Pharmacology Test 1
Day 1
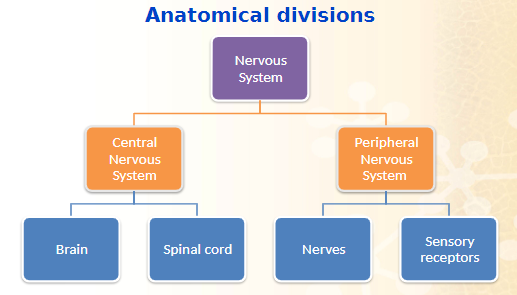
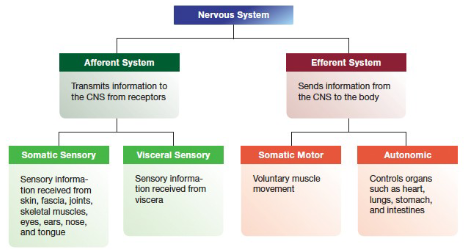
- Afferent System: transmits information to the CNS from Receptors
- Somatic Sensory: Sensory Information received from skin, fascia, joints, skeletal muscles, eyes, ears, nose, and tongue
- Visceral Sensory: Sensory Information received from viscera
- Efferent System: Sends information from the CNS to the body
- Somatic Motor: Voluntary muscle movement
- Autonomic: controls organs such as heart, lungs, stomach, and intestines
PNS - Efferent System
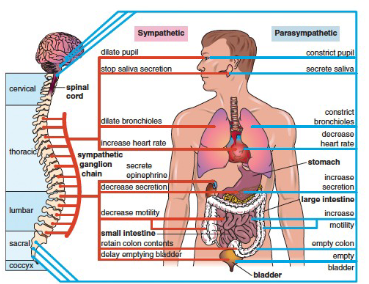
- Autonomic Nervous System: Involuntary activities: respiration, circulation, digestion, body temperature, metabolism, blood glucose, sweating
- Somatic nervous system: Acetylcholine only neurotransmitter between CNS and skeletal muscles
CNS and PNS Primary Neurotransmitters
CNS
- Acetylcholine (Ach)
- Dopamine
- Norepinephrine
- GABA (gamma-aminobutyric acid)
- Glutamate
- Serotonin
PNS
- Acetylcholine (Ach)
- Norepinephrine
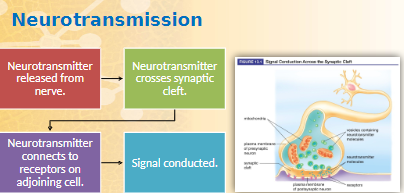
Nervous Tissue
- Chemical Signal is received on cell body and dendrites
- Chemical Signal is converted to electrical signal or
- Impulse travels down axon to the axon terminal
- Axon terminal releases neurotransmitters
Nervous System
- Acetylcholine: stimulates skeletal muscle, inhibits cardiac muscle, inhibits and excites smooth muscle and glands (CNS & PNS)
- Gamma-Aminobutyric Acid: Primary inhibitory neurotransmitter in the brain; can impact muscle tone (CNS)
- Dopamine: Inhibitory role; important in cognition, motivation, behavior, mood
- Epinephrine: Effects in thalamus, hypothalamus, spinal cord
- Norepinephrine: Modulates sympathetic part of the autonomic nervous system
- Serotonin: Functions related to sleep, appetite, cognition, mood
- Glutamate: Excitatory role; promotes cognitive function; most common neurotransmitter in the brain
- ACh and GABA
- ACh acts on receptors in smooth and cardiac muscle, skeletal muscle, and exocrine glands
- ACh receptors blocked by anticholinergics
- GABA regulates message delivery system of the brain
- Dopamine, Epinephrine, and Norepinephrine
- Dopamine acts on receptors in the CNS and kidneys
- Epinephrine acts on cardiac and bronchodilator receptors
- Norepinephrine acts on alpha and beta receptors
- Serotonin and Glutamate
- Serotonin acts on smooth muscle and gastric mucosa
- Causes vasoconstriction which decreases blood flow
- Emotional responses: depression, anxiety
- Glutamate may be crucial to some forms of learning and memory
Types of Receptors
- Alpha: vasoconstriction, raises blood pressure
- Beta-1: increases heart rate and contrastive force of the heart
- Beta-2: influences bronchodilation
Neurotransmitter mechanism of action
- Response of various adrenergic receptors to epinephrine/norepinephrine
- Alpha receptors
- Constriction of blood vessels
- Decongestion
- Beta-1 receptors
- Increases heart rate and contrastive force of heart
- Beta-2 receptors
- Dilation of bronchial tubes and blood vessels
- Drug Effects on the receptors (Nervous System)
- Neurotransmitter binding causes cell membrane to be more permeable to various ions.
