L10 Viral Hepatitis
Objectives
Understand viral hepatitis and the different types
Know the prevalence and risk factors
Understand the pathophysiology and transmission pathways of different hepatitis viruses
Know the clinical course and manifestations of Hep A, B, C
Distinguish vaccine candidates based on risk factors and serology results
Hep A = HAV
Hep B = HBV
Hep C = HCV
Notes
What is Viral Hepatitis
system pathogens that target the liver → hepatic infection and inflammation → Hep A-E (mainly A-C)
Hep B and C are major contributors to what
End Stage Liver Disease (ESLD)
What are the different, varying factors of Viral Hepatitis?
Transmission
Incubation
Hepatotoxicity
Prevention and Treatment
What are the criteria of ACUTE viral hepatitis
Discrete onset date
typically < 6 months
Jaundice
AST/ALT liver enzymes > 2.5 x ULN
What are the criteria of CHRONIC viral hepatitis
Inflammatory condition → Biologic/Virologic/Histologic changes
> 6 months
HBV, HCV, HDV risk factors
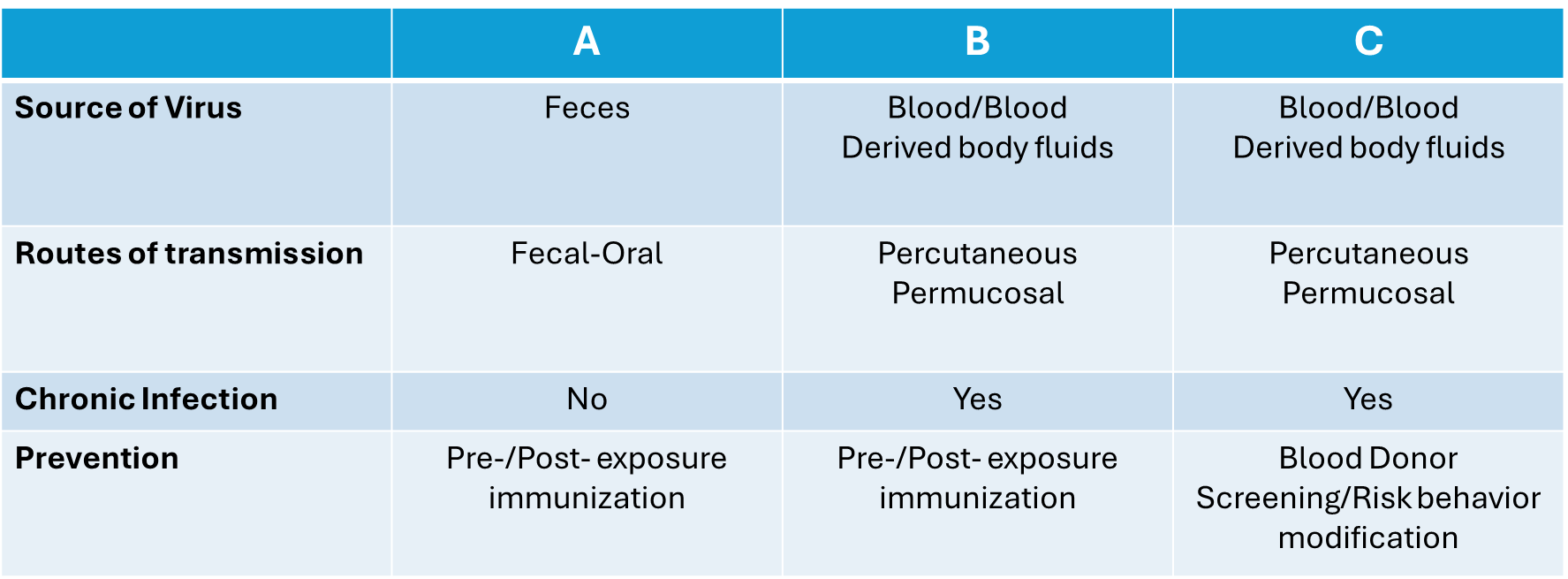
Distinguish main route of transmissions between Hep A-C
Fecal-Oral
A
Blood to Blood and Bodily Fluids
B and C
What type(s) of viral hepatitis have vaccines available for treatment
A and B
T/F: Those infected with Hep A will not experience reinfection
True, obtain life long immunity
What type does not have a cure?
