
Lecture 6: Alteration of Endocrine System
hormone definition: mainly peptides, shorter or longer, secreted in the bloodstream, travel long distances where they are received by other cells
endocrine system is a system of glands
elevated or depressed hormone levels: (what can cause it)
failure or respond (response?) to inappropriate signal of feedback systems
dysfunction of an endocrine gland
secretory cells are unable to produce, obtain, or convert hormone precursors
the endocrine gland synthesizes or releases excessive amounts of hormone
increased hormone degradation or inactivation
ectopic hormone release
target cell failure:
receptor associated disorders
decrease in number of receptors
impaired receptor function
presence of antibodies against specific receptors
antibodies that mimic hormone action
unusual expression of receptor function
how hormones work at the target cell (my notes, he said to know it)
the hormone binds to a receptor (either on plasma membrane or in cell depending on water/lipid solubility)
once the hormone binds to the receptor a signal cascade is triggered
for surface receptors, this often involves activating a g protein which is linked to the receptor and when inactive bound to gdp
once activated, the g protein released gdp and binds to gtp
the now activated g protein (attached to gtp) interacts with adenylate cyclase
adenylate cyclase converts atp into cyclic amp (cAMP) which is a second messenger
cAMP then goes and triggers a set of events that actually causes the cells response to the hormone
any issue in this process can cause disease
ex. receptor dysfunction, second messenger dysfunction, signaling pathway dysfunction
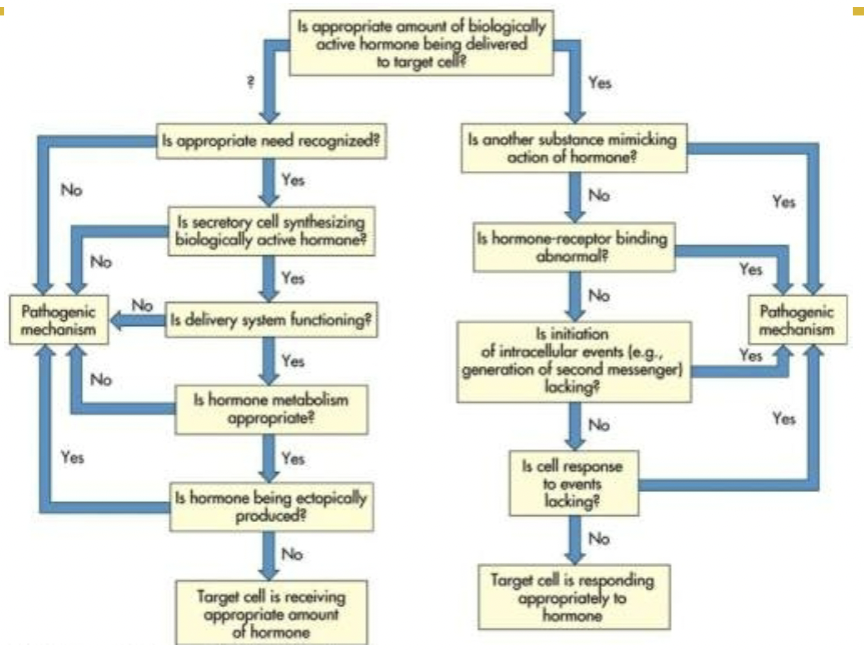
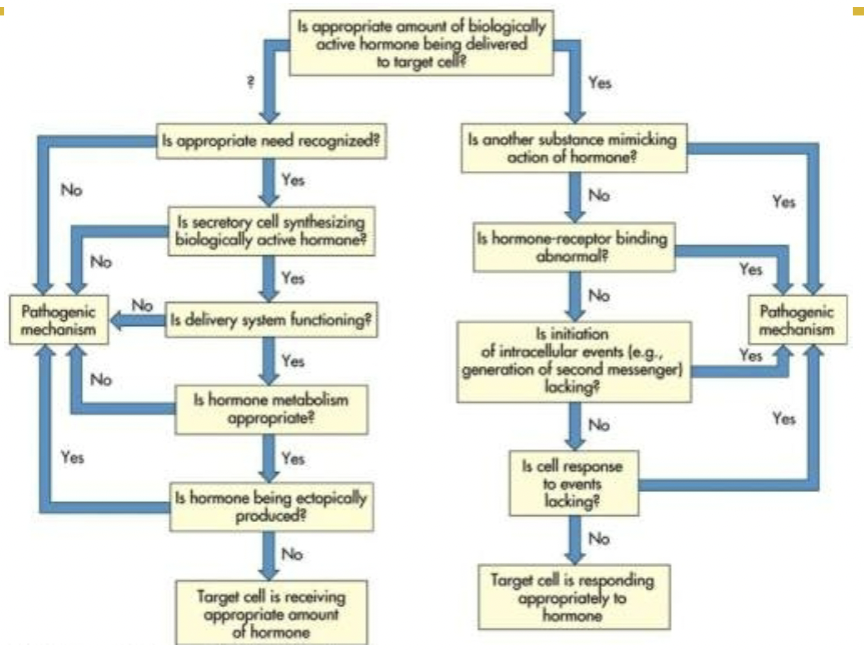
hormone delivery: (flow chart)
is appropriate amount of biologically active hormone being delivered to target cell?
