Test 3 - study guide
Pathophysiology Overview & Pharmacology for the Management of Diabetes Mellitus
Learning Objectives
- Demonstrate understanding of glucose and insulin metabolism
- Identify and differentiate between Type 1 and Type 2 Diabetes Mellitus
- Describe tests and associated values for diagnosing Diabetes Mellitus
- Explain treatments and medications for managing Diabetes Mellitus
Etiology of Diabetes Mellitus
- Defined: Hyperglycemia due to absent/insufficient insulin and/or poor utilization of insulin
- Genetic
- Autoimmune
- Environmental
Affects 29.1 million people
Seventh leading cause of death
A chronic, multisystem disease
Leading cause of:
Adult blindness
ESRD
Nontraumatic lower limb amputations
Major contributing factor:
Heart disease
Stroke
Normally…
- Your body needs glucose in the blood, to be transported to cells for energy
- Diabetes is too much glucose in the blood
- Glucose and Insulin Metabolism
- Insulin produced by beta cells in islets of Langerhans
- Continuous release into bloodstream with larger amounts released after ingesting food
- Keeps blood glucose level in range: 70-110 mg/dL- TEST
How Insulin Works
https://www.youtube.com/watch?v=CuQMpN7rM-4
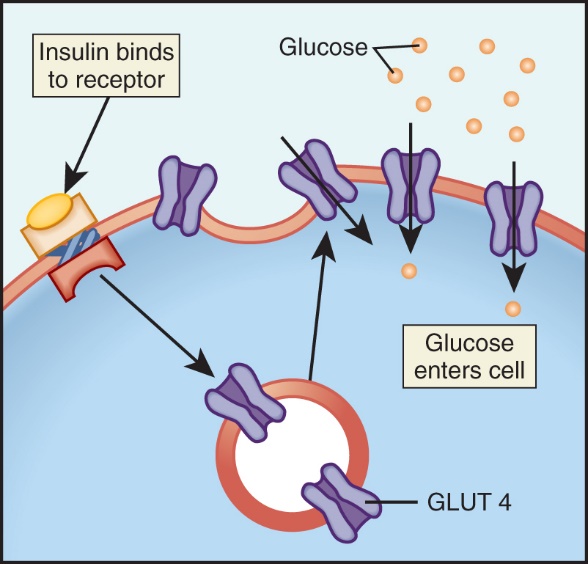
- Insulin promotes glucose transport from the bloodstream across the cell membrane to the cytoplasm of the cell.
- Cells break down glucose to make energy, and liver and muscle cells store excess glucose as glycogen.
- Skeletal muscle and adipose tissue have specific receptors for insulin and are considered insulin-dependent tissues. Insulin is required to “unlock” these receptor sites, allowing the transport of glucose into the cells to be used for energy. Other tissues (e.g., brain, liver, blood cells) do not directly depend on insulin for glucose transport, but require an adequate glucosen bv54ewa
- Normal glucose and insulin metabolism.
- Insulin binds to receptors along the cell walls of muscle, adipose, and liver cells.
- Glucose transport proteins (GLUT 4) then attach to the cell wall and allow glucose to enter the cell where it is either stored or used to make energy.
Your body increases blood glucose with:
- Glucagon
- epinephrine
- growth hormone
- cortisol
Oppose effects of insulin
Stimulate glucose production and release by the liver
Decrease movement of glucose into cell
Help maintain normal blood glucose levels
Glucagon, epinephrine, growth hormone, and cortisol are counterregulatory hormones that work to oppose the effects of insulin.
These hormones increase blood glucose levels by (1) stimulating glucose production and release by the liver and (2) decreasing the movement of glucose into the cells.
The counterregulatory hormones and insulin usually maintain blood glucose levels within the normal range by regulating the release of glucose for energy during food intake and periods of fasting.
Classes of Diabetes Mellitus
- Type 1
- Type 2
- Gestational
- Other specific types
- Prediabetes
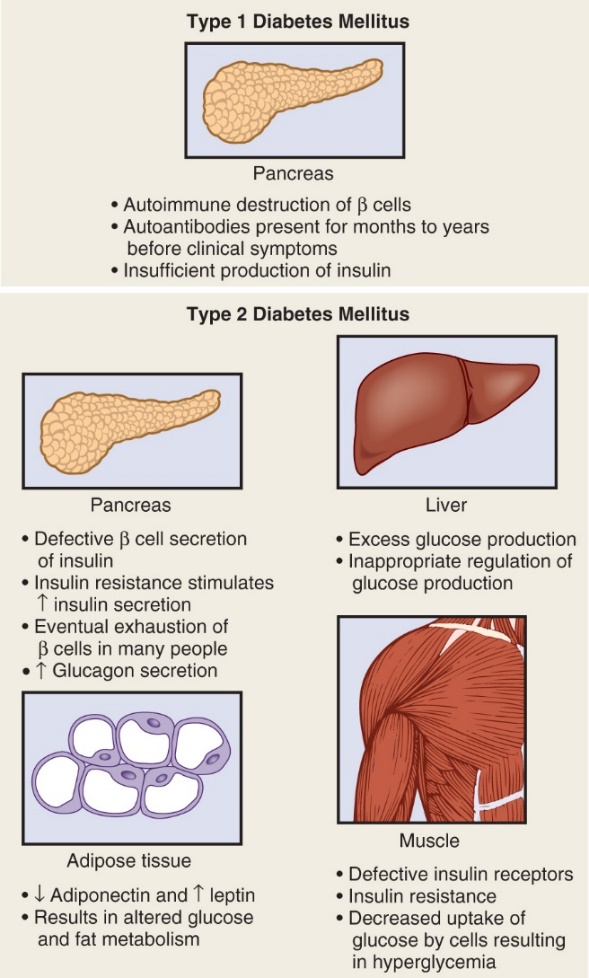
Type 1 DM- INSULIN DEPENDENT
- Formerly known as juvenile-onset or insulin-dependent diabetes
- 5-10% of all people with diabetes
- Typically, under age 40, but can occur at any age
- Autoimmune
- Genetics
- Idiopathic diabetes
- Onset of disease: once beta cell destruction leads to insufficient insulin release, onset is rapid, with ketoacidosis
- Clinical Manifestations
Classic symptoms
- Polyuria
- Polydypsia
- Polyphagia
- Weight loss
- Weakness
- Fatigue
Type 2 DM-
- Formerly known as adult-onset diabetes or non-insulin-dependent diabetes
- 90-95% of those with diabetes
- Risk factors: overweight, obesity, advanced age, family history (genetic link), metabolic syndrome
- Increasing in children
- Prevalence higher in ethnic groups
- Some endogenous insulin production, but
- Not enough insulin OR
- Body does not use insulin effectively (insulin resistance)
- Gradual onset: hyperglycemia undetected for years
Clinical Manifestations
- Genetic link
- Insulin resistance
- Decreased insulin production
- Inappropriate hepatic glucose production
- Altered hormone and cytokine production by adipose tissues (adipokines)
- Research continues on role of brain, kidneys, and gut in T2DM
- Metabolic syndrome increases risk for T2DM
- Elevated glucose levels
- Abdominal obesity
- Elevated BP
- High levels of triglycerides
- Decreased levels of HDLs
Nonspecific symptoms
- Fatigue
- Recurrent infection
- Recurrent vaginal yeast or candidal infection
- Prolonged wound healing
- Visual changes
LABS: Blood Glucose vs. Hgb A1C (Glycosolated Hemoglobin)
- Blood glucose – the finger stick - shows the amount currently in the blood stream (normal 70-110 mg/dL)
- Comprehensive metabolic panel (CMP), basic metabolic panel (BMP)
- Hemoglobin A1C
- Glycosylated hemoglobin: reflects glucose levels over past 2 to 3 months
- Used to diagnose, monitor response to therapy, and screen patients with prediabetes
- Goal: < 6.5% to 7%
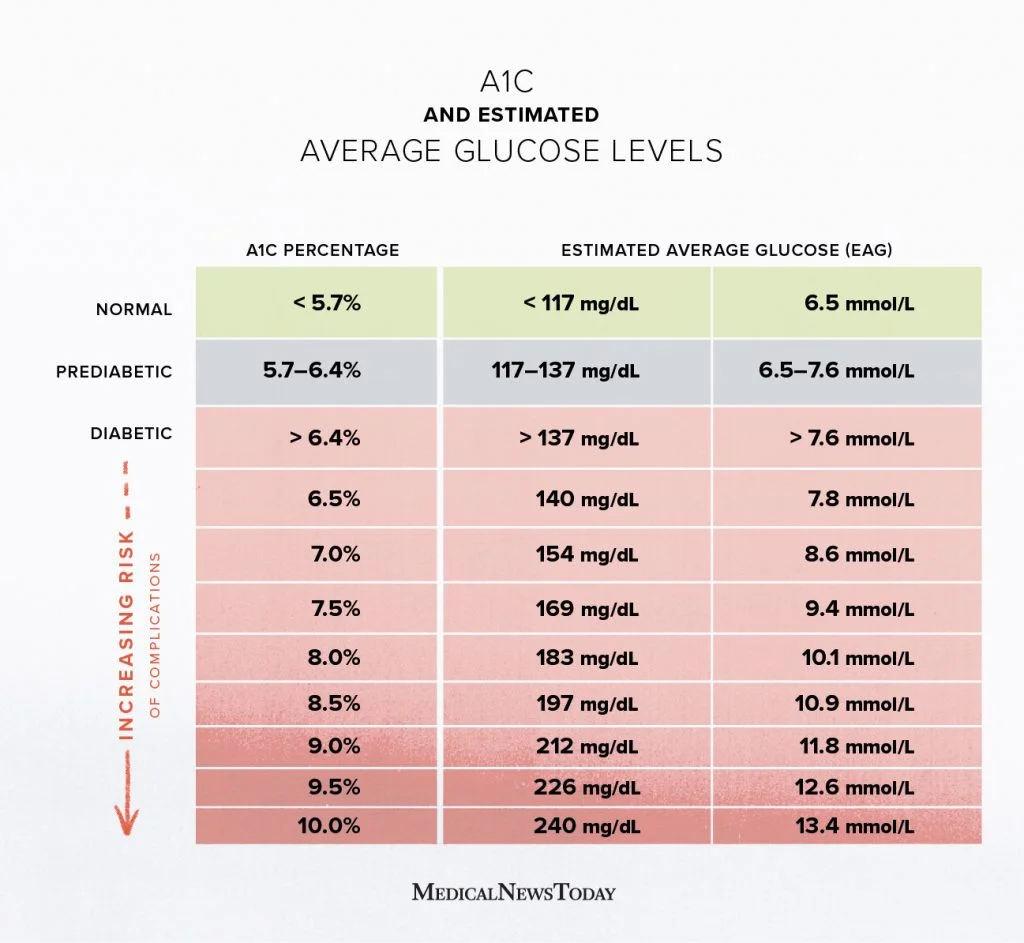
Diagnosing Diabetes Mellitus
- Hemoglobin A1C level: 6.5% or higher
- Fasting plasma glucose level: higher than 126 mg/dL
- Two-hour plasma glucose level during OGTT: 200 mg/dL (with glucose load of 75 g)
- Classic symptoms of hyperglycemia with random plasma glucose level of 200 mg/dL or higher
- Other: Fructosamine, Autoantibodies
The diagnosis of diabetes mellitus is made using one of four methods. These methods and their criteria for diagnosis are as follows:
