Session 9: Immune System Notes
The Immune System
Overview
The immune system provides resistance to disease and is made up of two intrinsic systems:
Innate (nonspecific) defense system
Constitutes first and second lines of defense
First line of defense: external body membranes (skin and mucosae)
Second line of defense: antimicrobial proteins, phagocytes, and other cells (inhibit spread of invaders; inflammation most important mechanism)
Adaptive (specific) defense system
Third line of defense attacks particular foreign substances (takes longer to react than innate)
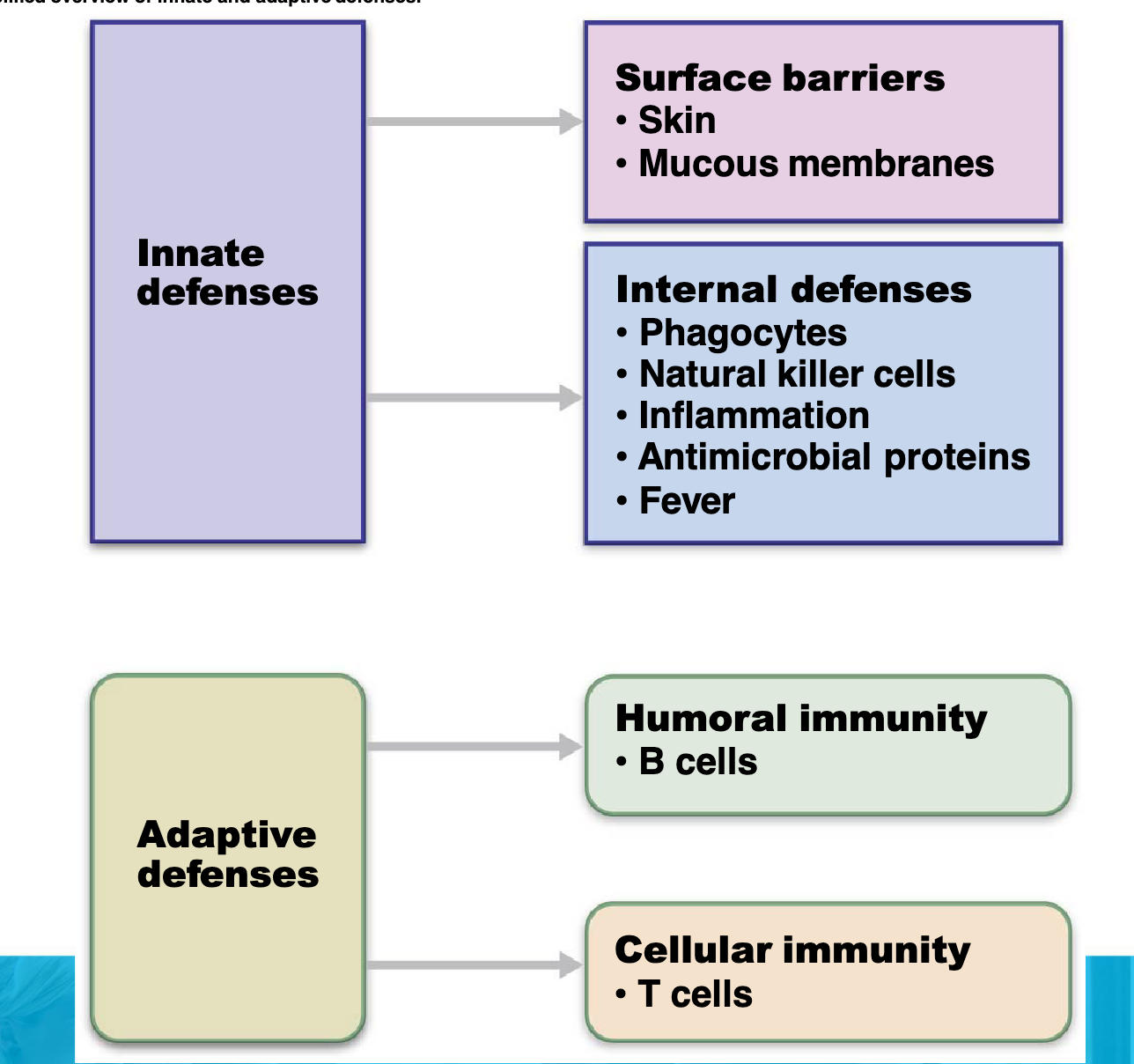
Innate (Non-Specific) Immunity
Protects the host from foreign substances, working against all bacteria or invasions, not just one.
