phlebotomy chapter 4 notes
Routine equipment includes evacuated tube holders, needles, different-sized syringes, winged collection sets, collection tubes tourniquets, antiseptic skin preparation solutions (povidone-iodine swabs, chlorhexidine swabs, 70% alcohol swabs), gloves, gauze pads, slides, markers and pencil, transfer devices and a sharps disposal container. An alcohol-based hand gel should also be carried or made readily accessible. The phlebotomist is often called to collect blood from a patient's ward. A phlebotomy tray is designed to carry all the needed equipment. It should be refilled and sanitized at least once a week. This prevents errors and inconveniences when collecting blood.
Evacuated Tube System: This is the most common method of venipuncture utilizing an evacuated tube or ETS. It has a double-pointed (multisample) needle. The unsheathed end punctures the vein, while another end (sheathed in a holder) punctures a collection tube. This system relies on a predetermined vacuum that automatically fills each evacuated tube. This eliminates manual specimen transfer, thereby decreasing the risk of exposure to biological hazards. It also ensures the correct blood-to-additive ratio to avoid incorrect test results.
Needles: Needles may be multisample, hypodermic or part of a winged set. They are usually described by gauge and length. Needles are packaged individually and come with a sterile shield and color-coded hub for easy identification. The phlebotomist chooses the right needle for venipuncture to ensure patient comfort while minimizing the risk of complications. A needle gauge indicates the size of its diameter. It can range from 16 to 25. A lower number indicates a thicker needle. A 21-gauge needle is thinner than a 16-gauge needle. A 21-gauge is the standard size of needle for most adults. Larger gauges are used for children and adults with smaller veins.
A 25-gauge needle is avoided for venipuncture. The narrow diameter can cause hemolysis. This may cause potassium and magnesium to leak out of the cells and falsely increase serum determinations. It also causes a false decrease in red cell count, hematocrit and APTT values.
The 20-gauge needle is also avoided. Patients on blood thinners may experience bleeding and hematomas after the procedure from the larger injury on the vein. The length of the hypodermic needles is usually an inch to an inch and a half, while winged collection needles are 0.5 to 0.75 inches. The structure of a needle varies when it is hypodermic, multisample or part of a winged collection set. All needles have a hub, shaft, bevel and point. It is important to look at your needle before you use it. Look for defects, like an absent bevel or breaks. If a needle is defective, discard it in the sharps container. Never recap a needle, used or unused.
Needle Holder: Double-pointed needles are attached to a needle holder. This is a clear, firm plastic and may come with a safety device. They are available in various types to fit collection tubes of varying sizes. These must fit securely. The ETS mainly uses this system. As one point of the needle inserts into the vein, blood is vacuumed through the other point into the evacuated tubes. This vacuum is created by puncturing the rubber stopper of the collecting tube with a rubber-sheathed needle. Each evacuated tube comes with a predetermined vacuum. When the tubes have filled, slightly twist them to remove them. When collecting multiple tubes, secure the needle first by firmly grasping the holder through its flanges. This holds the needle in the vein and avoids puncturing it.