yes → is another substance mimicking action of hormone?
yes → pathogenic mechanism
no → is hormone receptor binding abnormal?
yes → pathogenic mechanism
no → is initiation of intracellular events (ex. generation of second messenger) lacking?
yes → pathogenic mechanism
no → is cell response to events lacking?
yes → pathogenic mechanism
no → target cell is responding appropriately to hormone
? (unknown?) → is appropriate need recognized?
no → pathogenic mechanism
yes → is secretory cell synthesizing biologically active hormone?
no → pathogenic mechanism
yes → is delivery system functioning?
no → pathogenic mechanism
yes → is hormone metabolism appropriate? (is it being removed properly after release)
no → pathogenic mechanism
yes → is hormone being ectopically produced? (is it being produced somewhere where it shouldnt be)
no → target cell is receiving appropriate amount of hormone
yes → pathogenic mechanism
alterations of the hypothalamic-pituitary system:
(decreased hypothalamic function causes ___ which leads to anterior pituitary hormone effect __)
GnRH ↓ —> FSH ↓ && LH ↓
TRH ↓ —> TSH ↓
CRH ↓ —> ACTH ↓
PIF ↓ —> prolactin ↑
GHRH ↓ —> GH ↓
diseases of the posterior pituitary
syndrome of inappropriate antidiuretic hormone secretion (SIADH)
hypersecretion of adh without the presence of physiological stimuli
for diagnosis, normal adrenal and thyroid function must exist
clinical manifestations are related to enhanced renal water retention, hyponatremia, and hypoosmolarity
diabetes insipidus
insufficiency of adh
polyuria and polydipsia (frequent drinking/excessive thirst)
partial or total inability to concentrate urine
neurogenic
insufficient amounts of adh
nephrogenic
inadequate response to adh
diseases of the anterior pituitary
disorders of anterior pituitary may involve hypo or hyper function of the gland
hypopituitarism (deficiency or failure hormonal function)
one of the cause is pituitary infarction (death of tissue). pituitary infarction can be seen in
sheehan syndrome (ischemic pituitary necrosis)- pituitary gland is highly vascular so it is vulnerable to ischemia and infarction
hemorrhage
shock
others: head trauma, infections, and tumors
clinical manifestation depend on the affected area and affected hormones
hypopituitarism
panhypopituitarism- when all hormones are absent
acth deficiency leads to cortisol deficiency
tsh deficiency leads to thyroid hormone deficiency
fsh and lh deficiency leads to failure or loss of secondary sexual characteristics
gh deficiency leads to deficiency in growth