B, can be self-limiting and have life-long immunity but some may result in a chronic infection and require life-long treatment
What treatment/cure is used for Hep C?
no vaccine/immunoglobulin, antiviral treatment for 6-12 weeks
Which types are able to result in chronic infection
B and C
Which of the following viral infections has the highest prevalence in the US?
C
Which viral infection carries the highest risk for occupational transmission to healthcare workers?
B
T/F: Hep A has only been seen in humans
True
What type of virus is HAV
RNA virus
Explain the duration of infected stool of a person with Hep A
2-3 weeks prior to symptoms’ onset and 1 week after
What are the risk factors of Hep A
household or sexual contact
endemic regions
daycares
homelessness — no clean water
IV drug users (Parenteral)
Men who have sex with men (MSM)
HBV/HCV infection
Explain the pathophysiology of Hep A (HAV)
Virus ingestion, absorption, and uptake by liver
Viral replication in hepatocytes
New viral particles → bloodstream (viremia) → infect other hepatocytes or fecal excretion
Viremia (infected blood) within 1-2 weeks of exposure → viral shedding in feces
Asymptomatic but highly transmissible
Incubation period ~28 days but range 15-50
Immune response → Hepatocellular injury, Signs and Symptoms occur ~ 2 months
Viral Clearance
T/F: Hep A is generally a self limiting disease and rarely has complications/fatalities
