DMD 24. Introduction to Circulatory Disorders
Learning Outcomes
By the end of the lecture, you should be able to:
Describe vascular insufficiency and define key terms:
Ischaemia: Impaired blood flow or perfusion to tissues, leading to nutrient deprivation.
Infarction: Tissue death due to ischaemia.
List the main causes of ischaemia.
Describe thrombosis and Virchow’s triad.
Define embolus and describe the implications of thrombo-embolic events.
Importance of Circulatory Disease
Significance:
Major cause of morbidity and mortality.
Poses a massive burden on the NHS.
Dental Implications:
Patients with circulatory issues may require special dental considerations.
Key Terms to Know
Ischaemia/ Vascular Insufficiency -Vascular occlusion leading to decreased blood flow. ischaemia - Impaired blood flow depriving tissues of oxygen/nutrients
Infarction -Cell death (necrosis) resulting from ischaemia
Haemostasis
Thrombosis -A solid mass of blood constituents formed in the vascular system during life
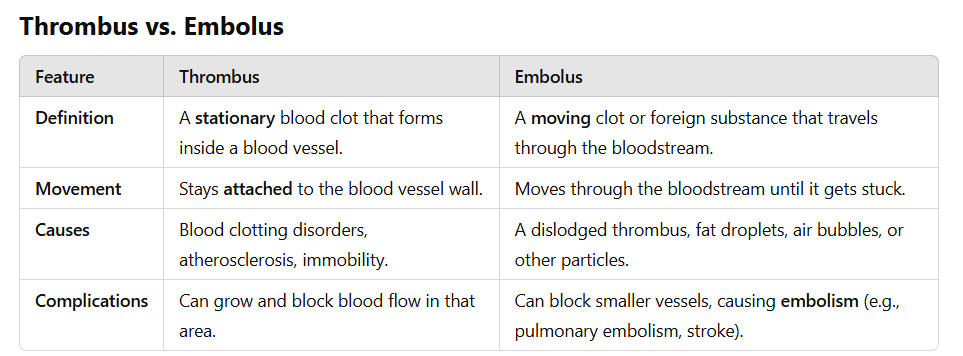
Embolism -blockage of a blood vessel by a foreign substance, such as a blood clot,
Atheroma -a fatty deposit that builds up in the walls of arteries
Normal Circulation
Vascular System:
Comprises the heart and vessels, delivering blood to organs/tissues and returning it to the heart.
Lymphatic System:
Passive drainage system that returns extracellular fluid to the vascular system.
Anatomy of Blood Vessels
Tunica Intima
Endothelium, subendothelium, internal elastic lamina.
Tunica Media
Smooth muscle layer, external elastic lamina.
Tunica Adventitia
Composed of collagen 1, vasa vasorum, nervi vasorum.
Complications of Blood Vessels
Issues:
Blocked or occluded (internally, externally, within the wall).
Dilated
dissected/ruptured
inflamed
abnormal growths (tumors hemangioma, congenital defects)-present from birth
Vascular Insufficiency
Definition: Vascular occlusion leading to decreased blood flow.
can affect both arterial and venous structure
effects depends on tissue involved, rate of occlusion, collateral blood suppy present
Ischaemia: - progressive occulsion, reversible
Impaired blood flow depriving tissues of oxygen/nutrients
may be reversible based on duration and metabolic demands of the tissye
Infarction - irreversible
Definition:
Cell death (necrosis) resulting from ischaemia; effects are irreversible and tissues vary in their repair abilities. elicit an inflammatory response
Appearance of Infarcts
Types of Infarcts:
Red Infarcts:
Caused by venous occlusion, found in loose tissues (e.g., lung), and areas with dual circulation.(lung and liver)
Pale (White) Infarcts:
Usually occur in solid organs (e.g., heart, spleen, kidney) with single blood supply.
Causes of Ischaemia/Vascular Insufficiency
Factors Leading to Ischaemia:
Vascular blockage, the occlusion of varying locations (internally, externally, or within the wall).
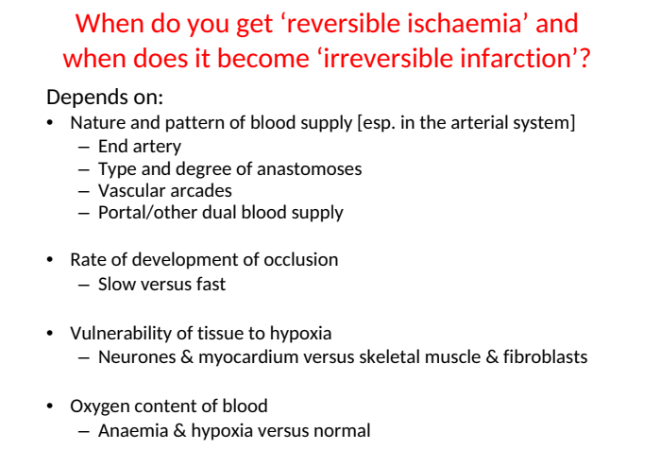
Irreversible infaction depends on and pattern of occlusion, collateral blood supply, tissue vulnerability to hypoxia.
Thrombus Formation
Definition:
A solid mass of blood constituents formed in the vascular system during life
Thrombus formed of alternating layer of platelet, fibrin and RBC
on damage endothelial wall with a platelet plug
grow in the direction of blood flow
pale deposit - platelet
dark deposit - dark
Lines of Zahn - alternating bands
Embolus can cause renal infaction
Distinction from Clots:
Clot: solid mass occurring outside the vascular tree or after death
Virchow’s Triad - 3 predisposing factors
Components:
Changes in the intimal surface of the vessel. (endothelial injury)
Changes in blood flow pattern (e.g., turbulence, stasis).
Changes in blood constituents (e.g., hypercoagulability).
arteries - atheroma
veins - stasis venous return
Changes to Endothelial Surface
Intima is only one cell thick, usually resist thrombus formation → damage expose extracellar matrix proteins and glycoprotein → inducing thrombosis
Factors Causing Damage:
Haemodynamic forces, hyperlipidemia (fat build up in artery) , cigarette smoke, immune complex deposition, infections, trauma, chemicals, infarction.
Changes in Blood Flow
Turbulence in arteries and stasis in veins contribute to thrombus formation.
Changes in Blood Constituents
Condition:
Blood may have increased susceptibility to coagulation (hypercoagulable state). By increase coagulation protein, platelet aggregation. Decreae anti thrombotic
seen in conditions like
polycythaemia - increase RBC
Burns - loss of plasma
thrombocythaemia - increase platelet
Myeloma - increase plasma protein in bone marrow
Clinical Implications of Thrombosis
Effects:
Variability influenced by the vascular system involved, speed of development, collateral flow availability, and tissue sensitivity to ischaemia.
 Knowt
Knowt