diagnosis: radioimmunoassay (measure hormone level), mri or ct (to measure size/look for abnormal areas)
treatment: hormone therapy
hyperpituitarism
commonly due to a benign, slow growing, pituitary adenoma
expansion of pituitary adenoma may cause both neurogenic (due to infiltration of cranial nerves) and secretory defect
manifestations
headache and fatigue
visual changes (if the tumor infiltrates the optic chiasm)
hyposecretion of neighboring anterior pituitary hormones
hypersecretion of growth hormone (gh)
acromegaly
hypersecretion of gh in adulthood (after growth plates close)
gigantism
hypersecretion of gh in children and adolescents (before growth plates close)
manifestation
interstitial edema
increased in size and function of sebaceous and sweat gland (causes increased body odor)
coarse (thick) skin
enlargement of facial bones
arthritis and backaches due to cartilaginous growth
hypersecretion of prolactin
caused by prolactinomas
in females, increased levels of prolactin cause amenorrhea (menstrual disturbances), galactorrhea (nonpuerperal milk production [milk production not caused by childbirth/breastfeeding]), hirsutism (excess hair growth), and osteopenia (reduced bone mass but not enough for osteoporosis)
in males, increased levels of prolactin cause hypogonadism (gonads dont produce enough sex hormones), erectile dysfunction, impaired libido, oligospermia (low sperm count), and diminished or decreased ejaculate volume
alterations of thyroid function
hyperthyroidism
thyrotoxicosis- primarily caused by excess thyroid hormones secreted by thyroid gland, but also could be caused by tsh secreting pituitary adenoma
manifestation: increased metabolic rate, cardiac output
graves disease- autoimmune disease
hyperthyroidism resulting from nodular thyroid disease
goiter
hypothyroidism can be primary or secondary
caused by
defective hormone synthesis due to autoimmune thyroiditis, iodine deficiency, or antithyroid drugs
loss of thyroid tissue
primary hypothyroidism
subacute thyroiditis- inflammation of thyroid by a viral infection
autoimmune thyroiditis- results granular destruction of thyroid tissue
postpartum thyroiditis
manifestation: decrease energy metabolism, low basal metabolic rate, cold intolerance, tiredness
diagnosis and treatment: clinical symptoms, decrease t4 (a hormone), hormone therapy
thyroid carcinoma
alterations of parathyroid function
hyperparathyroidism
primary hyperparathyroidism
excess secretion of pth from one or more parathyroid glands