- Activate enzyme systems that promote chemical reaction
- Blocking, preventing transmitters from binding to receptors
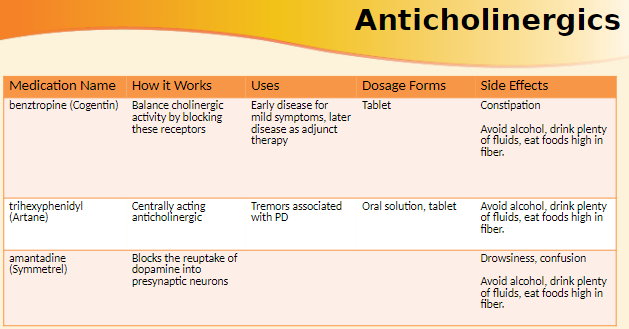
- Anticholinergics
- Side Effects of Anticholinergics
- Decreased GI motility (constipation)
- Decreased sweating
- Decreased urination
- Dilated pupil and blurred vision
- Dry eyes
- Dry mouth
Drugs for Central Nervous System Disorders
Seizure Disorders
- Seizure: Results from excessive firing of a small number of neurons with spread to adjacent neurons
- Conscious periods and loss of control over movements or distortion of the senses
- Convulsion: An involuntary contraction or series of contractions of voluntary muscles
- Seizures and convulsions are not interdependent
- Epilepsy: Neurologic disorder characterized by sudden and recurring seizures
- Involves disturbances of neuronal electrical activity that \n interfere with normal brain function
- All epilepsy patients have seizures but not all patients with \n seizures have epilepsy.
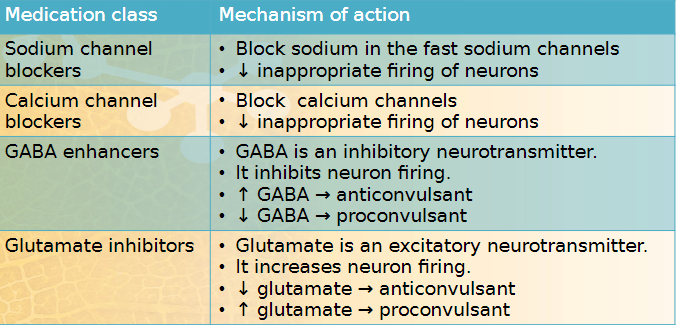
- Seizures: Factors which influence the firing of neurons \n • Positively charged ions increase firing. \n • Negatively charged ions inhibit firing. \n •Glutamate, an excitatory neurotransmitter, increases firing. \n •GABA, an inhibitory neurotransmitter, decreases firing. \n • Enzymes control neurotransmitter levels \n • Disruption in enzymes = disruption of neurotransmitters
- Causes of seizures \n • Alcohol or drug withdrawal/use \n • Epilepsy \n • High fever \n • Hypoglycemia and hyperglycemia \n • Infection \n • Brain tumors \n • Trauma or head injury
- Symptoms vary from staring to unconsciousness
Partial Seizures (focal)
- localized in a specific area of the brain
- almost always results from injury to cerebral cortex
- occurs in about 65% of people with epilepsy
- can progress to generalized seizures
Generalized Seizures
- Involves both hemispheres of the brain, no specific location
- Four types
- tonic-clinic
- absence
- myoclonic
- atonic
Types of Seizures
- Partial Seizure in a specific hemisphere
- Simple partial seizure: twitching and sensory hallucination with no loss of consciousness (focal motor)
- Complex partial seizure: blank stare, post seizure amnesia with impaired consciousness (psychomotor)
- Generalized Seizures
- Tonic-Clonic seizure: muscle rigidity followed by muscle jerks with shallow breathing, loss of bladder control, excess salivation (Grand Mal)
- Tonic: body becomes rigid, patient may fall, lasts a minute or less
