320: Exam 1
Animal Sciences 320:
Lecture Two:
Health: a state of complete physical, mental and social well-being, not merely the absence of disease or infirmity.
Disease: A condition of the living animal or plant body or of one of its parts that impairs normal functioning and is typically manifested by distinguishing signs and symptoms
Somewhat vague, what does normal necessarily mean? We need statistics.
Defining disease is actually pretty hard.
Some believe that our uses of health and disease reflect value judgments
Disease is relative to what people consider normal
One person's diarrhea is another person's normal day
Illness: a person’s subjective experience of their symptoms. What a patient brings to the healthcare provider
Disease: underlying pathology; biologically defined: the health care provider’s perspective
Sickness: social and cultural conception of this condition: cultural beliefs and reactions such as fear or rejection. These affect how the patient reacts.
Defining health and disease:
Naturalism:
Most prominent philosophical approach to defining health and disease
Reference class: a natural class of organisms of uniform functional design; specifically, an age group of a sex of a species
Normal function: part or process within members of the reference class is a statistically typical contribution by it to their individual survival and reproduction.
Disease: type of internal state which is either an impairment of normal function ability.
Criticisms:
Neglects the role values play in determining healthy or diseased
Provide definitions that rely exclusively on information from the biological sciences, but lack a basis in biological theory.
If you take a data sample, are you or the animal accurately represented in the study?
Normativism:
Disease is deviancy from some alternative state of affairs which is considered more desirable
Suggests that we (both lay people and medical professionals) should use health and disease in ways that reflect our values.
Physiological or psychological state we desire are called health and those states we want to avoid are labeled diseased
Criticisms:
Case where we agree that a state is undesirable but we disagree over whether it is a disease state
Overweightness, PMS
Values can change
Hybrid Theories:
The term disease should only apply to dis-valued states with the proper biological etiology.
You need a value that applies specifically to the individual and has a base to back it up.
Criticisms:
A state where there is no evolutionary dysfunction yet we disvalue that state
Microbio:
Bacteriome
Mycobacterial communities
Virome (virus)
Macrobiome (infancy in the knowledge field):
Protozoa
Helminths (worms, flukes)
We have a relationship with them, if you destroy the relationship, you can damage the immune system that prevents things like allergies.
Lots of kids have them, but we have treatments
Colonization (normal flora, cells that aren't ours that live on our body):
Human cells (36 trillion) vs colonizing cells (39 trillion prokaryotic cells, mostly bacteria)
“Normal Flora:”
Most areas of the body in contact with the outside environment harbor resident microbes
Microorganisms that normally reside at a given site and under normal circumstances do not cause disease
Normal flora is essential for health:
Create an environment that may prevent infections
Enhance host immune defenses
Internal organs, tissue, and fluid are microbe-free (relatively)
Transient Flora:
Occupy the body for only short periods
Usually picked up during daily activities
Surfaces (door knob, hand-shake, etc)
Often eliminated easily
Resident Flora
Are permanently established (or for long periods of time)
Types of relationships with microbiome
Mutualism
Both the host and the microbe benefit
Ruminants and their gut microorganisms
E. Coli- microbe receives nutrients, but produces vitamins K and B-complex
Commensalism
One partner benefits, and the other neither benefits nor is harmed
Parasitism
One organism benefits at the expense of the host
An external parasite to cause infestation
Internal parasite to cause infection
Pathogenic
Organism causes damage to the host during infection
Microbiomes are critical at an early age, they set things in motion
Initial Colonization
Uterus and contents are normally sterile and remain so until just before birth
Breaking of fetal membrane exposes the infant; all subsequent handling and feeding continue to introduce what will be normal flora
Is this paradigm entirely correct?
