Biology 30 Unit 2: Reproduction & Development
The Reproductive System
Male and female reproductive systems are characterized by distinct features
Gonads (testes vs. ovaries)
Sex hormones (testosterone vs. estrogen)
Gametes (sperm vs. eggs)
Primary sex characteristics (reproductive organs)
Secondary sex characteristics (features not directly related to reproduction)
Male Reproductive System
Key structures: ureter, large intestine, seminal vesicle, urinary bladder, ductus deferens, ejaculatory duct, urethra, prostate gland, Cowper's gland, glans penis, penis, epididymis, foreskin, testis, scrotum
Testes
composed of seminiferous tubules and interstitial cells
1. seminiferous tubules- produce sperm
2. interstitial cells- lie between the seminiferous tubules & secrete the male hormone, testosterone.
Sperm cells mature in the epididymis
Sperm develop from spermatogonia within seminiferous tubules
Sertoli cells provide metabolic support for developing sperm
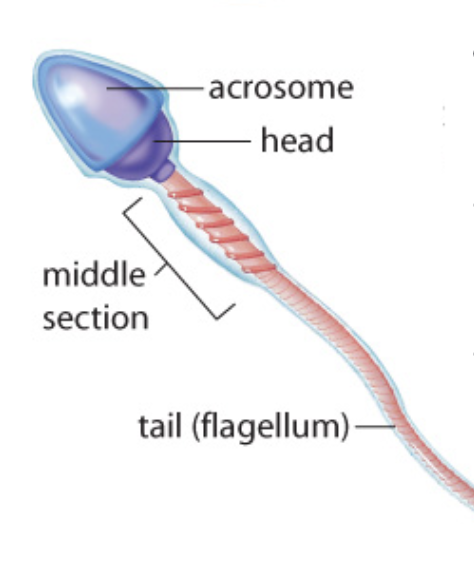
sperm
produced in large amounts
flagellum for propulsion
acrosome cap for penetration of the egg
During sexual arousal, the flow of blood increases to specialized erectile tissues in the penis. At the same time, veins that carry blood away become compressed causing erectile tissues to expand and as a result, the penis engorges with blood becoming erect. Sperm cells move out of each epididymis through the ducts deferens. As the sperm passes through the ducts deferens they are mixed with fluids for a series of glands.
Seminal vesicles
produce a mucus-like fluid that contains the sugar fructose
provides energy for sperm
prostate gland
secretes mucus-like fluids, as well as an alkaline fluid to neutralize acids found in the urine in the urethra
cowper’s gland
secretes mucus fluid and alkaline fluids
together the combination of sperm cells & fluids is called semen
if arousal continues, semen enters the urethra from the ducts’ deferens
sensory stimulation, arousal & coordination of muscular contractions combine to trigger the release, and ejaculation, of semen from the penis.
Male sex hormones (androgens)
At puberty, the hypothalamus produces GnRH.
GnRH stimulates the anterior pituitary to release FSH and LH.
FSH stimulates Sertoli cells in the seminiferous tubules to produce sperm.
LH stimulates interstitial cells in the testis to produce testosterone.
Testosterone levels increase during puberty, leading to the development of secondary sex characteristics- Facial hair, Body hair, Muscle development, Deeper voice, Narrow hips, Broad shoulders, etc…
Over time, most men experience a gradual decline in testosterone levels (a condition called andropause)
Hormone levels regulated through negative feedback
Steroids
like hGH, can disrupt reproductive hormone feedback systems.
Side effects in men include shrinking testicles, low sperm count, loss of body hair, and the development of breasts.