- Clonic: starts with muscle jerks, may be accompanied by shallow breathing, loss of bladder control, and excess salivation; lasts a few minutes
- Status Epilepticus: continuous tonic-Clonic convulsions, high fever, lack of oxygen; with or without loss of consciousness
- lasts at least 30 minutes
- high fever and lack of oxygen that can cause brain damage or death
- Absence seizure (petit Mal): interruption of activities by black stare, rotating eyes, uncontrolled facial movements, rapid eye blinking, twitching or jerking of an arm or leg
- no generalized convulsions
- 30 seconds or less
- typically stops at the age of 10 or develop tonic-Clonic
- Myoclonic seizure: occurs with sudden, massive brief muscle jerks which may throw patient down or nonpassive, quick jerks of the arms, hands, legs, or feet: consciousness not lost
- can occur during sleep
- Ten percent of patient who suffer from status epilepticus die regardless of treatment
- Two goals of Antiepileptic Therapy
- Seizure control or lessen the frequency
- Prevent emotional and behavioral changes that may result from seizures
- About 30% of patient do not comply due to side effects such as sedation and loss of cognitive processes
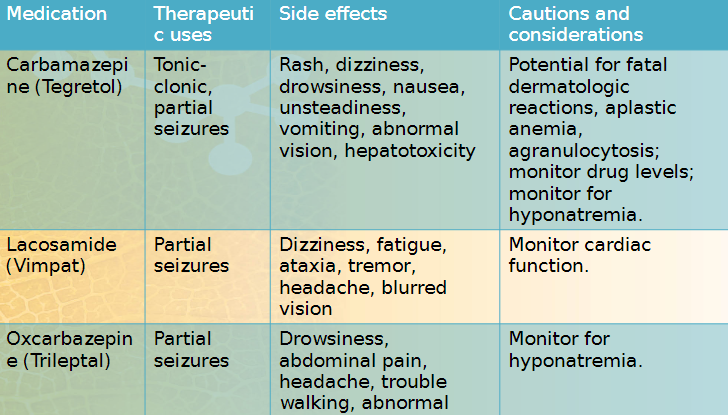
Antiepileptic Drug Therapy
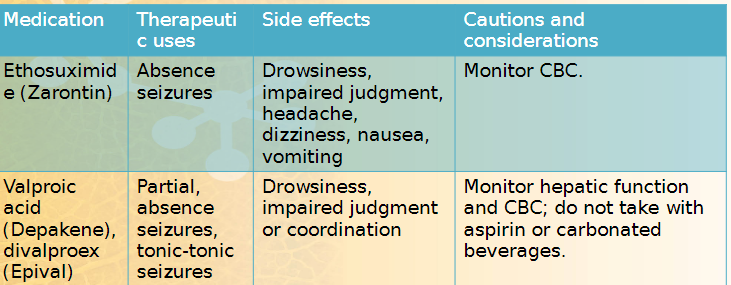
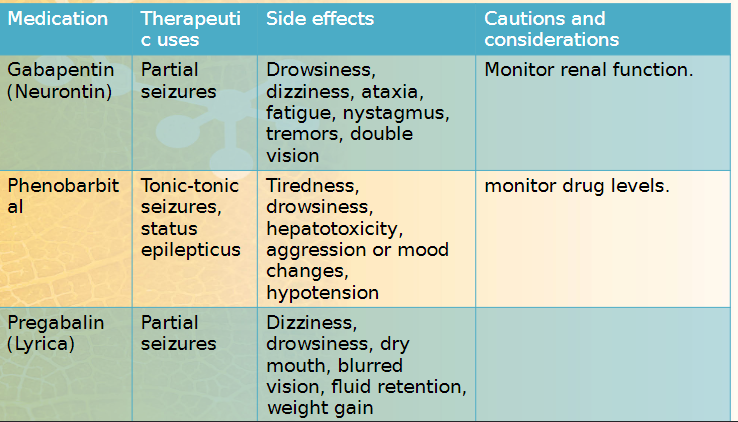
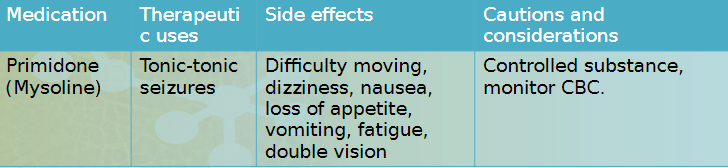
- Principles of treatment- Different seizure types require different drugs
- Initiate monotherapy at a low dose.
- Increase dose gradually over 3-4 weeks
- Monitor plasma concentrations, must be maintained at steady therapeutic levels
- If insufficient response, polytherapy can be considered (severe cases).
- Periodically evaluate continued need for therapy.
- Monitor for drug interactions.
- Watch for “dispense as written” on prescription.
- Dispense with medication guide.
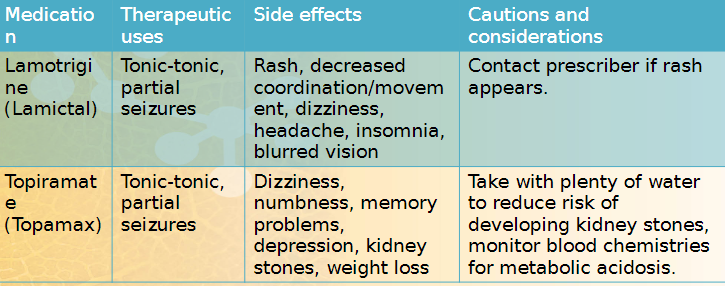
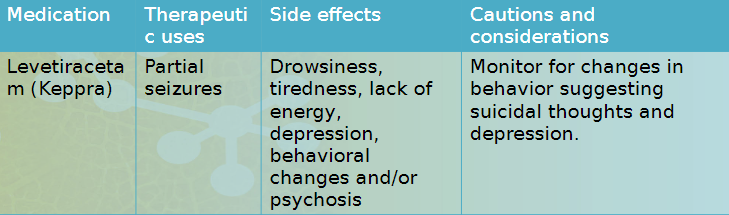
Newer drugs are seizure-specific
high potential for drug interactions
Anticonvulsants have narrow therapeutic ranges
prescribers often write for the brand name medications
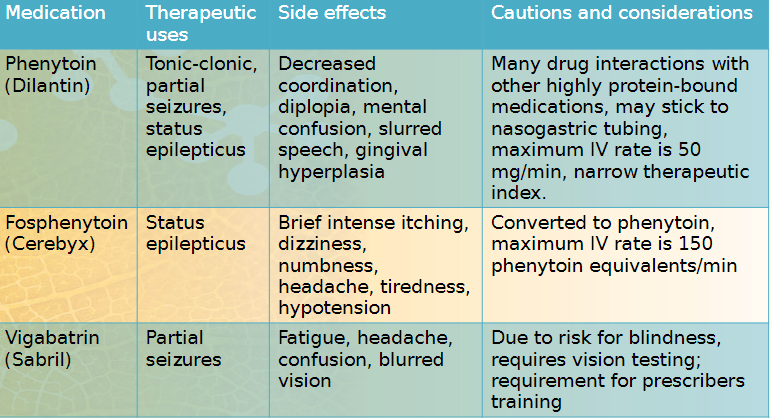
Barbiturates
- Sedatives with anticonvulsant action
- inhibit nerve impulse conduction and depress neurons in the brain
- ex. Phenobarbital
- oldest drug in the class
- still used
- sedation
<<more drugs Depakene and Epival are not interchangeable; Sabril is last chance drug<<
Benzodiazepines
- many clinical uses
- potential for abuse
- one use is as an anticonvulsant – acts on receptors in the brainstorm
- ex. diazepam