1. Hemoglobin A1C level of 6.5% or higher.
2. Fasting plasma glucose (FPG) level of 126 mg/dL (7.0 mmol/L) or higher. Fasting is defined as no caloric intake for at least 8 hours.
3. Two-hour plasma glucose level of 200 mg/dL (11.1 mmol/L) or higher during an OGTT, with a glucose load of 75 g.
4. In a patient with classic symptoms of hyperglycemia (polyuria, polydipsia, unexplained weight loss) or hyperglycemic crisis, a random plasma glucose level of 200 mg/dL (11.1 mmol/L) or higher.
If a patient presents with a hyperglycemic crisis or clear symptoms of hyperglycemia (polyuria, polydipsia, polyphagia) with a random plasma glucose level of 200 or higher, repeat testing is not warranted.
Otherwise, criteria 1 through 3 should be confirmed by repeat testing to rule out laboratory error. It is preferable for the repeat test to be the same test used initially. For example, if a random blood glucose test showed elevated blood glucose levels, the same test should be used again when the person is retested.
Fructosamine is another way to assess glucose levels. Fructosamine is formed by a chemical reaction of glucose with plasma protein. It reflects glycemia in the previous 1 to 3 weeks. Fructosamine levels may show a change in blood glucose levels before A1C does.
Islet cell autoantibody testing is ordered primarily to help distinguish between autoimmune type 1 diabetes and diabetes due to other causes.
Prediabetes
- Glycosylated hemoglobin (Hemoglobin A1C)
- 5.7 - 6.4
- Impaired glucose tolerance (IGT)
- OGTT 140-199 mg/dL
- Impaired fasting glucose (IFG)
- Fasting glucose of 100-125 mg/dL
- Patient Teaching**
Asymptomatic but long-term damage occurring
Undergo screening
Manage risk factors
Monitor for symptoms of DM
Maintain healthy weight, exercise, make healthy food choices
Persons with prediabetes usually do not have symptoms. However, long-term damage to the body, especially the heart and blood vessels, may already be occurring.
It is important for patients to undergo screening and to understand risk factors for diabetes.
Patients with prediabetes can take action to prevent or delay the development of type 2 diabetes. Encourage those with prediabetes to have their blood glucose and A1C checked regularly and monitor for symptoms of diabetes, such as polyuria, polyphagia, and polydipsia. Maintaining a healthy weight, exercising regularly, and making healthy food choices have all been found to reduce the risk of developing overt diabetes in people with prediabetes.
Gestational Diabetes
- Develops during pregnancy
- Increased risk of need for cesarean delivery and of perinatal complications
- Screen high-risk patients first visit; others at 24 to 28 weeks
- Usually glucose return to normal 6 weeks post-partum
Other Types of DM
- Results from pancreatic injury and interference with or destruction of beta-cell function
- Examples:
- Cushing syndrome
- Hyperthyroidism
- Recurrent pancreatitis
- Cystic fibrosis
- Hemochromatosis
- Parenteral nutrition
- Medications: Corticosteroids, Thiazides, Phenytoin, Atypical antipsychotics
PHARMACOLOGICAL MANAGEMENT OF DM
Insulin
- Exogenous insulin
- Insulin from an outside source
- Required for T1 DM
- Prescribed for T2 DM when cannot manage blood glucose levels by other means
- Genetically engineered in laboratories
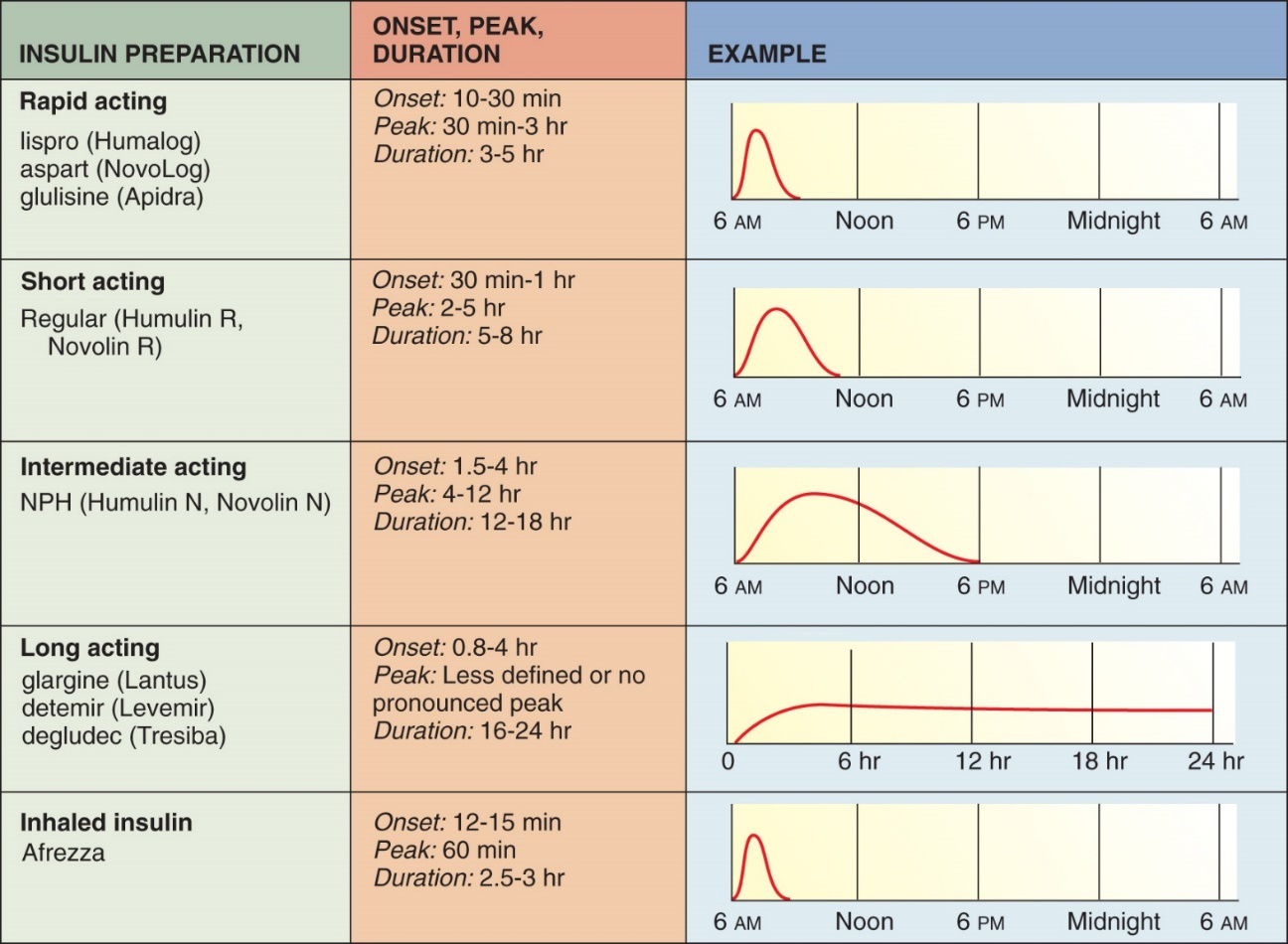
- Categorized according to onset, peak action, and duration:
- Rapid-acting
- Short-acting
- Intermediate-acting
- Long-acting
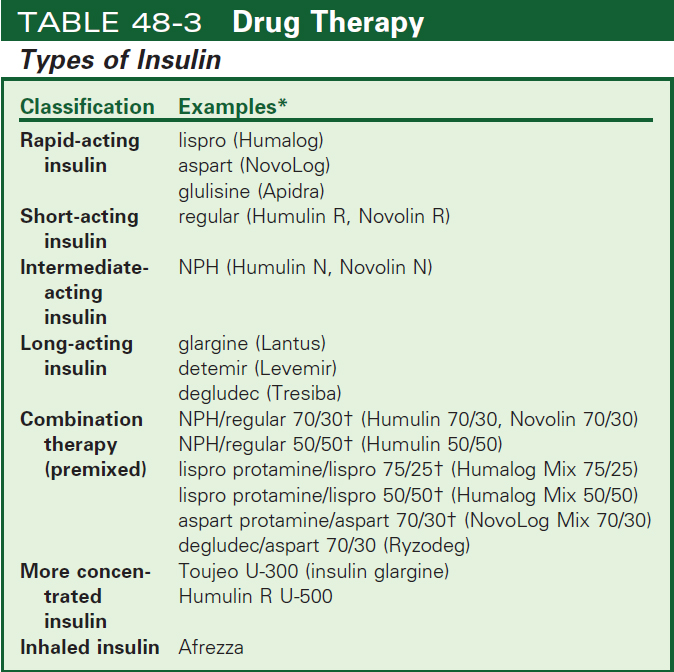
Insulin Regimens
- Basal-bolus regimen
- Most closely mimics endogenous insulin production
- Rapid- or short-acting (bolus) insulin AC (before meals) and sometimes HS (at night)
- Intermediate- or long-acting (basal) background insulin once a day- at HS (can see it given twice a day)
- Less intense regimens possible
Mealtime Insulin (Bolus)
- Insulin preparations
- Rapid-acting (bolus)
- Lispro, aspart, glulisine
- Onset of action: 15 minutes
- Injected within 15 minutes of mealtime
- Rapid-acting (bolus)
- Short-acting (bolus)
- Regular
- Onset of action 30-60 minutes
- Injected 30-45 minutes before meal
Background Insulin (Basal)
- Used to manage glucose levels between meals and overnight
- Intermediate-acting insulin NPH (basal)
- Long-acting (basal)
Background Insulin (Basal)
- Intermediate-acting insulin
- NPH
- Duration 12 to 18 hours
- Peak 4 to 12 hours
- Can mix with short- and rapid-acting insulins
- Cloudy; must agitate to mix
- Combination Insulin Therapy
- Mixing short- or rapid-acting insulin with intermediate-acting insulin in same syringe
- Provides mealtime (bolus) and basal coverage in one injection
- Commercially premixed or self-mix
- Long-acting (basal)
- Insulin glargine (Lantus) and detemir (Levemir)
- Released steadily and continuously with no peak action for many people
- Administered once a day- evening/HS (can see it used twice a day)
- Do not mix with any other insulin or solutions
Insulin Storage
- Do not heat/freeze
- In-use vials may be left at room temperature up to 4 weeks
- Extra insulin should be refrigerated
- Avoid exposure to direct sunlight, extreme heat or cold
- Store prefilled syringes upright for 1 week if 2 insulin types; 30 days for one
Administration of Insulin
- Usually available as U100 insulin (1 mL contains 100 Units of insulin)
- Syringes marked for units: various sizes
