Week 4 Care of Fetus During Perinatal Period
Embryonic and Fetal Structure
Embryonic stage of gestation - is the period after implantation during which all of the major organs and structures within the growing fetus are formed
PREGNANCY - the state of having a developing embryo or fetus within the body, state from conception to the delivery of the fetus
Decidua or Uterine Lining
After fertilization, the corpus luteum in the ovary continues to function rather than atrophying, because of the influence of human chorionic gonadotropin (hCG), a hormone secreted by the trophoblast cells.
After fertilization, the Corpus luteum, Causes the uterine endometrium to continue to grow in thickness and vascularity instead of sloughing off as in a usual menstrual cycle.
The Endometrium is now termed the Decidua (Latin word for “falling off”)because it will be discarded after the birth of the child.
Trophoblast - are cells forming the outer layer of a blastocyst, which provide nutrients to the embryo and develop into a large part of the placenta
Blastocyst – is the stage that the human embryo reaches approximately 5-6 days after fertilization
Decidua basalis
is the part of the endometrium that lies directly under the embryo or the portion where the trophoblast establish communication with the maternal blood vessels
Decidua capsularis
the portion of the endometrium that encapsulates the surface of the trophoblast
Decidua vera
is the remaining portion of the uterine lining.
as the embryo enlarges it brings the decidua capsularis into contact with the decidua vera and fuse,
At birth the entire inner surface of the uterus is stripped away, leaving the organ highly susceptible to hemorrhage and infection
Chorionic Villi
Once implantation is complete, trophoblastic layer of cells of the blastocyst begins to mature rapidly.
11th or 12th day - miniature villi that resemble probing fingers, termed chorionic villi, reach out from the single layer of cells into the uterine endometrium to begin formation of the placenta.
Syncytiotrophoblast (Syncytial Layer)
is the outer layer of cells that produces various placental hormones
a. hCG – Human Chorionic Gonadotropin Hormones
b. Somatomammotropin (Human Placental Lactogen)
c. Estrogen
d. Progesterone
Cytotrophoblast (Langhan’s Layer)
the middle layer, present as early as 12 days gestation.
Function in early pregnancy is to protect the growing embryo and fetus from certain infectious organisms spirochete of Syphilis
This layer of cells disappears - between 20th and 24 wks
Passive antibody begins at 20th wks.
Syphilis is not considered to have a high potential for fetal damage early in pregnancy, only after the point at which cytotrophoblast cells are no longer present The layer appears to offer little protection against viral infection
Placenta
a flat, disc shaped organ that is highly vascular, forms in the upper segment of the endometrium of the uterus.
Is responsible in the exchange of nutrients and gases between the fetus and the mother.
15-20 cm in diameter, 2-3 cm in depth
With 30 Cotyledons
Weight – 400g.- 600g
Purposes
Respiratory system – exchange of O2 and CO2 takes place in the placenta not in the fetal lungs.
Renal system – waste products are excreted through the placenta.
Circulatory system – fetal placental circulation takes place via the umbilical vein
Nutrients pass to the fetus via the placenta
Endocrine Function Hormones produced
a. Human Chorionic Gonadotropin (HCG)
b. Estrogen
c. Progesterone
d. Somatomammotropin (Human Placental Lactogen)
Placental Circulation
12th day of pregnancy - maternal blood begins to collect in the uterine endometrium surrounding the chorionic villi.
By the third week, oxygen and other nutrients, (glucose, amino acids, fatty acids, mineral, vitamins, and water) from the maternal blood through the cell layers of the chorionic villi into the villi capillaries.
From there, nutrients are transported to the developing embryo.
Fetal Membranes
Amnion
inner layer of the fetal membrane, gives rise to umbilical cord
Chorion
outermost membrane surrounding an embryo gives rise to the placenta
Umbilical cord
about 53 cm. (21 in) in length at term and about 2 cm. (0.75 in) thick
contains 2 arteries and one vein which are kept in place by the Wharton jelly
WHARTON’S JELLY - a gelatinous substance which prevents pressure on the vein and arteries.
Provides a circulatory pathway connecting the embryo to chorionic villi
Transport oxygen and nutrients to the fetus from the placenta return waste products from the fetus to the placenta
Amniotic Fluid (Bag of Water)
a clear, colorless, albuminous fluid in which the baby floats.
Containing little white packs of vernix caseosa and other solid particles.
Begins to form at 11-15 weeks gestation
The fetus continuously swallow the amniotic fluid and absorbed from the fetal intestine into the fetal bloodstream
it goes to the umbilical arteries to the placenta and is exchanged across the placenta to the mother’s bloodstream
Color: the same with water, Amount: 800-1200 ml, Ph 7.2 (Slightly Alkaline)
Purposes:
Shields against blows or pressure on the mother’s abdomen.
Protects against the sudden changes in temperature.
Protects the fetus from infection
Provides free movement for the fetus.
