Buruli ulcer (BU)
summary
Buruli Ulcer (BU), caused by Mycobacterium ulcerans, is a debilitating soft tissue infection characterized by chronic, progressive non-healing ulcers, leading to cosmetic deformity and functional impairment. It is most prevalent in Victoria (Bairnsdale ulcer) and Far North Queensland (Daintree or Mossman ulcer), with cases rising in urban areas like Melbourne and Geelong. Transmission occurs through direct contact with contaminated environments or potentially zoonotically from possums. The condition mostly affects older adults, presenting as painless lesions, which can develop into necrotic ulcers. Diagnosis usually requires PCR testing from ulcer swabs or biopsies. Management primarily involves antibiotic therapy, emphasizing informed patient expectations regarding prolonged healing times and potential paradoxical reactions post-treatment. Surgery may assist in wound care or rapid closure, while good wound care practices are essential in preventing infections and promoting healing. Protective measures against mosquito bites are advised as preventive strategies.
definition
caused by Mycobacterium ulcerans, is an under-recognised, debilitating soft tissue infection, which typically causes chronic progressive non-healing ulcers. These lesions can result in severe cosmetic deformity, functional impairment and substantial financial cost and have psychological consequences
epidemiology
Endemic regions include Victoria, where BU has been called Bairnsdale ulcer, and regions of Far North Queensland, where it is known as Daintree or Mossman ulcer.
increasing numbers of cases have been acquired in large urban centres of Melbourne and Geelong.
Acquisition is most likely during summer, when mosquito colonies tend to peak and humans have greater exposure to the outdoors.
the incubation period is four to five months, most cases are diagnosed in winter and spring
transmission
direct human contact with environmental sources, such as contaminated water, soil or vegetation
it is potentially a zoonotic disease » infection spills over from the possum population,
potentially through mosquito transmission to human hosts or through contact from environmental sources contaminated by possum excreta
no reported cases of human–human transmission
Clinical features:
median age: 66 y/o
location
often spare the soles of the feet and palms of the hands
commonly on the distal aspect of limbs» especially around large joints
lesions are usually solitary, but 5% have more than one lesion
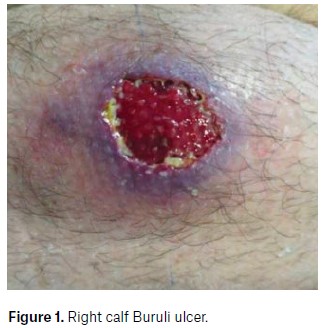
lesions are painless initially often manifest as non-ulcerative lesions, such as nodules, plaques or papules. Over time, these lesions ulcerate. They typically have a necrotic base, undermined edges and surrounding erythematous induration
Oedematous lesions, which clinically mimic cellulitis, account for 8% of cases and are the most rapidly progressive and destructive lesions.
Secondary bacterial infection of the wound is uncommon, but it should be suspected in the presence of pain, fever and wounds appearing inflamed
3 categories of severity:
1» lesion< 5cm
2» lesion 5-15 cm
3» lesion > 15 cm




DX
M. ulcerans nucleic acid detection by PCR testing on a swab of the ulcer is the diagnostic test of choice
Culture is less sensitive and it can often take weeks to months
Importantly, PCR swab needs to be specifically requested and sent separately to a culture swab, if performed.
In ulcerative lesions, the circumference of the undermined edge of the ulcer should be swabbed and visible wound material should be observed on the swab itself.
a negative PCR test does not exclude the diagnosis. This happens more frequently in children and lesions swabbed early on. When there is a high index of suspicion, repeat PCR should be performed, preferably with fresh tissue from a biopsy.
In non-ulcerative lesions, because M.ulcerans exists subcutaneously, these lesions require biopsy for diagnosis.
Management:
Antibiotic
Antibiotic therapy is the cornerstone of BU
Consultation with an infectious disease physician is recommended.
First-line treatment in adults includes :
rifampicin 10 mg/kg to a maximum daily dose of 600 mg/day (adult and child),
+ with either
clarithromycin 500 mg twice a day (child=7.5mg/kg BID, max=500mg BID)
or ciprofloxacin 500 mg twice a day (not recommended in children)
or moxifloxacin 400 mg/day (not recommended in children)
for 8 weeks.
Dose reduction of clarithromycin and ciprofloxacin if renal function is impaired.
educate patients about the side effects of long-term antibiotics:
gastrointestinal upset,
hepatotoxicity,
hypersensitivity,
C. difficile infection,
antibiotic-associated diarrhoea
rarely, neuropsychiatric side effects
peripheral neuropathy.
warn that it is normal to have red discolouration of bodily fluids due to rifampicin.
Clarithromycin and quinolones can cause QTc prolongation» take a baseline ECG
Fluroquinolones are associated with tendinopathy, and caution is advised in older patients and those on corticosteroid therapy.
Potential drug interactions are common
Due to the risk of hepatotoxicity, alcohol abstinence is also recommended.
Patient expectations
should be addressed prior to treatment, as most lesions persist after the completion of antibiotics, known to take up to 12 months to fully heal after treatment. one in five patients develop a paradoxical reaction to antimicrobial therapy, with deterioration in the appearance of the lesion after treatment commences and occasionally development of a new lesion in separate parts of the body.
Paradoxical reactions tend to occur more in :
oedematous lesions and
people aged >60 years.
relapse
it is important to monitor for signs of relapse after treatment completion. Risk factors for relapse include:
obese
male
on immunosuppressive agents.
Surgical management
Surgery is not required to cure lesions but continues to have a role when :
medical therapy is not tolerated,
when patient preference is for rapid wound closure in small ulcers,
debridement of necrotic tissue to improve wound healing,
in extensive ulceration when wound healing is felt to be significantly Small lesions can be cured by surgery alone with wide margins,
but large lesions benefit from adjuvant antibiotic therapy for four to eight weeks prior to surgery to reduce inflammation.
Wound care
Good wound care is important to improve healing rates and prevent secondary infection.
The general principles of wound care should be adhered to, including
debriding necrotic tissue,
reducing tissue oedema,
providing moisture and nutrition to the wound
protecting it from further soiling or trauma.
Necrotic wounds benefit from the use of topical debriding agents, and those with copious exudate might require daily to alternate daily dressing changes with absorbable materials.
Heat therapies
cause local controlled hyperthermia of infected soft tissue in the setting of BU. In vitro, M. ulcerans is nonviable at temperatures >37°C.
clinical trials using heat packs for an average of 10 hours per day for eight weeks showed the efficacy of heat therapy
Heat therapy could be considered when antibiotic therapy and surgical management are not possible or desired.
preventive strategies that reduce mosquito bites through repellents and nets are associated with reduced risk of BU. protective long-sleeved clothing is worn in endemic areas and proper wound care might also reduce acquisition risk