- Only self-administering user recaps syringe
- No alcohol swab for self-injection (wash with soap and water daily)
- Inject at 45-90 degree angle into fatty tissue-SQ
Administration of insulin
- Subcutaneous injection
- Absorption most consistent in: abdomen, followed by arm, thigh, and buttock
- Do not inject in site to be exercised
- Rotate injections within and between sites
- Regular insulin may be given IV
- Cannot be taken orally
Practice Case Study
You are caring for M.W. M.W. is hospitalized for pneumonia and has type 2 diabetes, insulin dependent. Using the orders and chart on the next slide, please determine how much insulin lispro (humalog) to give before each meal, based on the accu check values below:
0800 (pre breakfast) accucheck 210
1200 (pre lunch) accucheck 155
1700 (pre dinner) accucheck 188
How much insulin Lispro will you give at:
0800 -
1200-
1700 -
0800 10 units
1200 6 units
1700 6 units
35
Insulin Pumps
- Continuous subcutaneous infusion
- Battery-operated device
- Connected to catheter inserted into subcutaneous tissue in abdominal wall
- Program basal and bolus doses that can vary throughout the day
- Potential for keeping blood glucose levels in a tighter range
Continuous Glucose Monitoring
- CGM’s becoming more popular
- Know your institution’s policy on these!
Problems with Insulin Therapy
- Hypoglycemia
- Allergic reaction
- Lipodystrophy
Somogyi Effect
- Occurs when high doses of insulin cause night time hypoglycemia
- Usually occurs overnight after HS insulin administration
- Release of counterregulatory hormones then causes rebound hyperglycemia in the morning
Dawn Phenomenon
- Morning hyperglycemia present on awakening
- May be due to release of counterregulatory hormones in predawn hours
- Growth hormone and cortisol
- not associated with nighttime hypoglycemia
Inhaled Insulin
- Afrezza
- Rapid-acting inhaled insulin
- Administered at beginning of each meal or within 20 minutes after starting a meal
- Not a substitute for long-acting insulin
Oral Agents
- Address 3 defects of type 2 diabetes
- Insulin resistance
- Decreased insulin production
- Increased hepatic glucose production
- Different types can be used in combination
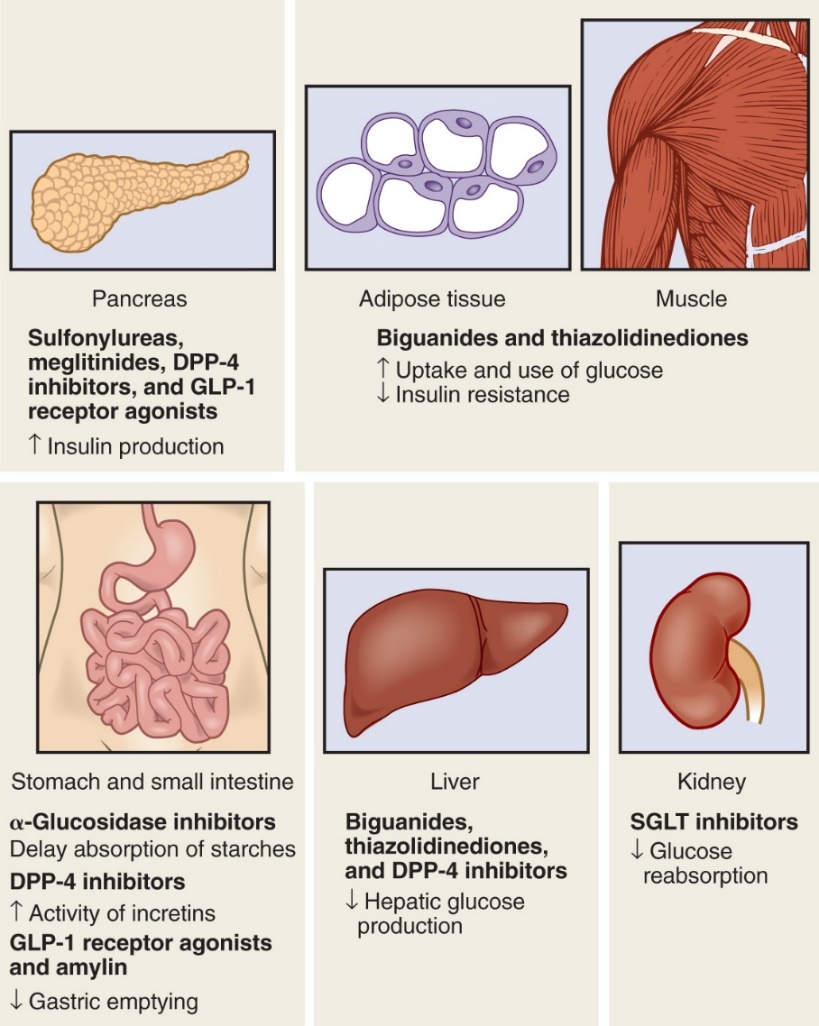
Biguanides
- Metformin (Glucophage)
- Reduces glucose production by liver
- Enhances insulin sensitivity
- Improves glucose transport
- May cause weight loss
- Used in prevention of type 2 diabetes
- Side effects:
- usually GI- NVD, upset stomach
Biguanides: Nursing considerations
- take with food to avoid GI upset
- Withhold if patient undergoing surgery or radiologic procedure with contrast medium
- 1-2 days before and at least 48 hours after
- Monitor serum creatinine
- Contraindications
- Renal, liver, cardiac disease
- Excessive alcohol intake
Sulfonylureas
- MOA: Increase insulin production from pancreas
- Major side effect: hypoglycemia
- alcohol can cause disulfiram reaction
- Nursing: teach about s/s of hypoglycemia/tx
Examples
- Glipizide (Glucotrol)
- Glyburide (Glynase)
- Glimepiride (Amaryl)
Meglitinides
- MOA: Increase insulin production from pancreas
- Rapid absorption and elimination = less hypoglycemia
- SE: hypoglycemia, sweating
- Taken 30 minutes to just before each meal
- Nursing/education: Should not be taken if meal skipped, s/s of hypoglycemia and tx
- Examples:
- Repaglinide (Prandin)
- Nateglinide (Starlix)
- Examples:
α-Glucosidase Inhibitors
- “Starch blockers” – slow down absorption of carbohydrate in small intestine
- SE: GI upset, flatulence, diarrhea
- Nursing/education: Take with first bite of each meal, s/s of hypoglycemia and tx
- Examples:
- Acarbose (Precose)
- Miglitol (Glyset)
Thiazolidinediones
- Most effective in those with insulin resistance
- Improve insulin sensitivity, transport, and utilization at target tissues
- SE: fluid retention, edema
- Nursing/education: s/s hypoglycemia and tx
- Examples:
- Pioglitazone (Actos)
- Rosiglitazone (Avandia)
- Rarely used because of adverse effects
Dipeptidyl Peptidase-4 (DDP-4) Inhibitors
- MOA: Blocks inactivation of incretin hormones resulting in…
- Increased insulin release
- Decreased glucagon secretion
- Decreased glucose production
- SE: HA, arthralgia, increased risk of UTI
- Nursing/education: s/s hypoglycemia and tx
- Examples (“gliptins”):
- Sitagliptin (Januvia)
- Saxagliptin (Onglyza)
- Linagliptin (Tradjenta)
Sodium-Glucose Co-Transporter 2 (SGLT2) Inhibitors
- MOA:
- Block reabsorption of glucose by kidney
- Increasing glucose excretion
- Lowering blood glucose levels
- SE: increased risk of UTI, yeast infections
- Nursing/education: s/s hypoglycemia and tx
Examples (“gliflozins”):
- Canagliflozin (Invokana)
- Dapagliflozin (Farxiga)
- Empagliflozin (Jardiance)
Glucagonlike Peptide-1 Receptor Agonists
- MOA: Simulate GLP-1…
- Increase insulin synthesis and release
- Inhibit glucagon secretion
- Slow gastric emptying
- Increases satiety
- SE: GI upset, nausea, site reaction
- Nursing/education: teach about injections, s/s hypoglycemia and tx
- Examples: injectable
- Exenatide (Byetta)
- Liraglutide (Victoza)
Amylin Analog
- MOA: Slows gastric emptying, reduces postprandial glucagon secretion, increases satiety
- injectable
- Only one: Pramlintide (Symlin)
- Used concurrently with insulin
- Subq in thigh or abdomen before meals
- Watch for hypoglycemia: must eat!