Two parts:
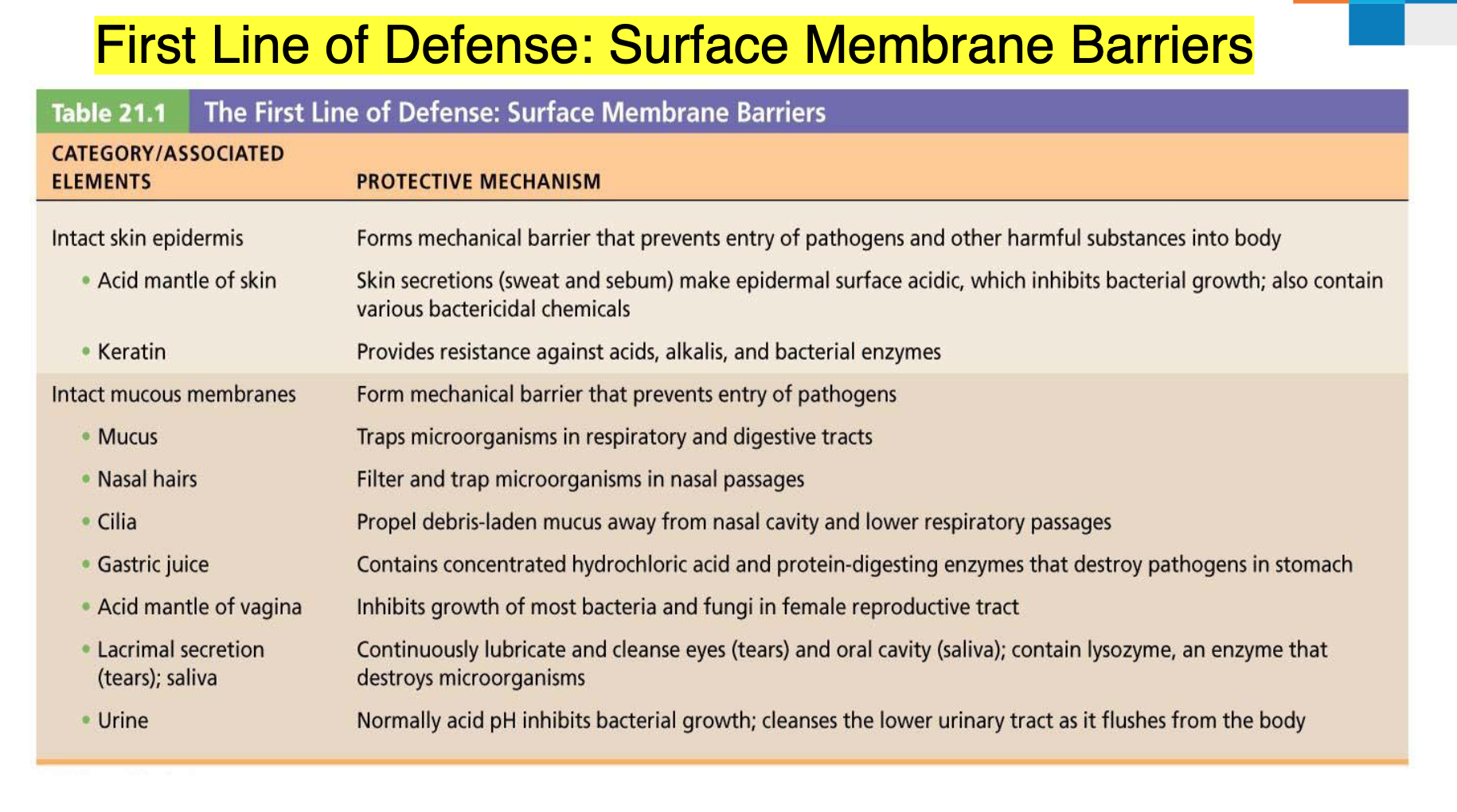
Protective barriers:
Skin and mucous membranes: provide a physical and chemical barrier using keratin, mucous, cilia, salivary enzymes, and acid secretions.