secondary hyperparathyroidism
increase in pth secondary to a chronic disease
manifestations: excessive osteoclastic activity, pathologic fractures, curvature of spine
hypoparathyroidism
abnormally low pth levels
usually caused by parathyroid damage in thyroid surgery
manifestation: muscle spasm, hyporreflexia, laryngeal spasm
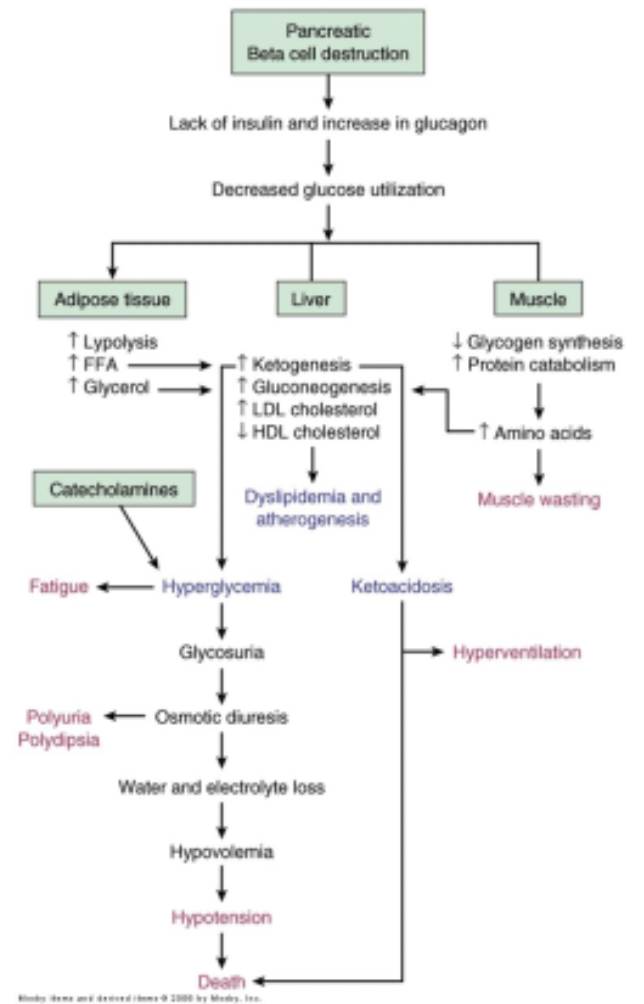
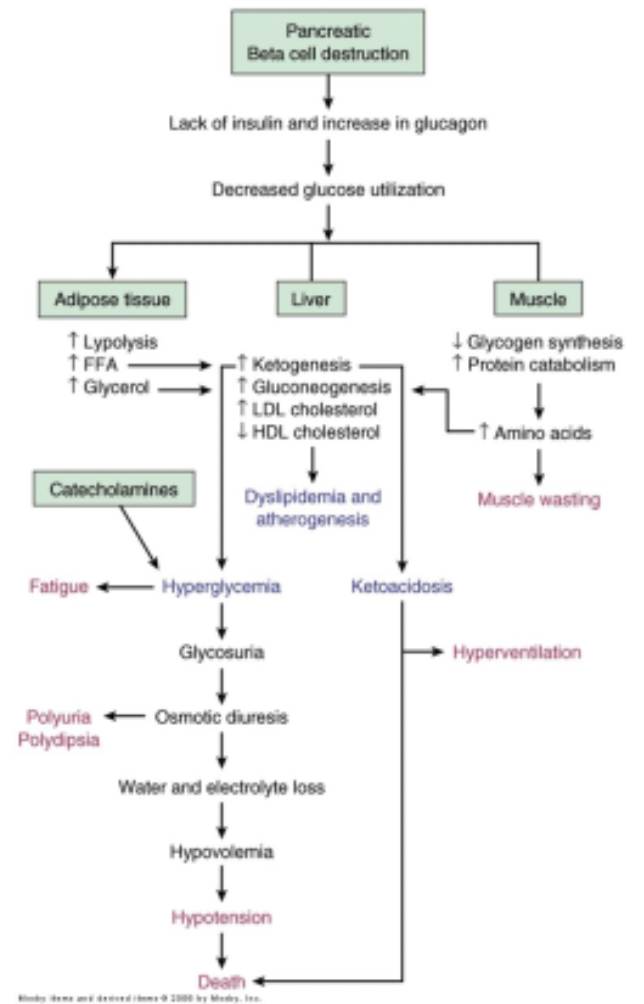
type 1 diabetes mellitus
demonstrates pancreatic atrophy and specific loss of beta cells
macrophages, t and b lymphocytes, and natural killer cells are present
two types
immune- environmental genetic factors result cell mediated destruction of beta cells
nonimmune- occurs secondary to other diseases
manifestations
type 1 diabetes affects metabolism of fat, protein, and carbohydrates
hyperglycemia, polydipsia, polyuris, polyphagia, weightloss, and fatigue
diagnosis- clinical symptoms

dysfunction of the pancreas
type 2 diabetes mellitus
maturity onset diabetes of youth (mody)
gestational diabetes mellitus (gdm)
common form of diabetes mellitus type 2
insulin resistance
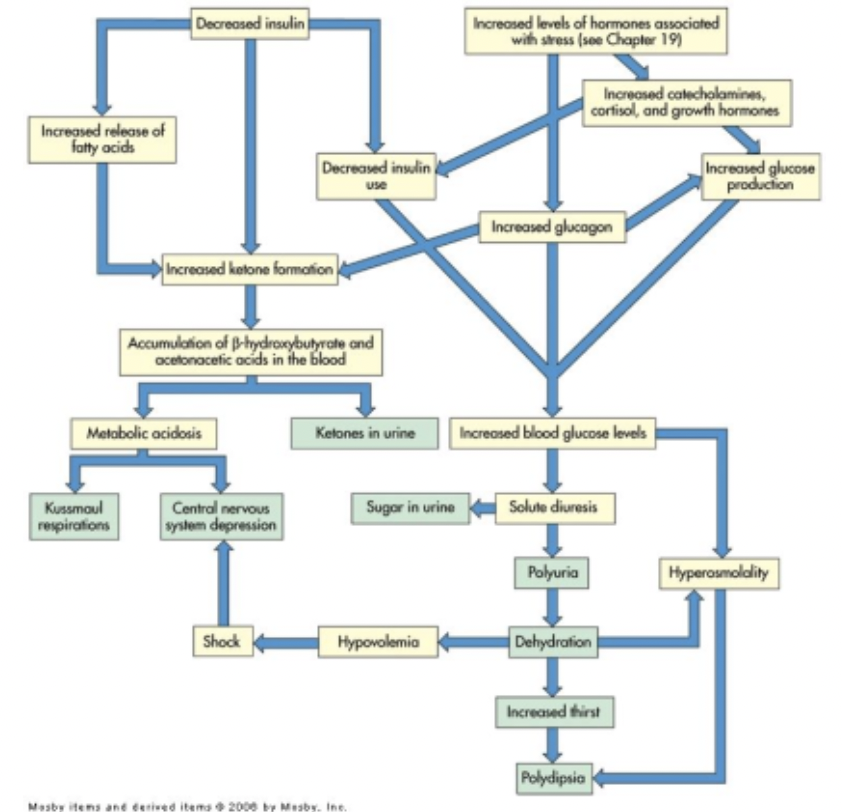
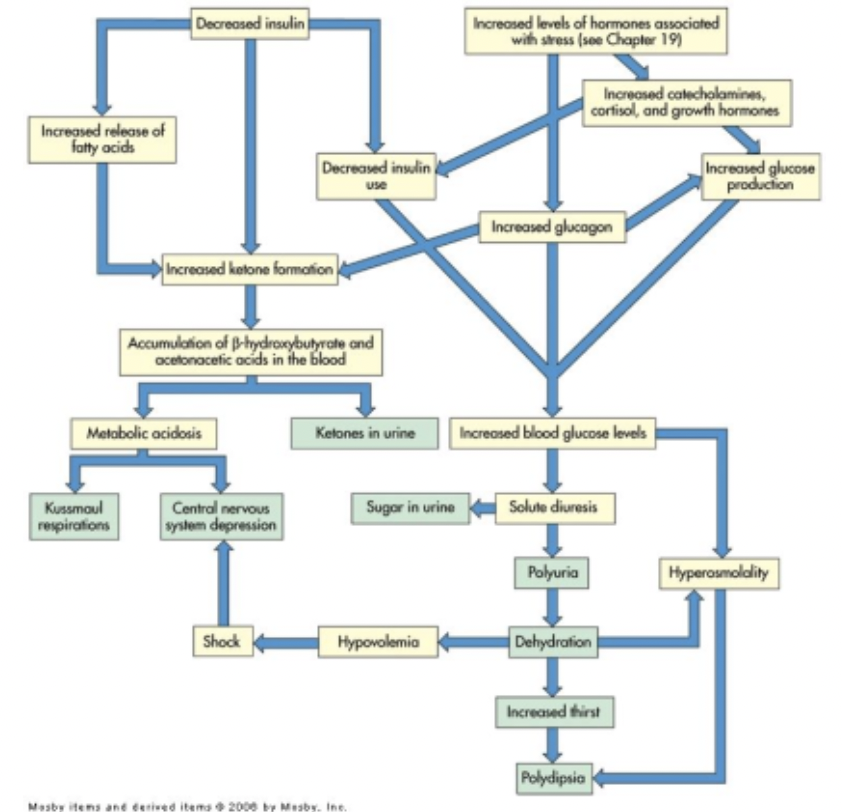
acute complications of diabetes mellitus
hypoglycemia
diabetic ketoacidosis
hyperosmolar hyperglycemic nonketotic syndrome (hhnks)
somogyi effect
dawn phenomenon
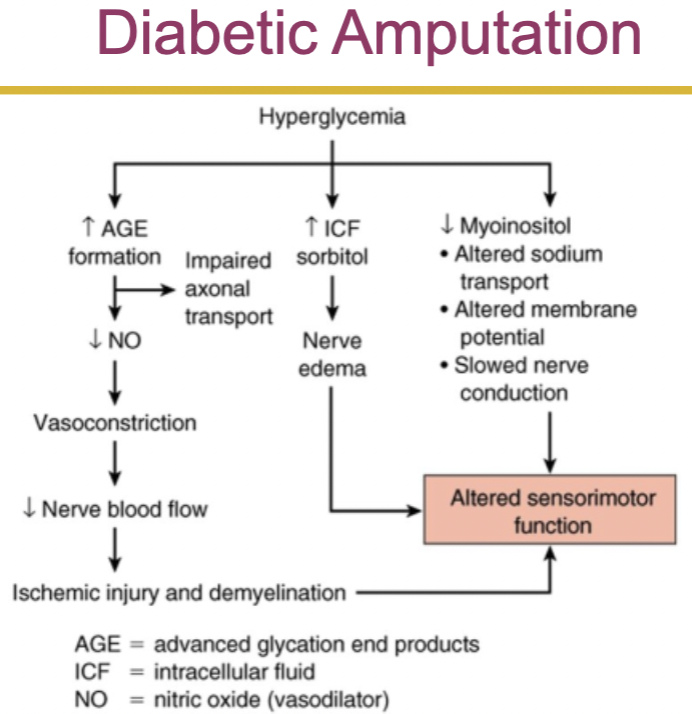
diabetic ketoacidosis:
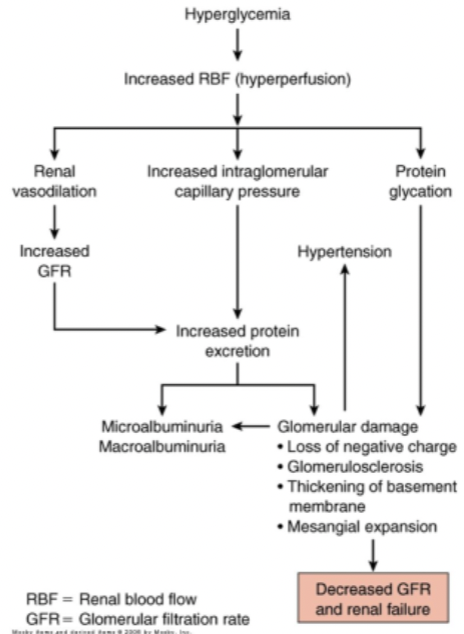
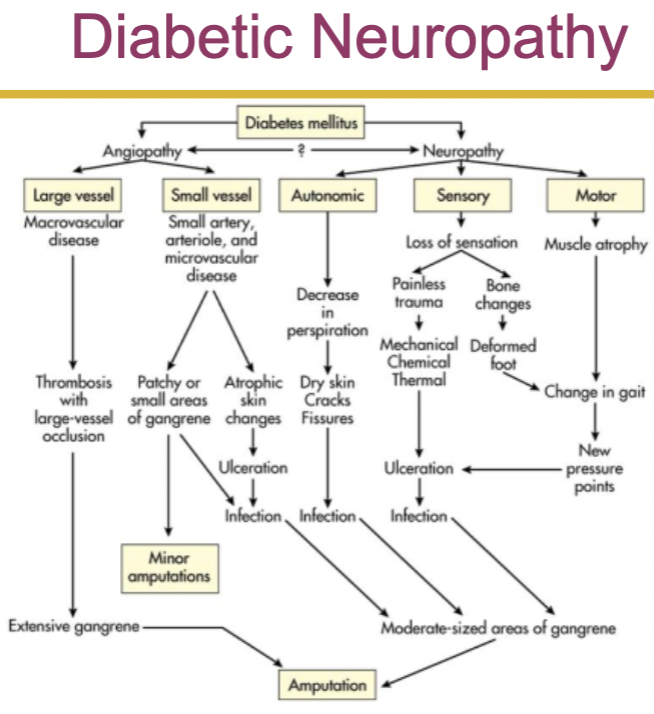
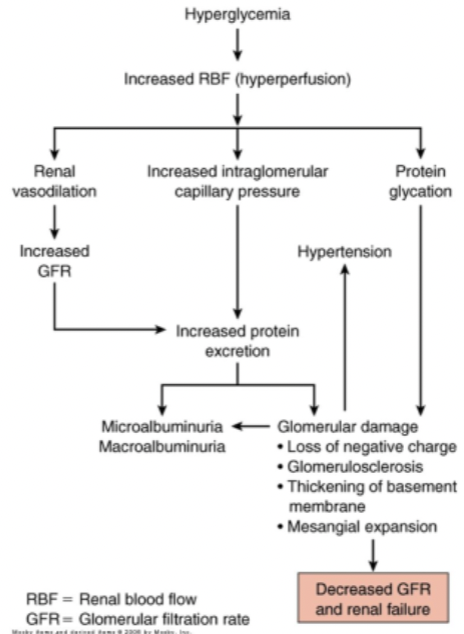
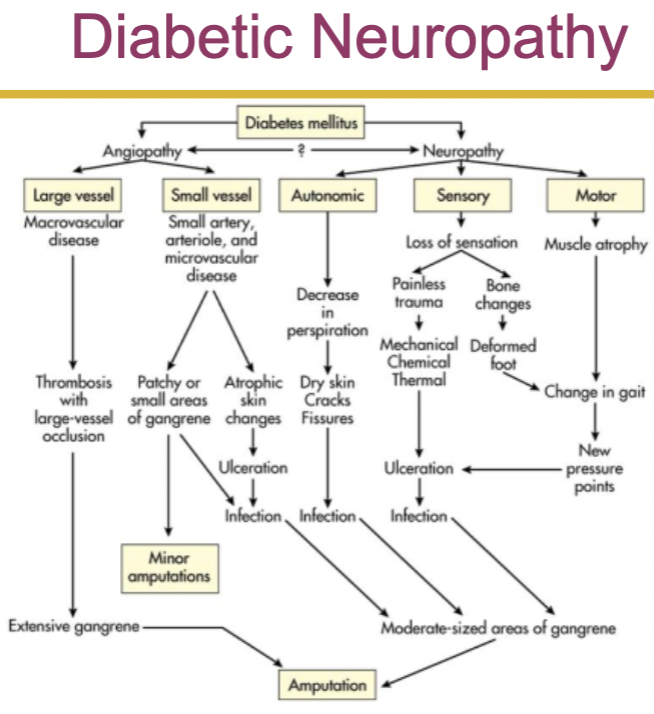
chronic complications of diabetes mellitus
hyperglycemia and nonenzymatic glycoslytion
hyperglycemia and the polyol pathway
protein kinase c
microvascular disease
retinopathy
diabetic nephropathy
macrovascular disease
coronary artery disease
stroke
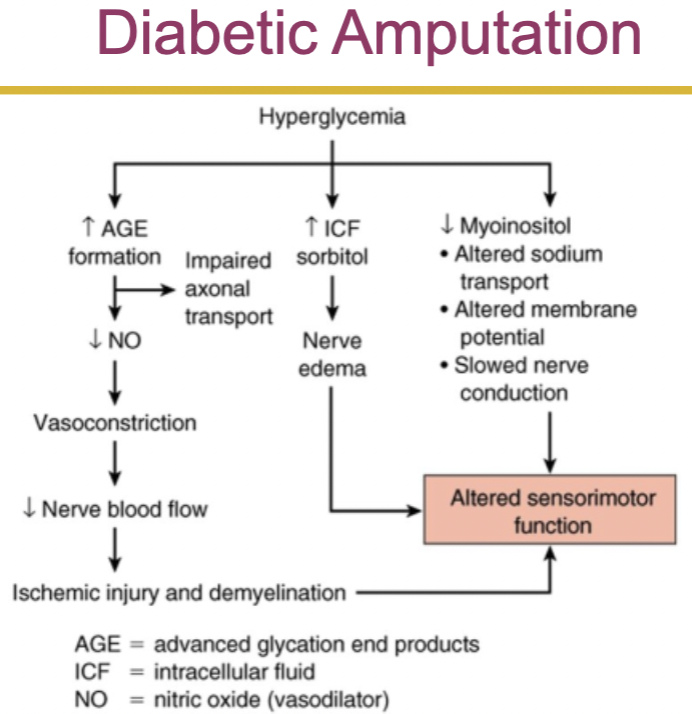
peripheral arterial disease
diabetic neuropathies
infection
alterations of adrenal function
disorders of the adrenal cortex
cushing disease
excessive anterior pituitary secretion of acth
cushing syndrome
excessive level of cortisol, regardless of cause
manifestation: hyperpigmentation, muscle wasting and protein wasting, weight gain due to:
accumulation of adipose tissue in the trunk, facial, and cervical areas
sodium and water retention
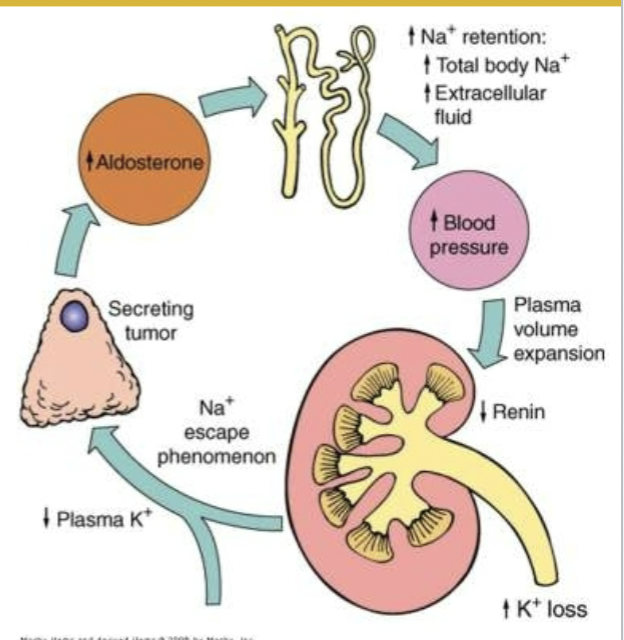
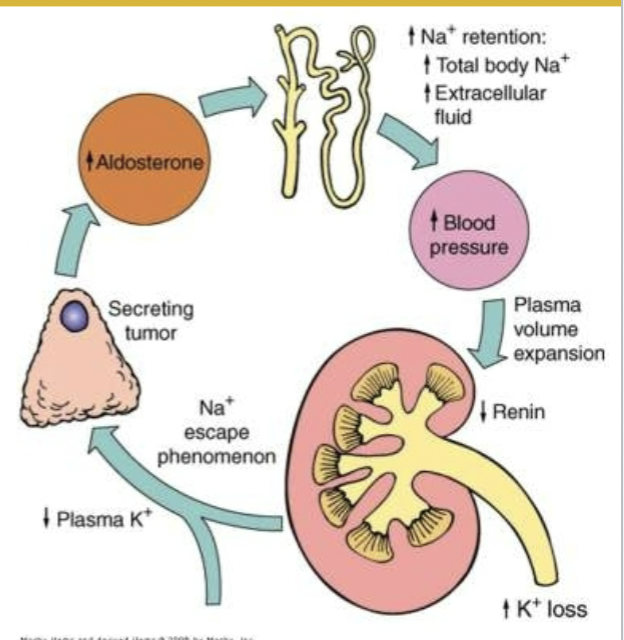
hypoaldosteronism
primary hyperaldosteronism (conn disease)
secondary hyperaldosteronism
manifestions: hypertension, hypokalemia, electrolyte and fluid imbalances