Female Reproductive System
Key structures: oviduct, ovary, ureter, fimbriae, uterus, urinary bladder, cervix, urethra, vagina, clitoris, labium minora, labium majora, vaginal orifice
Ovaries release a single mature egg (ovum) during ovulation
The endometrial lining of the uterus thickens in preparation for pregnancy
The ovum can survive in the oviduct for a period of 24 hours
Menstruation occurs if fertilization does not occur
Oogenesis occurs within follicle cells of the ovaries
follicle cells provide nutrients necessary for the ovum’s development
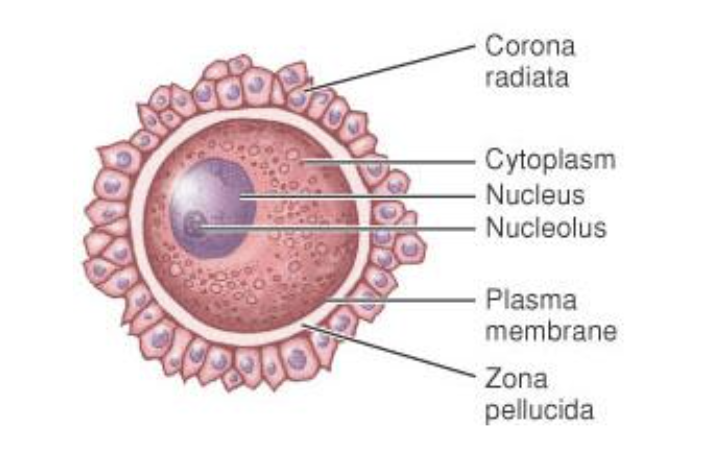
Mature ovum surrounded by corona radiata and zona pellucida
Once the ovum is released, surrounding follicle cells form the corpus luteum which secretes hormones essential for pregnancy.
A mature ovum
Females are born with a finite amount of oocytes; after a certain age, then, women no can longer ovulate (menopause)
Surrounded by two key layers:
the corona radiate which supplies vital proteins to the cell
a specialized coating called the zona pellucida which can only be penetrated by a single sperm
Non-motile
Secondary sex characteristics in females: minimal facial and body hair, breast development, higher voice, narrow shoulders, wider hips, less obvious muscle development
Sexually Transmitted Infections (STIs)
Caused by viruses, bacteria, or parasites
contracted through: unprotected sex, intravenous drug users sharing needles, children of mothers who are infected with HIV may be infected before or during birth or through breastfeeding
Impact on general health and reproductive ability
Examples of STIs:
HIV/AIDS- attacks a particular form of helper T cells in the immune system - as the level of helper T cells is low in the blood, an infected person becomes more vulnerable to infections
Hepatitis A - Transmission: Contact with infected blood, unprotected sex, and sharing needles. Symptoms: Fatigue, jaundice, abdominal pain, loss of appetite. Complications: Liver cirrhosis, liver cancer, liver failure. Prevention: Vaccination, practicing safe sex, avoiding sharing needles. Diagnosis: Blood tests for HBsAg, HBcAb, and HBV DNA. Treatment: Antiviral medications, supportive care, liver transplant.
HIV/AIDS- attacks a particular form of helper T cells in the immune system - as the level of helper T cells is low in the blood, an infected person becomes more vulnerable to infections
Hepatitis A - contracted through contact with infected blood, unprotected sex, and sharing needles. causes fatigue, jaundice, abdominal pain, and loss of appetite. Liver cirrhosis, liver cancer, liver failure. Prevention: Vaccination, practicing safe sex, avoiding sharing needles. Treatment: Antiviral medications, supportive care, liver transplant.
Hepatitis B- contracted through Blood, semen, vaginal fluids, and other body fluids. Causes Fatigue, jaundice, abdominal pain, and loss of appetite. Prevention: Vaccination, safe sex practices, avoiding sharing needles. Causes: Liver cirrhosis, liver cancer. Treatment: Antiviral medications, and supportive care.
Genital Herpes- Caused by herpes simplex virus (HSV), Transmitted through sexual contact. Primary symptoms: painful blisters, sores, itching. Can be asymptomatic or have mild symptoms. There is no cure, but antiviral medications can manage outbreaks and can increase the risk of HIV transmission. Practice safe sex to prevent transmission. Avoid sexual contact during outbreaks. can also cause genital herpes through oral-genital contact.
Syphilis- Caused by the bacterium Treponema pallidum. Transmitted through sexual contact or from mother to baby during pregnancy. rash, fever, swollen lymph nodes to severe complications affecting the heart, brain, and other organs. Can be diagnosed through blood tests. Treated with antibiotics, usually penicillin. Untreated syphilis can lead to serious health problems and even death. Prevention includes practicing safe sex and regular testing
Chlamydia- a sexually transmitted infection caused by the bacterium Chlamydia trachomatis. It is one of the most common STIs worldwide. Chlamydia can be asymptomatic, leading to delayed diagnosis and potential complications. Common symptoms include abnormal discharge, painful urination, and pelvic pain. Untreated chlamydia can cause serious complications like infertility and pelvic inflammatory disease. Chlamydia can be diagnosed through laboratory tests, including urine or swab samples. It is treated with antibiotics, and sexual partners should also be treated to prevent reinfection. Prevention includes practicing safe sex, using condoms, and getting regular STI screenings.