Non-specific cellular and chemical defenses:
Cells and chemicals that act against foreign invaders, abnormal cells, and damaged tissues; it's the "first line of defense": initial protection, fast, non-specific.
Second Line of Defense: Cells and Chemicals
Innate system necessary if microorganisms invade deeper tissues; includes:
Phagocytes: cells that engulf and destroy pathogens and debris.
Mast cells
Usually located along blood vessels
Detect pathogens and send out chemicals like histamine, triggering the inflammatory response.
Neutrophils
Most abundant type of white blood cell within the tissues.
Phagocytose pathogens and then die, contributing to pus formation.
Release chemicals that trigger the inflammatory response.
Macrophages
Originate from white blood cells called monocytes in the bloodstream.
Voracious and resilient phagocytes.
Can freely circulate or reside within loose connective tissue, bone marrow, and lymphoid tissue.
Do not die after phagocytosing pathogens.
Release inflammatory mediators.
Natural killer (NK) cells
Nonphagocytic, large granular lymphocytes that police blood and lymph.
Kill cancer and virus-infected cells before the adaptive immune system is activated.
Attack cells that lack “self” cell-surface receptors.
Kill by inducing apoptosis in cancer cells and virus-infected cells.
Secrete potent chemicals that enhance the inflammatory response.
Inflammatory response (macrophages, mast cells, WBCs, and inflammatory chemicals e.g., histamine)
Antimicrobial proteins (interferons and complement proteins).
Fever
Basophils
Associated with allergy response and hypersensitivity reactions.
Produce compounds that co-ordinate immune responses, including histamine and serotonin that induce inflammation
Eosinophils
Responsible for combating multicellular parasites and certain infections
Control mechanisms associated with allergy and asthma
Phagocytosis
Engulfing or ingestion of cells by another cell.
Steps:
Phagocyte adheres to pathogens or debris.
Phagocyte forms pseudopods that eventually engulf the particles, forming a phagosome.
Lysosome fuses with the phagocytic vesicle, forming a phagolysosome.
Toxic compounds and lysosomal enzymes destroy pathogens.
Sometimes exocytosis of the vesicle removes indigestible and residual material.
Inflammation
Triggered whenever body tissues are injured due to trauma, heat, irritating chemicals, or infections.
Benefits:
Prevents spread of damaging agents.
Disposes of cell debris and pathogens.
Alerts adaptive immune system.
Sets the stage for repair.
Four cardinal signs of acute inflammation:
Redness
Heat
Swelling
Pain
Sometimes, a fifth sign, impairment of function, is seen if movement or use of the area is hampered.
Stages:
Inflammatory chemical release (histamine, complement, kinins, prostaglandins, etc.)
Vasodilation and increased vascular permeability
Phagocyte mobilization
Leukocytosis (increased numbers of white blood cells in the bloodstream)
Leukocytes migrate to injured area
Margination (leukocytes cling to capillary walls)
Diapedesis (leukocytes pass through capillary walls)
Phagocytosis of pathogens and dead tissue cells (by neutrophils, short-term; by macrophages, long-term)
Pus may form
Area cleared of debris
Healing
Interferon
Released from virus-infected cells.
Briefly provides nonspecific resistance to viral infections.
Antiviral effect of interferon.
Acts as a “whistle-blower”.
Anticancer effects of interferon.
Markedly enhances actions of cell-killing cells.
Interferon Transiently Inhibits Multiplication of Viruses in Most Cells
Complement System
Comprise of 20+ types of plasma proteins that have a variation of functions including;
Accelerates the inflammatory process
Directly kills microorganisms by punching holes
Enhances both adaptive and innate immune responses
Formation of the membrane attack complex: C5 through C9 assemble into a large, doughnut-shaped protein complex.