adrenocortical hypofunction
primary adrenal insufficiency (addison disease)
idiopathic addison disease
secondary hypocortisolism
manifestation: weakness, fatigue, anorexia, weight loss, nausea, diarrhea, hypotension
hypersecretion of adrenal androgens and estrogens
feminization: development of female sexual characteristics (in males)
virilization: development of male sexual characteristics (in females)
disorders of the adrenal medulla
adrenal medulla hyperfunction
caused by tumors derived from the chromaffin cells of the adrenal medulla
pheochromocytoma’s
secrete catecholamines on a continuous or episodic basis
Lecture 6: Alteration of Endocrine System
hormone definition: mainly peptides, shorter or longer, secreted in the bloodstream, travel long distances where they are received by other cells
endocrine system is a system of glands
elevated or depressed hormone levels: (what can cause it)
failure or respond (response?) to inappropriate signal of feedback systems
dysfunction of an endocrine gland
secretory cells are unable to produce, obtain, or convert hormone precursors
the endocrine gland synthesizes or releases excessive amounts of hormone
increased hormone degradation or inactivation
ectopic hormone release
target cell failure:
receptor associated disorders
decrease in number of receptors
impaired receptor function
presence of antibodies against specific receptors
antibodies that mimic hormone action
unusual expression of receptor function
how hormones work at the target cell (my notes, he said to know it)
the hormone binds to a receptor (either on plasma membrane or in cell depending on water/lipid solubility)
once the hormone binds to the receptor a signal cascade is triggered
for surface receptors, this often involves activating a g protein which is linked to the receptor and when inactive bound to gdp
once activated, the g protein released gdp and binds to gtp
the now activated g protein (attached to gtp) interacts with adenylate cyclase
adenylate cyclase converts atp into cyclic amp (cAMP) which is a second messenger
cAMP then goes and triggers a set of events that actually causes the cells response to the hormone
any issue in this process can cause disease
ex. receptor dysfunction, second messenger dysfunction, signaling pathway dysfunction
hormone delivery: (flow chart)
is appropriate amount of biologically active hormone being delivered to target cell?
yes → is another substance mimicking action of hormone?
yes → pathogenic mechanism
no → is hormone receptor binding abnormal?