Nervous System
Parkinson’s Disease
Characterized by muscular difficulties and postural abnormalities
Signs
- tremors while resting, rigidity, akinesia
- manifests as poor posture control. shuffling gait, loss of overall muscle control
Cause
- Alterations in the extrapyramidal system which controls movement
- Imbalance between the neurotransmitters dopamine and Ach
- Part of the CNS that controls motor activities
- Made up of the basal nuclei (basal ganglia)
Chronic, degenerate condition
- part of the CNS that controls motor activities
- made up of basal nuclei (basal ganglia)
Most common extrapyramidal disease
Usually affects people over 60
Parkinson has no definitive test, diagnosed by symptoms
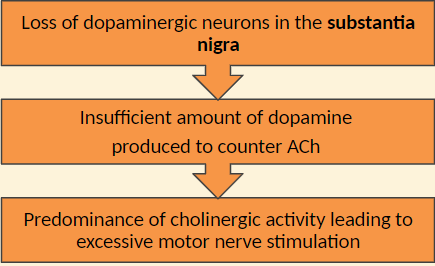
For normal muscle movement to be performed, 2 main neurotransmitters must be in balance
- dopamine (inhibitor)
- acetylcholine (stimulator)
In Parkinson disease, there neurotransmitters are not in balance
In the substania nigra, insufficient dopamine is released to counteract effects of Ach
This causes excessive motor nerve stimulation
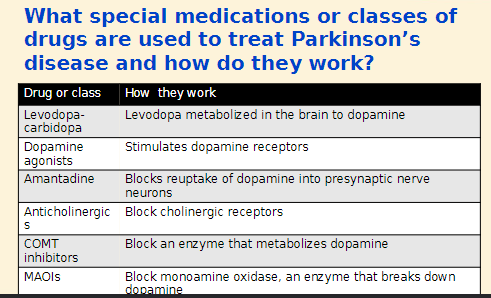
Drug Therapy
- Improves functional ability, clinical status, temporary remission
- Does not alter disease process
- side effects may necessitate numerous medication changes
Treatment Issues
- tolerance develops easily
- need larger doses
- more side effects
- Drug holiday
- lower dose required
- less side effects
- may be taken off completely for a couple weeks so it stays effective
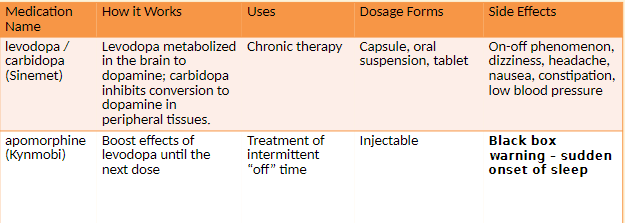
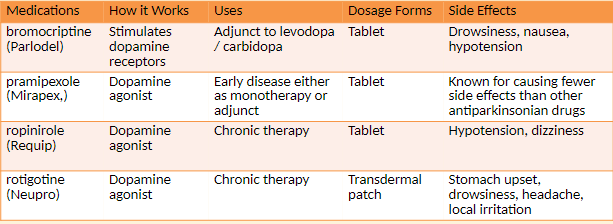
Dopamine
- does not cross the blood brain barrier
- not useful therapeutically
- precursor- Levodopa (L-Dopa)
- converted to Dopamine
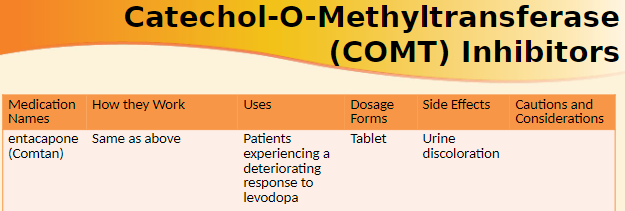
Treatment
Drugs that increase or enhance the action of dopamine in the brain
Drugs that inhibit the effect of acetylcholine
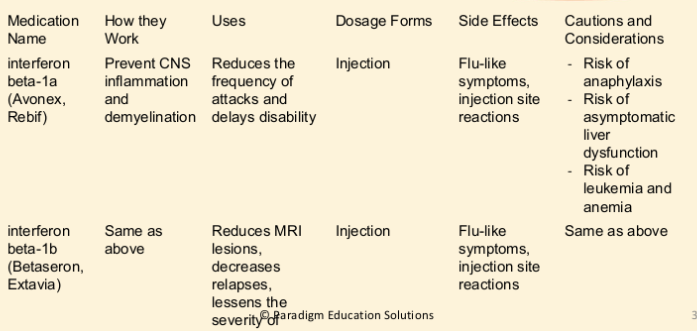
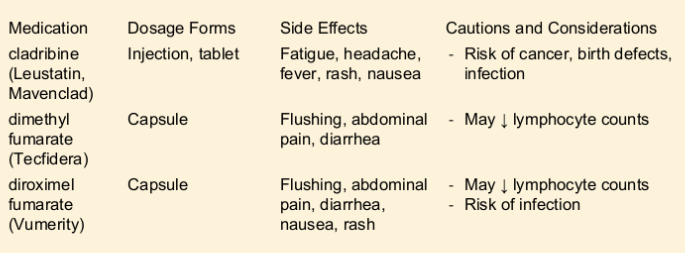
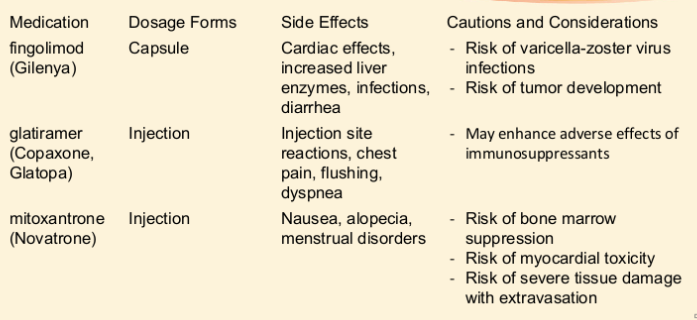
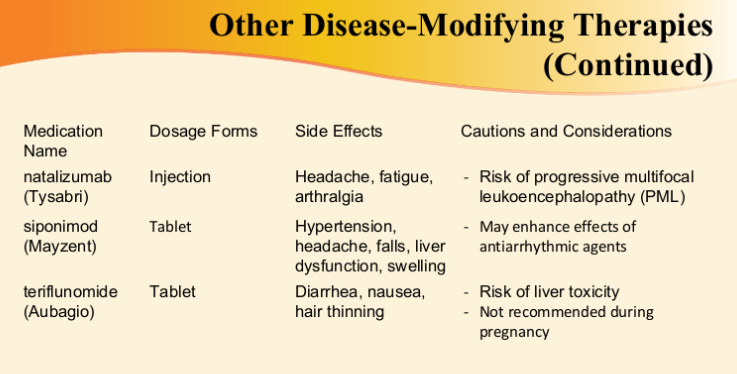
Multiple Sclerosis and Drug Treatments
Multiple Sclerosis: An autoimmune disease in which the myelin sheaths around nerves degenerate
Causes loss of muscle control
can affect eyesight
can result in severe trembling in later stages
no cure but medications used to slow progression
Alzheimer’s Disease
- Alzheimer’s Disease and Drug treatment:A degenerative brain disorder that leads to progressive dementia(symptom) and changes in personality and behavior, changes in personality and behavior, wandering, irritability or hostility