Pathways:
Alternate complement pathway: Binding directly to a foreign invader nonspecifically activates the complement cascade (an innate immune response).
Classical complement pathway: Binding to antibodies (Y-shaped molecules) produced against and attached to a particular foreign invader specifically activates the complement cascade (an adaptive immune response).
Fever
An abnormally high core body temperature acts as a more ‘global’ way of the body to destroy invading microorganisms in comparison to localized inflammation processes.
Some types of white blood cells release chemicals called pyrogens when they are exposed to certain foreign substances. These pyrogens act on the hypothalamus, which is the body’s thermostat to increase the core temperature.
There are a number of proposed ideas by which this helps the body combat infection;
Inhibit reproduction/activity of invading microbes
Speed up the body’s healing process
Antigens
Infectious agents (pathogens) contain a unique set of proteins they have on their surface membrane which is like a ‘name tag’ (called antigens). These are recognized by our immune system and can stimulate a protective response.
Most are large, complex molecules not normally found in the body (nonself).
Adaptive (Specific) Immunity
The ability of the host (e.g., a person) to recognize and mount a defense, which is targeted to a particular foreign substance, and to retain a memory of this for future use.
It is also called the adaptive response.
Specific immunity is:
antigen-specific
systemic (not localized to one part)
has memory
Lymphocytes and Antigen-Presenting Cells
Adaptive immune system involves three crucial types of cells
Two types of lymphocytes
B lymphocytes (B cells)—humoral immunity
T lymphocytes (T cells)—cellular immunity
Antigen-presenting cells (APCs)
Do not respond to specific antigens
Play essential auxiliary roles in immunity
Development of Lymphocytes
Red blood cells, platelets, monocytes, and granulocytes originate from hemopoietic precursor cells in the bone marrow.
During fetal life and early childhood, lymphocyte development occurs in the bone marrow and thymus.
After early childhood, it primarily occurs in the bone marrow.