True
What are the 2 different phases in Hep A Clinical Presentation
Prodromal and Icteric Phases
What is the Prodromal Phase
Non-specific viral syndrome with abrupt onset
~ days to > 1 week
Sx: fever, fatigue, anorexia, nausea weakness, headache, +/- abdominal pain
What is the Icteric Phase
begins 10-14 days after Prodromal Phase
1-4 weeks
Hepatitis specific Sx
Jaundice, Scleral Icterus, Dark Urine
T/F: Liver biopsy is the main diagnostic test for HAV
False, self limiting and doesn’t result in a chronic disease
Why is Serology testing the main diagnostic test for HAV
the body forms abs against HAV (IgM and IgG)
IgM specifically is used for diagnosing Active/Acute
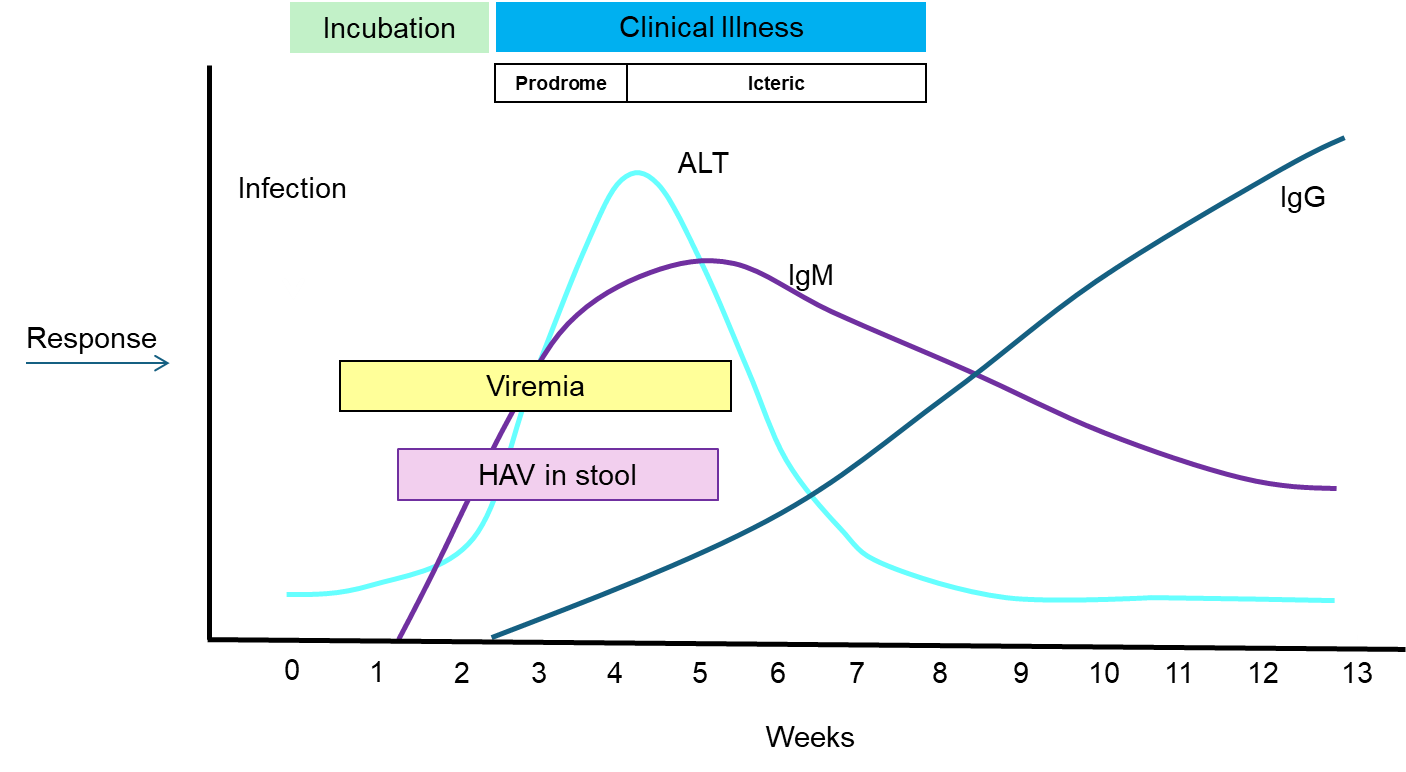
Explain the lifespan of IgM in HAV
occurs early in symptomatic phase
declines over the months
Explain the lifespan of IgG in HAV
occurs late in disease
persists for life
What is IgG presence able to indicate?
Evidence of past exposure and current protection
ex. seen in vaccinated individuals to indicate protection
T/F: HAV Vaccines are only given to adults who have not been vaccinated to travel to endemic countries
False, vaccine preventable disease that is recommended for children between 1-2 years old
T/F: HAV has Prophylaxis (action taken to prevent disease)
True
Pre-Exposure Prophylaxis (PrEP)
primarily vaccine for international travelers
Post-Exposure Prophylaxis (PEP)