Gonorrhea- Caused by Neisseria gonorrhoeae bacteria. Transmitted through sexual contact. Symptoms include painful urination, discharge, and pelvic pain. Can lead to serious complications if left untreated. Diagnosed through laboratory tests on urine or swab samples. Treated with antibiotics, but drug-resistant strains are emerging. Prevention through safe sex practices and regular testing. Untreated gonorrhea can increase the risk of HIV transmission. Screening is recommended for sexually active individuals. Partner notification and treatment are crucial to prevent reinfection
Human Papilloma Virus (HPV)- transmitted by skin-to-skin contact, develops flat or raised warts around the genital area, some forms can lead to cervical cancer, raised risk of tumours of the vulva, vagina, anus, and penis
Hormonal Regulation of the Reproductive System
Sex Determination
Chromosomal (genetic) sex determined at fertilization
Anatomic sex determined around the seventh week of development
Testosterone secretion encoded by genes on the Y chromosome leads to male differentiation
Absence of testosterone production results in female development
Possibility of Genetic and Anatomic Sex Mismatch
It is possible for a person to be genetically male but anatomically female, and vice versa.
Female Sex Hormones
Puberty begins when the hypothalamus triggers the release of LH and FSH from the pituitary.
FSH stimulates the development of female sex organs and follicle development within the ovaries.
As the follicle develops, it releases estrogen.
LH triggers ovulation, signalling egg maturation.
Hormones associated with puberty stimulate the development of secondary sex characteristics.
The Menstrual Cycle
The menstrual cycle is divided into four phases: the flow phase, the follicular phase, the ovulatory phase, and the luteal phase.
The flow phase -(days 0-7) is characterized by the shedding of the endometrium and low hormone levels.
The follicular phase - (days 7-14) is stimulated by GnRH, which causes follicle maturation and the secretion of estrogen.
Rising levels of estrogen inhibit the release of FSH.
The ovulatory phase - (day 14) is marked by a sharp increase in LH production, triggering the release of the mature ovum from the follicle.
The luteal phase - (days 14-28) is when the corpus luteum(structure holding the ovum) forms and secretes estrogen and progesterone.
Birth Control Pills
Birth control pills prevent pregnancy by regulating hormone levels.
They contain synthetic hormones that mimic the effects of estrogen and progesterone.
These hormones prevent ovulation and thicken the cervical mucus, making it difficult for sperm to reach the egg.
Menopause
Menopause is the stage when women stop producing eggs and hormone levels decline.
Symptoms of menopause include hot flashes, high cholesterol, diminished bone mass, and changes in mood.
Fertilization and Development
Fertilization
the joining of male and female gametes (sperm and egg) to form a zygote.
occurs within the oviduct.
The egg has unique coating layers (corona radiata and zona pellucida) that ensure only one sperm can successfully attach.
Sperm cells release enzymes to digest the outer coating of the egg.
Once a sperm enters the egg, the egg's plasma membrane depolarizes, preventing other sperm from entering.
The nuclei of the sperm and egg (23 each) fuse, forming a zygote with 46 chromosomes. (meiosis)
Stages
Embryonic period development- first 8 weeks - cells divide & become redistributed - tissues form as do structures that support & nourish the developing embryo
Fetal Period of development - about 9th week - baby grows rapidly & organs begin to function & coordinate to form organ systems
Cleavage and Implantation
After fertilization, the zygote undergoes several cell divisions through cleavage.
Cleavage is rapid cell division without enlargement.
Over 3-5 days, cleavage forms a sphere of 16 cells called the morula.
The morula develops into the blastocyst, consisting of the trophoblast and inner cell mass.