It might have an exposure even before birth
Triangle:
Microbiome→Immune system→Nutrition
Defining Infections
Infectious agents: viruses, bacteria, fungi, protozoa, worms, and prions
Infection: condition in which infectious agent penetrates host defenses
Infectious disease: an infection that causes damage or disruption to tissues and organs and/or physiological homeostasis
Endogenous infections
Occurs when normal flora is introduced to a site that was previously sterile
Exogenous Infections
Caused by organisms that are not normally present in the body but have gained entrance from the environment
Types of pathogens
True pathogen: infectious agent that causes disease in virtually any susceptible host
Opportunistic pathogen: normally harmless; causes disease when the normal flora is disrupted (i.e. by antibiotics) or when the host is immunocompromised
Patterns of Infection:
Localized infection: infectious agent enters the body and remains confined to a specific tissue
Systemic infection: infection spread to several sites and tissue fluids, usually the bloodstream
Focal infection: infectious agent breaks loose for a local infection and is carried to other tissue
Mixed infection: several microbes grow simultaneously at the infection site (polymicrobial)
Primary infection: refers to the first time you are exposed to (and infected by) a specific pathogen
Secondary infection: another infection by a different microbe, succeeding a primary infection (getting a UTI treatment and getting a yeast infection because of it)
What defines a particular disease
Signs (objective evidence): something can be detected/measured by someone else
Symptoms (subjective evidence): something that must be described by the one suffering from the disease
Syndrome: the complete set of signs and symptoms associated with a specific disease
Patterns of infection
Acute infection: comes on rapidly, with severe but short lived effects
Chronic (persistent) infection: progresses and persists over a long period of time
Infections that get unnoticed:
Asymptomatic (subclinical) infections: although infected, the host does not show any signs of disease
“Typhoid Mary”
First person in the USA identified as an asymptomatic carrier of the salmonella Typhoid Fever
Acquisition and Transmission of infectious agent:
Communicable infection: infected host can transmit the infectious agent to another host
Non-communicable infection: infection does not arise through transmission from host to host
Nosocomial infections
Infections acquired or developed during hospital stay
Presence of microorganisms in hospital environment→ compromised host→ chain of transmission
Lecture Four:
Epidemiology: the study and analysis of the patterns, causes, and effects of disease and health-related factors. “The study of what befalls upon people.”
Epi- on, upon, befall
Demo- people
Ology- the study of
Major areas of epidemiological study include
Disease etiology
Transmission
Outbreak investigation
Disease surveillance
Forensic epidemiology and screening
Biomonitoring
Comparisons of prevention/treatment outcomes
Epidemiologic Triad
Host(→vector) → environment(→vector) → agent(→vector), if you can break this link, you can control the vector
Pathogen Traits
Type: viruses, bacteria, fungi, protozoa, worms, prions
Other info
Virulence:
Ability to cause severe disease
Virulence factors: specific mechanisms that allow pathogen to adhere to or penetrate host cell, thwart immune defenses, damage host
Infectious Dose:
Minimum number of pathogens required to cause illness
Incubation Period:
Time it takes after first exposure for the pathogen to cause signs and symptoms; influences extent of spread
Things that sleep for a long time (takes a long time to show symptoms such as HIV) are harder to control since it can spread while no symptoms are present. Things that spread fast (like COVID) can wipe an entire village before it spreads and thus doesn't spread anymore.
Infectious Dose (ID)
If ID is not reached, infection will not occur
It is defined in a particular population, (young people vs old)
ID50
Amount of pathogenic microorganisms that will produce demonstrable infection in 50% of exposed hosts
Signs of clinical infections
Latent period: exposure, but no symptoms
Incubation period: no signs or symptoms, but infection has begun
Prodromal Period: mild signs or symptoms
Period of illness: most severe signs and symptoms
Period of decline: signs and symptoms
Period of convalescent: illness goes away are you are back to normal health
Host traits:
Immunity to Pathogen:
Previous exposure, immunization
Antigenic variation of pathogen can overcome
General Health:
Malnutrition, overcrowding, fatigue
Developing world more susceptible: crowding, poor nutrition, poor sanitation
Age:
Very young, elderly generally more susceptible
Immune system less developed in young: wanes in old.
Elderly also less likely to update immunizations
Genetic background
Natural immunity varies widely
Specific receptors critical for infection may differ in individuals
Sickle cell gene and resistance to malaria
Gender:
Pregnant animals are at more risk
Pregnant animals can pass on some diseases to offspring
Religious and cultural practices:
Breastfeeding provides protective antibodies to infant
Consumption of raw fish can increase exposure
Environmental Factors:
Environmental factors may increase likelihood of disease transmission opportunities or lower the hosts resistance to infection
Heat or cold stress
Food availability
Hygiene
Crowding
Cultural practices
Presence of vectors or reservoirs for pathogen
Routes of transmission
Direct contact: physical contact or fine aerosol droplets.
