Deep Vein Thrombosis and Pulmonary Embolism
thrombus is activation of clotting cascade intravascularly, can happen in artery and in vein
different from blood clot/haematoma
thrombus made up of fibrin, platelets and RBCs
coagulation cascade - intrinsic pathway, internal damage to endothelium, seen more frequently in arterial thrombosis
extrinsic pathway more trauma like putting something into
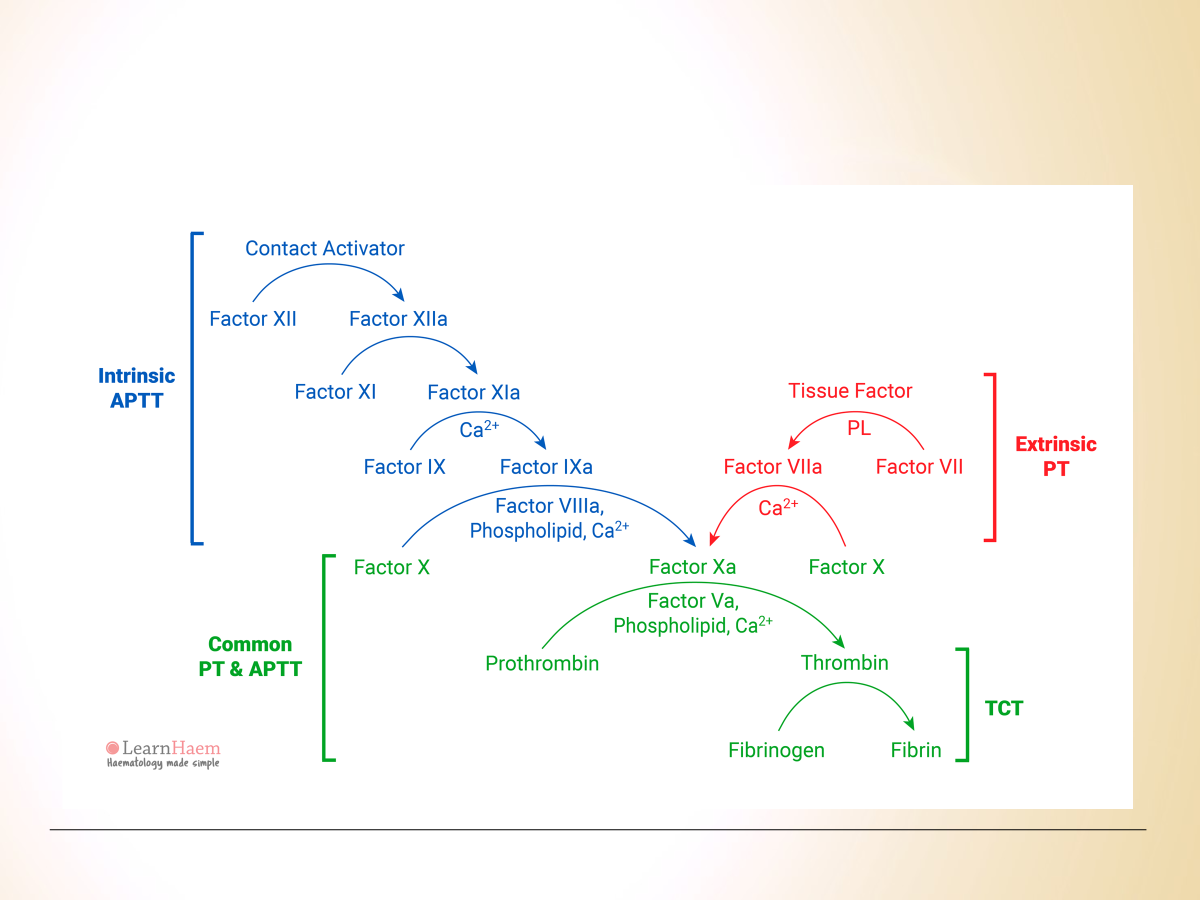
Intrinsic- Exposure of collagen etc
Extrinsic- release of TF from the adventitia of the the BV
apixaban, rivoroxaban
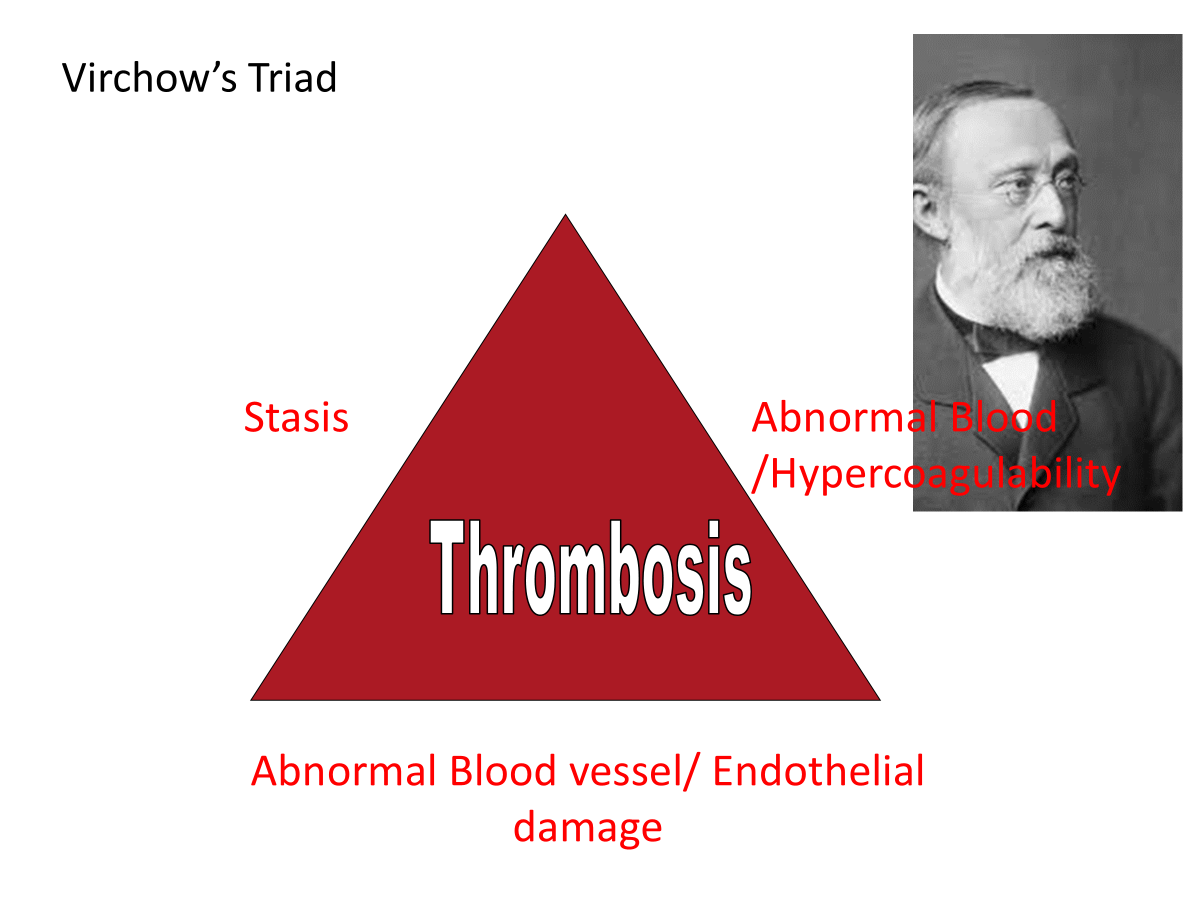
hypercoagulability - sepsis making thrombosis more likely
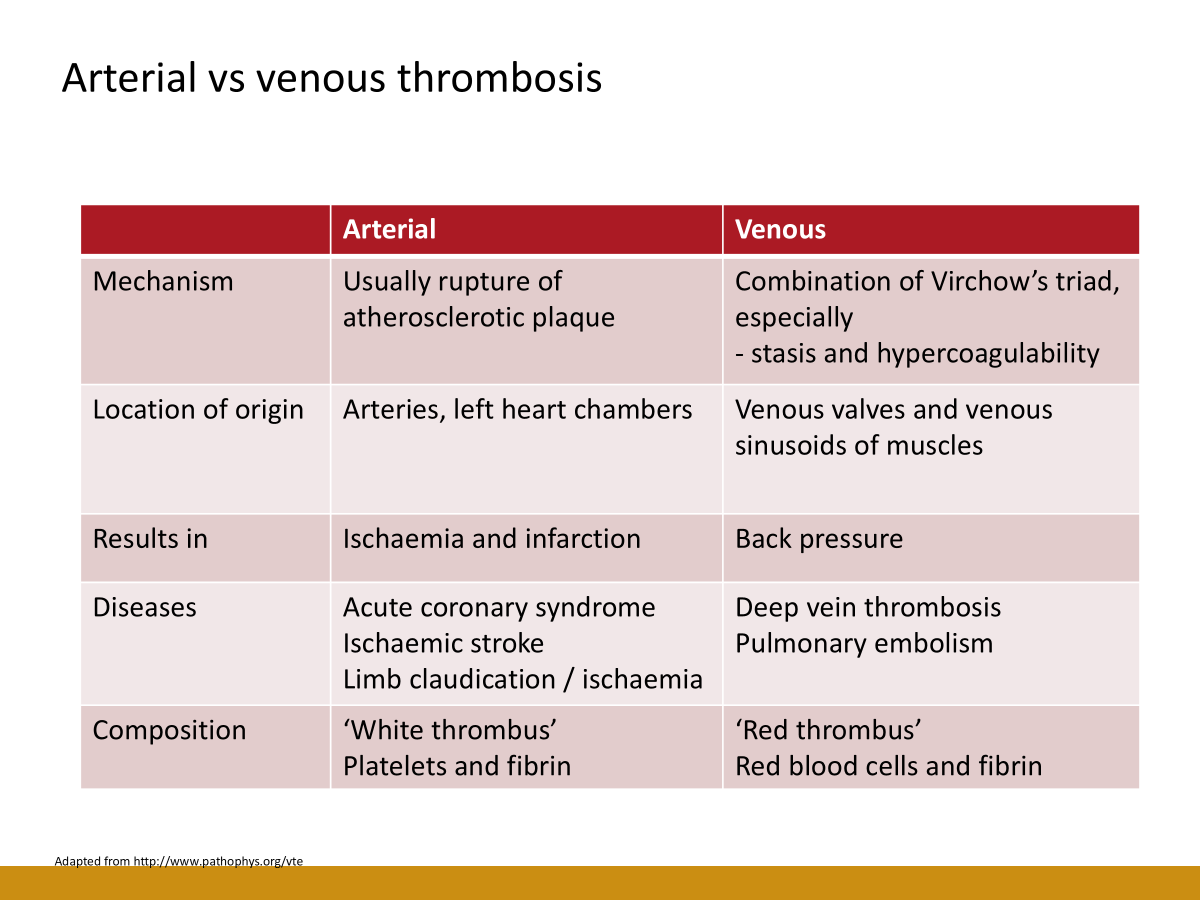
white arterial thrombus vs red venous thrombus
symptoms consequence of back pressure in venous thrombosis
long haul flights not the only cause of DVT, it’s associated with other factors e.g. dehydration, alcohol
superficial thrombosis within the veins - thrombophlebitis?
pregnancy associated increased risk of DVT in left leg 3rd trimester - oestregen strong pro thrombotic hormone
adenocarcinoma secrete factors that activate clotting cascade, leading to increased thrombosis
sepsis activated protective inflammatory system activation clotting system leading to thrombosis
pain and swelling in calf, distal leg, majority of DVT in lower limbs
thromboembolism - movement of thrombus along vessel
as supposed to fat embolism if someone had a fracture, fat moves along vessel
air embolism
venous thromboembolism
venous thrombosis can occur in veins of distal colon in some ischaemic colitis, those that present not due to arterial occlusion but due to congestal - frequent in women who are smokers
thrombosis in liver - kiary syndrome, within portal veins leading to infarction of liver
intracranial thrombosis - those pregnant or on contraceptive pill
for venous thromboembolism make diagnosis after CT if presented with stroke like symptoms, most in young female patients
leading cause of maternal death
if left untreated 1 in 3 people die
present with pleuritic chest pain on right, find PE on left in imaging, unrelated to pain on right hand side
more worried about segmental and..