Immunoglobulin for unvaccinated or immune compromised that were exposed to HAV
Why is Heb B still a worldwide health problem?
Outside the US, they do not have access to the vaccine treatment
2% of HBV infections → Acute and can lead to what?
Fulminant Hepatitis
rare but severe form of liver failure that rapidly progresses (60-90% mortality)
5-10% of HBV will develop into what?
Chronic Hep B (CHB)
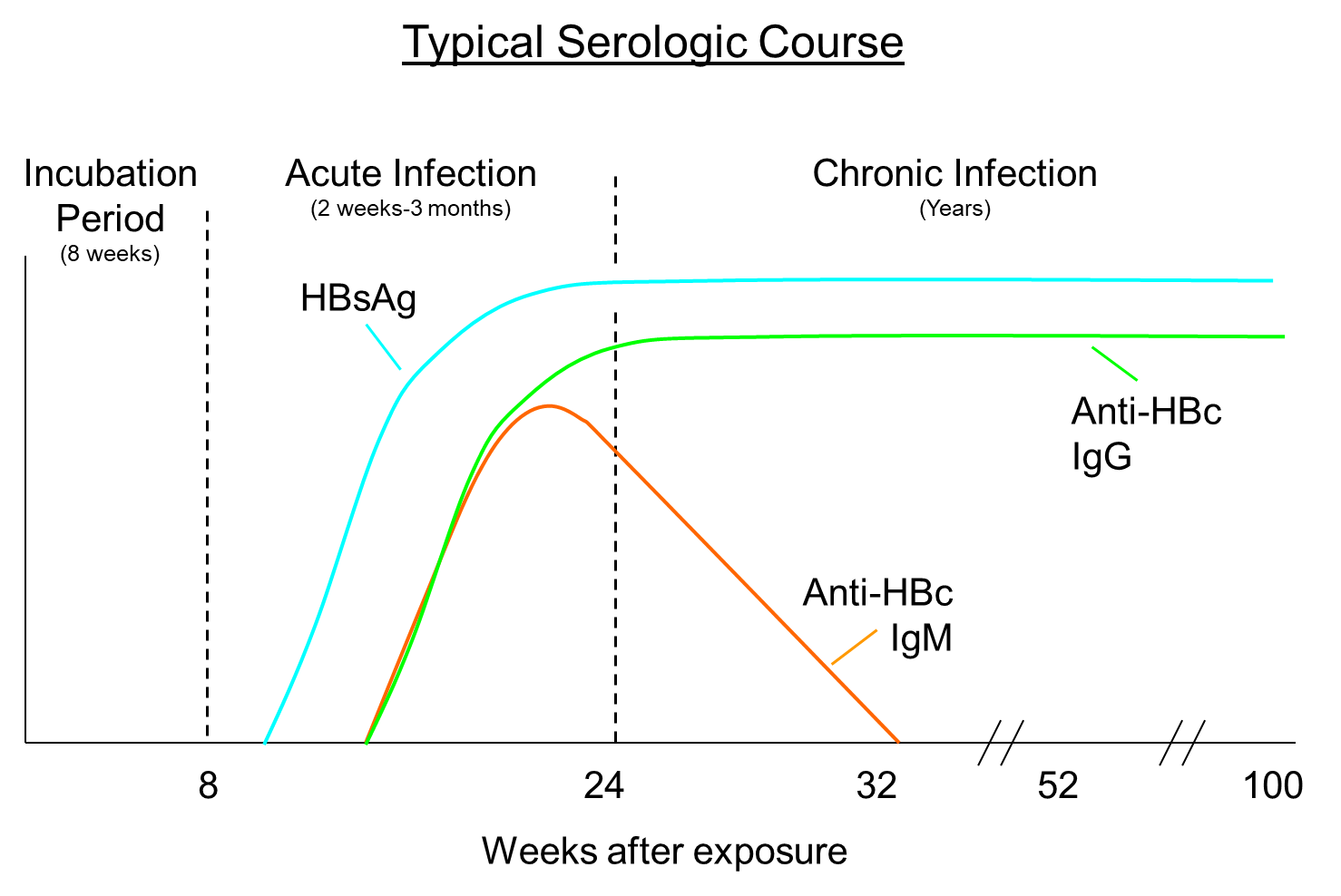
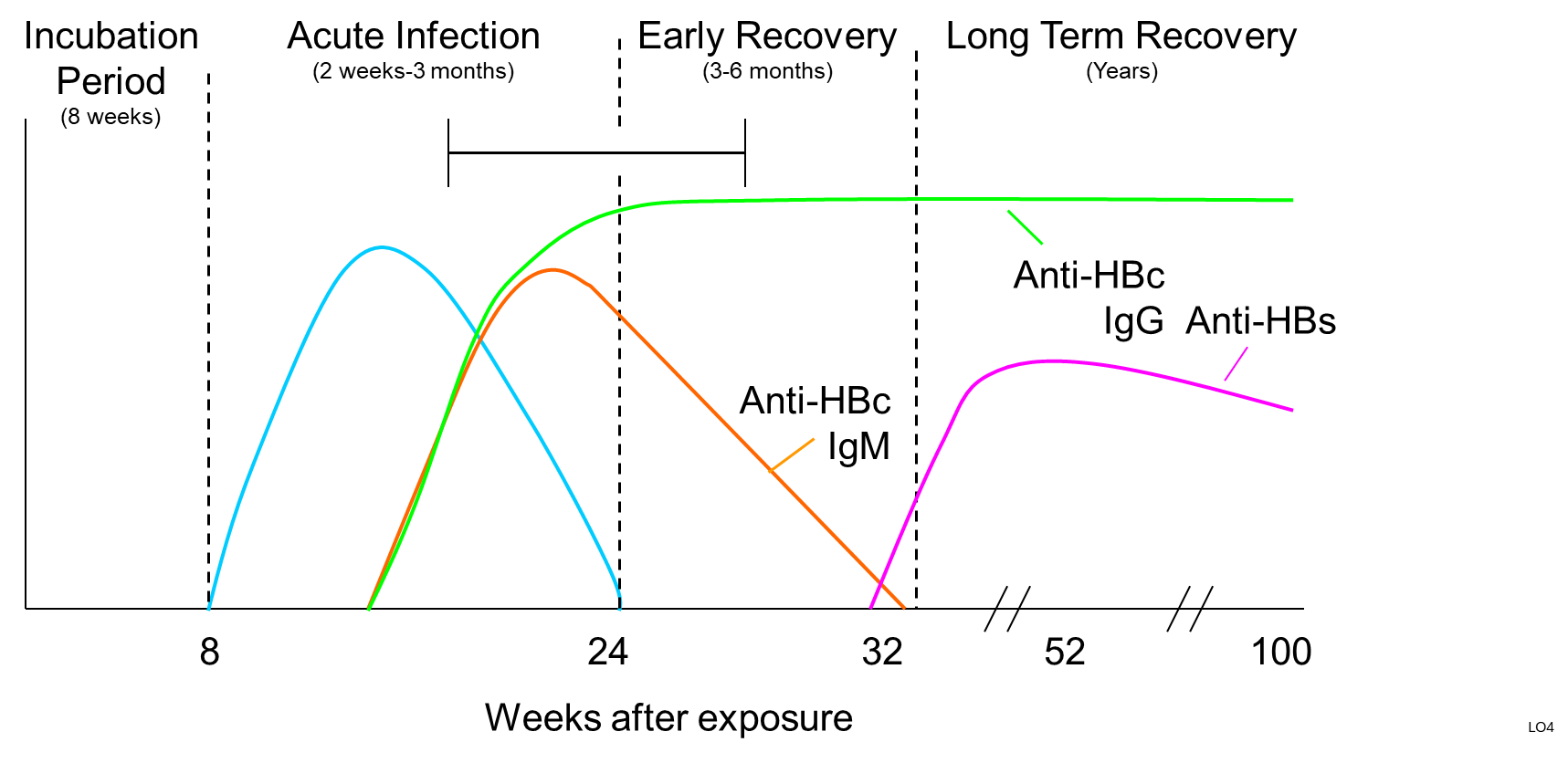
HBV Nomenclature
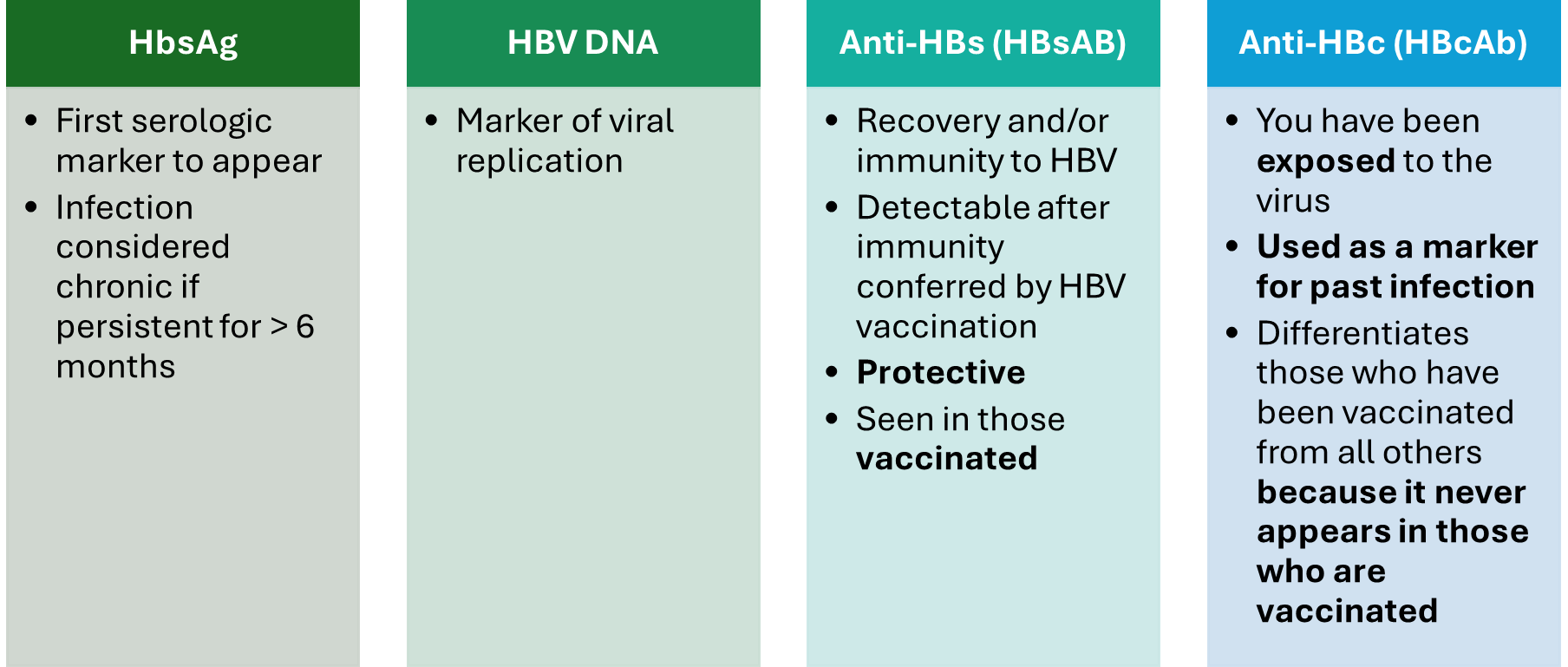
surface abs = HbsAb
core abs = HBcAb
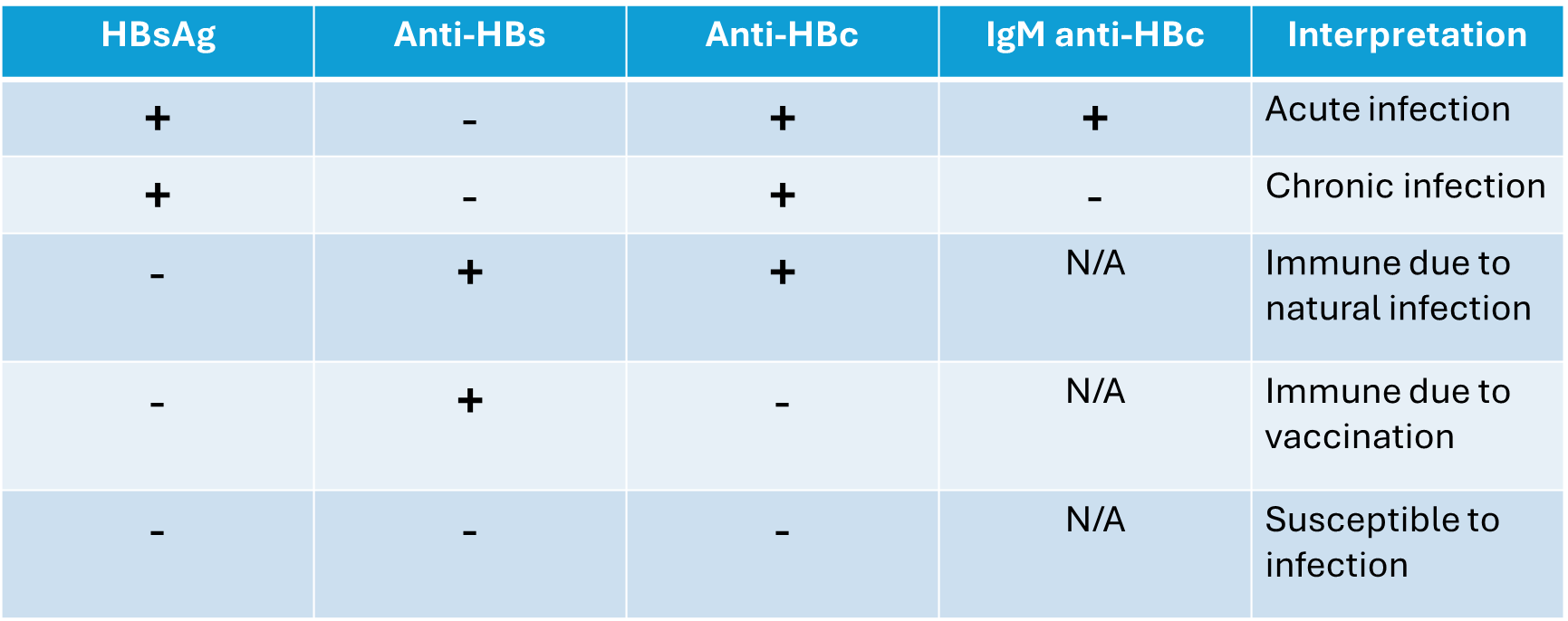
HBV Serology results
When is Chronic Hep B (CHB) most commonly occurs?