Some pathogens cannot survive in environment
Hand washing considered single most important measure for preventing spread of infectious disease
Horizontal vs vertical transmission
Indirect contact
Some pathogens can survive for a period outside the host
Transmission of infectious disease
Fomite: inanimate object that serves a role in disease transmission
Vector: any agent that carries a pathogen and transmits it to human or animal hosts
Vehicle: typically food, water or air, that transmits a pathogen to the host
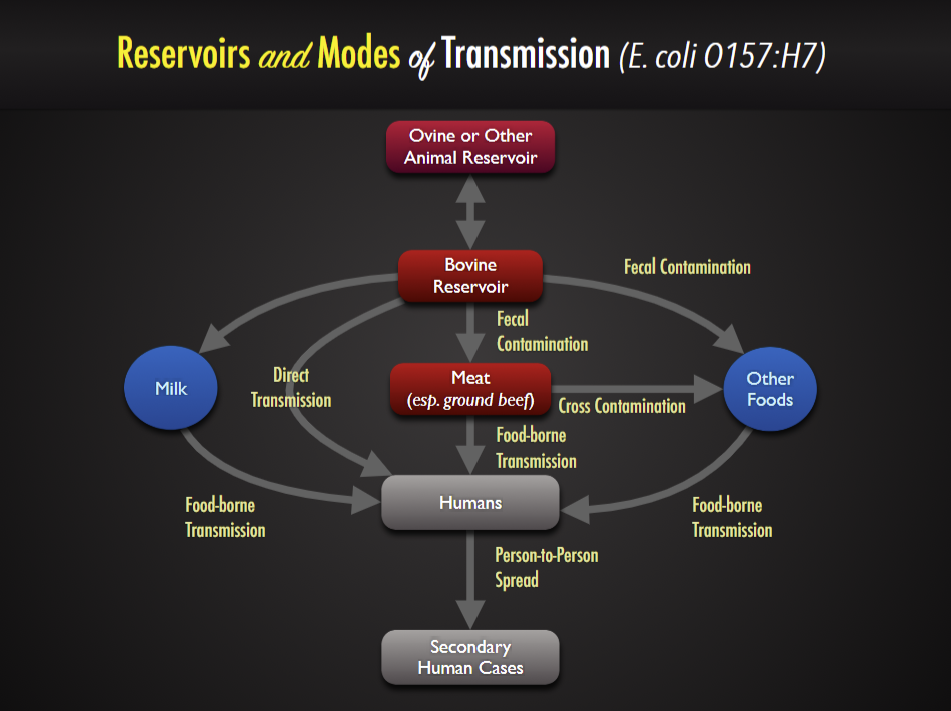
Reservoir: the natural habitat in which a pathogen lives and reproduces that serves as a source of infection
Living reservoir may be symptomatic or asymptomatic
Exclusively human reservoirs are easier to control
Non-human reservoirs challenging to control
Environmental reservoirs: difficult or impossible to eliminate
Lecture Five:
Portals of entry and exit
Skin
Gastrointestinal tract: food, drink, other ingested materials
Respiratory tract
Urogenital tract
Transplacental
Vehicles of entry and exit
feces/urine
semen/ vaginal secretions
Sputum
Spit
Cycle of transmission
Frequency of cases
Prevalence: total number or proportion of cases or events or conditions in a given population
Incidence: number of new cases during a specified time period
Morbidity Rate: number of people afflicted with a certain disease during a given period of time
Mortality rate: number of deaths in a population due to a certain disease during a given period of time
Case-fatality rate: percentage of people with a specific disease that dies from that disease
Attack rate: number of people affected by a disease divided by the number of people with a specific exposure
Disease occurrence patterns:
Endemic: a relatively steady frequency over a long period of time in a particular geographic locale (common cold)
Sporadic: when occasional cases are reported at irregular intervals (rabies)
Epidemic: increasing prevalence of a disease beyond what is expected
Pandemic: epidemic across countries and continents
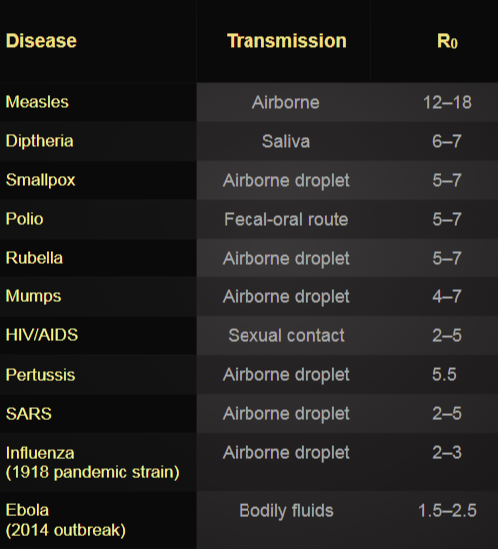
Basic Reproductive Number (R0)
The average number of new infections generated by one infection in a completely susceptible population
EX: is R0=2, for every infected person, two people will become infected
Measure of the intrinsic potential of an infectious agent to spread
R0 = C x P x D
C= contact rate (contact/time)
The average rate of contact between susceptible and infected individuals
P= transmissibility (infection/contact)
The probability of infection given contact between a susceptible and infected individual
D= duration of infectiousness (time/infection)
Effective reproductive number ®
A population will rarely be totally susceptible to an infection in the real world. The effective reproductive rate ® estimates the average number of secondary cases per infectious case in a population made up of both susceptible and non-susceptible hosts
R = R0 x S
R0= basic reproductive number
S= fraction of the host population that is susceptible
Lecture Six:
Koch’s Postulates
The microorganism must be found in abundance in all organisms suffering from the disease, but should not be found in healthy organisms.
