Clinical Imaging of the Thorax
LEARNING OBJECTIVES
Have an understanding of the range of common clinical imaging techniques available.
Describe the commonly used clinical imaging techniques and recognize the images produced by them.
Discuss the reasons for choosing a suitable imaging technique.
Identify the main features and organs of the thorax on X-ray.
Comment on considerations and suitability of a particular imaging technique/s for imaging any specific part/s of respiratory tract.
Introduction to radiology
Modalities
Radiography
Ultrasound
Radionuclide imaging
CT: Computed Tomogrpahy
MRI: Magnetic Resonance Imaging
PET: Positron Emission Tomography
DSA: Digital Subtraction angiography
SPECT: Single Photon Emission Computed Tomography
OCT: Optical Coherent Tomography → used to image walls of an artery by using infrared light.
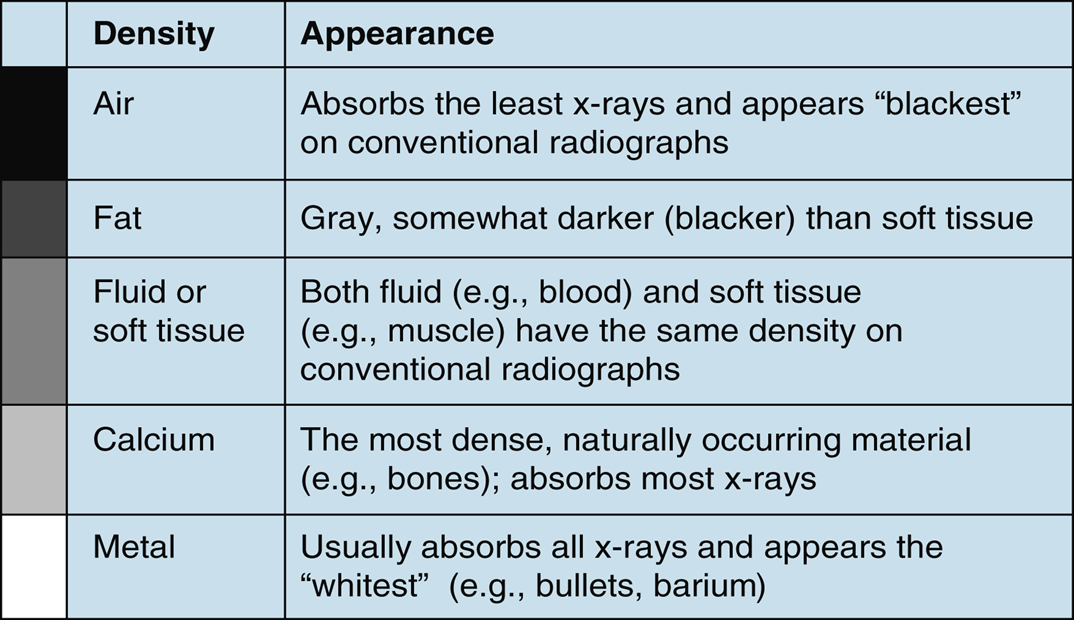
Densities
X-Ray: Beam of energy is aimed at the body part being studied.
Plate behind body part captures the variations of the energy beam after it passes through the various organs of the body, having different densities like skin, bone, muscle and other tissues of the body.
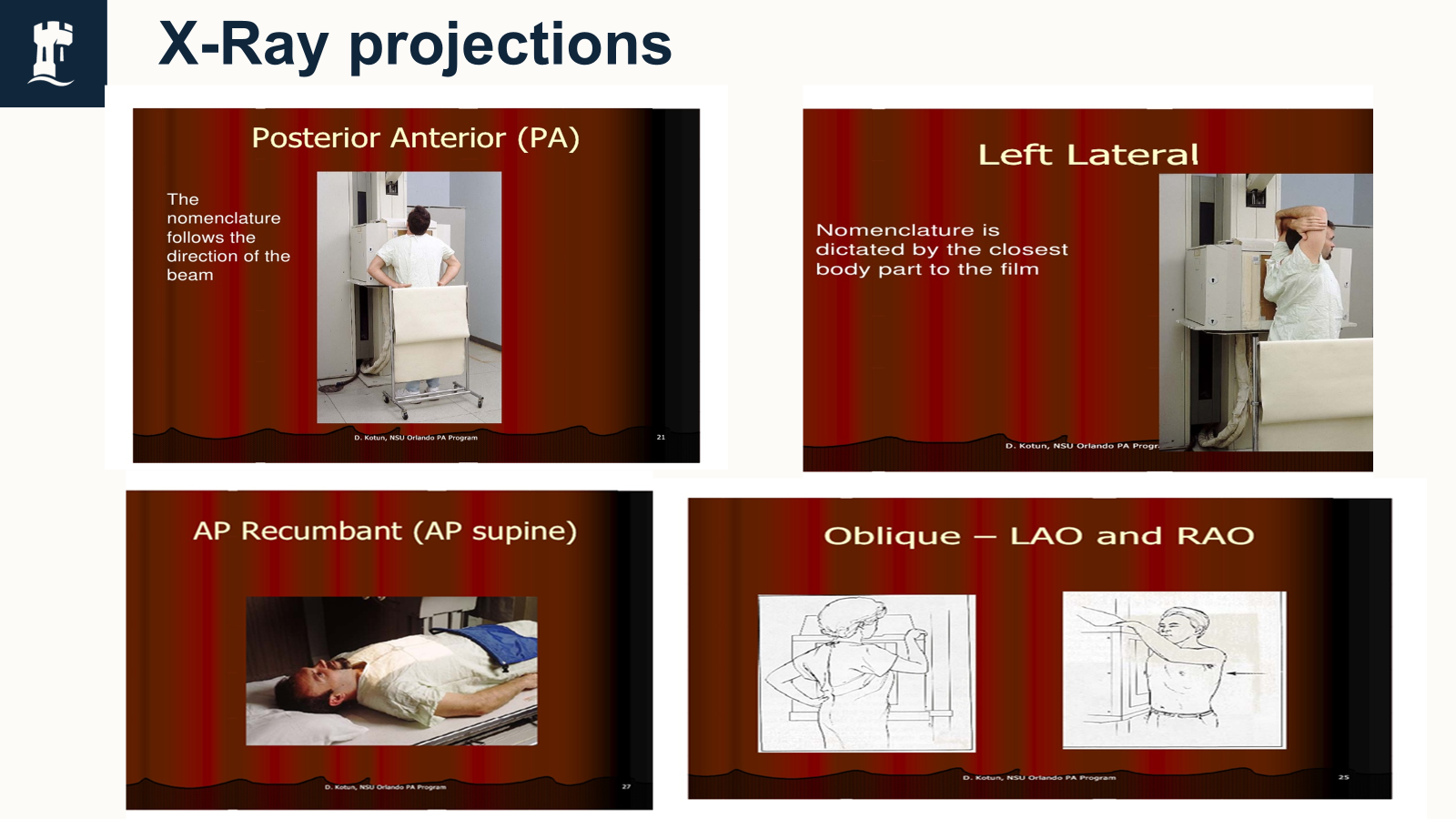
X-Ray techniques
Different views
PA, AP, Lateral, Oblique
More info needed.