yes → pathogenic mechanism
no → is initiation of intracellular events (ex. generation of second messenger) lacking?
yes → pathogenic mechanism
no → is cell response to events lacking?
yes → pathogenic mechanism
no → target cell is responding appropriately to hormone
? (unknown?) → is appropriate need recognized?
no → pathogenic mechanism
yes → is secretory cell synthesizing biologically active hormone?
no → pathogenic mechanism
yes → is delivery system functioning?
no → pathogenic mechanism
yes → is hormone metabolism appropriate? (is it being removed properly after release)
no → pathogenic mechanism
yes → is hormone being ectopically produced? (is it being produced somewhere where it shouldnt be)
no → target cell is receiving appropriate amount of hormone
yes → pathogenic mechanism
alterations of the hypothalamic-pituitary system:
(decreased hypothalamic function causes ___ which leads to anterior pituitary hormone effect __)
GnRH ↓ —> FSH ↓ && LH ↓
TRH ↓ —> TSH ↓
CRH ↓ —> ACTH ↓
PIF ↓ —> prolactin ↑
GHRH ↓ —> GH ↓
diseases of the posterior pituitary
syndrome of inappropriate antidiuretic hormone secretion (SIADH)
hypersecretion of adh without the presence of physiological stimuli
for diagnosis, normal adrenal and thyroid function must exist
clinical manifestations are related to enhanced renal water retention, hyponatremia, and hypoosmolarity
diabetes insipidus
insufficiency of adh
polyuria and polydipsia (frequent drinking/excessive thirst)
partial or total inability to concentrate urine
neurogenic
insufficient amounts of adh
nephrogenic
inadequate response to adh
diseases of the anterior pituitary
disorders of anterior pituitary may involve hypo or hyper function of the gland
hypopituitarism (deficiency or failure hormonal function)
one of the cause is pituitary infarction (death of tissue). pituitary infarction can be seen in
sheehan syndrome (ischemic pituitary necrosis)- pituitary gland is highly vascular so it is vulnerable to ischemia and infarction
hemorrhage
shock
others: head trauma, infections, and tumors
clinical manifestation depend on the affected area and affected hormones
hypopituitarism
panhypopituitarism- when all hormones are absent
acth deficiency leads to cortisol deficiency
tsh deficiency leads to thyroid hormone deficiency
fsh and lh deficiency leads to failure or loss of secondary sexual characteristics
gh deficiency leads to deficiency in growth
diagnosis: radioimmunoassay (measure hormone level), mri or ct (to measure size/look for abnormal areas)
treatment: hormone therapy