Drug Therapy
- Combination Oral Therapy
- Blends two different classes together
- Improves adherence because fewer pills to take
- eg. Janumet (sitagliptin and metformin)
- Consider other drugs affecting blood glucose
- Drug/substance interactions can potentiate hypoglycemia and hyperglycemia effects
Treating hypoglycemia
- Prevention is best
- Treat with 2-4 oz fruit juice or sugary drink
- Dextrose tablets
Remembering Lecutre 1
- Rapid-acting insulin:
- Examples: Lispro (Humalog), Aspart (NovoLog), Glulisine (Apidra)
- Characteristics: Quick onset, short duration
- Mnemonic: "LAG" - Lispro, Aspart, Glulisine
- Short-acting insulin:
- Example: Regular insulin (Humulin R, Novolin R)
- Characteristics: Slower onset than rapid-acting, short duration
- Mnemonic: "R for Regular"
- Intermediate-acting insulin:
- Examples: NPH insulin (Humulin N, Novolin N)
- Characteristics: Intermediate duration
- Mnemonic: "NPH" - stands for Neutral Protamine Hagedorn
- Long-acting insulin:
- Examples: Glargine (Lantus), Detemir (Levemir), Degludec (Tresiba)
- Characteristics: Long duration, provides basal insulin coverage
- Mnemonic: "Glide Long and Deep" - Glargine, Detemir, Degludec
Now, you can use the mnemonic "LAG, R, NPH, Glide Long and Deep" to remember the different kinds of insulin. Additionally, consider creating flashcards or charts to reinforce your memory, and repetition is key to retention. Practice recalling the information regularly to solidify your understanding.
Acute Complications of Diabetes Mellitus
Learning Objectives
- Explain acute complications of DM including DKA, HHS, and hypoglycemia
- Explain and identify chronic complications of DM
- Describe management and treatment for these complications
- Identify gerontologic considerations for patients with DM
Be on the lookout for…
- Diabetic ketoacidosis (DKA)
- Hyperosmolar hyperglycemic syndrome (HHS)
- Hypoglycemia
- The acute complications of diabetes mellitus arise from events associated with hyperglycemia and hypoglycemia.
- Hyperglycemia occurs when there is not enough insulin working, and hypoglycemia occurs when there is too much insulin working.
- It is important for the HCP to distinguish between hyperglycemia and hypoglycemia because hypoglycemia worsens rapidly and is a serious threat if action is not immediately taken.
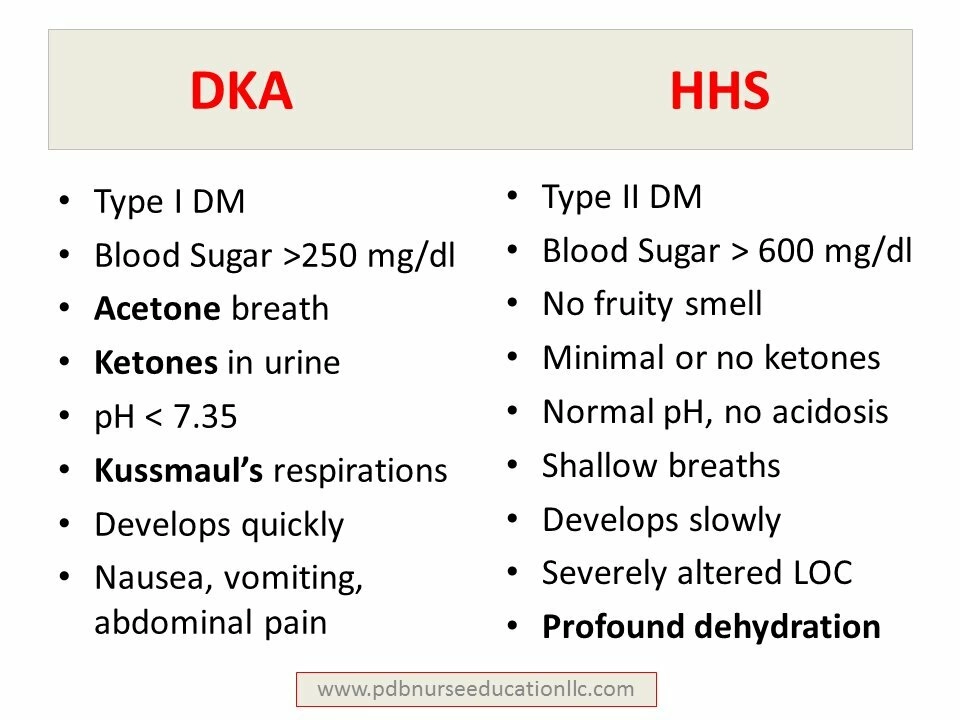
Diabetic Ketoacidosis (DKA)
- Cause: profound deficiency of insulin
- Characterized by
- Hyperglycemia
- Ketosis
- Acidosis
- Dehydration
- Most likely to occur in type 1 DM
- Precipitating factors
- Diabetic ketoacidosis (DKA) is caused by a profound deficiency of insulin and is characterized by hyperglycemia, ketosis, acidosis, and dehydration.
- It is most likely to occur in people with type 1 diabetes but may be seen in people with type 2 diabetes in conditions of severe illness or stress when the pancreas cannot meet the extra demand for insulin.
- Precipitating factors include illness and infection (stress), inadequate insulin dosage, undiagnosed type 1 diabetes, poor self-management, and neglect.
- When the circulating supply of insulin is insufficient, glucose cannot be properly used for energy. The body compensates by breaking down fat stores as a secondary source of fuel.
- Ketones are acidic by-products of fat metabolism that can cause serious problems when they become excessive in the blood. Ketosis alters the pH balance, causing metabolic acidosis to develop.
- Ketonuria is a process that occurs when ketone bodies are excreted in the urine. During this process, electrolytes become depleted as cations are eliminated along with the anionic ketones in an attempt to maintain electrical neutrality.
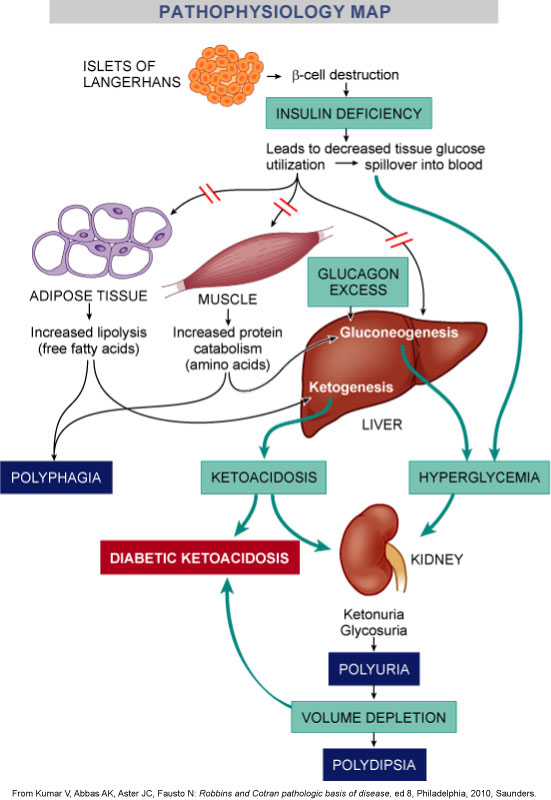
- Insulin deficiency impairs protein synthesis and causes excessive protein degradation. This results in nitrogen losses from the tissues.
- Insulin deficiency also stimulates the production of glucose from amino acids (from proteins) in the liver and leads to further hyperglycemia.
- Because there is a deficiency of insulin, the additional glucose cannot be used and the blood glucose level rises further, adding to the osmotic diuresis.
If not treated, the patient will develop severe depletion of sodium, potassium, chloride, magnesium, and phosphate.
- Vomiting caused by the acidosis results in more fluid and electrolyte losses.
- Eventually, hypovolemia will ensue and be followed by shock.
- Renal failure, which may eventually occur from hypovolemic shock, causes the retention of ketones and glucose, and the acidosis progresses.
- Untreated, the patient becomes comatose as a result of dehydration, electrolyte imbalance, and acidosis. If the condition is not treated, death is inevitable.
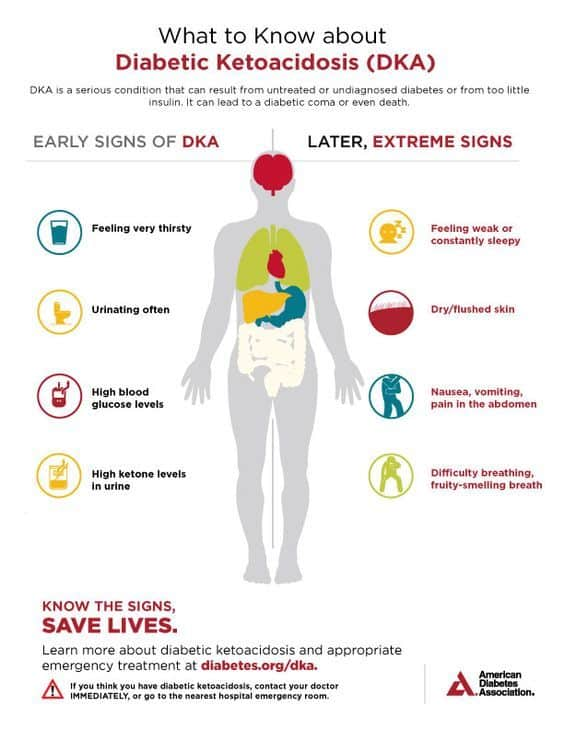 feeling thirsty, high BS, high ketones levels.
feeling thirsty, high BS, high ketones levels.