Abnormalities
Hydramnios – excessive amniotic fluid, more than 2000ml
Oligohydramnios – reduction in amniotic fluid, less than 300 ml
Reason if the fetus is unable to swallow (Esophageal atresia and Ancephaly)
Diagnostic
Amniocentesis
is the withdrawal of amniotic fluid to diagnose chromosomal abnormalities.
Meconium
stained amniotic fluid in non-breech presentation is a sign of fetal distress
Endocrine Function
Human Chorionic Gonadotropin (hCG)
First hormone produced as early as the missed menstruation until 100th day of pregnancy
Testing for HCG - proof that placental tissue is no longer present after birth.
At 8th wks. of pregnancy begin to ↓ HCG - placenta starts to produce progesterone
Functions
Ensure that the corpus luteum continues to produce progesterone and estrogen
Suppress the maternal immunologic response so that the placental tissue is not rejected
if the fetus is male, it exerts an effect on the production of testosterone
Estrogen (Hormone of Women)
Second hormone produced by syncytial cells
Function
Contribute to mammary glands development, in preparation for lactation.
Stimulates uterine growth to accommodate the developing fetus
Progesterone (Hormone of Mothers)
Functions
Maintain endometrial lining of the uterus.
Reduce the contractility of the uterus.
Human Placental Lactogen (HPL)
Functions
Promotes mammary gland growth in preparation for lactation
Regulates maternal glucose, protein, and fat levels
Origin and Development of Organ Systems
4 days: Zygote cells known as Totipotent
Totipotent stem cells – are undifferentiated cells that can develop a human being
After another 4 days: Totipotent cells become Pluripotent
Pluripotent Stem cells – specific body cells (Nerve, Brain, or Skin cells)
Another few days the Pluripotent cells become Multipotent
Multipotent cells - at the time of implantation, the blastocysts has two cavities in the inner structure (Amniotic cavity and Yolk sac)
Two cavities in the inner structure
Amniotic cavity
Yolk sac
supply nourishment only until implantation
Provide a source of RBC until the embryo can produce its own (12th wk.)
The Three Germ Layers: (Body Portions Form)
Ectoderm - skin, nervous system and sense organ
Mesoderm – musculoskeletal, circulatory and genitourinary
Endoderm – respiratory and GIT
Fetal Growth and Development
The life of the fetus is measured from the time of Ovulation or fertilization (Ovulation age)
Length of pregnancy - is measured from the First day of the Last menstrual period (Gestational age)
Gestational age: Lunar Months (4 wk. period) = 10 months (40 wks. / 280days)
Ovulation Age: Trimesters (3 months) = 9.5 lunar months (38 wks. / 266days)
Fetal Developmental milestones based on gestational weeks
Teminologies
Babinski Reflex
are responses that occur when the body receives a certain stimulus
Lanugo
is the fine, downy hair that covers a term newborn’s shoulder, back, upper arms, forehead and ears. It is the first type of hair that grows from hair follicles
Primigravida
woman that is pregnant for the first time
Multigravida
woman that has been pregnant two or more times
Meconium
is a collection of sticky cellular wastes, bile, fats, mucoproteins, mucopolysaccharides, and portion of vernix caseosa
Brown Fat
a special fat that aides in temperature regulation
Lung Surfactant
is a mixture of lipids and proteins which is secreted into the alveolar space by epithelial cell
Function is to lower the surface tension at the air or liquid interface within the alveoli of the lung
Moro Reflex
an infantile reflex that develops between 28–32 weeks of gestation an disappears between 3–6 months of age
It is a response to a sudden loss of support involves :
a. Spreading out the arms (abduction)
b. Pulling the arms in (adduction)
Vernix Caseosa
a white, cream cheese-like substance that protect the skin and serve as lubricant in utero during the last trimester of pregnancy.
End of 4th Gestational Week (1 month)
Length: 0.75 cm, Weight: 400 mg
The spinal cord is formed and fused at the midpoint.
The head is large in proportion and represents about one third of the entire structure
The rudimentary heart appears as a prominent bulge on the anterior surface.
Arms and legs are budlike structures
Rudimentary eyes, nose and ears are discernible
End of 8th Gestational Week (2 months)
Length: 2.5 cm (1 in), Weight: 20 g
Organogenesis is complete.
The heart, with a septum and valves, is beating rhythmically
Facial features are definitely discernible
Arms and legs have developed
External genitalia are forming, but sex is not yet distinguishable by simple observation
The abdomen bulges forward because the female intestine is growing so rapidly
A sonogram shows a Gestational sac, which is diagnostic of pregnancy
Gestational sac - is the large cavity of fluid surrounding the embryo.
End of 12th Gestational Week (3 months)
Length: 7–8 cm, Weight: 45 g.
Nail beds are forming on fingers and toes
Spontaneous movements are possible, although they are usually too faint to be felt by the mother
Some reflexes, such as the Babinski reflex, are present
Bone ossification centers begin to form
Tooth buds are present
Sex is distinguishable by outward appearance
Urine secretion begins but may not yet be evident in amniotic fluid.
The heartbeat is audible through Doppler technology.