Two views preferred
Distance between the X-ray tube and patient is between 30 to 38cm.
Patient needs to be stable.
Scapulae should be retracted.
Advantages
Quick
Cheap
Low-dose radiation
portable
can detect many pathologies
can be done anywhere
Disadvantages
Lack details
Ionizing radiation
Limited range of densities
Difficult to be performed in some patients
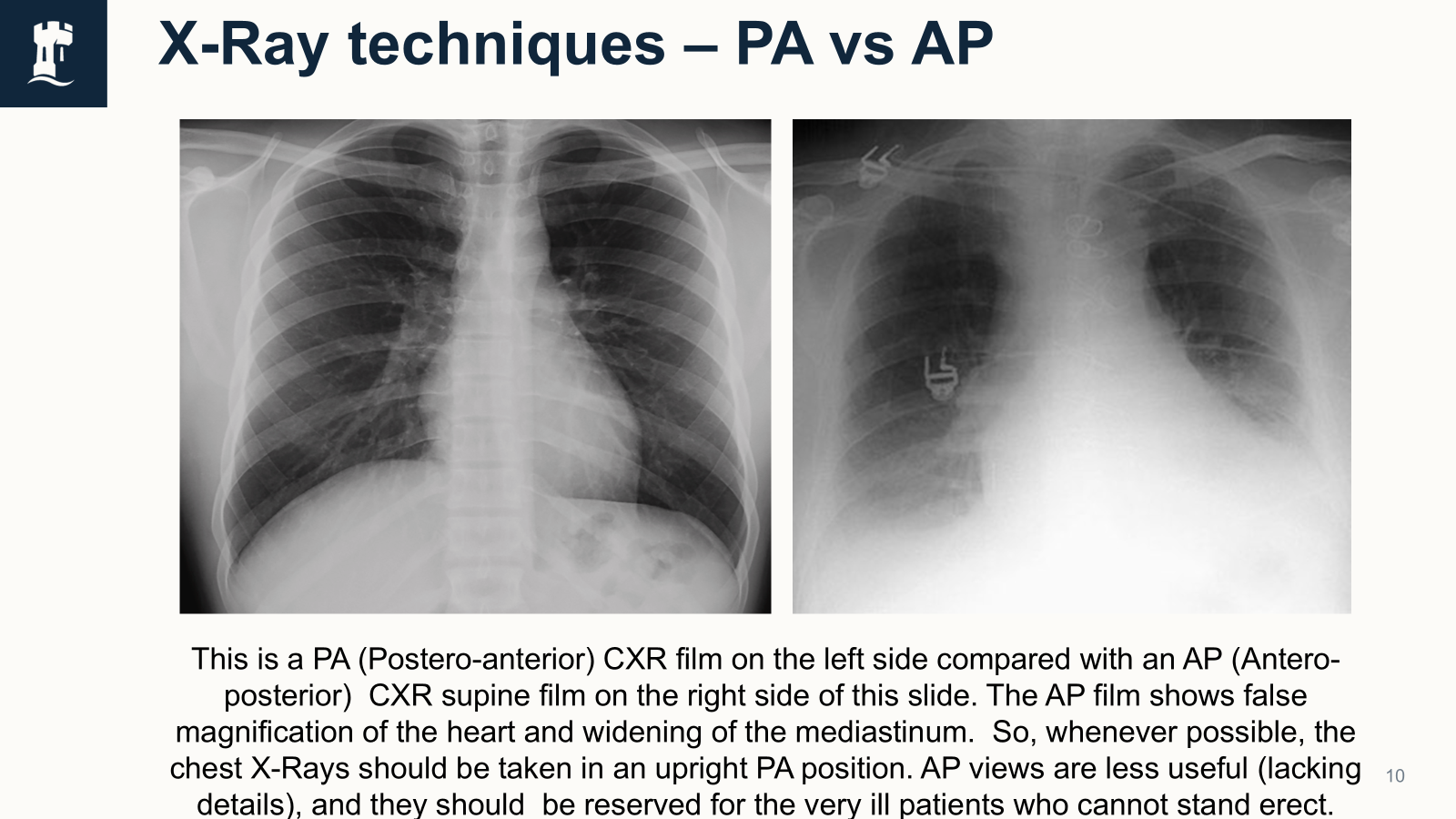
PA VS AP
PA: Standard/conventional projection. Higher quality and more accurately can asses the heart size than AP images. The apparent heart size is nearer to the real size, as the heart is relatively nearer to the real size, as the heart is relatively nearer the detector. The magnification of the heart is also minimized by the use of a narrower beam, produced by the increased distance between the source and the patient.
Both PA and AP views are viewed as if looking at the patient from the front. PA projection is not always possible e.g bed bound patients.
AP: Heart size is exaggerated because the heart is relatively farther away from the detector, and also because the X-ray beam is more divergent as the source is nearer the patient.
