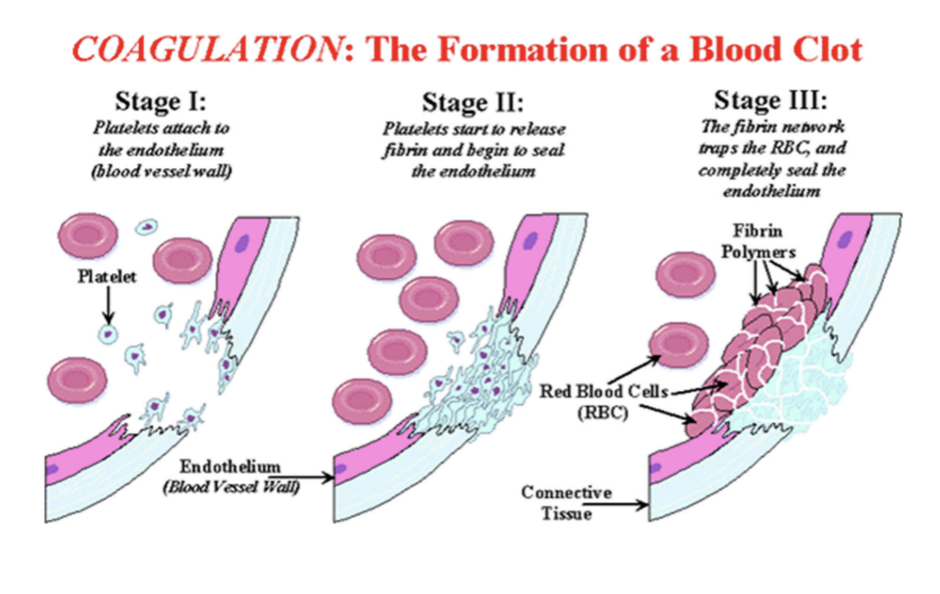
Tiny fragments of bone marrow cells
Hemostasis (clotting): use of prothrombin, thrombin, and fibrin to form fibers → connect using a positive feedback loop (reinforce)
Prevents bleeding, but can cause undesired blood clots preventing blood flow
Blood Vessels
Blood Vessels
Arteries
Carries blood AWAY from heart to organs
Veins
Carries blood FROM the organs BACK to the heart
Capillaries
Tiny vessels that connect arteries and veins
Thin walls that allow blood to exchange oxygen
Arterioles
Small blood vessels that branch off from arteries
Carry blood from arteries to capillaries
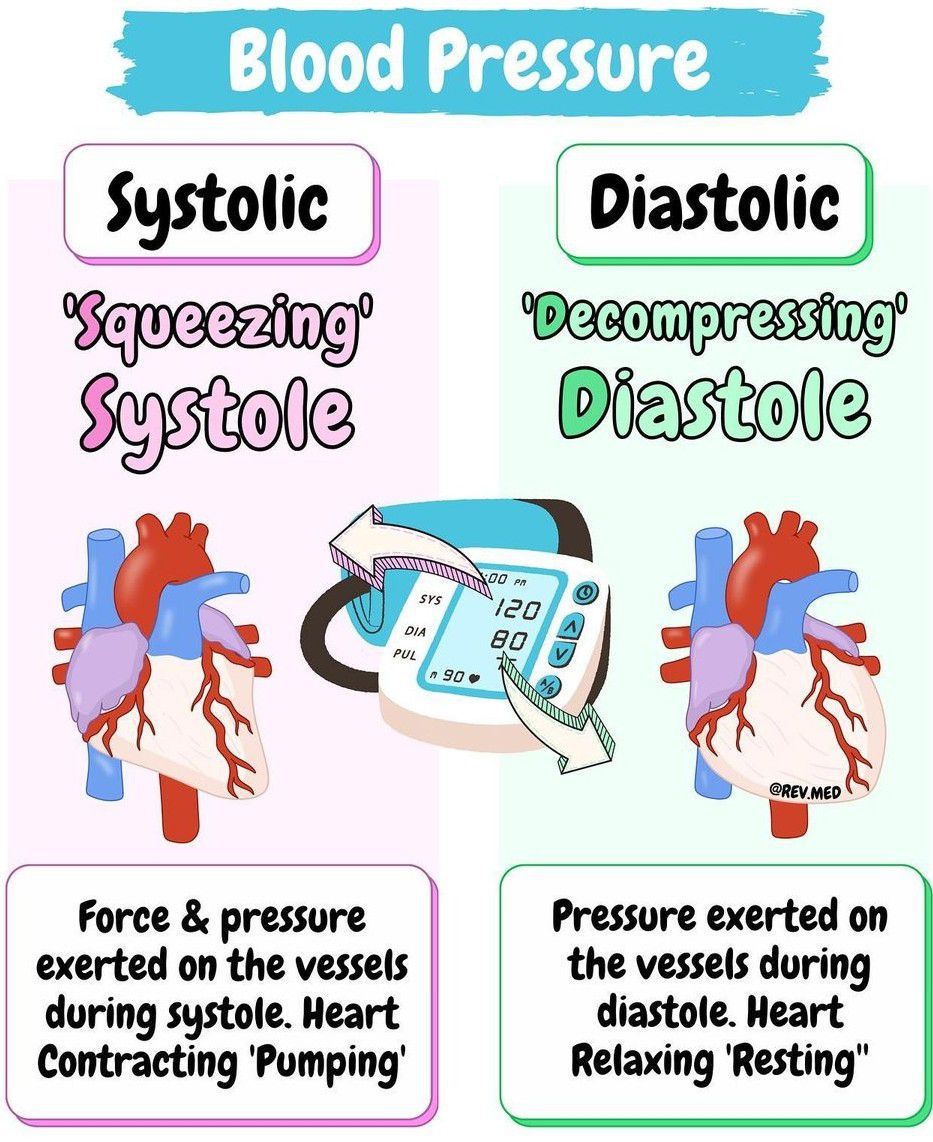
Systolic & Diastolic
Systolic
The top #
Measures the pressure in the arteries when the heart beats
Diastolic
The bottom #
Measures the pressure in the arteries between heartbeats.
Risk Factors/Activities
Alcohol Consumption
Caffeine
Lack of exercise
Obesity
Stress
Lack of sleep
Smoking
Non-controllable ones
Race
Family History
Gender
Age
Difference between essential & secondary hypertension
Essential hypertension
Often has no identifiable cause, but may be linked to genetics, aging, stress, salt, obesity, or lack of exercise
Secondary hypertension
Caused by an identifiable condition that affects the heart, kidneys, arteries, or endocrine system. It can also occur during pregnancy.
Heart attacks
Blockage in one or more of the coronary arteries
Blockage typically stems from the buildup of plaque (Atherosclerosis)
Plaque rupture (thrombosis)
Heart Failures
