Clinical Anatomy
Head and Neck
Challenging Spaces in the Skull
Rooms of the Skull
- Anterior Cranial Fossa
- Middle Cranial Fossa
- Posterior Cranial Fossa
- Orbit
- Maxillary Sinus
- Oral Cavity
Tentorium Cerebelli and the PCF
- Petrous Ridge - separates the MCF and the PCF
- Tentorium
- Below is the cerebellum, brain stem and visual cortex
- separating cerebellum & cortex below from cortex above
- Come together between the cerebral hemispheres at the falx cerebri
Things Happen Faster in the Posterior Fossa
- It takes smaller masses to obstruct and elevate CSF pressure when below than above the tentorium due to compression of Aqueduct of Sylvius
- 0 extra space, so any amount of CSF pressure can affect vision
Pterygopalatine Fossa
- On the backside of the Maxillary bone
- “behind the zygomatic arch”
- Contents:
- Maxillary nerve
- Vidian nerve
- greater superficial petrosal nerve
- deep petrosal nerve
- Pterygopalatine ganglion
- Maxillary artery
Infratemporal Fossa
- space behind the muscle and zygomatic arch
- temporalis muscle fills most of the IF
- Contents:
- Branches of the Maxillary Artery
- Middle Meningeal artery
- Inferior Alveolar artery
- Deep Temporal artery
- Buccal artery
- Pterygoid venous plexus
- lots of blood leaving the orbit will go here
- Nerves
- Mandibular nerve
- Inferior alveolar nerve
- lower teeth and gums
- Lingual nerve
- Buccal nerve
- Chorda tympani nerve
- Otic ganglion
Vasculature
Palpable Landmarks
- Face
- Frontal eminence
- Supraciliary ridge
- Auricle AKA Pinna
- Commissure of lips
- Super Alveolar ridge
- Glabella
- Nasion (bridge of nose)
- Zygomatic arch
- Nares (nostrils)
- Mental (chin)
- Head
- Preauricular lymph node
- Submandibular lymph node
- Angle of mandible
- Thyroid notch
- Laryngeal prominence AKA Adam’s apple
- Neck
- C7 - vetebra prominens
- Platysma
- Mastoid Process
- Sternocleidomastoideus
- Clavicular head
- Sternal head
Neck Muscles and Triangles
- Borders of carotid triangle
- Muscles - innervated by CN XI
- Sternocleidomastoid muscle
- Trapezius
==The Ear and Paranasal Sinuses==
Ear
Outer Ear
- Auricle (pinna)
- External Auditory Canal
- Tympanic membrane
Middle Ear
- Tympanic cavity
- Ossicles
- malleus
- incus
- stapes
- Eustacian tube
Inner ear
- Bony labyrinth
- Membranous labyrinth
@@Cranial Nerve V@@
Trigeminal AKA CN V
- Leaves the brainstem from the pons as a large sensory branch and a smaller motor branch which fuse to form the trigeminal ganglion AKA gasserian ganglion
- From the gasserian ganglion three divisions arrive:
- V1 - ophthalmic
- V2 - maxillary
- V1 and V2 are purely sensory
- V3 - mandibular
- mix of sensory and motor
CN V and the Cavernous Sinus
V1, V2 and the Pterygopalatine Fossa
Nasociliary Nerve
Herpes Zoster (Shingles)
V1, V2, and V3
- V1 sensory field includes cornea and superior palpebral, plus bulbar conjunctiva
Cranial Nerve VII
Bilateral Cortical Representation
- if CN VII doesn’t work, bilateral cortical representation will allow eyelid to still work
- lower facial muscles on the opposite side will not work
CN VII in the Ear
- stapedius muscle - dampens the vibrations in the stapes bone
- leaves where the pons meets the medulla
- stylomastoid foramen - main trunk of CN VII will emerge from the base of the skull
- internal acoustic meatus - here CN VII and CN VIII travel together
Glands, Lymphatics, and the Larynx
Submandibular Gland
- innervated by CN VII
Sublingual Gland
- salivary gland that is located under the tongue
- below is hypoglossal nerve (CN XII) that is responsible for moving the tongue
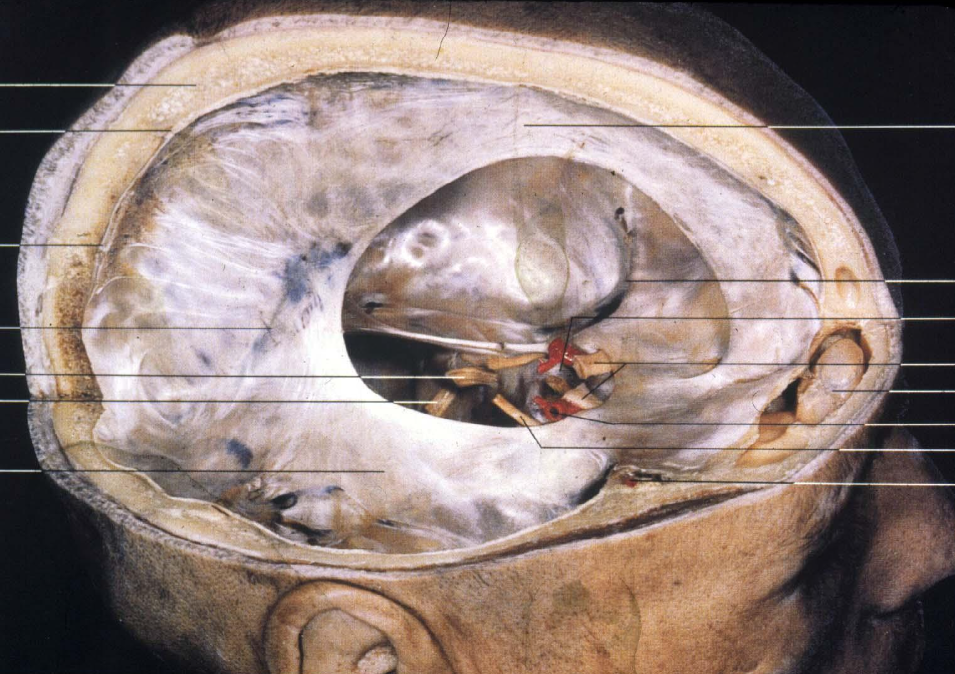
Parotid Gland Dissection
- grainy looking stuff in red box is parotid salivary gland
- makes saliva and brings it to the upper part of mouth
- duct crosses over chewing muscles, and enter mouth above and lateral to 2nd molar
- CN VII comes out of stylomastoid foramen behind ear, comes around and comes out of parotid gland
- swelling on one side, ipsilateral CN VII palsy → compromise in lid movement
- Platysma → served by cervical branch of CN VII
- Orbicularis oculi muscle
- Otic ganglion CN IX
- Parotid is seen as cloud, Stenson’s duct is the output of the parotid
Thyroid Gland
- bridges midline
- covers 2nd and 3rd tracheal ring
- endocrine gland
- participates in calcium regulation
- receives superior thyroid artery from external carotid and inferior thyroid artery from thyrocervical trunk
- superior and middle thyroid veins drain into internal jugular, inferior thyroid vein drains into brachiocephalic
- 2 arteries to serve, and 3 to drain
Parathyroid Glands
- also participate in calcium regulation
- 4 of them
- found attached to the back surface of the thyroid gland
- location can very substantially
- start from a nodule of tissue in neck, that then descend
- Roman numerals used to label it, refer to structures called ==brachio arches== in which these structures come from
- higher is IV, and lower is always III
- Sometimes the glands can be dragged into the mediastinum (area between 2 lungs)
- Around here is part of CN X, because of that recurrent laryngeal branch of CN X may occur