B cells mature in the bone marrow, while T cells mature in the thymus.
Mature lymphocytes populate peripheral lymphoid tissues like lymph nodes.
Foreign invasion triggers B and T cells to initiate antibody-mediated and cell-mediated immune responses, respectively.
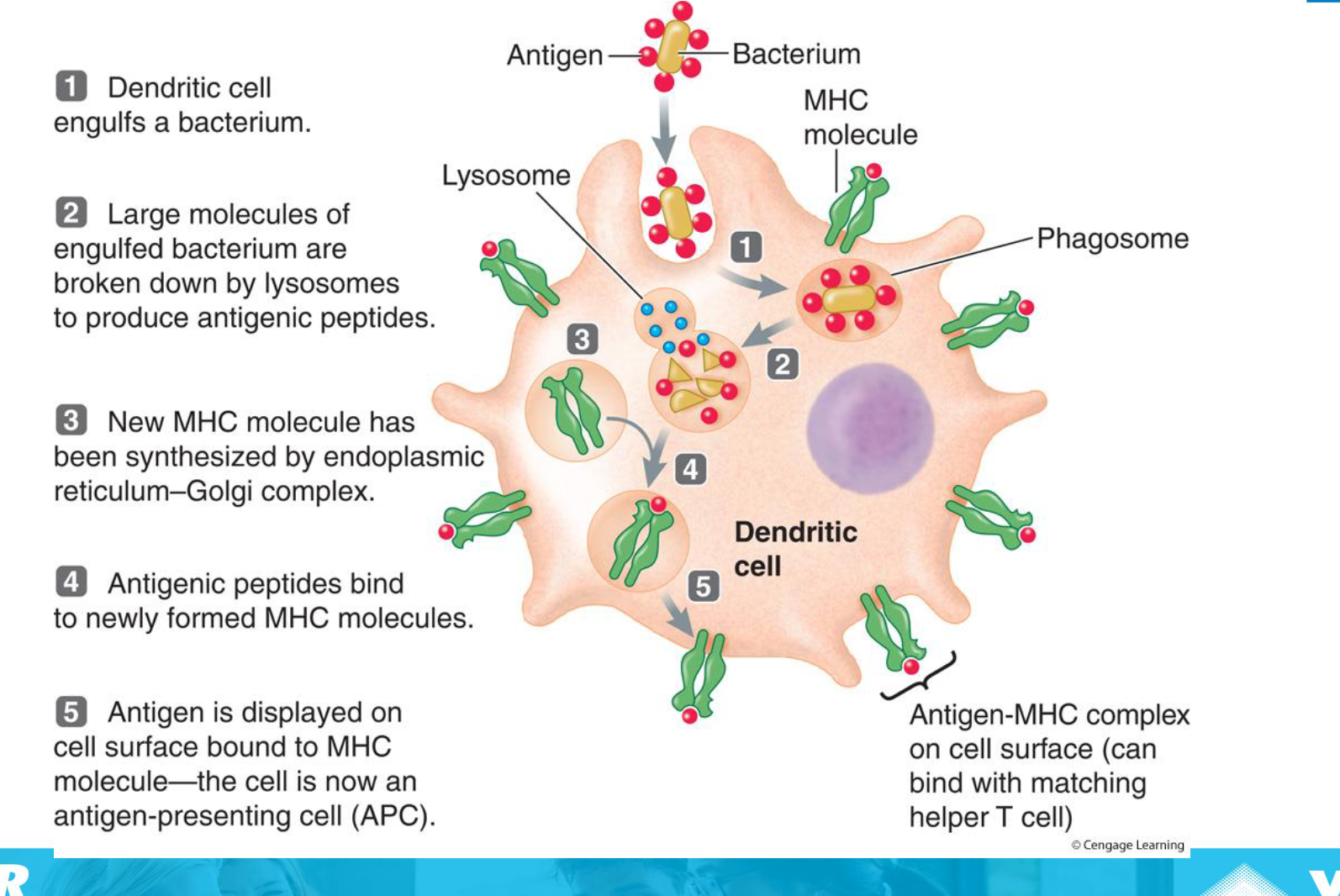
Antigen-Presenting Cells (APCs)
Dendritic cells (DC)
Bone marrow derived leukocytes (WBC).
Large surface area can communicate with a large number of other cells, making them effective messengers.
Located at sites where pathogens are likely to enter (e.g., skin, lungs, nose).
Ingest pathogens and retain the antigen (name tag) that was represented on the surface of that pathogen.
Travel to the lymphatic system and present that antigen to the cells of the ‘adaptive/acquired’ immune system, triggering a more specific and powerful response.
Key link between innate and adaptive immunity.
Humoral Immunity
Mediated by antibodies (proteins produced by B lymphocytes) present in body fluids (blood, lymph, etc.).
Antibodies attach and temporarily inactivate extracellular pathogens (bacteria, bacterial toxins, and free viruses).
They ‘mark’ the target which signals other cells (neutrophils, macrophages, complement proteins) to phagocytose them.
Cell-Mediated Immunity
Mediated by T lymphocytes.
Cytotoxic T-cells are ‘hitmen’ which directly target and destroy intracellular pathogens (viruses, some bacteria and parasites, cancer cells, and cells of foreign grafts).
T-helper cells act indirectly by releasing chemicals that enhance the immune response.
B Lymphocytes: Antibody-Mediated Immunity
Antigen binds to the B cell.
With the assistance of a T helper cell, the B cell divides rapidly, and then the cells differentiate into plasma cells.
Plasma cells produce large amounts of specific antibody (200 molecules per second).
Combine with the specific type of free antigen that stimulated activation of the plasma cell.
Antibody subclasses: IgM, IgC, IgE, IgA, and IgD.
Some of the B cells develop into memory cells.
B cell proliferation is turned off by T suppressor cells.
It takes 3-6 days after the first meeting with an antigen for an antibody response to be mounted peaking at about 10 days, then declining. B cells only survive for 5 days.