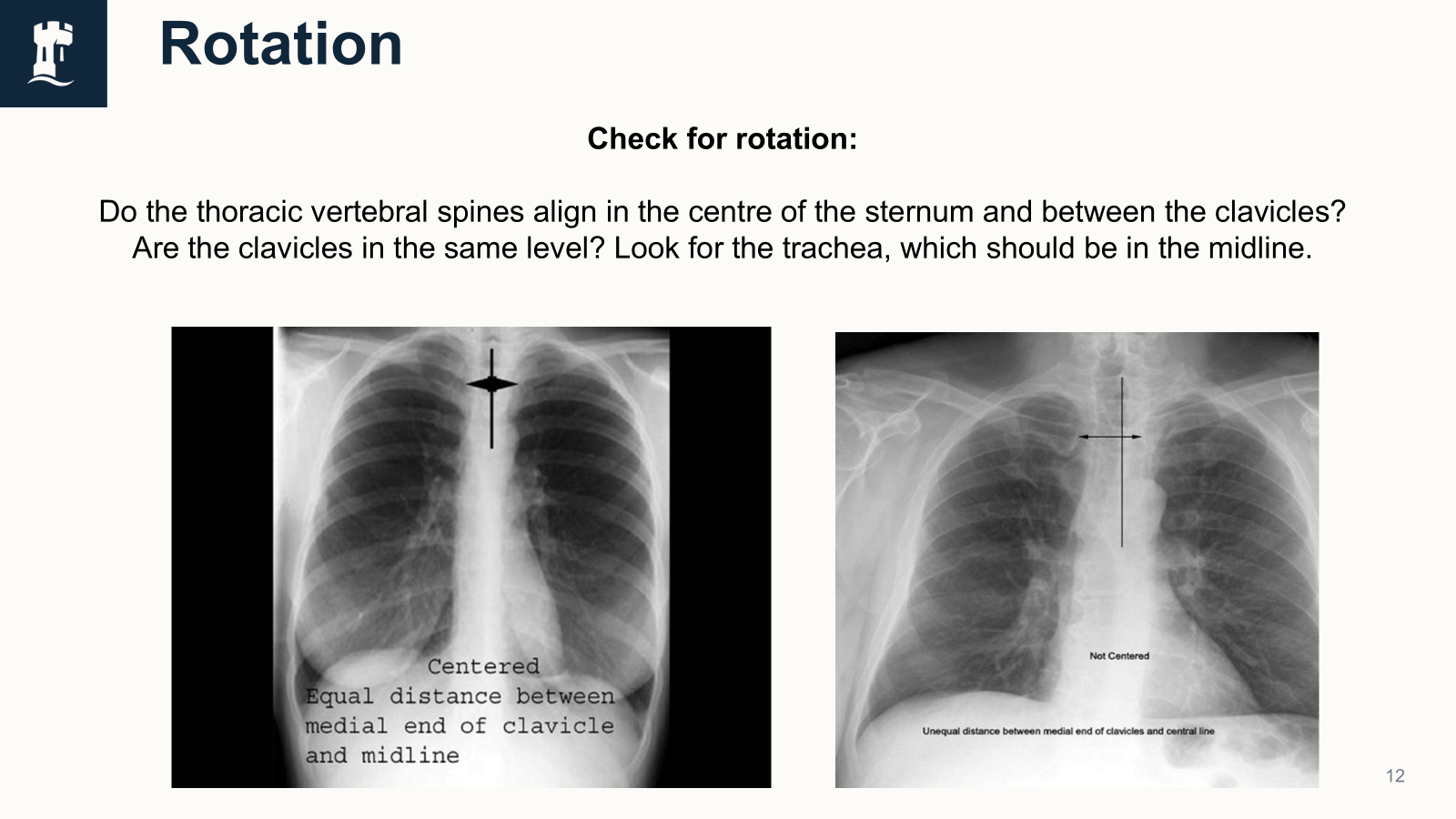
Rotation
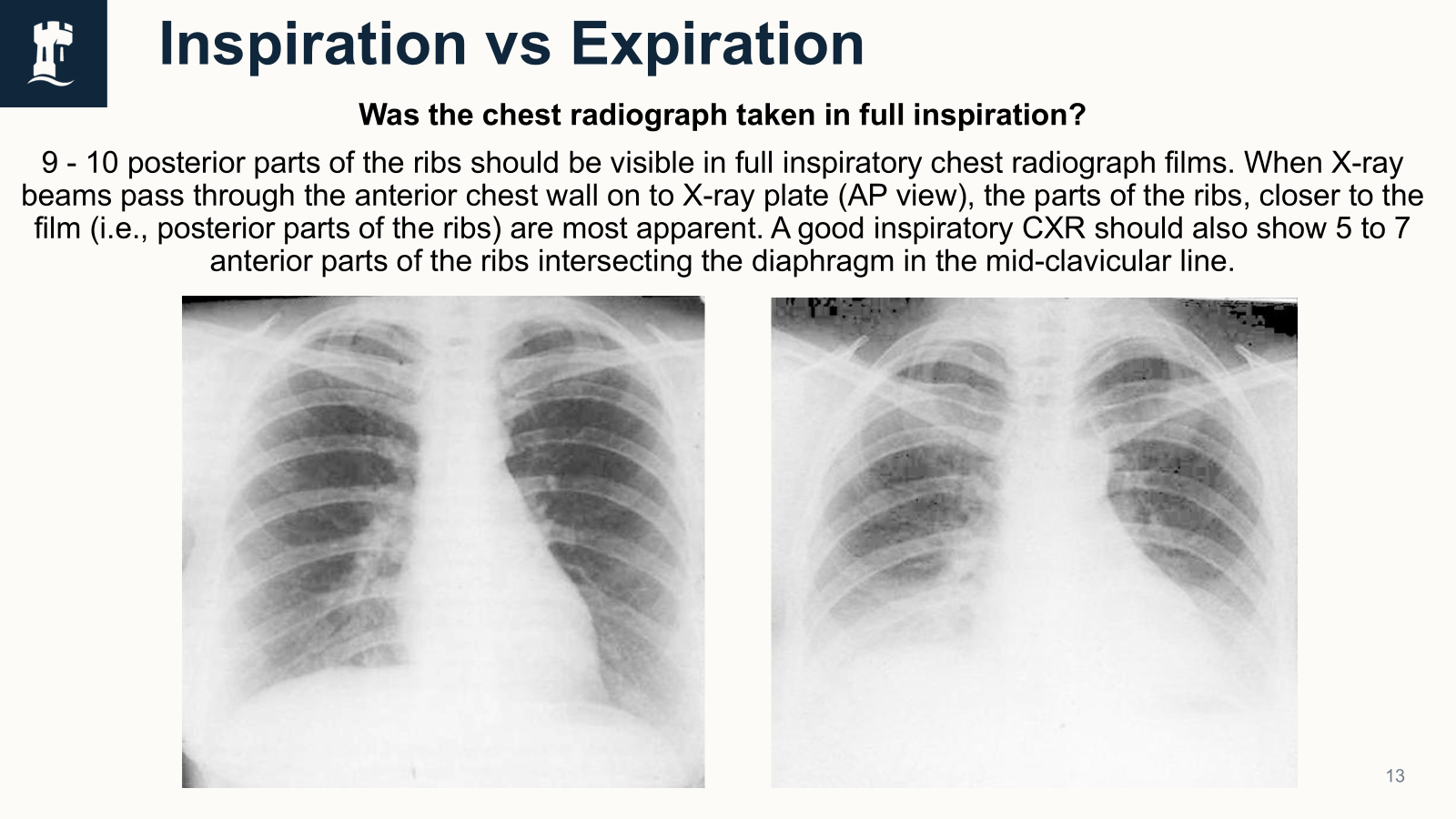
Inspiration vs expiration
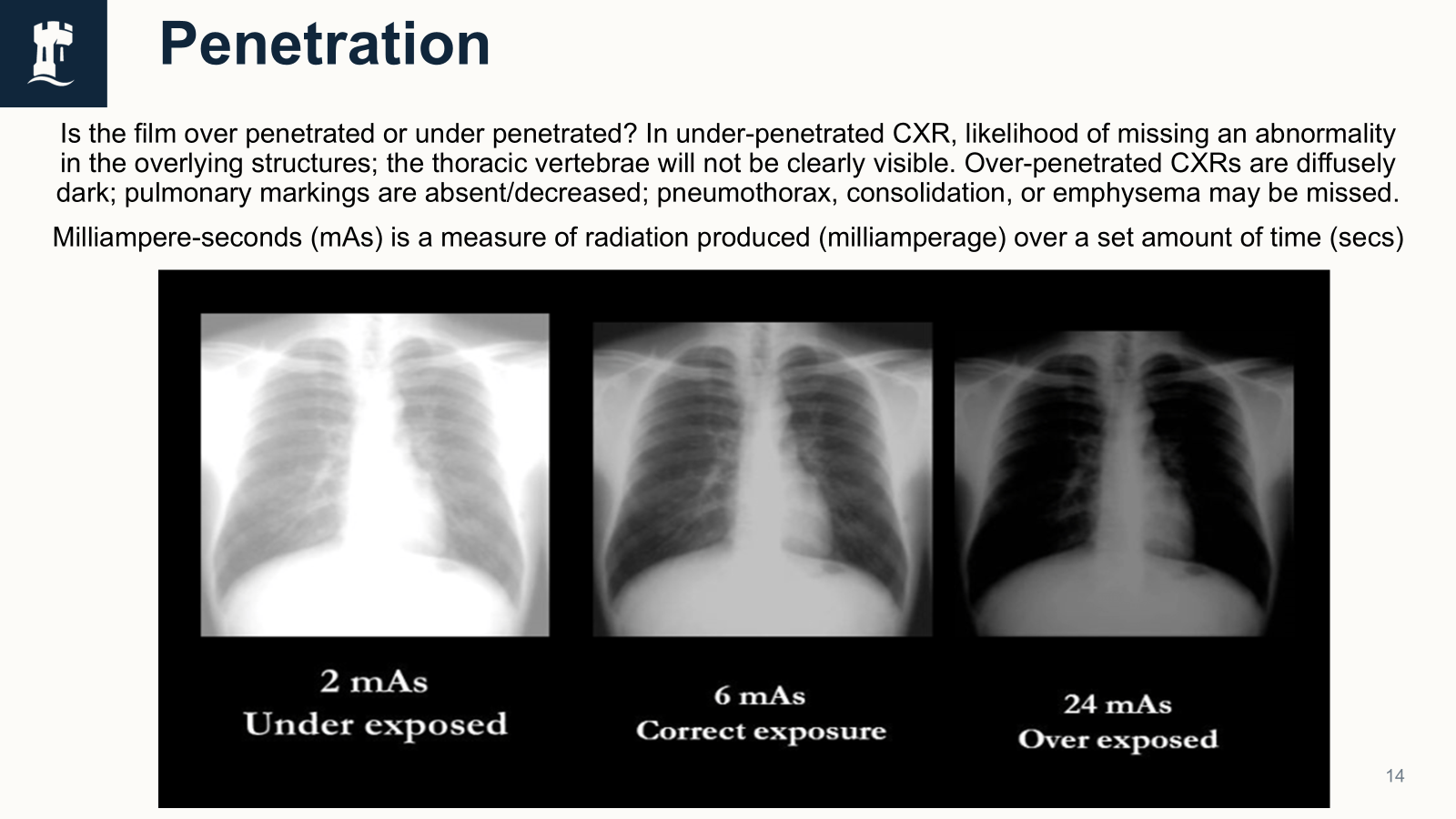
Penetration
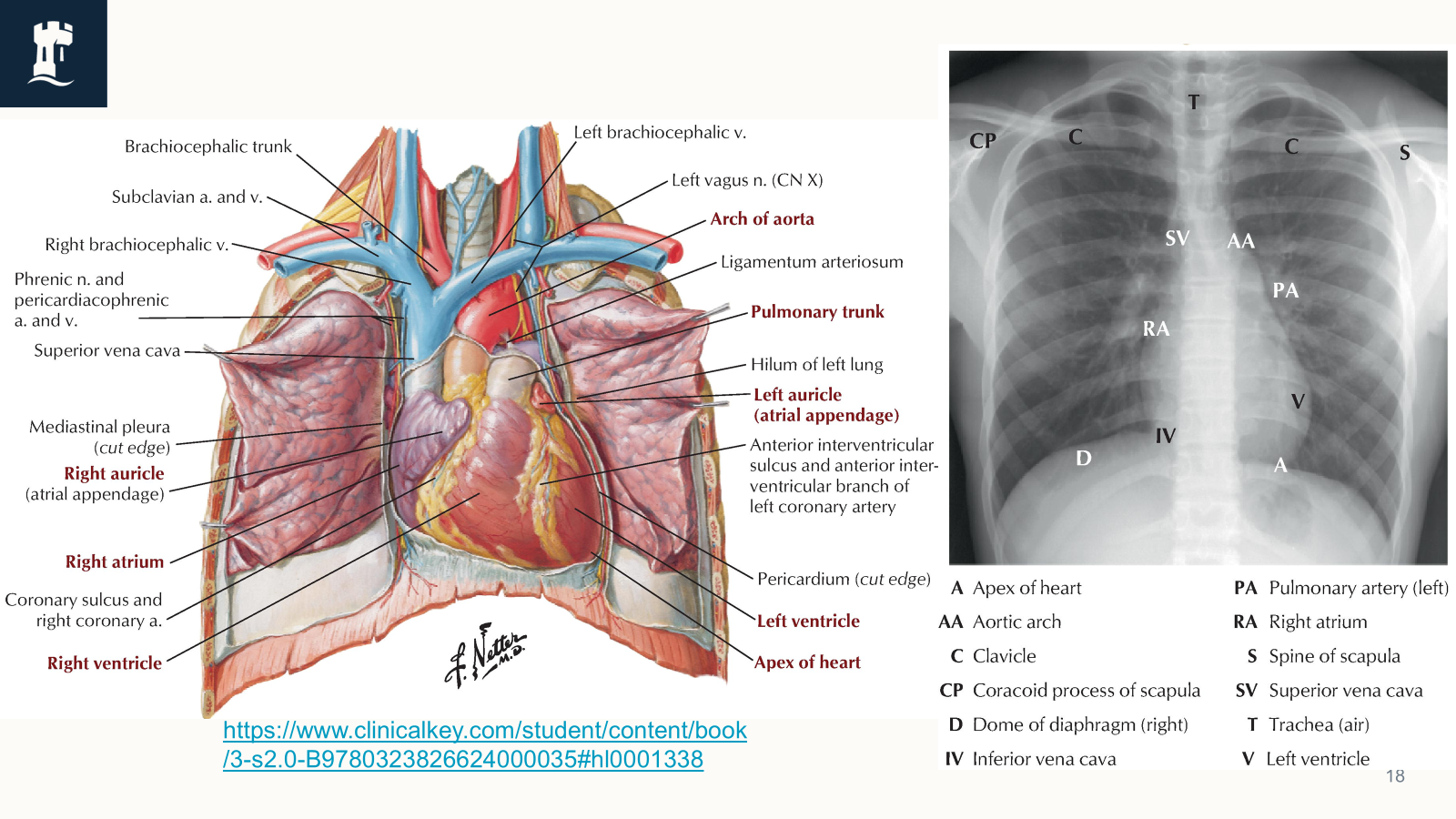
Cardiac Shadow
Size of the cardiac shadow.
Shape of the heart shadow.
Cardiac diameter: If maximum cardiac diameter is >1/2 of maximum thoracic diameter, it suggests an enlarged heart.