- left loops under the aortic arch (THORAX)
- right under subclavian artery (NECK - above 1st rib)
Tubarial Glands
- New salivary glands that have been discovered recently
- found at orbital apex, were lighting up on a scan that they were doing
- assume they receive parasympathetic innervation from the same pathway that would provide parasympathetics to the nasal and pharyngeal mucosa
Head and Neck Lymphatics
- Medial portion of the lids and conjunctiva → submandibular nodes
- Lateral portion of lids and conjunctiva → pre-auricular nodes
- AKA superficial parotid nodes
Lymphatic Basins
- neck divided into portions called lymphatic basins
- drainage patterns exist
Locating Sentinel Nodes by Scintigraphy
- dye or a radioactive material is injected in the tumor → lymphatic drainage delivers the injected material to the main draining mode
Larynx - External Views
- Surface features
- laryngeal prominence AKA adams apple
- thyroid notch
- both rise upon swallowing
- Principal functions
- valve separating airway from GI system
- voice production
9 Laryngeal Cartilages
- 3 paired and 3 unpaired
- Thyroid (U)
- Cricoid (U)
- Arytenoid
- Corniculate
- Cuneiform
- Epiglottis (U)
Thyroid Cartilage
- superior/inferior horn
- relative depth of voice is related to length of vocal cord
Posterior Larynx
- back of the hyoid bone
Laryngoscope View
- can see the false and true vocal cords, epiglottis and inside of the trachea
Larynx sections
- interior subdivided into false and true vocal folds
- [[vestibule - above false vocal folds[[
- ]]vestibular folds - false vocal folds]]
- {{ventricle - between true and false vocal folds{{
- }}infraglottic cavity - below true vocal folds}}
Phonation
- intrinsic muscles of the larynx innervated by recurrent laryngeal branch of CN X
- rima glottidis - aperture between vocal folds
- glottis - collective term for vocal folds, rima and narrow part of larynx at level of folds
Deglutition
voluntary - bolus is pushed from mouth → oropharynx
- tongue ends up against the hard palate
@@involuntary@@ - very rapid, no chewing and no breathing
- larynx is protected by closure of vestibule and epiglottis and posterior movement of base of tongue
voluntary - contraction of inferior constrictor of pharynx milks bolus into esophagus
Lids
Gross Features of the Lids
Lid Closure
- when the lid closes, the eye elevates
- if the lids are open during sleep, damage will be done to the inf cornea NOT the central cornea
Tear Meniscus and Lacrimal Lake
- tear meniscus present on both the top and bottom lids
Landmarks of the Lids
- MGO
- Grey Line
- Lashes
Layers of the Lid
- Lid skin
- epidermis
- dermis
- no hypodermis
- lids will never get thicker in weight gain because there is no fat there
- Orbicularis oculi muscle
- principle muscle, closes the lids
- (Levator Palpebral Muscle) - skeletal muscle
- raises the lid
- Levator Aponeurosis - orbital septum
- sheet that travels around the whole eye, “barrier”
- if infection occurs anteriorly to septum, it will be slowed down from entering the orbit
- Tarsal plate/Mueller’s muscle
- Across the lid like reinforcement, Meibomian (tarsal) glands reside here
- Mueller’s muscle is smooth muscle, attaches to the top of the Tarsal plate
- holds lid there once its been lifted
- smooth muscle → ANS
- Palpebral Conjunctival Stroma
- Palpebral Conjunctival Epithelium
Epidermis and Dermis
- Basal Cell layer
- Prickle cell layer
- Granular layer
- Keratinized layer
- Rete pegs
- Lid skin
Orbicularis Oculi Muscle - Temporal Branch of CNVII
- Orbital part
- portion that is over/outside the bone, outermost section
- Preseptal part
- below the orbital rim, but it about the tarsal plate
- Pretarsal part
- overlies the tarsal plate, getting closer to the lid margin
- Muscle of Riolan
- rims the lid margins, upper and lower lid
- Horner’s muscle
- where the superior and inferior muscle of Riolan fuse at the medial canthus, and attach to the bone
Bilateral Cortical Representation
- inputs to the portion of the motor nucleus of CN VII serving the temporal branch are bilateral
- lesion above nucleus
- lesion below nucleus, then bilateral cortical representation is affected, lid will not close effectively
Levator Aponeurosis and Whitnall’s Ligament (WL)
- striated white tissue that runs all the way around the lids
- Aponeurosis of Levator Palpebrae
- tendon that fans out to attach to the entire surface of the tarsal plate, which then means it can pull on it all at once and bring up the lid smooth
- Whitnall’s Ligament - large CT band that connects to upper medial portion behind the orbital rim, and then runs right along the levator all the way across to lacrimal gland
- looking from the side, the ligament just looks like support of the levator
- going through the slit of the ligament, we change the axis of the pull
- point to which the muscle is pulling the lid
Tarsal Plates
- DCT, laterally and medially stabilized by lateral and medial palpebral (canthal) ligaments
- Medial canthal ligament, attach to the medial tarsal plate….?
