CH 17 -The Reproductive System A&P
Chapter 17: The Reproductive System
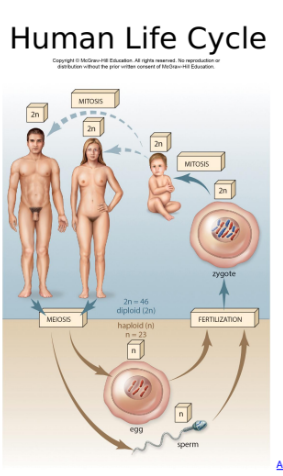
17.1 Human Life Cycle
Introduction to Human Life Cycle
Puberty: Sequence of events leading to sexual maturity.
Onset for females: ages 11-13.
Onset for males: ages 14-16.
Reproductive system functionality peaks at the end of puberty.
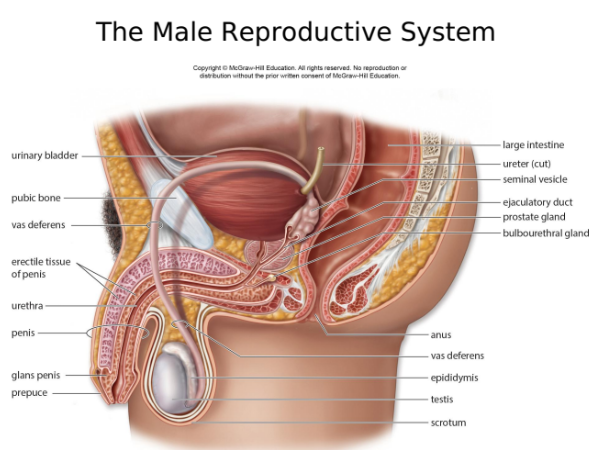
17.2 Male Reproductive System
Functions of the Reproductive Organs
Gamete (sperm) production and transport.
Key Organs:
Testes: Produce sperm and male hormones, located in the scrotum.
Accessory Ducts:
Epididymis, vas deferens, ejaculatory duct, urethra.
Accessory Glands:
Seminal vesicles, prostate gland, bulbourethral glands (Cowper's glands).
Seminal fluid supports sperm during ejaculation.
Male Internal Accessory Organs
Epididymides
Tightly coiled thread-like tube
• Lining consists of ciliated pseudostratified columnar epithelium
• Stores and supports sperm
• Peristaltic contractions move sperm alongas they mature
• Once sperm leave the epididymis, they areable to fertilize the egg even though theydon’t “swim” until they enter the vagina
Vas deferens
• Continuation of the epididymis
• Lined by pseudostratified columnar epithelium (partly ciliated)
• Contained within the spermatic cord: vas deferens, connective tissue, muscle , testicular artery, testicular vein, nerve
Vas deferens, cont.
• Spermatic cord enters the abdominal cavity via the inguinal canal and widens at the ampulla, located at the posterior base of the urinary bladder
• The testes descend through the inguinal canal into the scrotum in the fetus
• The canal remains weak and can be the site of an inguinal hernia
Joins with the duct of a seminal vesicle to form an ejaculatory duct
• The ejaculatory duct passes through the prostate gland to join the urethra
Seminal Vesicles
• Lateral to each vas deferens on the posterior bladder wall
•Secrete an alkaline fluid that contains fructose (energy for sperm) and prostaglandins (promotes muscular contractions in the female reproductive tract)
Prostate
• Encircles the urethra
Secretes an alkaline fluid that helps adjust the pH of seminal fluid and enhances the motility of sperm
Bulbourethral Glands (Cowper glands)
• Inferior to prostate gland
• Secrete a mucus-like fluid that lubricates the end of the penis
• Neutralizes acidic urine in the urethra
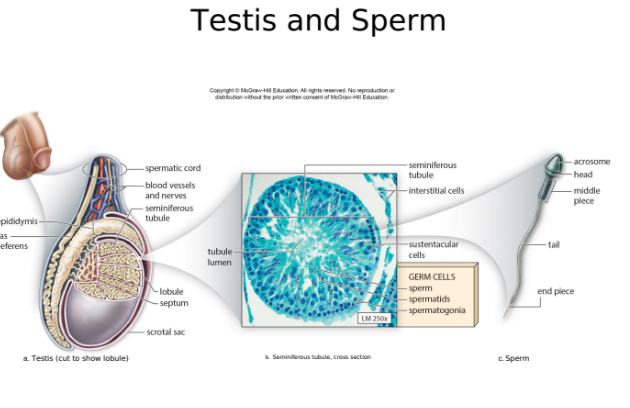
The Testes:
Produce sperm and the male sex hormonesLocated outside of the abdominal cavitywithin the scrotum – sperm require a lowertemperature to form
Testes develop in the abdominal cavity anddescend into the scrotum about twomonths before birth
Cryptorchidism – when the testes failto descend; causes infertility
Anatomy of a Testis
Enclosed by a fibrous capsule that extends to form the septa, which divides testis into lobules
Each lobule contains one to three seminiferous tubules
Seminiferous tubules contain cells that produce sperm
Interstitial (Leydig) cells produce androgens (testosterone)
The Testes:
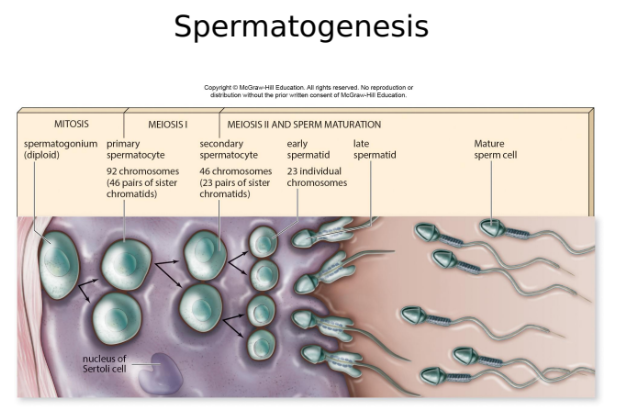
Spermatogenesis, cont.