Remember: The AP view films make the heart appear larger than it actually is (false magnification of the heart).
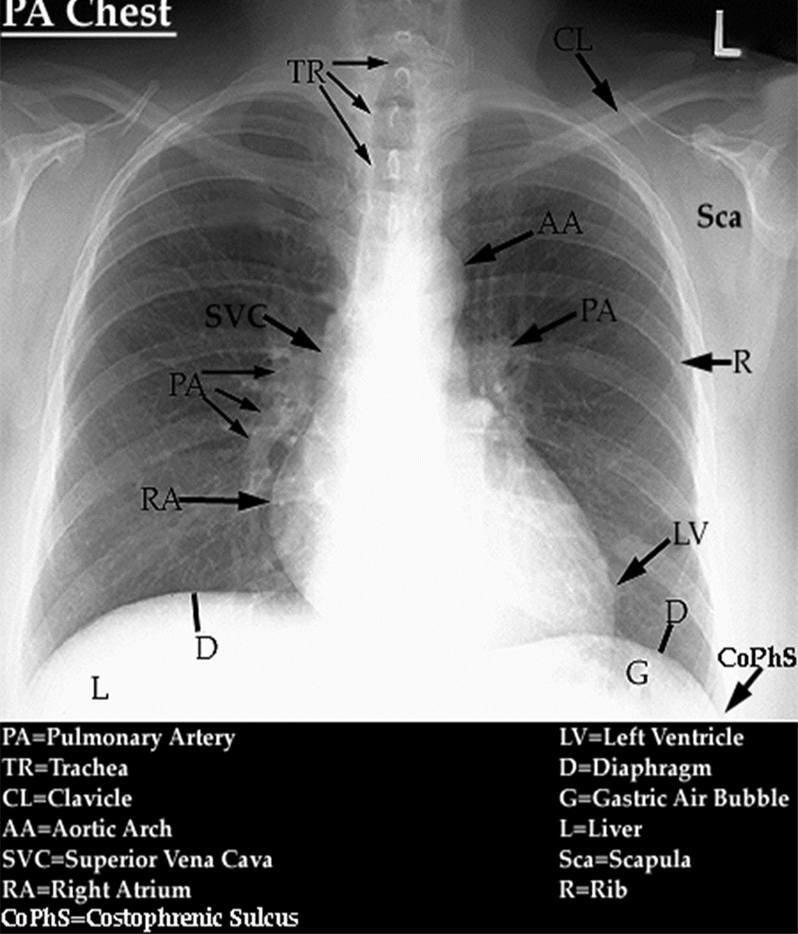
Look also at the following: Aortic arch, Ribs, Clavicles, Scapulae, Costo-phrenic angles, Right atrium, Right ventricle, Apex of left ventricle, Superior and inferior vena cave, Pulmonary trunk and the pulmonary arteries.
Other things to observe
Remember ABCDE
Airways: Trachea, endotracheal tube
Bones: clavicle, ribs, sternum, thoracic vertebrae
Cardiac shadow
Diaphragm: Remember the right hemidiaphragm is slightly higher
Everything else: any wire, tubes, pacemaker, effusions, etc.
Check also:
Apices and hila of the lungs
Identical size, shape, and density of hila, left hilum is higher than right.
Broncho-vascular markings
Behind the heart
Costo-phrenic angles
Diaphragm - look below it
right hemi-diaphragm is higher than the left
Soft tissues
like the breasts, any tumors.