Glands of Lids
- Sebaceous
- Accessory
- Moll-modified sweat glands
- Eccrine is the same as merocrine
- Meibomian glands
- Glands of Zeiss
- Glands of Moll
- modified sweat glands, need to get those hormones out into the sea already!
- Goblet cells
Blood Supply
- Lateral palpebral arteries → arise from lacrimal artery
- medial palpebral arteries → arise as direct branches of the ophthalmic artery
Danger Zone of the Face
- venous drainage of the face goes into the cavernous sinus
- infections in this area can cause cavernous sinus thrombosis or brain abscess
Nasolacrimal Drainage System
- exocrine gland, so needs a duct to help with travel
- Lacrimal gland → Inferior puncta → Lacrimal sac → Nasolacrimal duct → Inferior concha/meatus
- Blink cycle
- Lid is open, lacrimal sac is at atm pressure and is filled with tears, initiate a blink, lacrimal sac is squeezed, tears are squirted out the bottom into the inferior meatus, valve of Hasner closes after tears are deposited, lids come together, both puncta immersed in lacrimal lake and draw in fluid to reinflate the sac (relieve the negative pressure)
Embryology of Branchial Apparatus
Branchial Apparatus
- cranial region of embryo resembles a fish
- branchial apparatus in fish become the gills, for humans these structures become reabsorbed