B-Cell Activation and Clonal Selection
Population of unactivated B cells, each a member of a different B-cell clone that makes a specific antibody, which is displayed on the membrane surface as a BCR.
Binding of antigen and interaction with a helper T cell stimulates the matching B cells to divide and expand the clone of selected cells.
A few new B-cell clones differentiate into memory B cells, which respond to a later encounter with the same antigen.
Most of the new B-cell clones differentiate into plasma cells, which secrete antibodies.
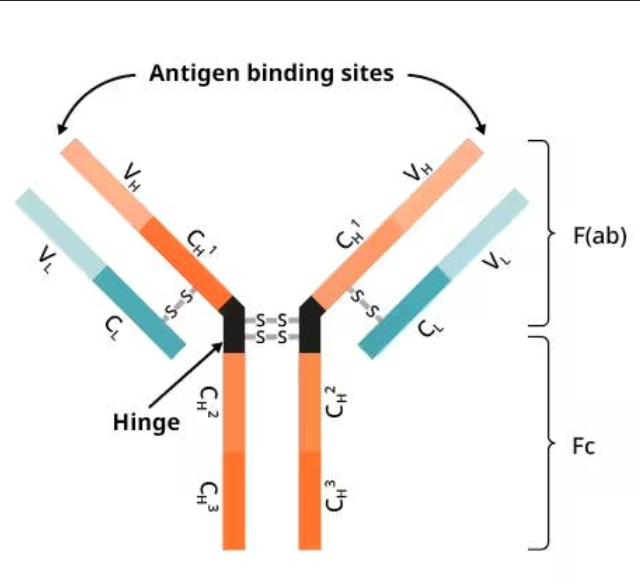
Antibodies (Immunoglobulins - Igs)
Proteins secreted by plasma cells.
Make up gamma globulin portion of blood
Capable of binding specifically with antigen detected by B cells.
Basic antibody structure
Overall T- or Y-shaped antibody monomer consists of four looping polypeptide chains linked by disulfide bonds
Four chains consist of:
Two identical heavy (H) chains with hinge region at “middles”
Two identical light (L) chains
Variable (V) regions at one end of each arm combine to form two identical antigen-binding sites
Antibody Classes (5 major types)
IgM, IgA, IgD, IgG, and IgE
IgM:
Pentamer (larger than others); first antibody released
Potent agglutinating agent
Readily fixes and activates complement
IgA (secretory IgA)
Monomer or dimer; found in mucus and other secretions
Helps prevent entry of pathogens
IgD
Monomer attached to surface of B cells
Functions as B cell receptor
IgG
Monomer; 75–85% of antibodies in plasma
From secondary and late primary responses
Crosses placental barrier
IgE
Monomer active in some allergies and parasitic infections
Causes mast cells and basophils to release histamine
Antibody Mechanisms
Antibodies do not directly kill cells but activate mechanisms that do.
Agglutination (clumping of antigenic cells)
Activation of complement system
Enhancement of phagocytosis (opsonization)
Stimulation of natural killer (NK) cells: antibody-dependent cellular cytotoxicity
Immunological Memory
Primary immune response:
cell proliferation and differentiation upon exposure to antigen for the first time
Lag period: 3 to 6 days
Peak levels of plasma antibody are reached in 10 days
Antibody levels then decline
Secondary immune response
Re-exposure to same antigen gives faster, more prolonged, more effective response
Sensitized memory cells provide immunological memory
Respond within hours, not days
Antibody levels peak in 2 to 3 days at much higher levels
Antibodies bind with greater affinity
Antibody level can remain high for weeks to months
Primary vs Secondary Immune Response
Primary response is the response of the immune system after first exposure to an antigen
Mounting specific response may take between 7-10 days
Secondary response is the response of the immune system after repeated exposure to an antigen
Response is faster as there are memory cells for the antigen
Active and Passive Humoral Immunity
Active:
Naturally acquired: Infection; contact with pathogen
Artificially acquired: Vaccine; dead or attenuated pathogens
Passive:
Naturally acquired: Antibodies passed from mother to fetus via placenta; or to infant in her milk
Artificially acquired: Injection of exogenous antibodies (gamma globulin)
T Lymphocytes: Cell-Mediated Immunity
T cells bind directly with their targets
The three types of T cells are cytotoxic, helper, and regulatory (suppressor) T cells
T cell recognizes antigen
T cell is activated by the foreign antigen
T cell enlarges and divides to produce a clone of cells, which differentiate to carry out the functions of the particular T cell class.