sub-segmental not sure but anticoagulate
risk increases as you get older
younger -common in women
older-common in men
risks
-pregnancy -malignancy -primary pulmonary hypertension -oestrogens -malignancy -lower limb problems
prevention
-early mobilisation
-anti embolism stockings
-other mechanical methods of thromboprophylaxis in patients anaesetised for long period of time to help venous return
-pharmacological thromboprophylaxis
sign guidelines say risk stratification for every patient
signs
-swelling of whole leg, persistent discomfort in calf or groin where the deep veins run, calf tenderness “tight shoes, socks causing discomfort”
-warmth
-redness-erythema
-prominent collateral veins
-unilateral pitting oedema
-very significant DVT leg can be ischaemic
very severe pain is not suspecting of DVT
blueish leg or swollen could be very significant DVT causing significant back pressure compromising arterial supply
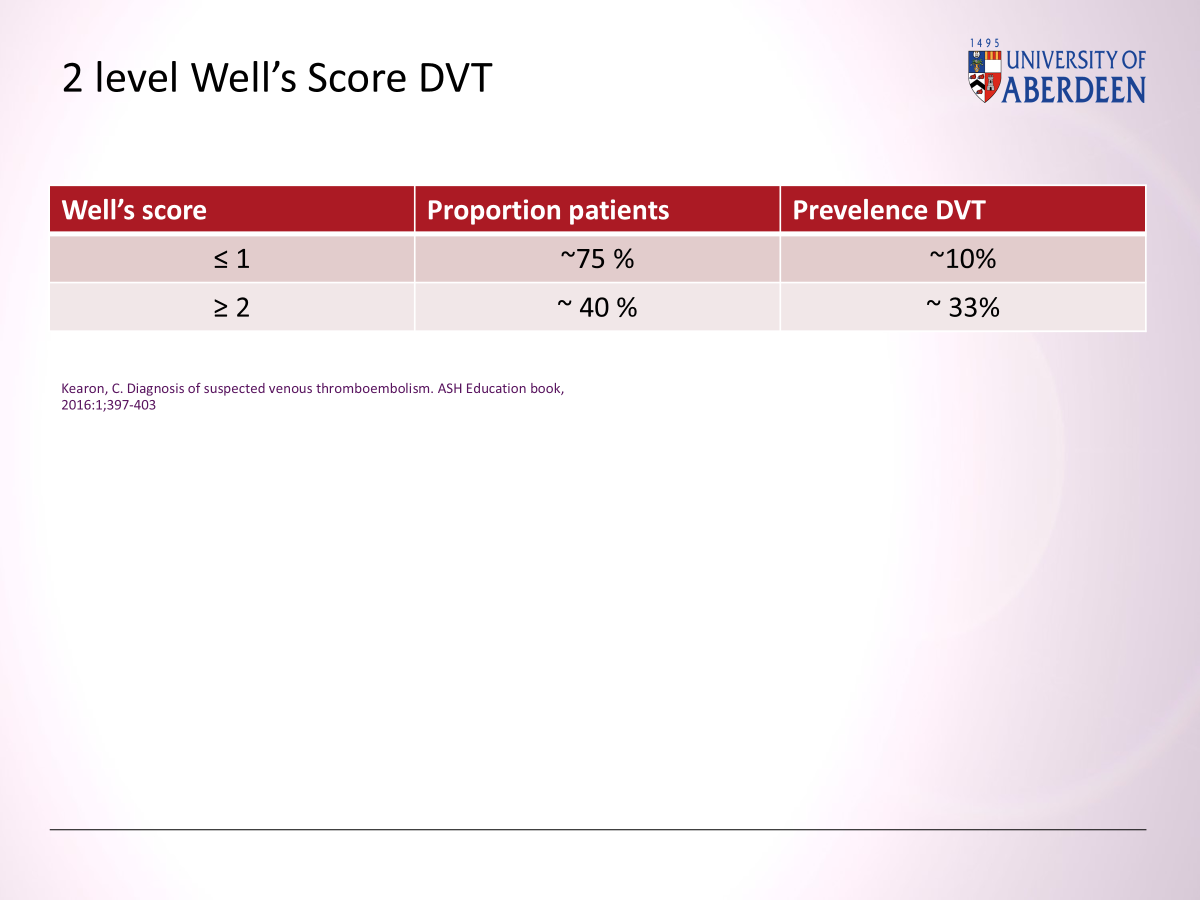
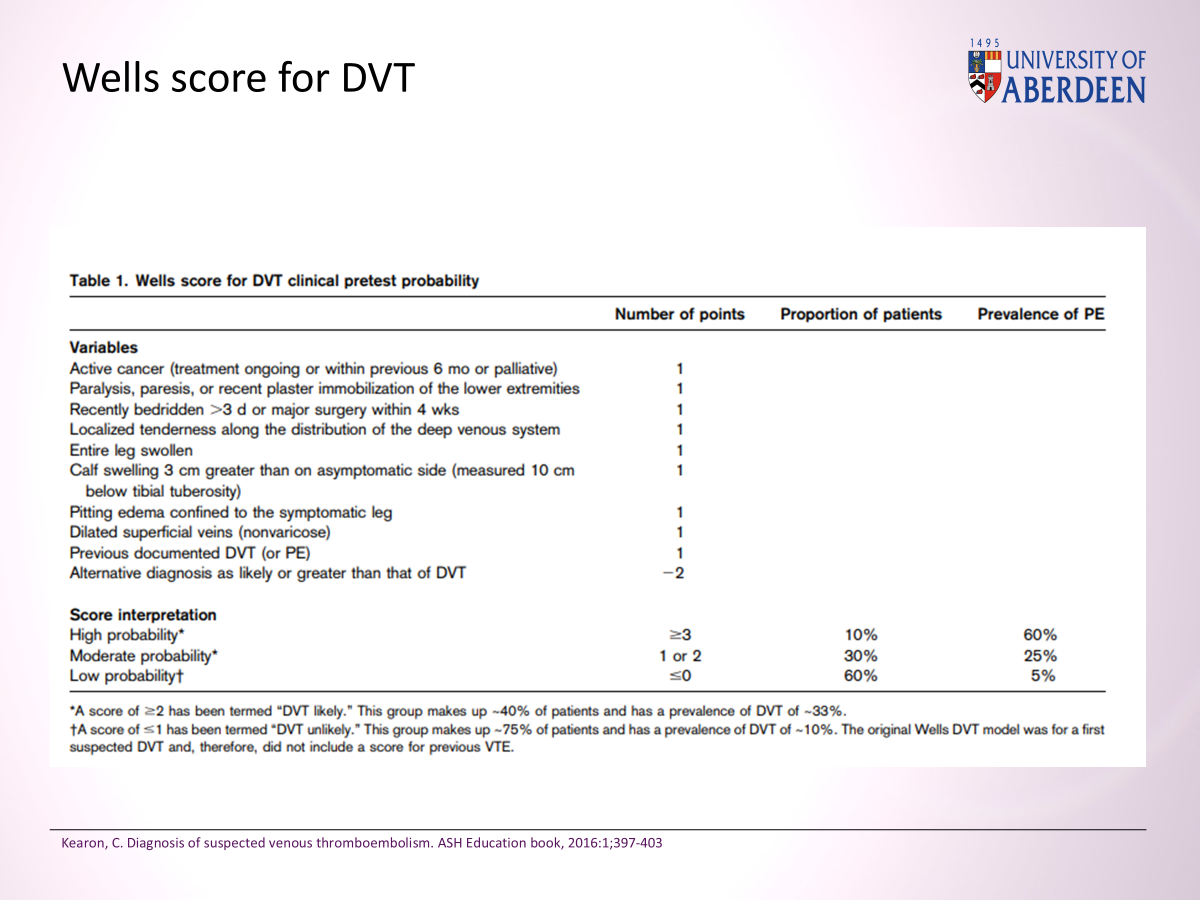
well’s score for DVT
low risk - d-dimer, if negative then excluded DVT
high risk -ultrasound
**can’t use well score in pregnant patient or those very high risk e.g. IV patients
GOLD STANDARD TEST: venous limogram?
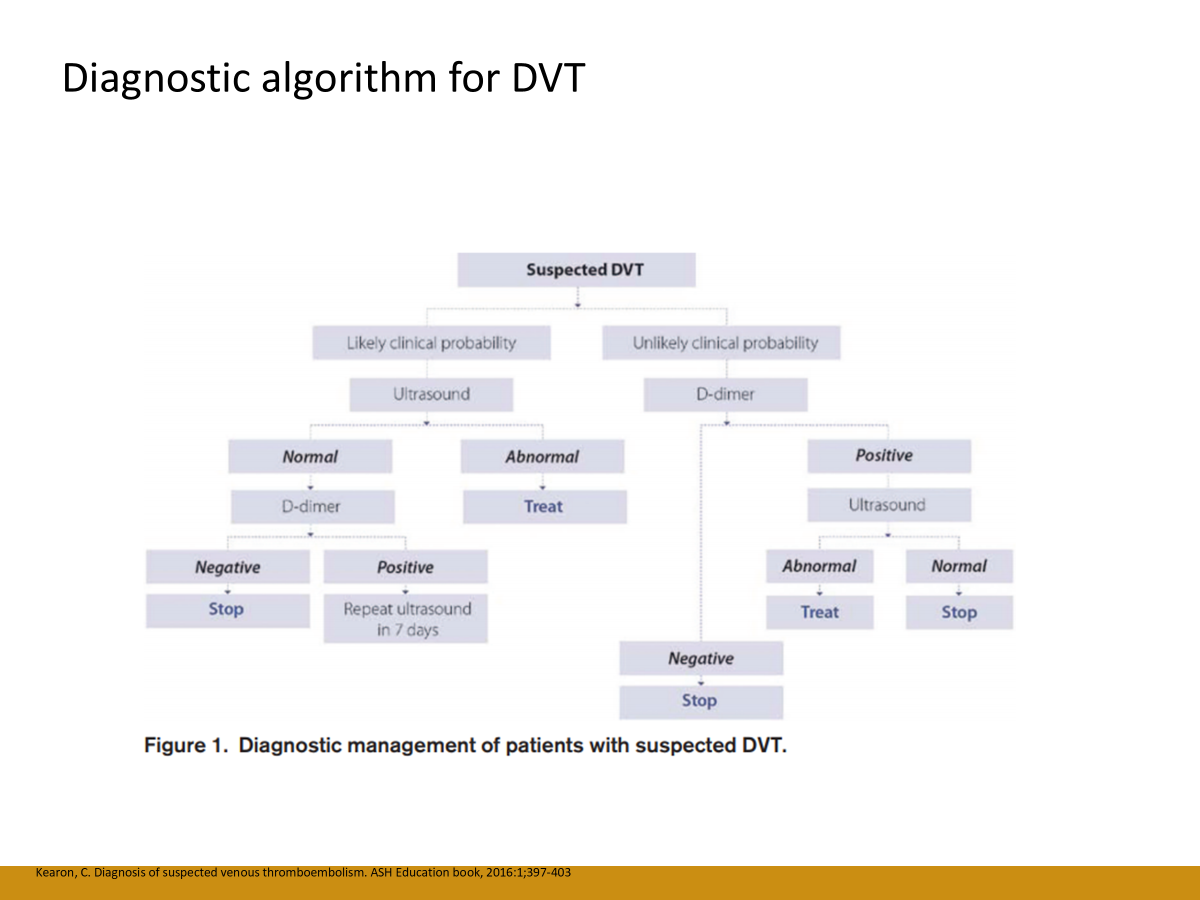