- symptoms include loss of memory, intellect, judgment, orientation, speech
- depression and anxiety are common
- in early stages, patient complain of memory deficit, forgetfulness, misplacement of ordinary items
- In final stages, disease progresses to incapacitation, disorientation, and failure to thrive.
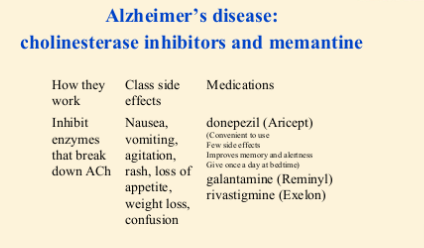
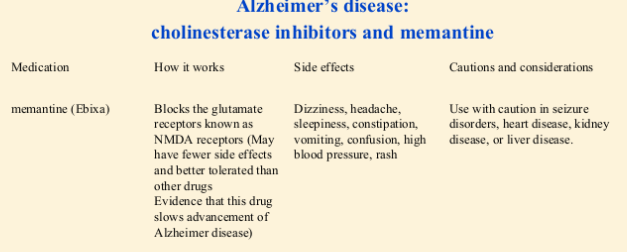
- Causes include insufficient ACh and hyperactive glutamate receptors
- Drug therapy slows the disease but does not cure or reverse it.
- Progressive and irreversible
Other Central Nervous System Disorders
Progression
- Memory deficit, forgetfulness, misplacements of ordinary items
- Inability to complete complex tasks
- Complete incapacitation, disorientation, and failure to thrive
Alzheimer’s= disease
dementia= a symptom
also symptoms of Parkinson’s, vascular dementia, AIDS dementia
Dementia: progressive and irreversible loss of mental capabilities
Treatment: use limited to disease stage
- expensive and controversial
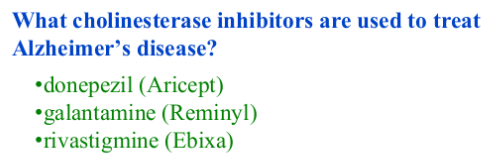
- Cholinesterase inhibitors and memantine
- Antipsychotics:
- to treat dementia associated with AD
- ex. olanzapine (Zyprexa)
Myasthenia Gravis
Myasthenia Gravis: a disorder of the interface between nerves and muscles in which the muscles cannot respond to the nerve signal in order to contract
Cause
- autoimmune damage to ACh receptors at the connection between a nerve and a muscle (neuromuscular junction); ACh receptors are destroyed at the motor end plate
- Symptoms
- weakness and fatigue especially of skeletal muscles
- ptosis (upper eyelid drooping)
- diplopia (double vision)
- dysarthria (imperfect articulation of speech
- dysphagia (difficulty swallowing)
- respiratory difficulty
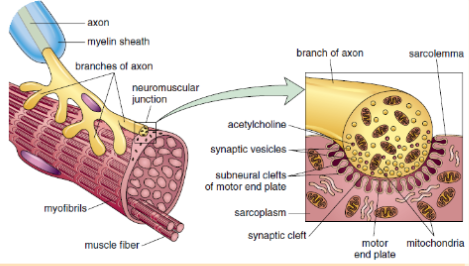
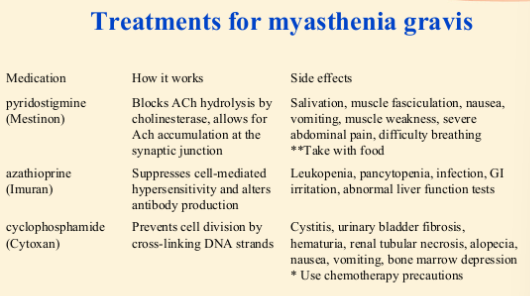
Treatment
- Acetylcholinesterase drugs can produce improvement in all forms of myasthenia gravis
- drug therapy doesn’t inhibit or reverse the immunologic flaw
Amyotrophic Lateral Sclerosis
- Description
- Lou Gehrig’s disease: a progressive degenerative disease of the nerves that leads to muscle weakness, paralysis, and eventually death
- Symptoms
- muscle weakness, muscle paralysis
- Cause
- excessive levels of glutamate which causes nerve damage
- riluzole (Rilutek)
- The only drug that prolongs ALS patient survival
- Works by inhibiting the release of glutamate and inactivating sodium channels
- Side effects include weakness, dizziness, gastrointestinal effects, liver enzyme elevation.