Stiff & inflexible making it difficult for the ventricles to relax
Hypertrophy: heart muscle may thicken as it works harder to compensate for reduced pumping capacity
High Blood Pressure
the constant high pressure forces the heart to work harder and damages the blood vessels, making them stiffer, narrower, and more prone to disease.
Systolic & Diastolic
Systolic & Diastolic
Systolic
The top #
Measures the pressure in the arteries when the heart beats
Diastolic
The bottom #
Measures the pressure in the arteries between heartbeats.
Risk Factors/Hypertension/Heart Attacks
Risk Factors/Activities
Alcohol Consumption
Caffeine
Lack of exercise
Obesity
Stress
Lack of sleep
Smoking
Non-controllable ones
Race
Family History
Gender
Age
Difference between essential & secondary hypertension
Essential hypertension
Often has no identifiable cause, but may be linked to genetics, aging, stress, salt, obesity, or lack of exercise
Secondary hypertension
Caused by an identifiable condition that affects the heart, kidneys, arteries, or endocrine system. It can also occur during pregnancy.
Heart attacks
Blockage in one or more of the coronary arteries
Blockage typically stems from the buildup of plaque (Atherosclerosis)
Plaque rupture (thrombosis)
Heart Failures
Stiff & inflexible making it difficult for the ventricles to relax
Hypertrophy: heart muscle may thicken as it works harder to compensate for reduced pumping capacity
High Blood Pressure
the constant high pressure forces the heart to work harder and damages the blood vessels, making them stiffer, narrower, and more prone to disease.