hyperpituitarism
commonly due to a benign, slow growing, pituitary adenoma
expansion of pituitary adenoma may cause both neurogenic (due to infiltration of cranial nerves) and secretory defect
manifestations
headache and fatigue
visual changes (if the tumor infiltrates the optic chiasm)
hyposecretion of neighboring anterior pituitary hormones
hypersecretion of growth hormone (gh)
acromegaly
hypersecretion of gh in adulthood (after growth plates close)
gigantism
hypersecretion of gh in children and adolescents (before growth plates close)
manifestation
interstitial edema
increased in size and function of sebaceous and sweat gland (causes increased body odor)
coarse (thick) skin
enlargement of facial bones
arthritis and backaches due to cartilaginous growth
hypersecretion of prolactin
caused by prolactinomas
in females, increased levels of prolactin cause amenorrhea (menstrual disturbances), galactorrhea (nonpuerperal milk production [milk production not caused by childbirth/breastfeeding]), hirsutism (excess hair growth), and osteopenia (reduced bone mass but not enough for osteoporosis)
in males, increased levels of prolactin cause hypogonadism (gonads dont produce enough sex hormones), erectile dysfunction, impaired libido, oligospermia (low sperm count), and diminished or decreased ejaculate volume
alterations of thyroid function
hyperthyroidism
thyrotoxicosis- primarily caused by excess thyroid hormones secreted by thyroid gland, but also could be caused by tsh secreting pituitary adenoma
manifestation: increased metabolic rate, cardiac output
graves disease- autoimmune disease
hyperthyroidism resulting from nodular thyroid disease
goiter
hypothyroidism can be primary or secondary
caused by
defective hormone synthesis due to autoimmune thyroiditis, iodine deficiency, or antithyroid drugs
loss of thyroid tissue
primary hypothyroidism
subacute thyroiditis- inflammation of thyroid by a viral infection
autoimmune thyroiditis- results granular destruction of thyroid tissue
postpartum thyroiditis
manifestation: decrease energy metabolism, low basal metabolic rate, cold intolerance, tiredness
diagnosis and treatment: clinical symptoms, decrease t4 (a hormone), hormone therapy
thyroid carcinoma
alterations of parathyroid function
hyperparathyroidism
primary hyperparathyroidism
excess secretion of pth from one or more parathyroid glands
secondary hyperparathyroidism
increase in pth secondary to a chronic disease
manifestations: excessive osteoclastic activity, pathologic fractures, curvature of spine