If the T cell is a helper cell it secretes lymphokines which stimulate other T and B cells
If the T cell is a cytotoxic cell it causes cell lysis of virus-infected or tumor cells in a number of ways. E.g. by punching holes in the cell membrane using perforin, or by secreting tumor necrosis factor.
T memory cells are also produced.
When the infection is overcome, T suppressor cells secrete substances to turn off the attack.
T-Cell Activation and Function
Cytotoxic T cells recognize foreign antigen in association with self-antigen on the surface of infected host cells.
Helper T cells interact with antigen-presenting cells (APCs) displaying foreign antigen bound to class II MHC molecules.
This interaction activates helper T cells, leading to cytokine secretion, which stimulates B cell proliferation and enhances other immune activities.
B-Lymphocytes
The antigen binds to the B cell.
With the assistance of a T helper cell, the B cell divides rapidly, and then the cells differentiate into plasma cells.
The plasma cells produce large amounts of specific antibody (200 molecules/sec).
Some of the B cells develop into memory cells
B cell proliferation is turned off by T suppressor cells.
T-Lymphocytes
The T cell recognises antigen and divides to produce a clone of cells, which differentiate to carry out the functions of the particular T cell class.
If the T cell is a helper cell it stimulates other T and B cells
If the T cell is a cytotoxic cell it causes cell lysis of infected or tumour cells
T memory cells are also produced.
When the infection is overcome, T suppressor cells secrete substances to turn off the attack.
Activation of Helper T Cells by Antigen Presentation
Bacterium is taken up by phagocytosis and degraded in a lysosome.
Bacterial antigenic peptides are displayed on APC cell surface bound to class II MHC molecules and presented to helper (CD4+) T cells with TCRs that recognize the antigen.
APC secretes cytokines that activate T cell.
Activated T cell secretes cytokines that stimulate T cell to proliferate to expand clone of selected cells.
Cloned helper T cells are ready to activate B cells and enhance other immune activities.
Activation of B Cells Responsive to T-Dependent Antigen
BCR binds to antigen. Antigen is internalized by receptor-mediated endocytosis and its macromolecules degraded. Antigenic peptides produced are displayed on cell surface bound to class II MHC molecules.
TCR of a helper T cell recognizes specific antigen on B cell, and CD4 coreceptor links the two cells together.
Helper T cell secretes cytokines that stimulate B cell proliferation to produce clone of selected cells.
Some cloned B cells differentiate into plasma cells, which secrete antibodies specific for the antigen, while a few differentiate into memory B cells.
Antibodies bind with antigen, targeting antigenic invader for destruction by the innate immune system.
LYMPHATIC SYSTEM
Functions of the Lymphatic System:
Fluid balance: Excess interstitial fluid enters lymphatic capillaries and becomes lymph (30L from capillaries into interstitial fluid, 27L return leaving 3L).
Fat absorption: Absorption of fat and other substances from the digestive tract via lacteals. Fluid called chyme.
Defense: Microorganisms and other foreign substances are filtered from lymph by lymph nodes and from blood by spleen.
Components of the Lymphatic System
lymph, a fluid that resembles plasma but contains a much lower concentration of suspended proteins;
a network of lymphatic vessels, which begin in peripheral tissues and end at connections to veins;
an array of lymphoid tissues and lymphoid organs such as lymph nodes, spleen, and thymus scattered throughout the body;
Lymph nodes occur near the body surface in inguinal, axillary, and cervical regions of the body Their two basic functions are:
Filtration – macrophages destroy microorganisms and debris
Immune system activation – monitor for antigens and mount an attack against them
The lymphoid system is organized to provide specific defenses against a wide array of biological hazards and diseases