Structures in chest radiographs
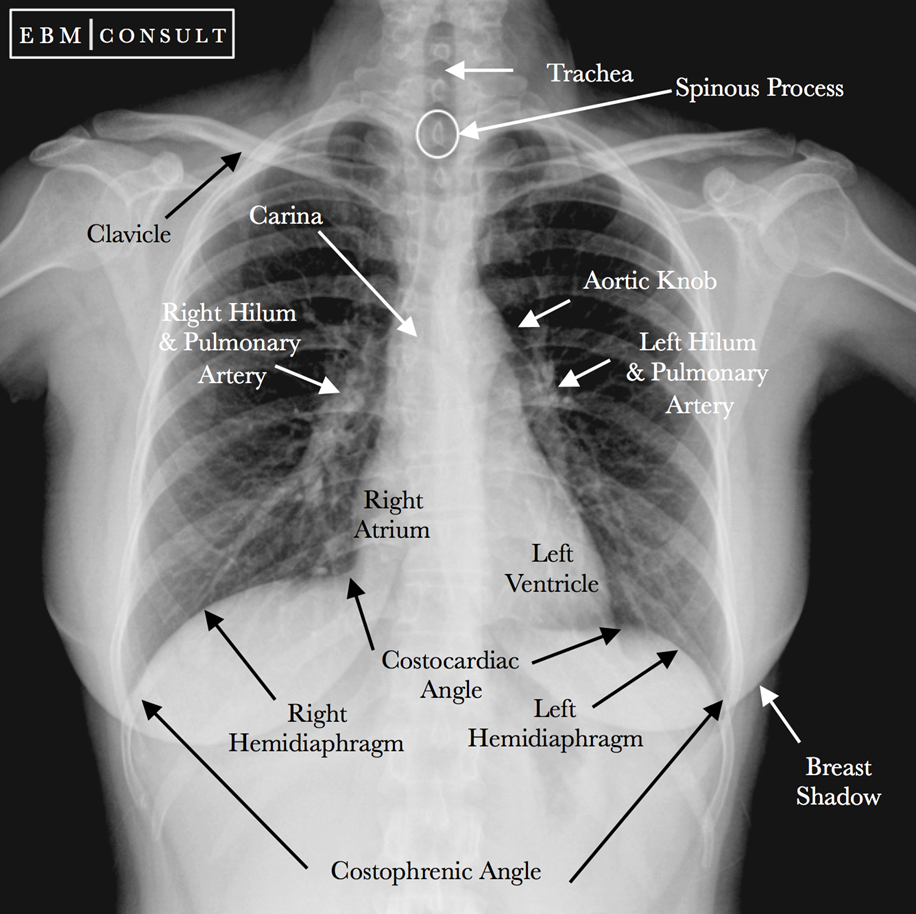
Aortic knob/knuckle should be visualized in the normal chest radiograph around the level of T4/T5 or just lateral to the carina.
The costo-phrenic and the costo-cardiac angles should be sharp and well defined. If they are blunted or lost, there is a chance of presence of any kind of fluid in the pleural cavity.
If free air is found under the right hemi diaphragm, it might be a bowel perforation. It should not be confused with the normal gastric bubble, seen normally under the left hemidiaphragm.
Any deviation of the trachea from the midline could suggest the presence of a mediastinal mass, or presence of tension pneumothorax.
Thoracic Imaging
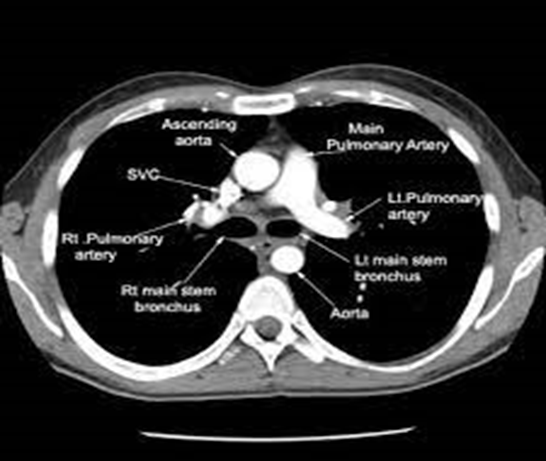
CT scan
A diagnostic imaging procedure; uses X-rays and computer technology to produce internal body images.
Shows detailed images of any part of the body, including bones, muscles, fat, organs and blood vessels.
Can diagnose tumors, investigate internal bleeding or check for other internal injuries.
Also used for tissue or fluid biopsy.
In CT, the X-ray beam moves in a circle around the body. This allows many different views of the same organ and provides much greater detail.
The X-ray information is then sent to a computer that interprets the X-ray data and displays it in two-dimensional form on a monitor.
Newer technology and computer software makes three-dimensional images possible.
Magnetic resonance imaging
Capable of producing both anatomic and physiological data that utilizes the molecular composition of tissues, especially water, to generate images with extraordinary contrast between soft tissues.
MRI uses a very strong magnetic field to manipulate the electromagnetic activity of atomic nuclei that releases energy int he form of radiofrequency signals, which are recorded and them computer-processed to form an image. Clinical MRI scanners utilize the properties of hydrogen nuclei due to their abundance in the human body.
Can assess functions of heart’s chambers, thickness of heart walls, extend of damage from MI, aortic aneurysms, blockages in blood vessels, joint abnormalities etc.
When a person lies inside an MRI machine, the magnetic field temporarily realigns water molecules of the body. Radio waves cause these aligned atoms to produce faint signals, which are used to create cross-sectional MRI images.
The MRI machine can also produce 3D images that can be viewed from different angles.
MRI can check for tumors or other abnormalities in many organs.
CT vs MRI
CT ADVANTAGES | MRI ADVANTAGES |
Less expensive | Produce more detailed images |
Quicker to perform | Do not use radiation so are safer |
Identify internal bleeding, tumors, cancer development and fractures. | Identify pathologies in soft tissues, joints, organs, brain, and heart better than the CT scans |
Whole body of person does not need to enter the CT scanner |
CT DISADVANTAGES | MRI DISADVANTAGES |
Involves introduction of a very small dose of ionizing radiation → could increase chance of developing cancer. | Create loud noises which some people may find stressful. |
Not recommended for pregnant women unless its an emergency. | Medical or metal implants may interfere with the MRI scan e.g hip replacements, pacemakers |
Contrast dye is used during a CT scan which might cause an allergic reaction in some patients. | Those who suffer from claustrophobia may find MRI machines uncomfortable. |
Contrast dye may be used and can cause an allergic reaction. |
Ultrasound Scan
Used to examine internal body structures.
US imaging emits high-frequency sound waves, directed at tissues or organs being examined, and recording the reflected sound or echoes to create and image.
Usually non invasive;
exceptions: trans-vaginal, trans-esophageal
Indications include investigations of the pelvic and abdominal organs, to identify vascular pathologies, monitor fetal age, and diagnose developmental anomalies of fetus during pregnancy.