End of 16th Gestational Week (4 months)
Length: 10–17 cm, Weight: 55–120 g
Fetal heart sounds are audible by an ordinary stethoscope
Lanugo is well formed
Liver and pancreas are functioning
Fetus actively swallows amniotic fluid
Demonstrating an intact but uncoordinated swallowing reflex
Urine is present in amniotic fluid
Sex can be determined by ultrasound
End of 20th Gestational Week (5 months)
Length: 25 cm, Weight: 223 g
Antibody production is possible
Hair including eyebrows forms on the head, vernix caseosa begins to cover the skin
Spontaneous fetal movements can be sensed by the mother
4th month – multigravida
5th month - primigravidaMeconium is present in the upper intestine
Brown fat begins to form behind the kidneys, sternum, and posterior neck, can produce heat to warm the body
Passive antibody transfer from mother to fetus begins
Definite sleeping and activity patterns are distinguishable, fetus develops biorhythms that will guide sleep/wake patterns throughout life
End of 24th Gestational Week (6 months)
Length: 28–36 cm, Weight: 550 g
Meconium is present as far as the rectum
Active production of lung surfactant begin
Eyelids, previously fused since the 12th week, now open pupils reacting to light.
Eyebrow and eyelashes become well defined
When fetuses reach 24 weeks, or 500-600 g they have achieved a practical low-end age of viability if they are cared for after birth in a modern intensive care facility.
Hearing can be demonstrated by response to sudden sound.
End of 28th Gestational Week (7 months)
Length: 35–38 cm., Weight: 1200 g
Lung alveoli begin to mature, and surfactant can be demonstrated in amniotic fluid.
Testes begin to descend into the scrotal sac from the lower abdominal cavity.
The blood vessels of the retina are formed but thin and extremely susceptible to damage from high oxygen concentrations
an important consideration when caring for preterm infants who need oxygen
End of 32nd Gestational Week (8 months)
Length: 38–43 cm, Weight: 1600 g
Subcutaneous fat begins to be deposited (the former stringy, “little old man” appearance is lost)
Fetus responds by movement to sounds outside the mother’s body.
Iron stores, which provide iron for the time during which the neonate will ingest only milk after birth, are beginning to be developed
Fingernails grow to reach the end of fingertips.
Active Moro reflex is present.
End of 36th Gestational Week (9 months)
Length: 42–48 cm., Weight: 1800–2700 g (5–6 lb.)
Body stores of glycogen, iron, carbohydrate, and calcium are deposited.
Additional amounts of subcutaneous fat are deposited
Sole of the foot has one or two crisscross creases, compared with the full crisscross pattern that will be evident at term.
Fetus kicks actively
Most babies turn into a Vertex (Head down) presentation during this month
End of 40th Gestational Week (10 months)
Amount of lanugo begins to diminish
Fetal hemoglobin begins its conversion to adult hemoglobin
Fingernails extend over the fingertips 2/3 of the sole with creases
Vernix caseosa fully formed
Fetal Circulation
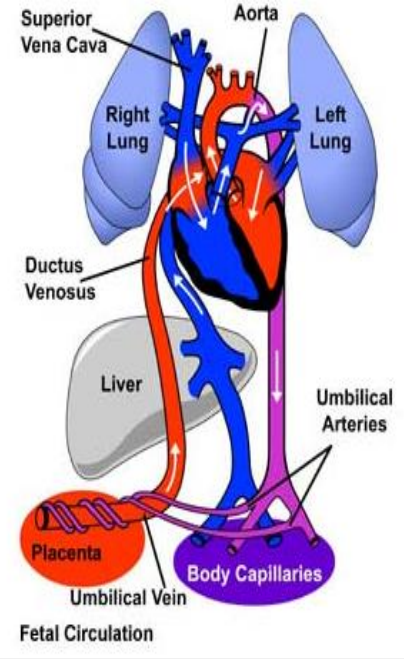
Structures involved in Fetal Circulation
Placenta
where gas exchange takes place during fetal life.
Umbilical Arteries
carry deoxygenated blood from fetus to placenta.
Umbilical Veins
carry oxygenated blood from the placenta to the fetus
Ductus Venosus
carries oxygenated blood from umbilical vein to inferior venaca va bypassing fetal liver
Ductus Arteriosus
It closes during normal neonatal respiration. Allows the blood to bypass the fetal lungs.
Foramen Ovale
temporary opening that connects the left and right atrium.
It pushes blood from the right atrium to the left atrium.
normally this opening closes at birth, when the lungs become functional
Adaptation to Extra-Uterine Life
At birth, the baby takes a breath and blood drawn to the lungs through the pulmonary arteries.
It is then collected and returned to Left Atrium via the pulmonary veins resulting in a sudden inflow of blood
The placental circulation ceases soon after birth and so less blood returns to the right side of the heart.
The pressure in the left side of the heart is greater, while in the right side is lesser.
This results in the closure of the flap over the foramen ovale , which separates the 2 sides of the heart and stops the blood from flowing from right to left.
With the establishment of pulmonary respiration the oxygen concentration in the blood stream rises.
This causes the ductus arteriosus to constrict and closes.