- Composed of
- pharyngeal/branchial arches
- branchial grooves
- pharyngeal pouches
Branchial Arches
appear at 3rd week
6 arches - 5th and 6th are vestigial in humans
First 2 arches are named:
- Mandibular
- divided into smaller → upper maxillary processes and lower, larger mandibular processes
- Hyoid
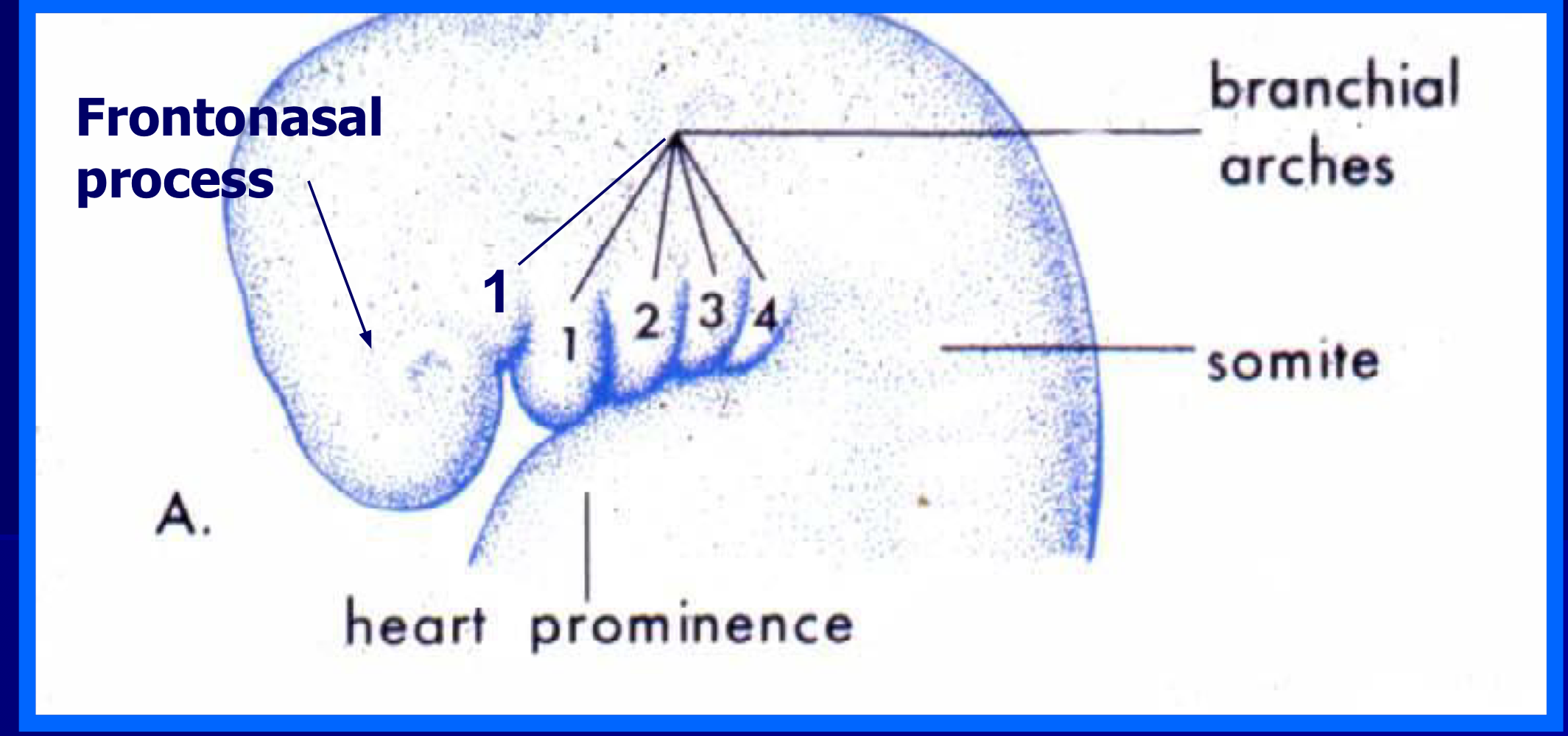
Above the first arch is the frontonasal process
Each arch contains:
Aortic arch artery
original pattern is 6, in humans it is 4
1st and 2nd arch arteries resorbed completely - stapedial artery, a branch of second aortic arch, pierces Reichert’s cartilage and accounts for whole in stapes bone when artery is reabsorbed
asymmetric reabsorption accounts for recurrent laryngeal looping under aortic arch on left vs higher subclavian on the right
Cartilaginous bar
1st arch - Meckel’s
- skull is membrane bone, this cartilage establishes plane for formation of mandible but does not ossify to form it
- ossification does create malleus and incus
2nd arch - Reichert’s
- upper hyoid bone, stylohyoid ligament, styloid process and stapes
3rd arch - remainder of hyoid bone
4-6th arch - cartilages of the larynx
some muscle
[[Arch 1 – muscles of mastication[[