Perinatal (around birth)
Infections in older children become chronic only around 30% of the time
T/F: CHB cannot be cleared
False, 90-95% will spontaneously clear the infection and develop lifelong immunity
Where geographically is found to account for 75% of CHB?
Southeast Asia
What type of virus is HBV
DNA Virus
List HBV Risk Factors
Parenteral (IV Drug — needles/syringes)
Birth from an infected mother
Multi-transfused patient before 1972
Needle sticks/sharp instrument exposures for healthcare workers
MSM
Contact with blood or open sores of infection
Sharing razors/toothbrushes/etc
T/F: HBV is Cytopathic (infection directly kills cells)
False, damage from immune system’s inability to clear the virus
Poor cytotoxic T-cell response to viral antigens → persistent inflammation → CHB, Cirrhosis, Hepatocellular Carcinoma
Why does HBV persists in the body
Slow liver blood supply → T-cells’ overexposure to HBV antigens → Desensitization → HBV persistence
Long-term (decades) HBV infection weakens T-cell antiviral potential
What treatments can be used for HBV
Therapeutic Vaccines, Prophylaxis, and Immunomodulators
more effective in younger patients with less impacted T-cell functions
HBV Lifecycle (don’t memorize ?)
HBV → Hepatocytes
HBV DNA Polymerase → covalently closed circular DNA (cccDNA) in Nucleus
Host provides RNA template → viral DNA production
Viral proteins synthesis (HBsAg, HbcAg, HbeAg)
Viral replication → Matured Virions → Blood
What is the Clinical Presentation for Acute HBV
Asymptomatic but can have non-specific viral syndrome
Fever, fatigue, weakness, anorexia, nausea, myalgias +/- abdominal pain and hepatomegaly
What is Immune Tolerance
Virus present but the body is not reacting
associated with Remission phase where symptoms lessened or not present
What is the Immune Active Phase
When the body is attack the infection
What is the Clinical Presentation of Chronic HBV
Periods of remission followed by recurring flares of hepatitis, often still asymptomatic
immune cells responding to HBV replication and destroying hepatocytes
What is happening during flares even though the patient may be asymptomatic
progressive liver damage → scarring, fibrosis → Cirrhosis
How long can it take for Chronic HBV symptoms to appear
30 years → similar to acute sympt and advanced liver disease
T/F: HBV is more prevalent in the US then HVC
False
What is HCV a leading cause and indicator (respectively) for?