The microorganism must be isolated from a diseased organism and grown in pure culture. (not all microorganisms can be put on a pure culture)
The cultured microorganism should cause disease when introduced into a healthy organism.
The microorganism must be reisolated from the inoculated, disease experimental host and identified as being identical to the original specific causative agent.
Bacterial Shapes
Coccus (round ball)
Bacillus (rod)
Spiral
Coccobacillus
Vibrio (rod and spiral shape)
Flagella
Presence is species/strain dependent
For motility
Number and arrangement vary
Pili/fimbriae:
Hair-like structures, fimbriae shorter than pili
adhere/attach to surfaces
F or sex pilus: used for transfer of genetic material from one bacteria to another
Can provide resistance against engulfment by phagocytes.
Endospore formation
Under stressful environments, certain gram-positive bacteria are capable of forming endospores.
Types of Bacterial Pathogen
True Pathogen: infectious agent that causes disease in virtually any susceptible host
Opportunistic pathogen: (pseudomonas, staph), normally harmless; causes disease when the normal flora is disrupted or when the host is immunocompromised
Bacterial Adhesion:
Necessary to avoid innate host defense mechanisms
Adhesion is often an essential preliminary step to colonization and then penetration through tissues.
At the molecular level, adhesion involves surface interactions between specific receptors on host cell membrane and ligands on the bacterial surface.
Nonspecific surface properties of the bacterium, including surface charge and hydrophobicity, also contribute to the initial stages of the adhesion process.
Mechanisms of Adherence to cell or Tissue surfaces
Non-specific adherence: reversible attachment to the surface
Specific adherence: irreversible permanent attachment to the surface.
Tissue tropism: particular bacteria are known to have an apparent preference for certain tissues over others
Species specificity: certain pathogenic bacteria infect only certain species of animals.
Genetic specificity within a species: certain strains or races within a species are genetically immune to a pathogen.
Exotoxins: proteins produced inside the pathogenic bacteria, most commonly gram-positive bacteria, as part of their growth and metabolism. The exotoxins are then secreted into the surrounding medium during the log phase.
Most powerful human poisons known and retain high activity at very high dilutions.
Endotoxins: lipid portions of lipopolysaccharides that are part of the outer membrane of the cell wall of gram-negative bacteria. The endotoxins are liberated when the bacteria die and the cell wall breaks apart.
Lecture Seven:
Virions/Viruses
Acellular and the virion consist of:
DNA or RNA core
Protein coat (capsid)
Lipid envelope (spikes on some viruses)
Can infect all types of life forms including bacteria and archaea
Can replicate only when within living host cell
Two systems of virus classification:
Hierarchical virus classification system
nature of the nucleic acid: RNA or DNA
symmetry of the capsid
presence of absence of an envelope
dimensions of the virion and capsid
The Baltimore classification
viruses can be classified into seven (arbitrary) groups
Viral Attachment and Entry
Direct Penetration
Membrane fusion
Endocytosis
Transmission → attachment absorption → Entry→ (Latency-survival in host) → replication→ shedding (pathology to Host)
Virtual Replication
Uncoating
transcription/mRNA production
Synthesis of virus components
Virion Assembly
Viral Shedding
Via Budding
Via Apoptosis