Needle Safety Features: The Needlestick Prevention and Safety Act mandates that every needle has a safety feature. This may be a device that blunts, shields or retracts the needle after use. After performing venipuncture, you should activate the safety device.
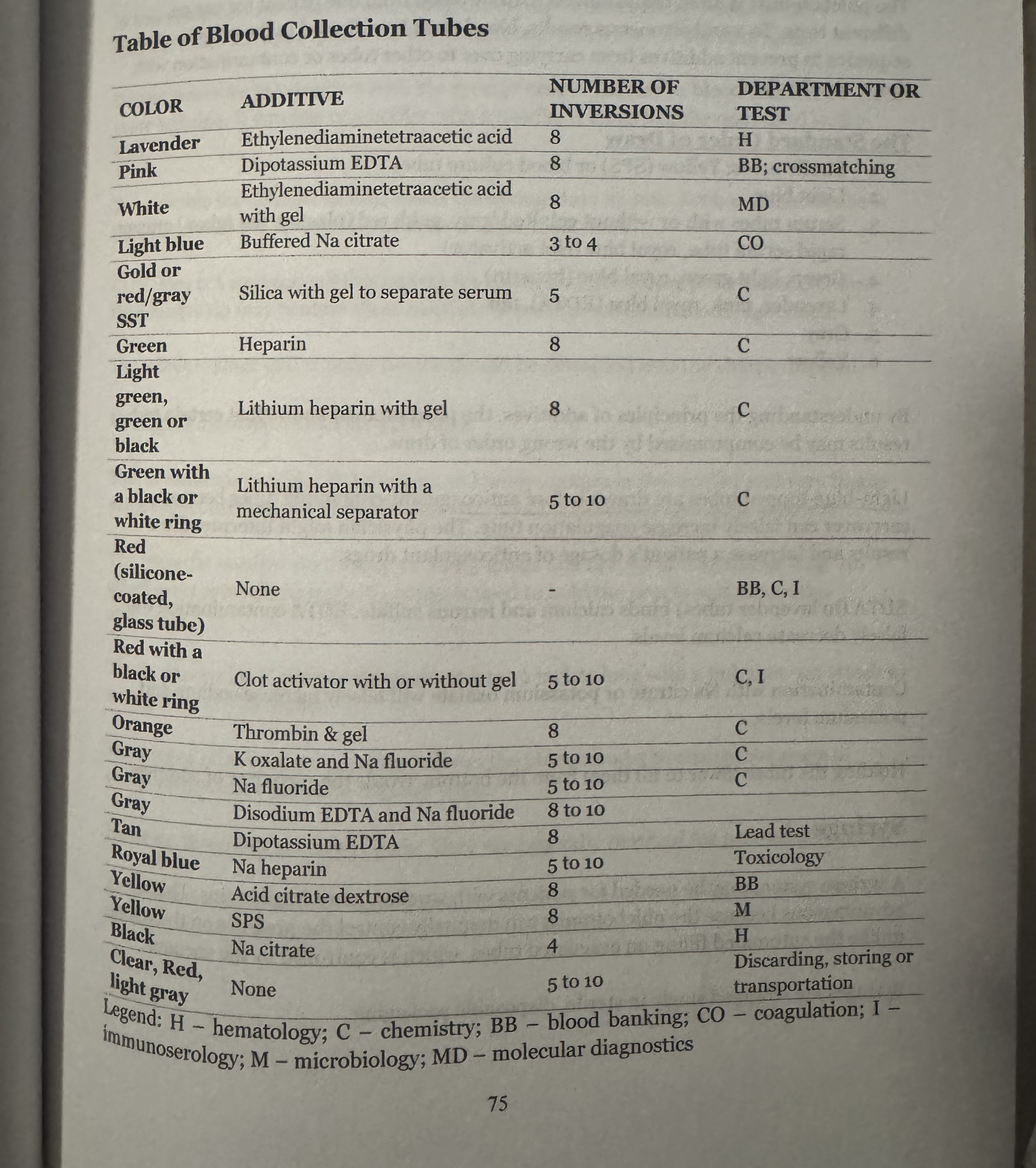
Blood Collection Tubes: Blood collection tubes or evacuated tubes are specialized containers used to collect and transport blood samples. There are varying sizes that can collect from 1.8 up to 15 militers of blood. Each tube is sterile and designed for specific purposes. It may or may not contain an additive. It may be made of glass or plastic. Glass tubes are generally avoided since these may break and increase the risk of BBP exposure. The phlebotomist selects the appropriate tube based on the patient's age and veins, the tests being ordered and the amount of blood required. Tubes have a thick rubber stopper, which is thinner in the center for puncturing. It comes with a color-coded shield to prevent splatters. The colors vary by the type of additives coated in the tube. The colors are generally universal, with slight variations per manufacturer. Removal of tube stoppers should be avoided. They cause aerosols and may spread BBPs. When necessary, open the tube by covering the stopper with a gauze pad and loosening it slowly, directed away from you. Evacuated tubes in the ETS fill automatically to a predetermined level. Tubes that fill partially usually have a white ring on the cap. Each tube is labeled with its additives, volume and expiration date. Tubes that have already lost their vacuum may cause a failed collection.
Factors that can cause a tube to lose its vacuum are: • Manufacturer error • Expired tubes • Dropped tubes • Opened or punctured tubes • Improperly stored tubes • Improper venipuncture technique (i.e., the tube is advanced too soon; the bevel. is dislodged accidentally)
Blood Collection Tube Additives: A test may require either whole blood or only serum or plasma. Some test determinants may need certain chemicals to act as stabilizers, preservatives or anticoagulants. Tubes contain these chemicals, which are called additives. Anticoagulants may be required for tests using whole blood to prevent coagulation, which interferes with the reading of the results. These chemicals prevent the formation of a blood clot by binding calcium (ethylenediaminetetraacetic acid) or inhibiting thrombin (heparin). These tubes must be inverted an appropriate number of times to properly mix and prevent microclots. Do not shake. Shaking may cause hemolysis. The formation of air bubbles through the tube while inverting ensures adequate mixing. Some tubes use a powdered form of anticoagulants. When using these, tap the tube gently to loosen the particles and ensure proper mixing. Do not transfer blood from an additive-containing tube into another tube with other additives. This produces contamination and incorrect test results. A color-coding system helps identify which tubes to use for a test. This helps to easily identify which specimens should go in a particular tube. This is generally universal, although different manufacturers may utilize slightly different colors.