]]Arch 2 – muscles of facial expression]]
{{Arch 3 – various but not a specific grouping{{
}}Arch 4 – intrinsic muscles of larynx}}
cranial nerve
[[1st arch - CN V[[
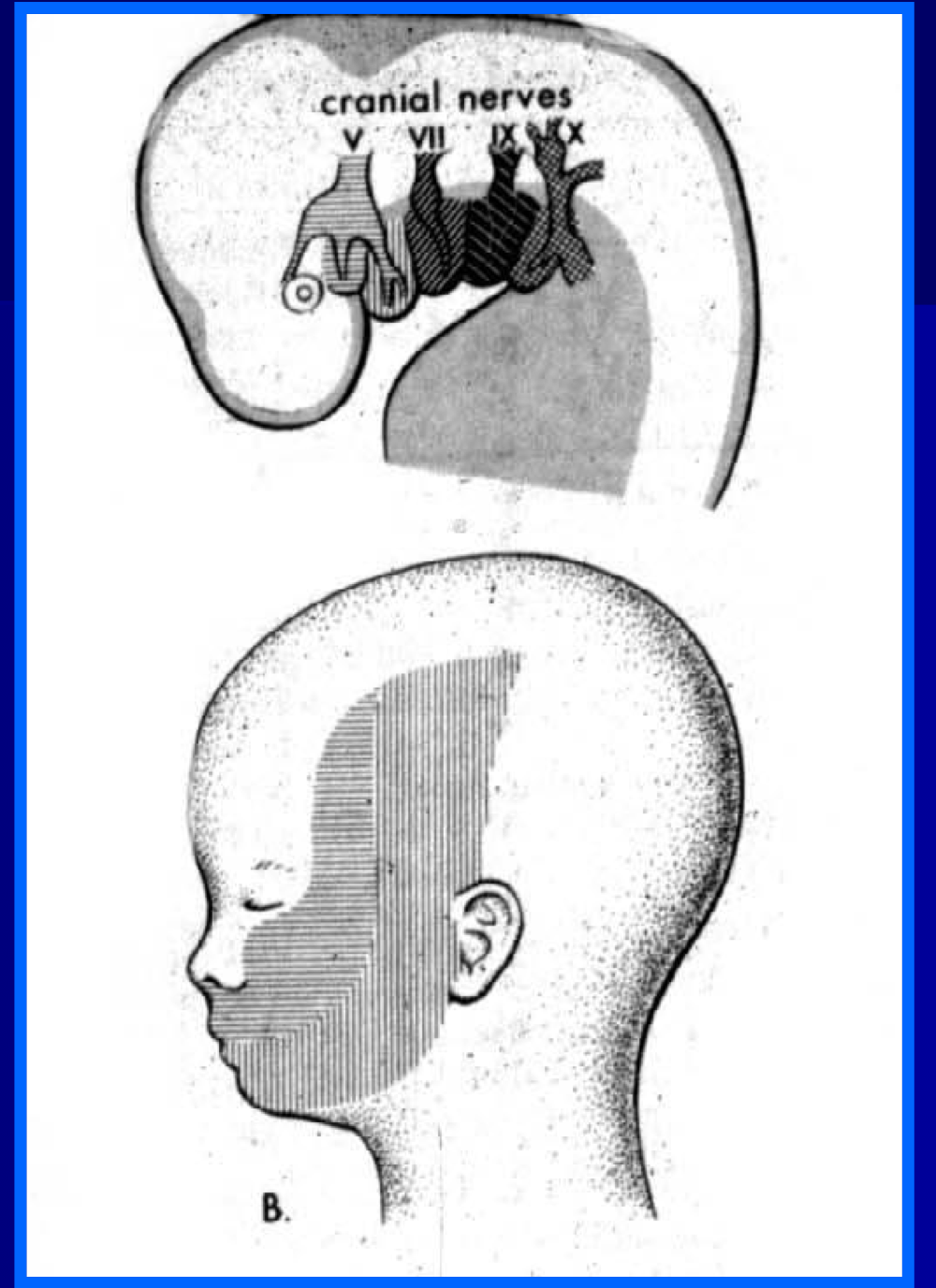
- [[V1 serves frontonasal process[[
- [[V2 serves maxillary process of Arch 1[[
- [[V3 serves mandibular process of Arch 1[[
- [[explains the sensory distribution of the three divisions (e.g. nose and forehead as grouping for ophthalmic division) and grouping of muscles of mastication all being innervated by third division of CN V[[
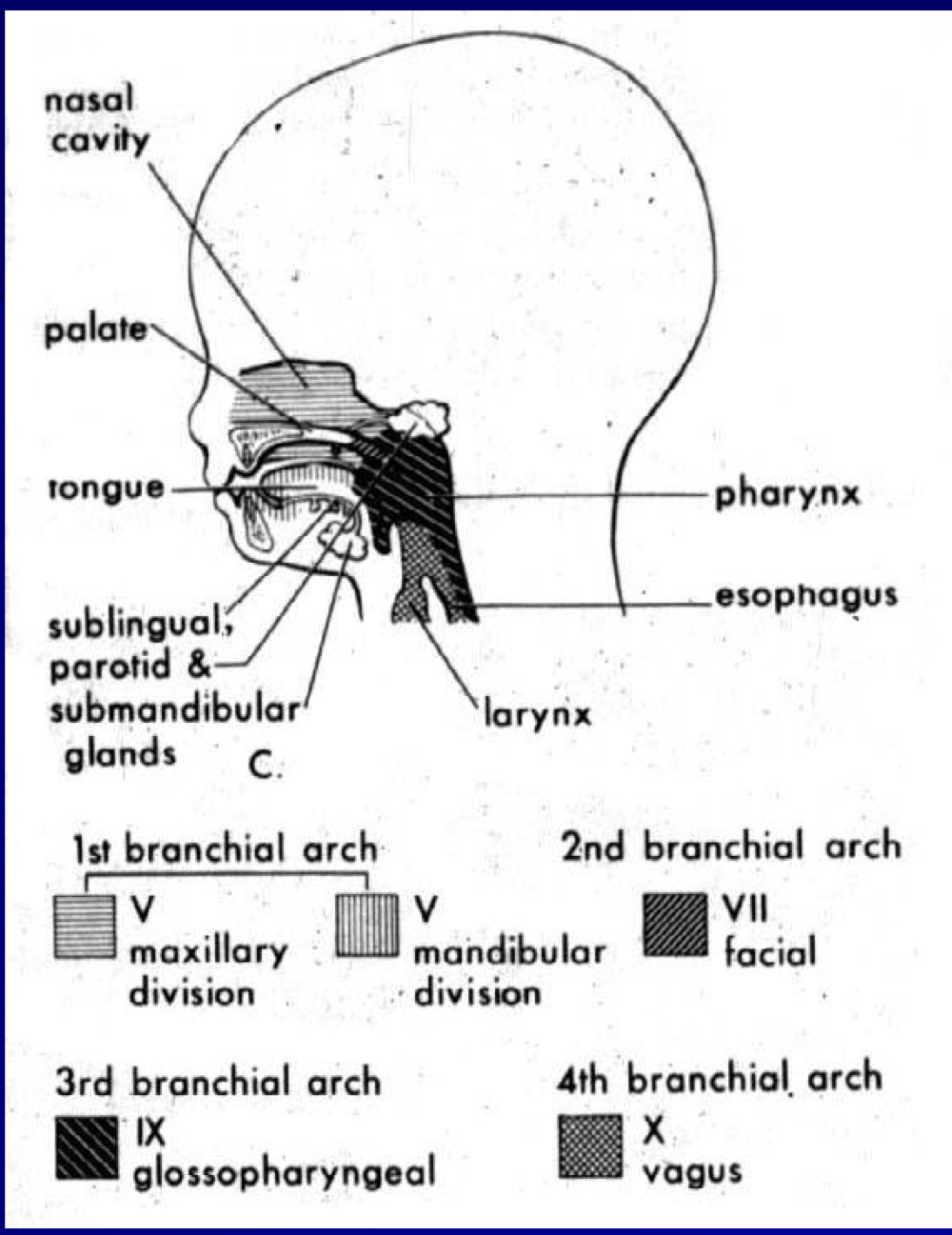
]]2nd arch - CN VII]]
- ]]Muscles of Arch 2 are muscles of facial expression]]
{{3rd arch - CN IX{{
- {{glossopharyngeal, pharynx, esophagus{{
}}4th-6th arch - CN X}}
- }}Recurrent laryngeal branch of CNX innervates}}
Each arch is lined on outside with surface ^^ectoderm^^, on inside with endoderm, which cover ==mesoderm== and some neural crest
The “pinch” between the arches is called a ^^branchial groove^^ on the outside and a pharyngeal pouch on the inside
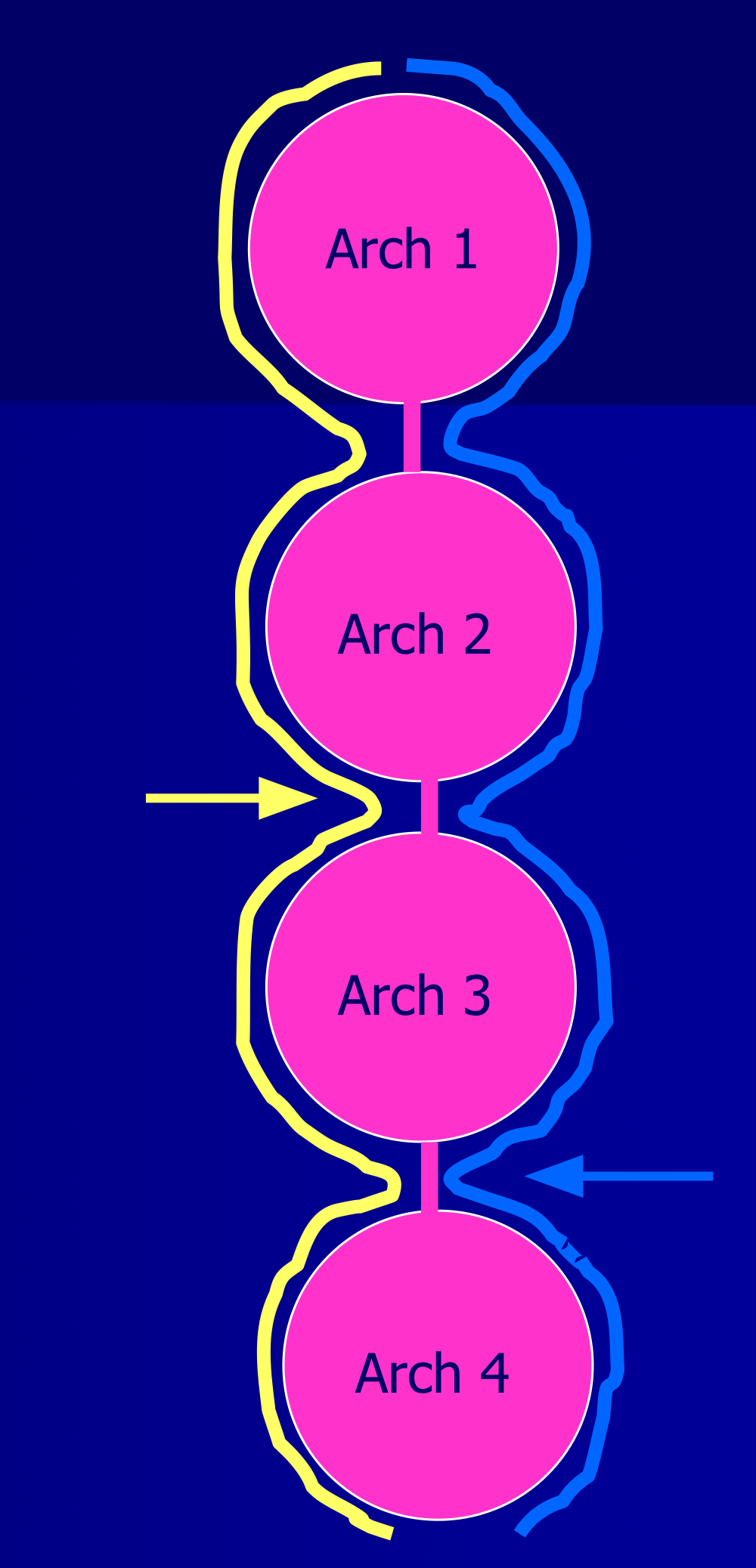
Branchial Grooves
Branchial Groove #1, positioned between arch 1 and arch 2, remains in adults as external auditory meatus, meeting first pouch and giving trilaminar tympanic membrane.