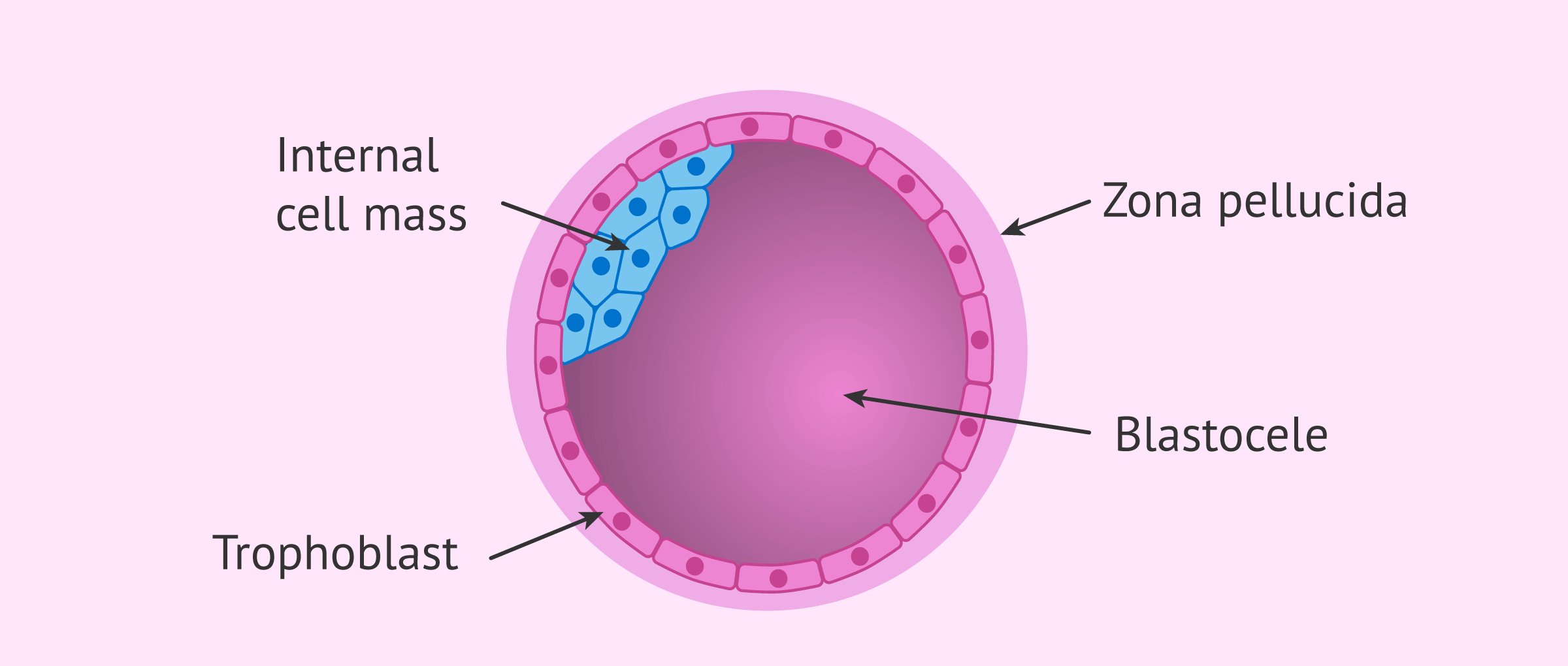
The blastocyst attaches to the endometrium of the uterus through implantation.
Implantation is complete by days 10-14, indicating pregnancy.
Post-Implantation
After implantation, the trophoblast secretes human chorionic gonadotropin (hCG).
hCG maintains the corpus luteum, which continues secreting estrogen and progesterone.
This maintains the endometrium and prevents menstruation.
hCG levels decline after the second month of pregnancy when the placenta takes over hormone secretion.
Gastrulation and Organ Formation
During week 2, the blastocyst undergoes gastrulation.
The amniotic cavity forms between the inner cell mass and the trophoblast.
The inner cell mass flattens into three layers: ectoderm, endoderm, and mesoderm.
Each layer differentiates into specific tissues and organs.
Organ formation occurs between weeks 3 and 8, with the development of the notochord, primitive heart, lungs, kidneys, limbs, brain, and external genitalia.
Week 3 = Formation of the notochord (will develop into brain and spinal cord through a process called neurulation*), the primitive heart starts beating
Week 4 = Formation of blood cells. Lungs and kidneys take shape, and small buds (which will develop into arms and legs) appear. A distinct head is visible.
Week 5 = Eyes open, cells of the brain undergo rapid differentiation.
Week 6 = Continued development of the brain, and lengthening of limbs.
Week 7 = Organs and skeletons almost completely formed, and external genitalia begin to differentiate. The nervous system begins to coordinate body activity
Week 8 = Embryo is the size of a paperclip. 90% of organs are established.
Neurulation and Spina Bifida
Neurulation is the folding of germ layers to form the notochord, which develops into the brain and spinal cord.
Folic acid must be present for proper notochord formation.
Inadequate folic acid during pregnancy can lead to spina bifida.
Structures Supporting the Embryo
The allantois, placenta, amnion, yolk sac, and chorion are supportive structures during embryonic development.