DKA: Clinical Manifestations
- Dehydration
- Poor skin turgor
- Dry mucous membranes
- Tachycardia
- Orthostatic hypotension
- Lethargy and weakness early
- Skin dry and loose; eyes soft and sunken
- Abdominal pain, anorexia, nausea/vomiting
- Kussmaul respirations
- Sweet, fruity breath odor
- Blood glucose level of ≥ 250 mg/dL
- Blood pH lower than 7.30
- Serum bicarbonate level < 16 mEq/L
- Moderate to high ketone levels in urine or serum
- Dehydration occurs in DKA with manifestations of poor skin turgor, dry mucous membranes, tachycardia, and orthostatic hypotension.
- Early symptoms may include lethargy and weakness.
- As the patient becomes severely dehydrated, the skin becomes dry and loose, and the eyes become soft and sunken.
- Abdominal pain may be present and accompanied by anorexia, nausea, and vomiting.
- Kussmaul respirations (rapid, deep breathing associated with dyspnea) are the body’s attempt to reverse metabolic acidosis through the exhalation of excess carbon dioxide.
- Acetone is noted on the breath as a sweet, fruity odor.
- Laboratory findings include a blood glucose level of 250 mg/dL (13.9 mmol/L) or higher, arterial blood pH less than 7.30, serum bicarbonate level less than 16 mEq/L (16 mmol/L), and moderate to high ketone levels in the urine or serum.
DKA: Treatment
- Outpatient v. Inpatient
- Ensure patent airway; administer O2
- Establish IV access; begin fluid resuscitation
- NaCl 0.45% or 0.9%
- When BG = approx 250, add 5% dextrose to prevent hypogylcemia or sudden drop in BG
- Continuous regular insulin drip 0.1 U/kg/hr
- Potassium replacement as needed
- Before the advent of self-monitoring of blood glucose, patients with DKA required hospitalization for treatment.
- Today, hospitalization may not be required.
- When fluid and electrolyte imbalances are not severe and blood glucose levels can be safely monitored at home, less severe forms of DKA may be managed on an outpatient basis.
- Other factors that are considered in decisions of where the patient is managed include the presence of fever, nausea/vomiting, and diarrhea; altered mental status; nature of the cause of the ketoacidosis; and availability of frequent communication with the HCP (every few hours).
- Patients with DKA who have an illness such as pneumonia or a urinary tract infection are usually admitted to the hospital.
- DKA is a serious condition that proceeds rapidly and must be treated promptly.
- Ensure an patent airway and administer oxygen via nasal cannula or non-rebreather mask.
- Because fluid imbalance is potentially life-threatening, the initial goal of therapy is to establish IV access and begin fluid and electrolyte replacement.
- Typically, the initial fluid therapy regimen consists of an infusion of 0.45% or 0.9% NaCl at a rate to restore urine output to 30 to 60 mL/hr and to raise blood pressure.
- When blood glucose levels approach 250 mg/dL (13.9 mmol/L), add 5% to 10% dextrose to the fluid regimen to prevent hypoglycemia, as well as a sudden drop in glucose that can be associated with cerebral edema.
- Overzealous rehydration, especially with hypotonic IV solutions, can result in cerebral edema.
- Monitor patients with renal or cardiac compromise for fluid overload.
- Measure serum potassium level before starting insulin. If the patient is hypokalemic, insulin administration will further decrease the potassium levels, making early potassium replacement is essential. Although initial serum potassium value may be normal or high, levels can decrease rapidly once therapy starts, as insulin drives potassium into the cells, leading to life-threatening hypokalemia.
- IV insulin administration is therapy directed toward correcting hyperglycemia and hyperketonemia.
- Insulin is immediately started at 0.1 U/kg/hr by a continuous infusion.
- It is important to prevent rapid drops in serum glucose to avoid cerebral edema. A blood glucose reduction of 36 to 54 mg/dL (2 to 3 mmol/L) per hour will avoid complications.
- Insulin allows water and potassium to enter the cell along with glucose and can lead to a depletion of vascular volume and hypokalemia; therefore, monitor the patient’s fluid balance and potassium levels
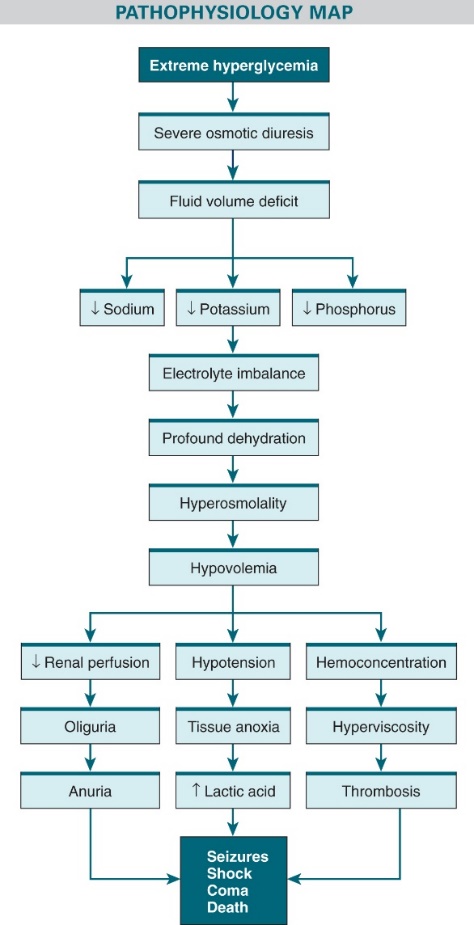
Hyperosmolar Hyperglycemic Syndrome (HHS)
- Life-threatening syndrome
- Occurs with type 2 diabetes
- Precipitating factors
- UTIs, pneumonia, sepsis
- Acute illness
- Newly diagnosed type 2 diabetes
- Impaired thirst sensation and/or inability to replace fluids
- Hyperosmolar hyperglycemic syndrome (HHS) is a life-threatening syndrome that can occur in the patient with diabetes who is able to produce enough insulin to prevent DKA but not enough to prevent severe hyperglycemia, osmotic diuresis, and extracellular fluid depletion.
- HHS is less common than DKA. It often occurs in patients older than 60 years with type 2 diabetes.
- Common causes of HHS are urinary tract infections, pneumonia, sepsis, any acute illness, and newly diagnosed type 2 diabetes.
- HHS is often related to impaired thirst sensation and/or a functional inability to replace fluids.
- There is usually a history of inadequate fluid intake, increasing mental depression, and polyuria.
- Hyperosmolar hyperglycemic syndrome (HHS) is a life-threatening syndrome that can occur in the patient with diabetes who is able to produce enough insulin to prevent DKA but not enough to prevent severe hyperglycemia, osmotic diuresis, and extracellular fluid depletion.
- HHS is less common than DKA. It often occurs in patients older than 60 years with type 2 diabetes.
- Common causes of HHS are urinary tract infections, pneumonia, sepsis, any acute illness, and newly diagnosed type 2 diabetes.
- HHS is often related to impaired thirst sensation and/or a functional inability to replace fluids.
- There is usually a history of inadequate fluid intake, increasing mental depression, and polyuria.
HHS: Clinical Manifestations
- Enough circulating insulin to prevent ketoacidosis
- Fewer symptoms lead to higher glucose levels (>600 mg/dL)
- More severe neurologic manifestations because of ↑ serum osmolality
- Ketones absent or minimal in blood and urine
- The main difference between HHS and DKA is that the patient with HHS usually has enough circulating insulin so that ketoacidosis does not occur.
- Because HHS produces fewer symptoms in the earlier stages, blood glucose levels can climb quite high before the problem is recognized.
- The higher blood glucose levels increase serum osmolality and produce more severe neurologic manifestations, such as somnolence, coma, seizures, hemiparesis, and aphasia.
- Because these manifestations resemble a stroke, immediate determination of the glucose level is critical for correct diagnosis and treatment.
- Laboratory values in HHS include a blood glucose level greater than 600 mg/dL (33.33 mmol/L) and a marked increase in serum osmolality.
- Ketone bodies are absent or minimal in both blood and urine.
HHS: Treatment
- Medical emergency
- High mortality rate
- Therapy similar to that for DKA
- IV insulin and NaCl infusions
- More fluid replacement needed
- Monitor serum potassium and replace as needed
- Correct underlying precipitating cause
- HHS constitutes a medical emergency and has a high mortality rate.
- The management of DKA and that of HHS are similar and includes immediate IV administration insulin and either 0.9% or 0.45% NaCl.
- HHS usually necessitates greater volumes of fluid replacement. This should be accomplished slowly and carefully.
- Patients with HHS are commonly older and may have cardiac or renal compromise, necessitating hemodynamic monitoring to avoid fluid overload during fluid replacement.
- When blood glucose levels fall to approximately 250 mg/dL (13.9 mmol/L), IV fluids containing dextrose are administered to prevent hypoglycemia.
- Electrolytes are monitored and replaced as needed. Hypokalemia is not as significant in HHS as it is in DKA, although fluid losses may result in milder potassium deficits that necessitate replacement.
- Assess vital signs, intake and output, tissue turgor, laboratory values, and cardiac monitoring to check the efficacy of fluid and electrolyte replacement. This includes monitoring of serum osmolality and frequent assessment of cardiac, renal, and mental status.
- Once the patient is stabilized, attempts to detect and correct the underlying precipitating cause should be initiated.
DKA & HHS: Nursing Management
- Monitor
- IV fluids
- Insulin therapy
- Electrolytes
- Assess
- Renal status
- Cardiopulmonary status
- Level of consciousness
- Closely monitor blood glucose and urine for output and ketones, as well laboratory data to determine appropriate patient care.
- Monitor the administration of (1) IV fluids to correct dehydration, (2) insulin therapy to reduce blood glucose and serum acetone levels, and (3) electrolytes given to correct electrolyte imbalance.
- Assess renal status and cardiopulmonary status related to hydration and electrolyte levels.
- Monitor the level of consciousness.
- Assess for signs of potassium imbalance resulting from hypoinsulinemia and osmotic diuresis.