- Seems to improve survival rate by 3 months in some patients
Restless Leg Syndrome and Fibromyalgia
- Restless leg syndrome: Severe pain or unpleasant sensations in the leg
- Usually occurs at bedtime, can cause sleep disturbances
- Cause unknown, may be worsened by stress
- Symptoms may be related to withdrawal from sedatives, or to use of lithium, calcium channel blockers, or caffeine.
- Non drug treatment includes stretching exercises, massage, and warm baths.
- Drug therapy includes gabapentin (Neurontin), pramipexole (Mirapex), and ropinirole (Requip).
- Fibromyalgia
- Long-term pain over entire body; tenderness in joints, muscles, and tendons
- Linked to sleep problems, fatigue, headaches, anxiety, and depression
- Cause unknown; may be triggered by trauma, sleep disturbances, infection
- Nondrug treatment includes physical therapy, exercise, light massage, and relaxation techniques.
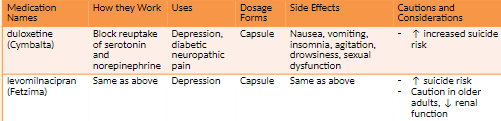
- Drug therapy includes duloxetine (Cymbalta) or pregabalin (Lyrica).
Thursday
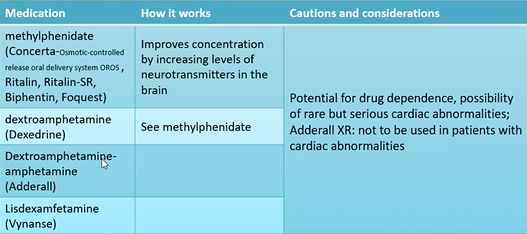
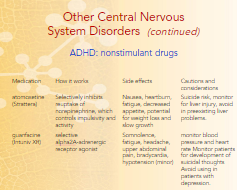
Attention Deficit Hyperactivity Disorder and drug treatments
Attention deficit hyperactivity disorder (ADHD)
Symptoms include inattention, impulsivity, hyperactivity
Diagnosis involve documenting > 6 symptoms of inattention and > 6 symptoms of hyperactivity/impulsivity that impair life in > 2 settings for at least 6 months
Onset by age three, decline in hyperactivity with age but potential for persistence of inattention and impulsivity into adulthood
Coexisting conditions include learning disabilities, depression, anxiety
Inattention, hyperactivity, and impulsivity are used to diagnose ADHD
Complementary or Alternative Therapies
- Yoga
- Used in epilepsy and ADHD
- 5-hydroxytryptophan
- Used in Parkinson’s disease to improve motor symptoms
- Music therapy
- Used in Parkinson’s disease to improve motor symptoms, speech, and bradykinesia
- Ginkgo biloba
- May provide slight benefit patients with early Alzheimer’s disease
- Questionable benefit in preventing Alzheimer’s disease
- Risks include variability in content of products; anti-platelet effects; interaction with warfarin, aspirin, anticonvulsants.