The placenta attaches the fetus to the uterine wall and facilitates metabolic exchange.
The amnion encloses the fluid-filled sac that protects the embryo.
The chorion forms the fetal portion of the placenta.
Functions of the Placenta
The placenta has several functions, including nutritional, excretory, respiratory, endocrine, and immune functions.
It transports nutrients from the mother to the fetus and stores nutrients.
It transports wastes from fetal blood to the mother's blood.
It transports oxygen from the mother to the fetus and carbon dioxide from the fetus to the mother.
It secretes hormones and allows hormones to diffuse between the fetus and mother.
It transports antibodies from the mother to the fetus.
The placenta does not filter out harmful substances like drugs and alcohol.
These substances can pass through the placenta to the fetus's blood.
This can have severe consequences, such as Fetal Alcohol Spectrum Disorder (FASD).
Substances that can harm the fetus are referred to as teratogens.
Fetal development
first trimester (weeks 1-12).
Fetal development is divided into the embryonic period (weeks 1-8) and the fetal period (weeks 9-12).
During this time, the body continues to grow and the skeleton begins to harden.
External reproductive organs become distinguishable.
second trimester (weeks 13-24)
The heartbeat becomes strong enough to hear with a stethoscope.
Rapid brain growth occurs, and the nervous system begins to function.
The mother begins to feel movement.
The fetus would not likely survive if born at this stage.
third trimester (weeks 25-38)
Rapid brain development and organ maturation take place.
The fetus nearly doubles in size.
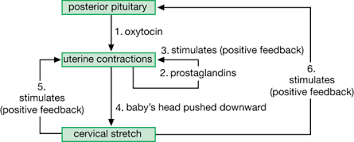
Parturition
the delivery of the baby- is regulated by positive feedback mechanisms.
Contractions continue until birth occurs.
Prostaglandins, a group of hormones, aid in contractions.
Prostaglandins act on the same tissue they are produced by.
Hormonal control of lactation
During pregnancy, high levels of estrogen and progesterone suppress milk production.
After birth, prolactin is secreted by the pituitary gland, stimulating milk production.
The release of milk from the breasts (lactation) is mediated by oxytocin.
Oxytocin causes contractions within the mammary lobules.
Suckling motions send signals to the hypothalamus, which stimulates the pituitary to release oxytocin.
The sound of an infant crying can also stimulate the production of oxytocin in some women.
Reproduction Technology
fertile- able to conceive/ host an offspring
sterile- unable to create offspring (infertile)
male
obstruction in the ductus deferens potentially caused by STIs
low sperm count or abnormal/non-viable sperm ( overrated testes, smoking, alcohol, exposure to toxins/chemicals, steroids,)
inability to achieve erection/ejaculation (vascular disease, nervous system injuries, age, stress, hormone imbalance, medication)
female
Blocked oviducts
failure to ovulate due to hormonal imbalance
endometriosis
damaged eggs
caused by smoking, alcohol, exposure to toxins/chemicals, steroids, vascular disease, nervous system injuries, age, stress, hormone imbalance, medication…
Technologies to help:
Artificial insemination - a reproductive technique used in humans and animals. It involves introducing sperm into the female reproductive tract without sexual intercourse. AI can use fresh, chilled, or frozen sperm and techniques like IUI or IVF. It helps with male infertility, genetic disorders, and animal breeding programs, improving the chances of successful reproduction.
In vitro fertilization(IVF) - a medical procedure where an egg is fertilized by sperm outside the body, typically in a laboratory setting. The resulting embryo is then transferred to the uterus for implantation, with the goal of achieving pregnancy. IVF is commonly used to assist couples with fertility issues or individuals who may not be able to conceive naturally.
Surrogate Mother - a woman who carries and gives birth to a baby on behalf of another person or couple, typically because they are unable to conceive or carry a pregnancy themselves.
superovulation - a process in which a woman's ovaries are stimulated to produce multiple eggs during a single menstrual cycle. This is typically achieved through the administration of fertility drugs, such as follicle-stimulating hormone (FSH). Superovulation is commonly used in assisted reproductive technologies, such as in vitro fertilization (IVF), to increase the chances of successful fertilization and pregnancy.
Technologies to prevent
Tubolization or vasectomy (oviducts/ ductus deferens cut or tied off)
hormone treatments (pills, injections…)
physical barriers (condoms, diaphragm…)
rhythmic method (timing along with your cycle)
.