- When treatment with insulin begins, serum potassium levels may decrease rapidly as potassium moves into the cells once insulin becomes available. This movement of potassium into and out of extracellular fluid influences cardiac functioning.
- Cardiac monitoring is a useful aid in detecting hyperkalemia and hypokalemia because characteristic changes indicating potassium excess or deficit are observable on electrocardiographic tracings.
- Assess vital signs often to determine the presence of fever, hypovolemic shock, tachycardia, and Kussmaul respirations.
Hypoglycemia
- Too much insulin in proportion to glucose in the blood
- Blood glucose level < 70 mg/dL
- Neuroendocrine hormones released
- Autonomic nervous system activated
- Common Manifestations:
- Shakiness
- Palpitations
- Nervousness
- Diaphoresis
- Anxiety
- Hunger
- Pallor
- Hypoglycemia, or low blood glucose level, occurs when there is too much insulin in proportion to available glucose in the blood.
- This causes the blood glucose level to drop to less than 70 mg/dL (3.9 mmol/L).
- When plasma glucose level drops below 70 mg/dL (3.9 mmol/L), neuroendocrine hormones are released, and the autonomic nervous system is activated.
Hypoglycemia
- Altered mental functioning
- Difficulty speaking
- Visual disturbances
- Stupor
- Confusion
- Coma
- Untreated hypoglycemia can progress to loss of consciousness, seizures, coma, and death
- HYPOGLYCEMIA UNAWARENESS
- Because the brain requires a constant supply of glucose in sufficient quantities to function properly, hypoglycemia can affect mental functioning.
- The manifestations are speaking difficulties, visual disturbances, stupor, confusion, and coma.
- Manifestations of hypoglycemia can mimic those of alcohol intoxication.
- Untreated hypoglycemia can progress to loss of consciousness, seizures, coma, and death.
- Hypoglycemia unawareness is a condition in which a person does not experience the warning signs and symptoms of hypoglycemia until the glucose levels reach a critical point. Then the person may become incoherent and combative or lose consciousness.
- This is often related to autonomic neuropathy of diabetes that interferes with the secretion of counterregulatory hormones that produce these symptoms.
- Patients at risk for hypoglycemia unawareness include those who have had repeated episodes of hypoglycemia, older patients, and patients who use β-adrenergic blockers.
- Using intensive treatment to get tight blood glucose levels in patients who are at risk for hypoglycemia unawareness may not be an appropriate goal because a major drawback is hypoglycemia.
- These patients are usually managed with blood glucose goals that are somewhat higher than those of patients who are able to detect and manage the onset of hypoglycemia.
Causes of Hypoglycemia
- Causes
- Too much insulin or oral hypoglycemic agents
- Too little food
- Delaying time of eating
- Too much exercise- check blood sugar frequently
- Symptoms can also occur when high glucose level falls too rapidly
- Causes of hypoglycemia are often related to a mismatch in the timing of food intake and the peak action of insulin or oral hypoglycemic agents that increase endogenous insulin secretion.
- The balance between blood glucose and insulin can be disrupted by administering too much insulin or medication, ingesting too little food, delaying the time of eating, and performing unusual amounts of exercise.
- Hypoglycemia can occur at any time, but most episodes occur when the OA or insulin is at its peak of action or when the patient’s daily routine is disrupted without adequate adjustments in diet, medications, and activity. Although hypoglycemia is more common with insulin therapy, it can occur with OAs, and it may be severe and persist for an extended time because of the longer duration of action of these drugs.
- Symptoms of hypoglycemia may occur when a very high blood glucose level falls too rapidly (e.g., a blood glucose level of 300 mg/dL [16.7 mmol/L] falling quickly to 180 mg/dL [10 mmol/L]).
- Although the blood glucose level is above normal by definition and measurement, the sudden metabolic shift can evoke hypoglycemia symptoms. Overly vigorous management of hyperglycemia with insulin can cause this type of situation.
Hypoglycemia: Treatment
- Check blood glucose level
- If < 70 mg/dL, begin treatment
- If > 70 mg/dL, investigate further for cause of signs/symptoms
- If monitoring equipment not available, treatment should be initiated
- Treatment: rule of 15
- Consume 15 g of a simple carbohydrate
- Fruit juice or regular soft drink, 4 to 6 oz
- Consume 15 g of a simple carbohydrate
- Recheck glucose level in 15 minutes
- Repeat 15 gm of simple carbohydrate if still < 70 gm/dL
- Avoid foods with fat
- Decrease absorption of sugar
- Avoid overtreatment
- Give complex CHO after recovery
- Hypoglycemia can usually be quickly reversed with effective treatment.
- At the first sign of hypoglycemia, check the blood glucose level if possible.
- If it is less than 70 mg/dL (3.9 mmol/L), immediately begin treatment for hypoglycemia.
- If the blood glucose is greater than 70 mg/dL (3.9 mmol/L), investigate other possible causes of the signs and symptoms.
- If the patient has manifestations of hypoglycemia and monitoring equipment is not available or the patient has a history of fluctuating blood glucose levels, hypoglycemia should be assumed and treatment should be initiated.
- Follow the “Rule of 15” to treat hypoglycemia.
- A blood glucose level less than 70 mg/dL is treated by ingestion of 15 g of a simple (fast-acting) carbohydrate, such as 4 to 6 oz of fruit juice or a regular soft drink.
- Commercial products such as gels or tablets containing specific amounts of glucose are convenient for carrying in a purse or pocket to be used in such situations.
- Recheck the blood glucose level 15 minutes later. If the value is still less than 70 mg/dL, ingest 15 g more of carbohydrate and recheck the blood glucose in 15 minutes.
- If there is no significant improvement in the patient’s condition after two to three doses of 15 g of simple carbohydrate, contact the HCP.
- After an acute episode of hypoglycemia, have the patient ingest a complex carbohydrate after recovery to prevent repeat hypoglycemia.
- Avoid treatment with carbohydrates that contain fat, such as candy bars, cookies, whole milk, and ice cream.
- The fat in those foods will slow down the absorption of the sugar and delay the response to treatment.
- Avoid overtreatment with large quantities of quick-acting carbohydrates so that a rapid fluctuation to hyperglycemia does not occur.
Hypoglycemia: Treatment cont’d
- Treatment
- In acute care settings if patient not alert enough to swallow
- Fifty percent dextrose 20 to 50 mL IV push
- Glucagon 1 mg IM or subcutaneously
- In acute care settings if patient not alert enough to swallow
- Explore reason why occurred
- In an acute care setting, patients with hypoglycemia may be treated with 20 to 50 mL of 50% dextrose, IV push.
- If the patient is not alert enough to swallow and no IV access is available, another option is to administer 1 mg of glucagon by intramuscular (IM) or subcutaneous injection.
- An IM injection in a site such as the deltoid muscle will result in a quicker response.
- Glucagon stimulates a strong hepatic response to convert glycogen to glucose and therefore makes glucose rapidly available.
- Nausea is a common reaction after glucagon injection.
- Therefore, to prevent aspiration if vomiting occurs, turn the patient on the side until he or she becomes alert.
- Once the acute hypoglycemia has been reversed, explore with the patient the reasons why the situation developed. This assessment may indicate the need for additional teaching of the patient and the family to avoid future episodes of hypoglycemia.
Chronic Complications of Diabetes Mellitus
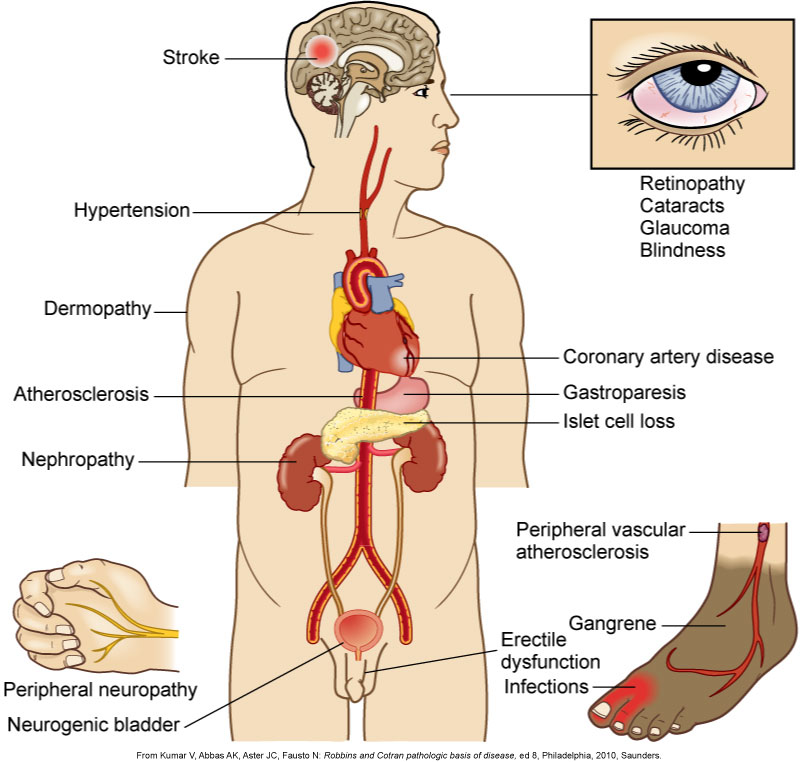
- Patients with diabetes can decrease several risk factors associated with macrovascular complications, such as obesity, smoking, hypertension, high fat intake, and sedentary lifestyle. Smoking, which is detrimental to health in general, is especially injurious to people with diabetes and significantly increases their risk for blood vessel and cardiovascular disease (CVD), stroke, and lower extremity amputation. The ADA recommends yearly screening for CVD risk factors in people with diabetes.
- Optimizing BP control in patients with diabetes is significant for the prevention of cardiovascular and renal disease.
- Treating hypertension in those with diabetes results in a decrease in macrovascular and microvascular complications. Hypertension causes an increase in mortality rate among people with diabetes in comparison with those with hypertension without diabetes. A target BP of less than 140/90 mm Hg is recommended for all patients with diabetes.