Monday
Nervous System, Mental Health, and Drug Therapy: Depression, Mood Disorders, and Drug Treatments
Depression: feelings of pessimism worry, intense sadness, loss of concentration, slowing of mental processes, problems eating and sleeping
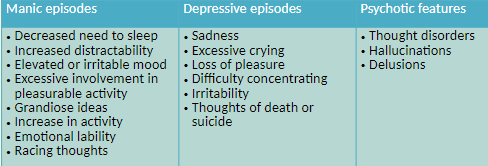
Mania: mental and physical hyperactivity, disorganized behaviour, elevated mood; mood of extreme excitement, excessive elation, hyperactivity, agitation, increased psychomotor activity
Bipolar disorder: alternating episodes of depression and mania; mood swings that alternate between periods of major depression and periods of mild to severe chronic agitation
Post Traumatic Stress Disorder: Triggered by a traumatic event that leaves a person with intense, disturbing thoughts and feelings long after the event; Persistent anxiety or recurrent fear after a terrifying event
Seasonal Affective Disorder: depression which occurs in the fall and winter and remits in the spring and summer
Neurotransmitters
- produced by a nerve cell and transmit information
- ie. serotonin, norepinephrine, dopamine
- psychiatric and mood disorders
- deficiency of neurotransmitters
- dysfunction of neurotransmitters
Antidepressants
- goal of therapy is to change neurotransmitter levels
- take 10-21 days to start working
- medication Guide required
Overview of Disorders
- hard to diagnose
- often occur together in same patient
- Need multiple medications for treatment
- Good communication essential among patient family or caregivers. prescriber, pharmacist
Antidepressants
- delay of onset of 10-21 days
- not used on “as needed” basis
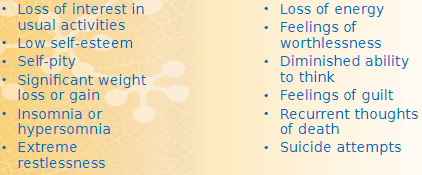
Depression
- underlying causes: exogenous vs. endogenous sources
- signs: crying, loss of interest in life or social activities, increased focus on death, significant weight loss or gain
- symptoms: low self-esteem, pessimism, sleep disturbances, loss of energy and ability to think, feelings of worthlessness and guilt, poor memory, thoughts of suicide
- neurotransmitters involved in mood: norepinephrine, serotonin, dopamine
Drug Regimens and Treatments for Depression
- Patient response to drug therapy
- response not immediate
- may take 3-6 weeks for full response
- drug therapy trial of at least 3-4 weeks
- Risk for suicide
- teens and young adults
- highest risk is when starting drug therapy
- monitor for worsening signs of depression, suicidal thoughts, unusual behaviours
- Stopping Therapy
- risk of facute withdrawal symptoms if stopped abruptly
- worsened depression symptoms if dose not tapered
Clinical depression is the most severe psychiatric disorder
women more likely than men to have depression
depression occurs later in life in men
Selective Serotonin Reuptake Inhibitors (SSRI): block reuptake of serotonin, little effect on norepinephrine
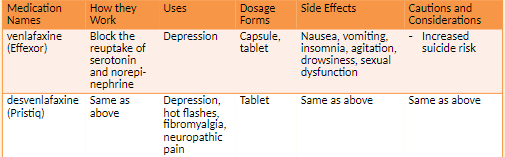
Serotonin Norepinephrine Reuptake Inhibitors (SNRI): increase both serotonin and norepinephrine
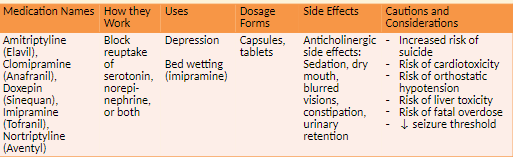
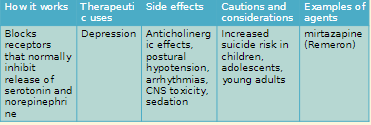
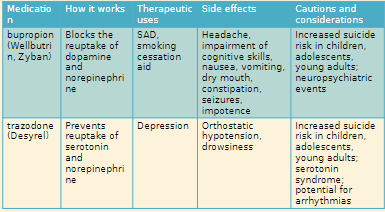
- Tricyclic Antidepressants (TCA): prevent reuptake of serotonin and/or norepinephrine
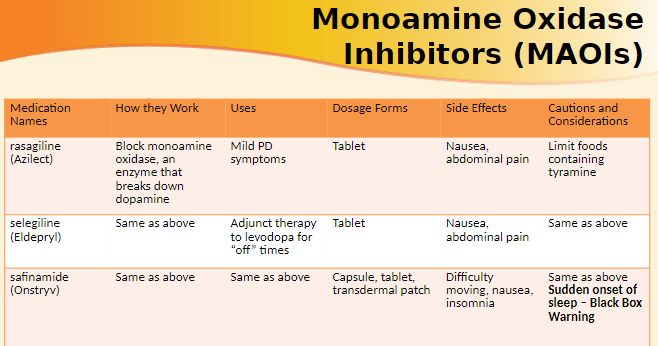
Monoamine Oxidase Inhibitors (MAOIs): inhibit enzymes that break down serotonin and norepinephrine
Depression
Serotonin syndrome
- cause: presence of too much serotonin
- Signs: racing heart, fever, high blood pressure, headache
- risk factors: taking more than one antidepressant, taking St. John’s wort
- Prognosis: potentially fatal
Selective Serotonin Reuptake Inhibitors: block the reuptake of serotonin
- classified effects: Nausea, vomiting, dry mouth, drowsiness, insomnia, headache, diarrhea, sexual dysfunction, serotonin syndrome
Patients wish antidepressants worked immediately, but it is important to realize that it may take four weeks for these medications to achieve full effect. Antidepressants should help with sleep problems within a week or so, but other psychiatric effects may take longer to achieve full efficacy.
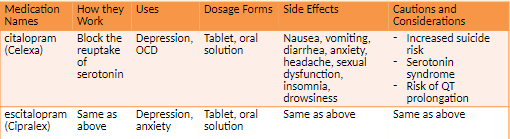
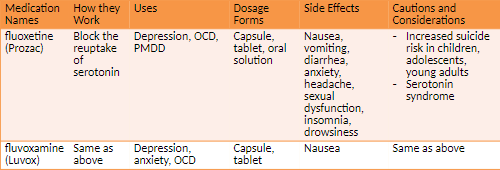
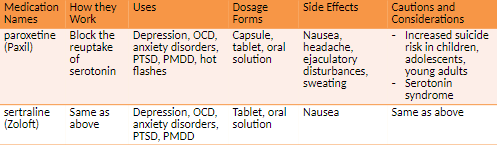
Additional uses for SSRIS Obsessive-compulsive disorder (OCD) A form of anxiety Obsessive thoughts impair function.