Remaining grooves covered by fusion of arch 3 and 4-6 producing temporary cervical sinus. Sinus ultimately resorbed, giving smooth contour to neck, instead of gill slits in fish
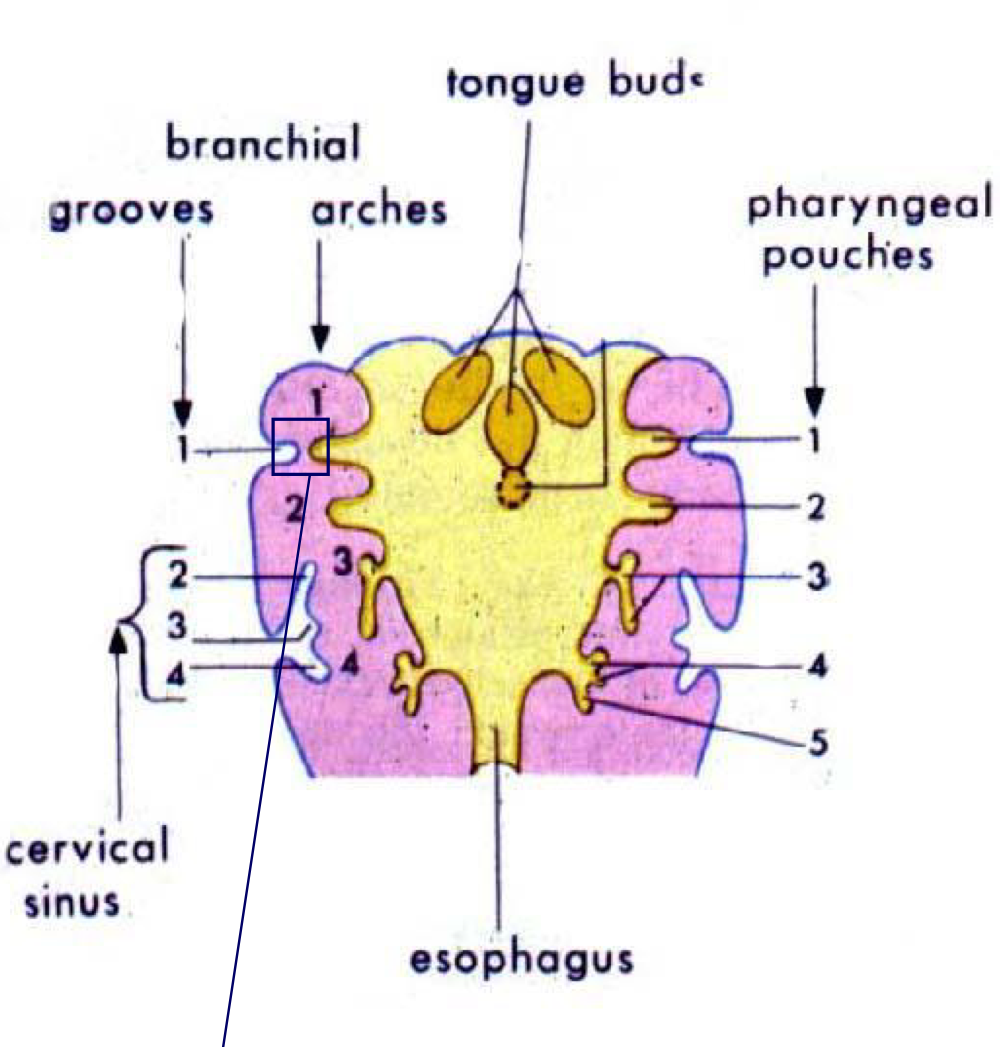
Pharyngeal Pouches
- [[1st pouch - pharyngotympanic (eustachian) tube from middle ear cavity to back of oropharynx[[
- ]]2nd pouch - ducts of palatine tonsils]]
- {{3rd pouch - lower parathyroids{{
- }}4th pouch - upper parathyroids}}
- <<5th-6th pouch - ultimobranchial bodies which give parafollicular cells of thyroid contributing to regulation of calcium<<
- descent leaves scar on back of tongue called foramen cecum
Development of Face and Nasolacrimal Duct
- Surface ectoderm buried in crease between frontonasal process and upper edge of maxillary process of arch 1
- hollows out an ectodermal-lined tube from medial canthus to nasal cavity → nasolacrimal duct
- Failure to fuse nasal elevations contribute to cleft lip and/or palate
- Pattern of development explains sensory fields of three divisions of CN V
- Dacryocystitis - inflammation of the lacrimal sac which typically occurs secondary to obstruction within the nasolacrimal duct and the resultant backup and stagnation of tears within the lacrimal sac
Hyaloid Remnants
- Bergmeister's Papilla - An atrophic partially elevated membrane is seen connected with the disc
- remnant of the embryological vascular system to the lens
Orbit
Sella Turcica
To enter the orbit, we have to start from the back door → where everything enters/leaves the orbit
straddle the sella turcica like two saddle bags, usually attached by 2 straps
ophthalmic vein → cavernous sinus
in sella turcica you can see the sphenoid behind it
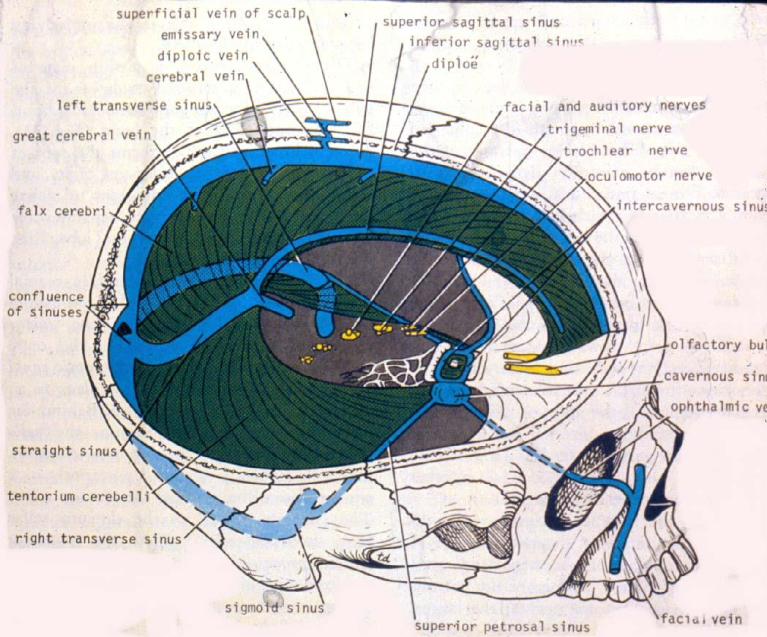
Cavernous Sinus
optic nerves are above the cavernous sinus
when the cavernous sinus are unhappy, there is no direct threat to the optic nerves, but everything else that had to enter the optic tract has to deal with the cavernous sinus
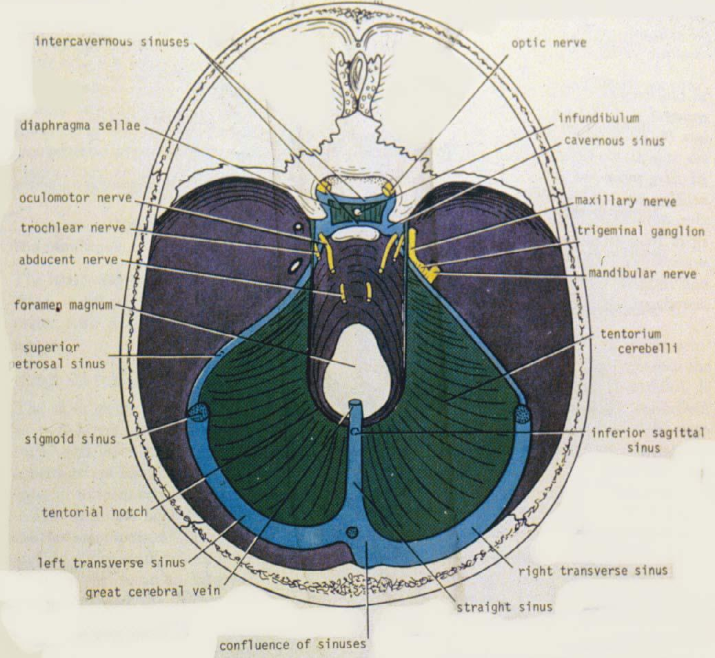
inner and outer walls of cavernous sinus are dura mater
things that pass with the cavernous sinus pass in order!
CN 6 pathway forward form the brain stem takes it past the crest, can be smacked on the petrous ridge, instead of going through the cavernous sinus, it passes through the blood space, goes with the internal carotid artery
keep in mind: carotid is high pressure hose, it is running through garbage bag that is filled with venous blood at low pressure → what if someone pokes howl in high pressure hose in low pressure bag? (bag will become that same pressure as the hose)
White box - roughly where the cavernous sinus would be
What passes through the cavernous sinus:
- 3, 4, V1, V2, 6
Carotid Canal
Sinus Fistula
bounced the back of his head, shattered his skull, carotid was going to move with the bone but couldn’t because it is trapped in the cavernous sinus
4 pictures show individual trying to look up, down, left, right
- right eye moves fine but the left eye doesn’t move
- lid is lagging as well, so there is a ptosis
- if you can’t move the eye at all, then 3, 4, and 6 are unhappy!
Will need to test V1 and V2 as well!
- V1 - can you feel forehead on right side? yes because it is intact. can you feel feel forehead on left side? no because that is where lesion is. what about corneas on both sides?
- V2 - can you feel right cheek? yes. can you feel left cheek?no, because of lesion. what about tip of nose on each side?
- V3 - can feel on both sides because it does not pass through the cavernous sinus
Arterial pressure from the ophthalmic artery is will strong enough to drive new blood into the orbit, but the venous blood cannot escape because the cavernous sinus has risen in pressure → venous stasis
**IOP could be 80mmHg, optic nerve cannot withstand this pressure for long → possible because not one drop of AH can leave the eye
Orbit - Anterior View
Doorways into and out of orbit
superior orbital fissure
optic canal - feature of sphenoid bone
inferior orbital fissure
what we bring things into the orbit, we divide them into 2 categories because there is a tendinous attachment of the rectus muscles