Other uses - musculoskeletal scans (to check joins like shoulder, hip, elbow), breast scans for tumors.
Abdominal US scans are used to examine the gallbladder, bile ducts, liver, pancreas, spleen, kidneys and large blood vessels. Structures that contain air (such as the stomach and bowels) can’t be examined easily by ultrasound because air prevents the transfer of the sound waves.
Doppler ultrasound, is used to detect speed and direction of blood flow in certain regions of the body, for example, neck arteries and leg veins.
VQ scan
Nuclear medicine scan that uses radioactive material to examine the airflow (ventilation) and the blood flow (perfusion) in the lungs.
Aim is to look for evidence of any pulmonary embolism (PE) in the lungs, that might be fatal, if late untreated.
It is carried out in two parts. Firstly, a radioactive material is breathed in via a nebulizer, and pictures are taken to look at airflow in the lungs by gamma camera.
In second part, a different radioactive material is injected into an arm vein, and more images are taken to see the blood flow in the lungs
The entire imaging process takes 30-60 minutes. There are no side-effects from a VQ scan.
Allergic reactions to radiopharmaceuticals are rare. The radioactive materials used in a VQ scan are not known to interfere with any medications.
PET scan
Positron emission tomography is a nuclear imaging test that can reveal the metabolic or biochemical functions of the tissues and organs.
Uses radioactive drug (tracer) to show both the typical and atypical metabolic activities of the body.
Injected tracer collects into the body areas of higher levels of metabolic/biochemical activities, which pinpoints the disease location.
PET images typically are combined with CT or MRI scans, which are called PET-CT or PET-MRI scans.
PET is used in diagnosis and staging of lung cancer. PET and PET-CT can also assess early metabolic responses to therapy.
PET is an effective way to help discover a variety of conditions, including cancer, heart diseases and brain disorders. Cancer cells show up as bright spots on PET scans as they have a higher metabolic rate than the normal cells. PET scans are useful in detecting cancer, revealing cancer spread, and finding a cancer recurrence.
PET scans can reveal areas of decreased blood flow in the heart and help in early diagnosis.
PET scans are also used to check certain brain disorders like tumors, Alzheimer’s disease etc.
SPECT scan
Single photon emission computerized tomography (SPECT) scan analyses many organs, tissues, and bones of the body. This nuclear imaging test uses a radioactive substance and a special camera to detailed 3D images.
It produces images that show how well blood is flowing in the heart and brain; which areas of the brain are active; or which bones are affected by cancer.
It also helps diagnose certain vascular brain disorders, treat seizure disorders (like epilepsy) by pinpointing the exact areas of seizure activity in the brain.
Areas of bone healing or bone cancer progression usually light up on SPECT scans.
A specific SPECT scan called the Dopamine transporter scan (DaTscan) is used to confirm the diagnosis of Parkinson’s disease, a progressive neurological disorder. It also help evaluate other brain conditions, like dementia or head trauma.
SPECT can check for narrowed cardiac arteries, damaged myocardium, and can detect reduced pumping efficiency of the heart chambers.
Endoscopy
Medical procedure that uses an endoscope to examine the interior of a hollow organ or body cavity by introducing endoscopes directly into the organs.
Many types of endoscopies depending on the site. Patient may be fully conscious or anesthetized during procedure.
Types:
To inspect the esophagus, stomach and duodenum → esophagogastroduodenoscopy
Small intestine → enterscopy
Large intestine → colonoscopy
Bile duct and the gall bladder → cholecystoscopy
Endoscopic retrograde cholangiopancreatography (ECRP)
Rectum or sigmoid colon → Proctoscopy or sigmoidoscopy
Respiratory tract
Nose → Rhinoscopy
URT ) → Laryngoscopy
LRT → Bronchoscopy
Ear → otoscopy
Urinary tract → cystoscopy
Female reproductive system
Cervix and vagina → colposcopy
uterus → hysteroscopy
Closed body cavities
abdominal, peritoneal, pelvic cavity → laparoscopy
interior of a joint → arthroscopy
organs of the chest → thoracoscopy or mediastinoscopy
Orthopedic surgeries
Remocing bursae → bursectomy
Need to know Disease Presentations
Pleural effusion
Collection of fluid in pleural cavity, caused by many pathological conditions, which overwhelm the pleura’s ability to reabsorb the fluid that gathers in the lowest part of chest.
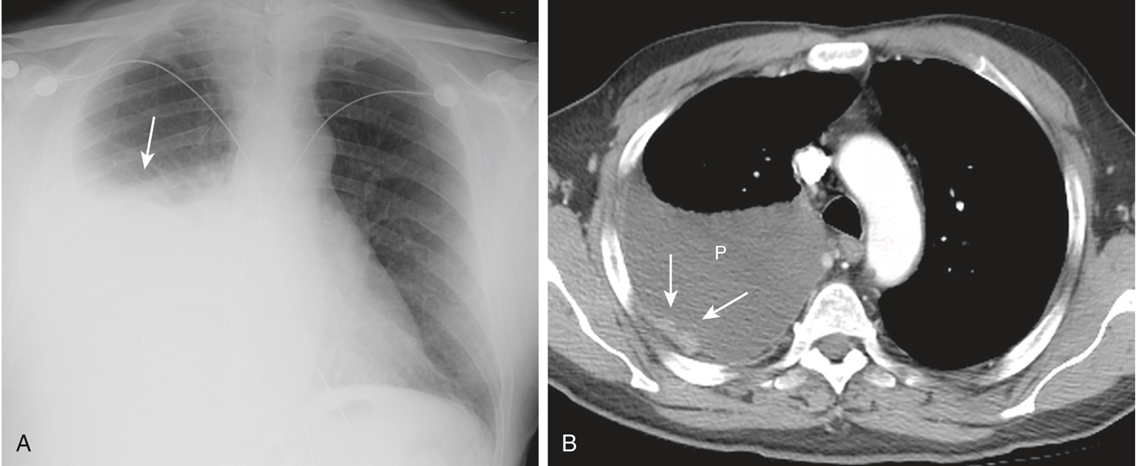
CXR findings
If the patient is upright when the X-ray is taken, then fluid will surround the lung base forming a ‘meniscus’, a concave line obscuring costophrenic angle, heart borders, and the hemidiaphragm.