Repetitive behaviors relieve fears and anxiety. Premenstrual dysphoric disorder (PMDD) Emotional and behavioral changes during second half of a woman's menstrual cycle Similar symptoms to PMS but more severe Posttraumatic stress disorder (PTSD), fibromyalgia, anxiety, panic disorder, nerve pain (duloxetine)
Often confused
- Celexa
- Celebrex (arthritis)
Look-a-like
- Prozac
- Proscar (prostrated enlargement)
not alcohol
do not stop abruptly
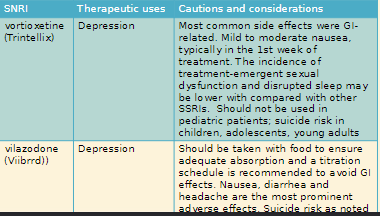
Serotonin and norepinephrine Reuptake inhibitors work by blocking the reuptake of serotonin and norepinephrine
- side effects: nausea, vomiting, insomnia, agitation, drowsiness
Chapter 8 day 2
Depression and Mood Disorders
2 Weeks washout period before starting new class of antidepressants
severe hypertensive reactions with food containing high levels of tyramine
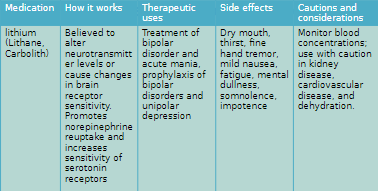
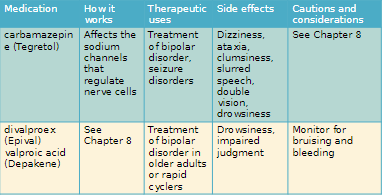
Bipolar Disorder
Periods of depression alternating with periods of mania, a state of overly high energy, excitement, hyperactivity, optimism, and increased psychomotor activity
Increased psychomotor activity can involve irritability, excessive involvement in work or other activities, grandiose ideas, racing thoughts, decreased need for sleep
Goals of Therapy
- Treat acute episodes and prevent subsequent attacks
Mania: mood of extreme excitement, excessive elation, hyperactivity, agitation, and increased psychomotor activity
Bipolar Disorder: mood swings that alternate between major depression and mania
Unipolar Depression: major depression with no previous occurrence of mania
Post-traumatic stress disorder: Disorder characterized by persistent agitation or persistent, \n recurrent fear after the end of a traumatic event and lasting for over a month or impairing work or relationship
Seasonal Affective Disorder: Form of depression that recurs in the fall and winter and remits in the spring and summer
The two-fold objective of drug therapy is to treat acute episodes and prevent subsequent attacks
Schizophrenia, Psychosis and drug Treatments
Schizophrenia: A chronic mental health disorder characterized by delusions, disorganized speech and behavior, decrease in emotional range, neurocognitive deficit
- Cause excessive dopamine levels in the limbic system
- Positive symptoms include hallucinations and delusions
- Negative symptoms are withdrawal, ambivalence, behaviour changes, memory loss and confusion
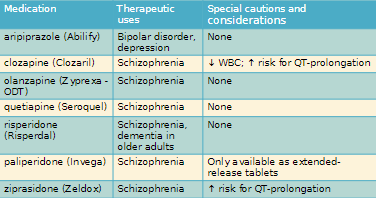
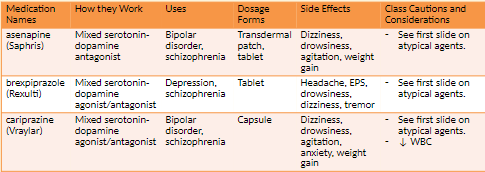
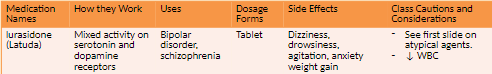
Treatment
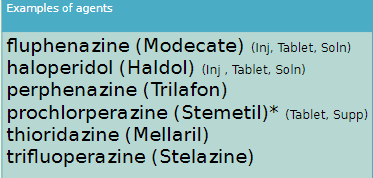
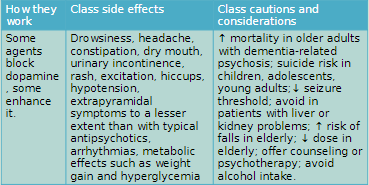
- Typical antipsychotic
- Block dopamine receptors in all four dopamine pathways
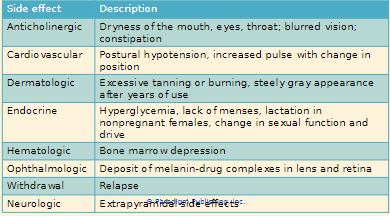
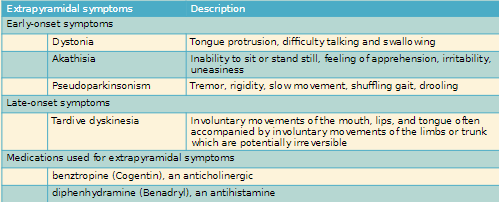
- Lead to unfavorable side effects extrapyramidal symptoms (EPS)
- Atypical antipsychotics
- Block dopamine receptors in the limbic system pathway instead of all four pathways
- Improved efficacy and fewer side effects
Goals of Therapy: reduce symptoms such as thought disorder, hallucination, delusions