- Patients with diabetes have an increase in lipid abnormalities.
- This contributes to the increase in cardiovascular disease seen in this population. The American Diabetes Association recommends the LDL cholesterol goal of less than 100 mg/dL (2.6 mmol/L), triglyceride levels of less than 150 mg/dL (1.7 mmol/L), and HDL cholesterol levels greater than 40 mg/dL (1.0 mmol/L) in men and greater than 50 mg/dL (1.3 mmol/L) in women as target values.
- The ADA advocates lifestyle interventions including nutritional therapy, exercise, and weight loss and smoking cessation to treat hyperlipidemia.
- In patients over age 40 years, and if clinically indicated, statin treatment is used in addition to lifestyle therapy. In patients under 40 years of age and in those with type 1 diabetes, treatment with a statin is used if the patient has increased CVD risk factors.
- The earliest and most treatable stages of diabetic retinopathy often produce no changes in the vision.
- Therefore, patients with type 2 diabetes should have an eye examination with pupil dilation by an ophthalmologist or a specially trained optometrist at the time of diagnosis and annually thereafter for early detection and treatment.
- A person with type 1 diabetes should have the eye examined with dilation within 5 years after the onset of diabetes and then repeat this examination annually.
- The best approach to the management of diabetes-related eye disease is to prevent it by maintaining healthy blood glucose levels and managing hypertension.
- Patients with diabetes are screened for nephropathy annually for albuminuria and a measurement of the albumin-to-creatinine ratio in a random spot urine collection. Serum creatinine is also measured. Serum creatinine measurements provide an estimation of the glomerular filtration rate and thus the degree of kidney function.
- Patients with diabetes who have albuminuria receive either angiotensin-converting enzyme (ACE) inhibitor drugs (e.g., lisinopril [Prinivil, Zestril]) or angiotensin II receptor antagonists (e.g., losartan [Cozaar]).
- Both classifications of these drugs are used to treat hypertension and have been found to delay the progression of nephropathy in patients with diabetes.
- Hypertension will significantly accelerate the progression of nephropathy. Therefore, aggressive blood pressure management is indicated for all patients with diabetes. Keeping blood glucose levels in a healthy range is also critical for the prevention and delay of diabetes-related nephropathy.
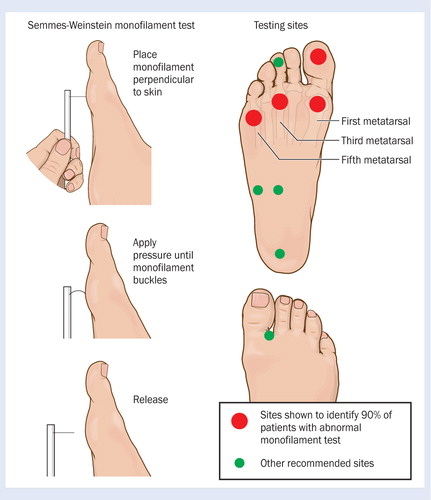
Diabetic Neuropathy: Sensory and Autonomic
- Microvascular and nerve damage due to metabolic derangements of diabetes
- 60% to 70% of patients with diabetes have some degree of neuropathy
- Reduced nerve conduction and demyelinization
- Sensory and/ or autonomic
- Sensory neuropathy
- Loss of protective sensation in lower extremities
- Major risk for amputation
- Distal symmetric polyneuropathy
- Diabetic neuropathy is nerve damage that occurs because of the metabolic derangements associated with diabetes mellitus.
- Approximately 60% to 70% of patients with diabetes have some degree of neuropathy.
- Screening for neuropathy begins in patients with type 2 diabetes at the time of diagnosis and 5 years after diagnosis in patients with type 1 diabetes.
- The pathophysiologic processes of diabetic neuropathy are not well understood.
- Several theories exist, including metabolic, vascular, and autoimmune factors.
- The prevailing theory is that persistent hyperglycemia leads to an accumulation of sorbitol and fructose in the nerves that causes damage by an unknown mechanism.
- The result is reduced nerve conduction and demyelinization.
- Ischemia in blood vessels damaged by chronic hyperglycemia that supply the peripheral nerves is also implicated in the development of diabetes-related neuropathy.
- Neuropathy can precede, accompany, or follow the diagnosis of diabetes.
- The two major categories of diabetes-related neuropathy are sensory neuropathy, which affects the peripheral nervous system, and autonomic neuropathy. Each of these types can take several forms.
- Sensory neuropathy: This can lead to the loss of protective sensation in the lower extremities, and, coupled with other factors, this significantly increases the risk for complications that result in a lower limb amputation.
- The most common form of sensory neuropathy is distal symmetric polyneuropathy, which affects the hands and/or feet bilaterally.
- This is sometimes referred to as stocking-glove neuropathy.
- Characteristics of distal symmetric polyneuropathy include loss of sensation, abnormal sensations, pain, and paresthesias.
- The pain, which is often described as burning, cramping, crushing, or tearing, is usually worse at night and may occur only at that time.
- The paresthesias may be associated with tingling, burning, and itching sensations.
- The patient may report a feeling of walking on pillows or numb feet.
- At times the skin becomes so sensitive (hyperesthesia) that even light pressure from bed sheets cannot be tolerated.
- Complete or partial loss of sensitivity to touch and temperature is common.
- Foot injury and ulcerations can occur without the patient’s ever having pain. Neuropathy can also cause atrophy of the small muscles of the hands and feet, causing deformity and limiting fine movement.
Sensory Neuropathy: Treatment
- Managing blood glucose levels
- Drug therapy
- Topical creams
- Tricyclic antidepressants
- Selective serotonin and norepinephrine reuptake inhibitors
- Antiseizure medications
- Managing blood glucose is the only treatment for diabetes-related neuropathy. It is effective in many, but not all, cases.
- Drug therapy may be used to treat neuropathic symptoms, particularly pain.
- Medications commonly used include topical creams (e.g., capsaicin [Zostrix]), tricyclic antidepressants (e.g., amitriptyline [Elavil]), selective serotonin and norepinephrine reuptake inhibitors (e.g., duloxetine [Cymbalta]), and antiseizure medications (e.g., gabapentin [Neurontin], pregabalin [Lyrica]).
- Capsaicin is a moderately effective topical cream made from chili peppers. It depletes the accumulation of pain-mediating chemicals in the peripheral sensory neurons. The cream is applied three to four times a day. There is usually an increase in symptoms at the start of therapy, which is followed by relief of pain in 2 to 3 weeks.
- Tricyclic antidepressants are moderately effective in treating the symptoms of diabetic neuropathy. They work by inhibiting the reuptake of norepinephrine and serotonin, which are neurotransmitters believed to play a role in the transmission of pain through the spinal cord. Duloxetine is thought to relieve pain by increasing the levels of serotonin and norepinephrine, which improves the body’s ability to regulate pain.
- Antiseizure medications decrease the release of neurotransmitters that transmit pain.
Autonomic Neuropathy
- Can affect nearly all body systems
- Gastroparesis
- Delayed gastric emptying
- Cardiovascular abnormalities
- Postural hypotension, resting tachycardia, painless myocardial infarction
- Sexual function
- Erectile dysfunction
- Decreased libido
- Vaginal infections
- Neurogenic bladder → urinary retention
- Empty frequently, use Credé’s maneuver
- Medications
- Self-catheterization
- Autonomic neuropathy can affect nearly all body systems and lead to hypoglycemia unawareness, bowel incontinence and diarrhea, and urinary retention.
- Gastroparesis (delayed gastric emptying) is a complication of autonomic neuropathy that can produce anorexia, nausea, vomiting, gastroesophageal reflux, and persistent feelings of fullness. Gastroparesis can trigger hypoglycemia by delaying food absorption.
- Cardiovascular abnormalities associated with autonomic neuropathy are postural hypotension, resting tachycardia, and painless myocardial infarction. Assess patients with diabetes for postural hypotension to determine if they are at risk for falls. Instruct the patient with postural hypotension to change from a lying or sitting position slowly.
- Diabetes can affect sexual function in men and women.
- Erectile dysfunction (ED) in men with diabetes is well recognized and common, often being the first manifestation of autonomic neuropathy. ED in diabetes is also associated with other factors, including vascular disease, elevated blood glucose levels, endocrine disorders, psychogenic factors, and medications.
- Decreased libido is a problem for some women with diabetes.
- Candidal and nonspecific vaginitis are also common.
- ED or sexual dysfunction necessitates sensitive therapeutic counseling for both the patient and the patient’s partner.
- A neurogenic bladder may develop as the sensation in the inner bladder wall decreases, causing urinary retention.
- A patient with retention has infrequent voiding, difficulty in voiding, and a weak stream of urine.
- Emptying the bladder every 3 hours in a sitting position helps prevent stasis and subsequent infection.
- Tightening the abdominal muscles during voiding and using Credé’s maneuver (mild massage downward over the lower abdomen and bladder) may also help with complete bladder emptying.
- Cholinergic agonist drugs such as bethanechol (Urecholine) may be used. The patient may also need to learn self-catheterization
Preventing Foot Complications
- Patient teaching to prevent foot ulcers-daily checks
- Proper footwear/socks
- Avoidance of foot injury
- Skin and nail care
- Daily inspection of feet
- Prompt treatment of small problems
- Diligent wound care for foot ulcers
- Neuropathic arthropathy (Charcot’s foot)
- If the patient has LOPS or PAD, aggressive measures must be taken to teach the patient how to prevent foot ulcers. These measures include the selection of proper footwear, including prescription shoes. Other measures are to carefully avoid injury to the foot, practice diligent skin and nail care, inspect the foot thoroughly each day, and treat small problems promptly.
- Proper care of a foot ulcer is critical for wound healing.
- Several forms of treatment can be used for management of the foot ulcers.
- Casting can be done to redistribute the weight on the plantar surface of the foot.
- Wound care for the ulcer can include debridement, dressings, advanced wound healing products (becaplermin [Regranex]), vacuum-assisted closure, ultrasonography, hyperbaric oxygen, and skin grafting.