• Two types of cells in the seminiferous tubules: germ cells and sustentacular cells
• Germ cells – involved in spermatogenesis
• Spermatogonia – divide by mitosis toproduce more cells
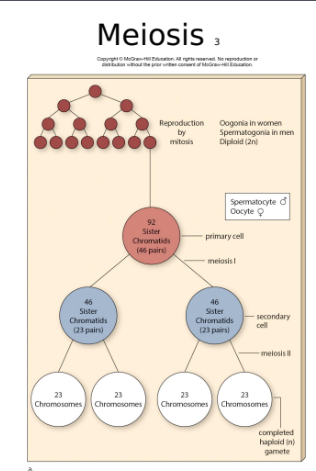
•Primary spermatocytes – contain 92chromatids (diploid – 46 pairs); startmeiosis
Germ cells, cont.•
Secondary spermatocytes – the result of meiosis I
• Contain 46 chromatids (23 pairs)
• Spermatids – the result of meiosis II• Haploid
Two types of cells in the seminiferous tubules, cont.
• Sustentacular (Sertoli) cells –support, nourish, and regulate the development of cells undergoing spermatogenesis
The Testes:
Spermatogenesis, cont.
• Spermatids mature into spermatozoa (sperm) and are transported to the epididymis
• Sperm have three distinct parts:
• Head – contains a nucleus covered by the acrosome
• Middle piece – contains mitochondria
• Tail – provides motility• Sperm typically survive for about 48 hoursin the female reproductive tract
Spermatogenesis:
Process of sperm production in the testes:
Involves meiosis for gamete formation.
Two types of cells involved: Germ cells and sustentacular cells.
Spermatogonia undergo mitosis to generate primary spermatocytes (diploid).
Meiosis I results in secondary spermatocytes (haploid).
Meiosis II produces spermatids, which mature into spermatozoa.
17.3 Female Reproductive System
Functions of the Female Reproductive Organs
Primary Sex Organs: Ovaries produce ova and female hormones.
Accessory Organs: Uterine tubes (transport ova), uterus (embryo development), vagina (birth canal).
Vulva (external genitals): Mons pubis, clitoris, labia majora, labia minora.
Oogenesis:
Process of ovum production, involving meiosis.
Primary follicle develops through secondary follicle to mature (Graafian) follicle, releasing a secondary oocyte during ovulation.
If fertilization occurs, meiosis II is completed.
Meiosis
Reduction divison- chromosome number is reduced from 46 (2n diploid to 23 (n, haploid) - Takes place in the tests of male and the ovaries of female
Meiosis I: Chromosme number cut it
Meiosis II: Regular mitosis
Fertilization results in a zygote, which isdiploid – a combination of the egg’s DNA andthe sperm’s DNAMeiosis ensures that fertilization resultsin a diploid cell
The zygote divides by mitosis• Growth of fetus, child, and adult is bymitosis
Meiosis
Each division has the same stages as mitosis:
Prophase
Metaphase
Anaphase
Telophase
Meiosis
Differences between mitosis and meiosis• Mitosis has one cell division, meiosis has two (so meiosis produces four daughter cells)• Mitosis daughter cells are identical to the parent cell; meiosis daughter cells are haploid and genetically different from the parent cell
17.4 Control of Reproduction and STIs
Contraception Methods:
Prescription hormonal methods (pills, injections, etc.).
IUDs, diaphragms, and condoms.
Surgical methods (vasectomy, tubal ligation).
Sexually Transmitted Infections (STIs):
Various organisms cause STIs; prevention methods include condom usage.
Some STIs can cause severe health implications (e.g., HPV leading to cancer).
17.5 Effects of Aging
Hormone levels decline with age, affecting reproductive systems.
Menopause typically occurs ages 45-55 in females.
In men, testosterone production declines gradually which may lead to issues like prostate enlargement.
17.6 Homeostasis
Estrogen:
Promotes fat deposition, protein synthesis, and bone health.
Androgens:
Impact muscle structure and enzyme activity in various organs.
The chapter illustrates the complex interplay between reproductive health, hormonal regulation, and aging, emphasizing knowledge critical for maintaining long-term health and understanding human development.
 Knowt
Knowt