hypoparathyroidism
abnormally low pth levels
usually caused by parathyroid damage in thyroid surgery
manifestation: muscle spasm, hyporreflexia, laryngeal spasm
type 1 diabetes mellitus
demonstrates pancreatic atrophy and specific loss of beta cells
macrophages, t and b lymphocytes, and natural killer cells are present
two types
immune- environmental genetic factors result cell mediated destruction of beta cells
nonimmune- occurs secondary to other diseases
manifestations
type 1 diabetes affects metabolism of fat, protein, and carbohydrates
hyperglycemia, polydipsia, polyuris, polyphagia, weightloss, and fatigue
diagnosis- clinical symptoms

dysfunction of the pancreas
type 2 diabetes mellitus
maturity onset diabetes of youth (mody)
gestational diabetes mellitus (gdm)
common form of diabetes mellitus type 2
insulin resistance
acute complications of diabetes mellitus
hypoglycemia
diabetic ketoacidosis
hyperosmolar hyperglycemic nonketotic syndrome (hhnks)
somogyi effect
dawn phenomenon
diabetic ketoacidosis:
chronic complications of diabetes mellitus
hyperglycemia and nonenzymatic glycoslytion
hyperglycemia and the polyol pathway
protein kinase c
microvascular disease
retinopathy
diabetic nephropathy
macrovascular disease
coronary artery disease
stroke
peripheral arterial disease
diabetic neuropathies
infection
alterations of adrenal function
disorders of the adrenal cortex
cushing disease
excessive anterior pituitary secretion of acth
cushing syndrome
excessive level of cortisol, regardless of cause
manifestation: hyperpigmentation, muscle wasting and protein wasting, weight gain due to:
accumulation of adipose tissue in the trunk, facial, and cervical areas
sodium and water retention
hypoaldosteronism
primary hyperaldosteronism (conn disease)
secondary hyperaldosteronism
manifestions: hypertension, hypokalemia, electrolyte and fluid imbalances
adrenocortical hypofunction
primary adrenal insufficiency (addison disease)
idiopathic addison disease
secondary hypocortisolism
manifestation: weakness, fatigue, anorexia, weight loss, nausea, diarrhea, hypotension
hypersecretion of adrenal androgens and estrogens
feminization: development of female sexual characteristics (in males)
virilization: development of male sexual characteristics (in females)
disorders of the adrenal medulla
adrenal medulla hyperfunction
caused by tumors derived from the chromaffin cells of the adrenal medulla
pheochromocytoma’s
secrete catecholamines on a continuous or episodic basis
 Knowt
Knowt