if ultrasound abnormal -treat
in higher risk do ultrasound, if it’s normal then you do d-dimer, if it is positive you repeat ultrasound in 7 days
as DVT progress above knee- most risk of PE
essential two tests to exclude DVT
well score, d-dimer
and carry on from there
D-dimer very sensitive for VTE
non specific if patient has bruise, bleeding, malignancy, anything that activated clotting cascade can lead to positive D-dimer
high sensitivity, low specificity
symptoms and signs of PE
•Pleuritic chest pain
•Breathlessness- dyspnoea
•[Blood in sputum- haemoptysis
•Rapid heart rate- tachycardia → likely sinus tachycardia some non specific T wave changes
•Pleural rub on auscultation- very rarely, usually as pulmonary infarction and consolidation, sounds like walking on fresh snow
•usually due to pulmonary infarction
**acute breathlessness
massive PE relatively rare
•Severe dyspnoea of sudden onset
•Collapse
•Blue lips and tongue - cyanosis
•Tachycardia
•Low blood pressure
•Raised jugular venous pressure
•May cause sudden death
well score PE also excludes pregnancy but can use in some who are IV drug users
well score positive → d-dimer, if negative stop (low risk), excluded pulmonary embolism
well score positive → CT angiogram (high risk) / isotope ventilation or perfusion scan
^history first and pre test probability
when starting treatment looking at why PE has happened, signs of malignancy?
those with PE can have malignancy in next 12-24 months
provoked DVT is below level that you would give anticoagulant
risk of bleeding from anticoagulant 1-2%
young patients with unprovoked VTE, get VTE analysed in more depth by haematologist to see if inheritance thrombophilias
•Consider risk of recurrence
•Clinical Risk
•Cancer patients
•DASH score/ HERDoo2 etc
main treatment is anticoagulation
provoked 3 months because provoked would eventually go away
unprovoked and high risk of reocurrence - lifelong anticoagulation if BMI above 30, cancer, something that won’t go away
patients very obese warfarin instead of DOAC
thrombectomy if causing ischaemia
thrombolysis if PE so big like in cardiac arrest or high risk, reserved for extremist situation e.g. alteplase
lots of effort
aim of treatment
•Prevent clot extension
•Prevent clot embolization
•Prevent recurrent clot
most patients with DVT will have ongoing swelling after that
most recover fully from PE
some develop pulmonary arterial hypertension
some follow up with echo after 3 months or first if they’re breathless
 Knowt
Knowt