imagine the muscles extending from the back of the eye - we have created a conical structure called the muscle cone
anything that enters the orbit from the optic canal, also enter the muscle cone
- optic nerve
- ophthalmic artery
- nerve plexus around the artery
- brain has to remember that sympathetics are on board with the artery
superior orbital fissure - some contents go into muscle cone and some do not
skeletal muscles prefer to receive innervation and vascular supply from the inner protective surfaces
CN 3 - only serves ocular muscle so would rather receive it from inner protective surface, passes through the muscle cone to hit the muscles they must innervate
- superior division of CN 3, innervate all muscles in the orbit that have “superior rectus” and “superior levator palpebrae”
- inferior division - everything else that 3 would serve
- medial rectus, lateral rectus, interior rectus
CN 4 - has to serve superior oblique, but is running outside of the common tendinous ring, which means that the inner surface of CN 4 is outside of the muscle cone → will stay out of the muscle cone
CN 6 - inside the cone, happily jumps inside the cone
CN V1 - just as V1 is leaving the front wall of the cavernous sinus, it splits into 3 nerves:
frontal, highest anatomical part of the orbit cause headed for the forehead, does not enter muscle cone
lacrimal, runs along top edge of LR, but also outside of muscle cone
nasociliary (in muscle cone),has to get to the ciliary ganglion, which is in the muscle cone, ends up at the medial wall of the orbit eventually
CN V2 -
walk out of the superior orbital fissure, then we are walking into MCF
what if walk out __? then we end up in pterygopalatine fossa
inf. ophthalmic vein → inferior orbital fissure
CN III
leaves the brainstem in the midbrain, passes in relationship to the posterior communicating artery
enters the wall of the cavernous sinus, the uppermost structures, passes through the cavernous sinus then passes through the superior orbital fissure
once it leaves the cavernous sinus, the 3rd nerve splits into 2 branches: superior division & inferior division
Superior Division:
- superior rectus
- levator palpebrae superioris
Inferior division:
- medial rectus
- inferior rectus
- inferior oblique
parasympathetics are wrapped around the nerve
when CN 3 leaves the cavernous sinus, every bit of the parasympathetic fibers will go into the inferior division
parasympathetics of inferior division that go to inferior oblique is also attached to the ciliary ganglion
ophthalmic artery will go to the roof, lateral side and medial side of the orbit
for V2, entered the orbit from the PPF, gives some branches upwards but pretty much stayed on the floor
infraorbital artery (being a branch of the maxillary artery) goes thru PPF as well, but enters through the inferior orbital fissure
the ophthalmic artery enters the orbit as the first branch of the internal carotid artery, and that branch is given off the moment the internal carotid emerges from the roof of the cavernous sinus, it emerges so far forward that it is right in front of the optic canal. the ophthalmic artery passes under the optic nerve and enters the orbit through the optic canal (the third thing that enters the orbit is the sympathetic plexus) as the artery passes forward now in the orbit, it emerges from underneath the nerve and its intention is to come up and over the nerve heading for the medial side of the orbit (the main trunk of the vessel wants to head towards the medial side of the orbit), we cant neglect the lateral side so we give off the lacrimal artery
remember: think about where the lacrimal nerve went when it came from V1, where did it travel from? right along the lateral rectus → the artery does the same thing
on its way out, it throws a strange little branch, for a certain amount of distance along the lateral wall of the orbit, if you go through the outside of the lateral wall, you will be coming from the middle cranial fossa
when it punches through the MCF, it joins up with the middle meningeal artery!