Chronic Liver Disease and Liver Transplant
What type of virus is HCV
Single stranded RNA
6 major genotypes
Why does HCV have frequent viral mutations
Lacks proofreading polymerase
Why does HCV persist in the body
inadequate humoral and cellular response
What is a result of HCV having a serum half-life of 2-3 hours
fast viral replication
What are the Risk Factors of HCV
Parenteral
sex with infected partner
perinatal
sharps (healthcare workers, unsterile tattoos)
blood/open sores
What are the clinical presentation of Acute HCV
asymptomatic
non-specific
flu-like, weight loss
What are the clinical presentations of Chronic HCV
remission periods but less than HBV
viral RNA > 6 months
chronic liver inflammation
asymp
Cirrhosis ~ 30 yrs
15-25% of acute HCV result in what
HVC RNA Clearance
75-85% of Acute HCV result in what
Chronic infection
50-75% → Extrahepatic Diseases
10-20% → Cirrhosis over 20 years → Hepatocellular carcinoma (14%) or Decompensated Cirrhosis (50% 5 year survival rate)
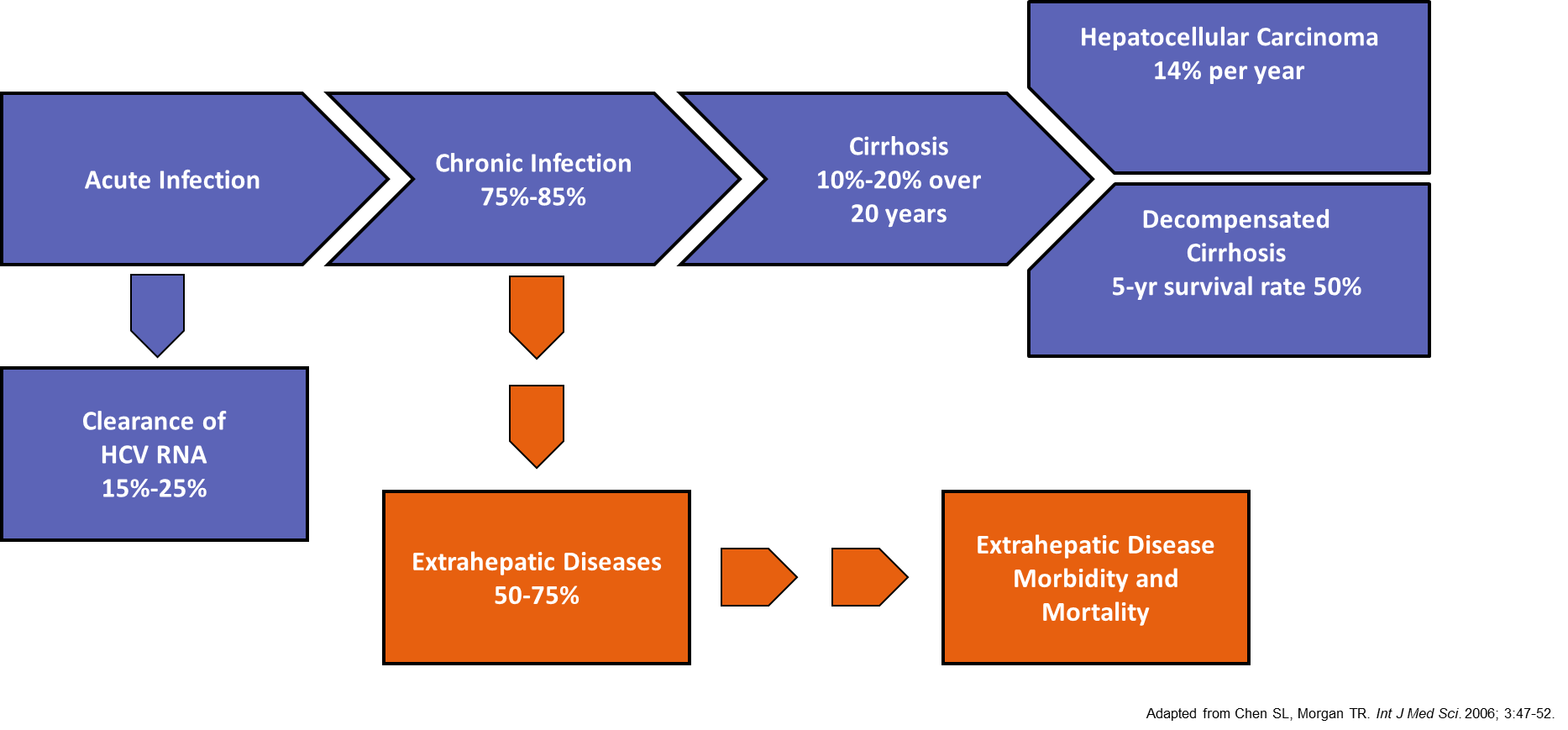
Chronic HCV persists for decades in who
untreated patients
HC V Life Cycle (don’t memorize)
Virus enters cell → RNA release → ER → Translate and Produce Polyprotein → protein cleavage via Protease Enzymes → RNA Replication via Polymerase → Viral Assembly, Budding, and Release
What are used from serologies/tests for diagnosing HCV
IgG
detectable within 2 months
past/current exposure
persists for years
HCV RNA
detectable within 2 weeks of infection
Review
What population has the highest risk for HCV
IV drug users