In supine patient, this sign is not seen. Loss of the costophrenic angle, increased density of affected hemithorax, pseudo-elevation of diaphragm, loss of lower lobe vessels are seen.
If the patient is upright when the X-ray is taken, then fluid will surround the lung base forming a ‘meniscus’, a concave line obscuring costophrenic angle, heart borders, and the hemidiaphragm.
In supine patient, this sign is not seen. Loss of the costophrenic angle, increased density of affected hemithorax, pseudo-elevation of diaphragm, loss of lower lobe vessels are seen.
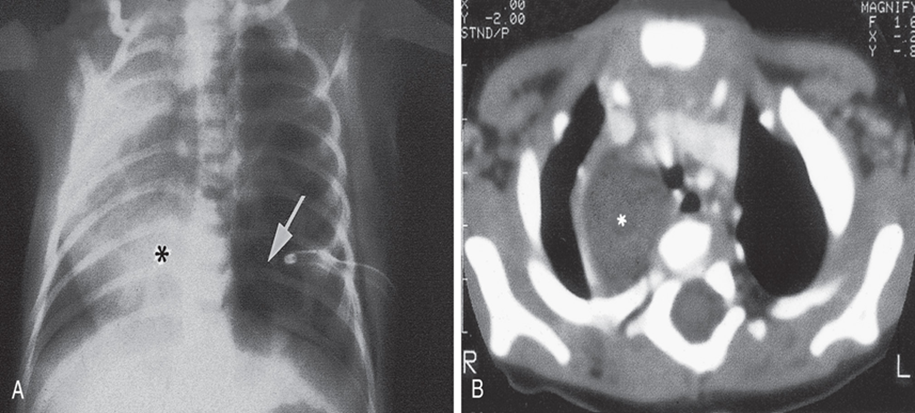
CHEST CT FINDINGS
A large pleural effusion appears as a sickle-shaped opacity in most dependent part of the thorax with lateral upward sloping of a meniscus-shaped contour. The diaphragmatic contour is partially or completely obliterated, depending on the amount of the fluid (silhouette sign).
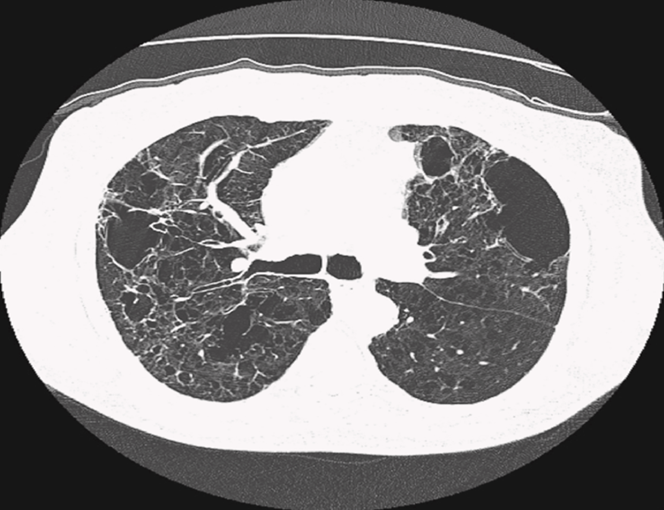
Emphysema
Abnormal permanent enlargement of airspaces distal to the terminal bronchioles accompanied by destruction of the alveolar wall. It is best evaluated on CT.
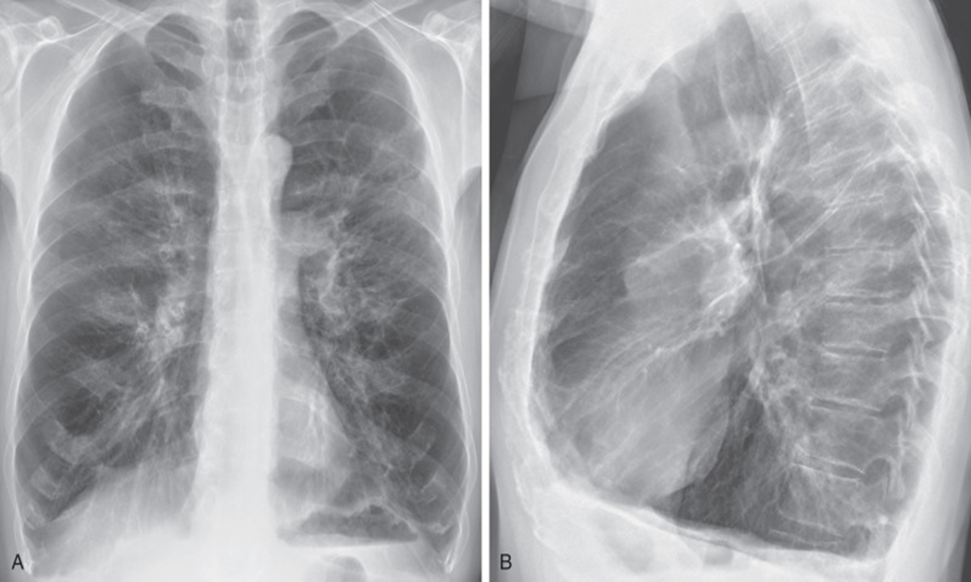
CXR Findings
Hyperinflated lungs with low flattened hemidiaphragm, increased radiolucency (hyperlucency) of the lungs, increased retrosternal airspace, increased AP chest diameter, vertical heart, widely spaced ribs, sternal bowing, and blunting of the costophrenic angles.
CT Scan Findings
Appearance of dark or low attenuation areas, overinflation/damage of air sacs. Centrilobular emphysema shows up as small, round dark areas within the central part of lung lobules. Pan lobular shows uniformly distributed areas of low attenuation throughout lungs.
Pneumothorax
Presence of air between parietal and visceral pleurae (pleural cavity), caused commonly by trauma or injury. If not caused by trauma, it is known as spontaneous. When this air/gas constantly increases with resulting compression of the mediastinal structures, it is known as a tension pneumothorax.
Chest Radiographic findings
Visible visceral pleural edge seen as a very thin, sharp white line. No lung markings are seen peripheral to this line. Peripheral space is radiolucent compared to the adjacent lung. Lung may collapse. Mediastinum shift usually seen in tension pneumothorax.
Chest CT Findings
Rims of gas (black) seen around edges of the lung which may track up the fissures. Small pneumothoraces, pneumomediastinum, and blebs can be detected on chest CT.