- branch of the maxillary artery
- travels to the intertemporal fossa
- enters the skull through foramen spinosum
- exact vessel that creates dents on the inside surface of the skull
whats on the other side of the bone is orbit, through here where the little branch comes
common carotid artery came up and split into 2 little pipes
- internal carotid
- external carotid
where in the body are able to split, then come back together later on
vessel needs to be able to dilate, but it is running through a bony canal that is only a bit bigger than itself, only place this can happen is the scalp…?
central retinal artery, even in picture it is even shown as second, CRA branches at the nerve, 12 or 14 mm behind the eye. able to enter the nerve because of fetal fissure closed around it
sometimes 2 or 3 posterios ciliary arteries, one on medial side eand one on lateral side (3rd sometimes enters above
usually the lateral and medial PCAs will subdivide to make the LPCA on each side of the optic nerve, and 10-20 SPCA that reach the back of the eye and end up forming a ring around the nerve
going back to the lacrimal, it is going to serve the lacrimal gland
recall that the lacrimal nerve went out and gave us the lateral palpebral that serve sensation around the medial canthus
blood vessel land: that vessel is going to come out…?
supraorbital artery is going to follow V1, and is also going to the same place → contributes to the vasculature of the scalp, way at the end that you will not feel the pulse
if you have a patient that you suspect is having an internal carotid insufficiency, then patient will have increased blood flow to scalp and you will feel pulse in the supraorbital fissure
the nerve that we had that went medially was the nasociliary, and after it gave its branches to the ciliary ganglion, it was the one that then moved to the medial wall and it gave off the branches that went into the ethmoidal sinuses
the muscular branches serve the extraocular muscles which also means that of those vessels that serve the rectus muscle
nasociliary nerve that is running along the medial wall, and we have a nerve that is running along the medial wall as well
- each have a branch that go into posterior ethmoidal and anterior ethmoidal area
as we go forward than we will give rise to the medial palpebral arteries → lateral and medial will form arcades of the lids
when we get to the two terminal branches
- supratrochlear - will merge on the scalp, will serve the midline of the scalp, will anastomose in the middle of the forehead with the contralateral supratrochlear
- dorsal nasal - AKA frontal artery distribution of blood supple
infraorbital enters the inferior orbital fissure, runs on the floor and follows the path of V2, and makes some contribution of the inferior oblique ad inferior rectus muscle
Orbital Fascia
fascia in the orbit not only provide compartmentalization in the orbital space, but there is increasing evidence that the fascial connections between the rectus muscles and the orbital walls around them: play an integral role in ocular motility
kind of like stretchy rubber bands, add precision
bolded black represents fascia
each EOM is completely enveloped in fascia, (epimysium of the muscles) on the MR and LR, not only are the muscles covered in fascia, but they also extend out to the medial and lateral walls → extensions are called medial and lateral check ligaments!
on the bottom of the eye, the fascias that connect the SO and IO, where the IR and IO cross the fascia merge, they extend: both in terms of depth and width
create what is called the suspensory ligament → basically like a hammock
- job is to hold up the weight of the eye
- think about how complex it would be to move the eye of the superior muscles also had to suspend the eye, allow the eye to move as a weightless structure
Fascia of the LPS and SR are connected
- tissue come from common embryonic tissue
- can see the short sections that connect the LPS and SR from lateral view
- because of fascial connection if i drag the SR, then i am making the LRS contract more than it would have by itself
Aerial view
where the fascia is on the inside surface of the muscle…?
merger of tenon’s capsule and fascia of the muscle
merger of fascia of the muscle and the periorbita
periosteum of forehead is continuous with the periorbita of the frontal
behind orbital septum = in the orbit
all the space with white and nothing in it - filled with orbital fat, designed to flop into any void that it can
- as the orbital septum becomes old and lest elastic, the orbital fat will push it forward
- orbital fat is prolapsing forward
preseptal space in the lid, then behind the septum is what we defined as the orbit
Preseptal Cellulitis
infection of CT compartment of the lid
in scan you can see the bulge of the lid, but you can see the orbit is not involved, and this is because of the barrier that it provided by the orbital septum
- can be managed on an outpatient basis with medications
Orbital Cellulitis
infection BEHIND the orbital septum, imaging can confirm this
- infection happening in sinuses can chew through paper thin bone, through periorbita then hits the eye
- patient is septic, infection of bloodstream, then can occur anywhere
- immediate hospitalization with 4-5 IV antibiotics, because we are usually close to being on a life saving status right now
Horizontal Section through Eyes
if there was sphenoid sinusitis, and it chewed through the bone at “sun”, then it can wipe out the optic nerve
eye is so far out that you can see the optic nerve is stretched straight
Grave’s Orbitopathy
exophthalmus