- Neuropathic arthropathy, or Charcot’s foot, results in ankle and foot changes that ultimately lead to joint dysfunction and footdrop. These changes occur gradually and promote an abnormal distribution of weight over the foot, further increasing the chances of developing a foot ulcer as new pressure points emerge. Foot deformity should be recognized early and proper footwear fitted before ulceration occurs.
Charcot foot
Monofilament testing of feet
Skin Problems
- Diabetic dermopathy
- Most common
- Red-brown, round or oval patches
- Acanthosis nigricans
- Manifestation of insulin resistance
- Velvety light brown to black skin
- Necrobiosis lipoidica diabeticorum
- Red-yellow lesions
- Up to two thirds of persons with diabetes develop skin problems.
- Diabetes-related dermopathy, the most common diabetic skin lesion, is characterized by reddish-brown and round or oval patches. They initially are scaly and then flatten out and become indented. The lesions appear most frequently on the shins but can also be found on the front of the thighs, forearm, side of the foot, scalp, and trunk.
- Acanthosis nigricans is a manifestation of insulin resistance. It can appear as a velvety light brown to black skin thickening seen predominantly on flexures, axillae, and the neck.
- Necrobiosis lipoidica diabeticorum usually appears as red-yellow lesions, with atrophic skin that becomes shiny and transparent, revealing tiny blood vessels under the surface. (an uncommon finding!!!)
ACANTHOSIS NIGRICANS

necrobiosis lipoidica diabeticorum

Other Chronic Complications of Diabetes
- Infection
- Psychologic
- Depression
- lifestyle changes
- Anxiety
- disordered eating
- A person with diabetes is more susceptible to infections. This is due to a defect in the mobilization of inflammatory cells and impaired phagocytosis by neutrophils and monocytes.
- Recurring or persistent infections such as Candida albicans, as well as boils and furuncles, in patients with undiagnosed diabetes often lead the HCP to suspect diabetes.
- Loss of sensation (neuropathy) may delay the detection of an infection.
- Persistent glycosuria may predispose to bladder infections, especially in patients with a neurogenic bladder.
- Decreased circulation resulting from angiopathy can prevent or delay the immune response.
- Antibiotic therapy has prevented infection from being a major cause of death among patients with diabetes.
- The treatment of infections must be prompt and vigorous.
- Teach patients measures to prevent infection. People with diabetes should practice good hand hygiene and avoid exposure to individuals who have a communicable illness. An annual influenza vaccine is advisable. In addition, a pneumococcal vaccine (Pneumovax) is recommended.
- Patients with diabetes have high rates of depression, anxiety, and eating disorders. Depression contributes to diminished diabetes self-care, feelings of helplessness related to chronic illness, and poor outcomes. Assess patients for manifestations of depression and/or diabetes distress.
- Disordered eating behaviors (DEB) can occur in people with both type 1 and type 2 diabetes. DEBs include anorexia, bulimia, binge eating, excessive restriction of calories, and intense exercise. The greatest incidence of eating disorders is seen in females. Adolescent girls with diabetes are more than twice as likely to develop DEB than those who do not have diabetes. Patients may intentionally decrease their dose of insulin or omit the dose. This is called “diabulimia” and leads to weight loss, hyperglycemia, and glycosuria because the food ingested cannot be used for energy without adequate insulin. Insulin omission and DEBs can have serious consequences, including retinopathy, neuropathy, lipid abnormalities, DKA, and death.
- Open communication is critical to identify these behaviors early. Patients with eating disorders need to be seen by a mental health professional with expertise in eating disorders and an understanding of diabetes management.
Gerontologic Considerations
- Increased prevalence and mortality
- Glycemic control challenging
- Increased hypoglycemic unawareness
- Functional limitations
- Renal insufficiency
- Meal planning and exercise
- Patient teaching must be adapted to needs
- Diabetes is present in more than 25% of persons older than 65 years, and this age group is the fastest growing segment of the population developing diabetes.
- The prevalence of diabetes increases with age. A major reason for this is that the process of aging is associated with a reduction in β-cell function, decreased insulin sensitivity, and altered carbohydrate metabolism.
- Older people with diabetes have higher rates of premature death, functional disability, and coexisting illnesses such as hypertension and stroke than do those without diabetes.
- One reason is that hypoglycemic unawareness is more common in older adults, and so these patients are more likely to suffer adverse consequences from blood glucose–lowering therapy. They may have delayed psychomotor function that could interfere with the ability to treat hypoglycemia. Other factors to consider in establishing glycemic goals for an older patient include the patient’s own desire for treatment and other coexisting medical problems such as cognitive impairment.
- Compounding the challenge, diabetes increases the rate of decline of cognitive function. Although it is generally agreed that a level of treatment is indicated to prevent complications intensive diabetes management may be difficult and dangerous to achieve, especially in older adults.
- Meal planning and exercise are recommended as therapy for older adult patients with diabetes.
- This therapy should take into account functional limitations that may interfere with physical activity and the ability to prepare meals.
- Because of the physiologic changes that occur with aging, the therapeutic outcome for the older adult with diabetes who receives OAs may be altered.
- Assess renal function and creatinine clearance in patients older than 80 years who are taking metformin. Monitor those taking sulfonylurea drugs (e.g., glipizide) for hypoglycemia and for renal and liver dysfunction. Insulin therapy may be instituted if OAs are not effective.
- However, it is important to recognize that older adults are more likely to have limitations in the manual dexterity and visual acuity necessary for accurate insulin administration. Insulin pens may be a safer alternative for older adults.
- Patient education issues for the older patient include those related to altered vision, mobility, cognitive status, and functional ability.
- Plan patient teaching based on the individual’s needs; for patients with cognitive and functional limitations, use a slower pace with simple printed or audio materials. It is important to include the family or caregiver in the teaching. Consider the patient’s financial and social situation, as well as the effect of multiple medications, eating habits, and quality-of-life issues.
The nurse is caring for a patient with type 1 diabetes mellitus who is admitted for diabetic ketoacidosis. The nurse would expect which laboratory test result?
- Hypokalemia
- Fluid overload
- Hypoglycemia
- Hyperphosphatemia
Answer: A
Rationale: Electrolytes are depleted in diabetic ketoacidosis. Osmotic diuresis occurs with depletion of sodium, potassium, chloride, magnesium, and phosphate levels. A patient with diabetic ketoacidosis will be dehydrated (fluid volume deficit), and blood glucose levels would be elevated (hyperglycemia).
The nurse is caring for patient hospitalized with DM would look for which laboratory test to obtain information on the patient’s past glucose control?
- prealbumin level
- urine ketone level
- fasting glucose
- glycosylated hemoglobin level
Answer: D
Thyroid Disorders
Learning Objectives
- Explain presentation and treatment of hyperthyroidism and hypothyroidism
- Describe tests and associated values for diagnosing thyroid disorders
- Identify considerations for older and younger adults with thyroid disorders
- Explain presentation and treatment of Cushing’s, SIADH, and DI
- Provide teaching for corticosteroid therapy
Continuum of Thyroid Dysfunction

Thyroid labs
- TSH: 0.4-4.5 IU/mL
- *T3, T4, Free T3, Free T4 are other labs with varying normal ranges
- Thyroid antibodies
Hyperthyroidism
- A sustained increase in synthesis and release of thyroid hormones by thyroid gland
- Graves’ disease (75%)-more prevalent in females
- Other causes:
- Toxic nodular goiter
- Thyroiditis
- Excess iodine intake
- Pituitary tumors
- Thyroid cancer
- Hyperthyroidism is hyperactivity of the thyroid gland with sustained increase in synthesis and release of thyroid hormones.
- It occurs in women more than men, with the highest frequency in persons 20 to 40 years old.
- Subclinical hyperthyroidism
- Serum TSH level below 0.4 mIU/L
- Normal t4 and T3 levels
- Overt hyperthyroidism
- Low or undetectable TSH
- Elevated T4 and T3 levels
- Symptoms may or may not be present
Graves’ Disease: Etiology & Pathophysiology
- Autoimmune disease
- Diffuse thyroid enlargement
- Excess thyroid hormone secretion
- Precipitating factors interact with genetic factors
- Women >5 times more likely than me to develop Graves’ disease
- Risk factors: low iodine, smoking, infection, stress, genetic factors
Graves’ disease is an autoimmune disease of unknown etiology characterized by diffuse thyroid enlargement and excess thyroid hormone secretion.
In Graves’ disease the patient develops antibodies to the TSH receptor. These antibodies attach to the receptors and stimulate the thyroid gland to release T3, T4, or both.
Graves’ disease accounts for up to 75% of the cases of hyperthyroidism.
Women are five times more likely than men to develop Graves’ disease.
Precipitating factors such as insufficient iodine supply, cigarette smoking, infection, and stressful life events may interact with genetic factors to cause Graves’ disease.
The disease is characterized by remissions and exacerbations with or without treatment.
It may progress to destruction of the thyroid tissue, ultimately causing hypothyroidism.
Graves’ disease is associated with the presence of other autoimmune disorders, including rheumatoid arthritis, pernicious anemia, SLE, Addison’s disease, celiac disease, and vitiligo.
Clinical manifestations: Signs and Symptoms
- Related to effect of thyroid hormone excess
- Increased metabolism
- Increased tissue sensitivity to stimulation by sympathetic nervous system
- Goiter
- Inspection
- Auscultation: bruits
- Ophthalmopathy
- Exophthalmos
Another common finding is ophthalmopathy, a term used to describe abnormal eye appearance or function.
A classic finding in Graves’ disease is exophthalmos, a protrusion of the eyeballs from the orbits that is usually bilateral.
Exophthalmos results from increased fat deposits and fluid (edema) in the orbital tissues and ocular muscles.
The increased pressure forces the eyeballs outward. The upper lids are usually retracted and elevated, with the sclera visible above the iris. When the eyelids do not close completely, the exposed corneal surfaces become dry and irritated. Serious consequences, such as corneal ulcers and eventual loss of vision, can occur. The changes in the ocular muscles result in muscle weakness, causing diplopia.
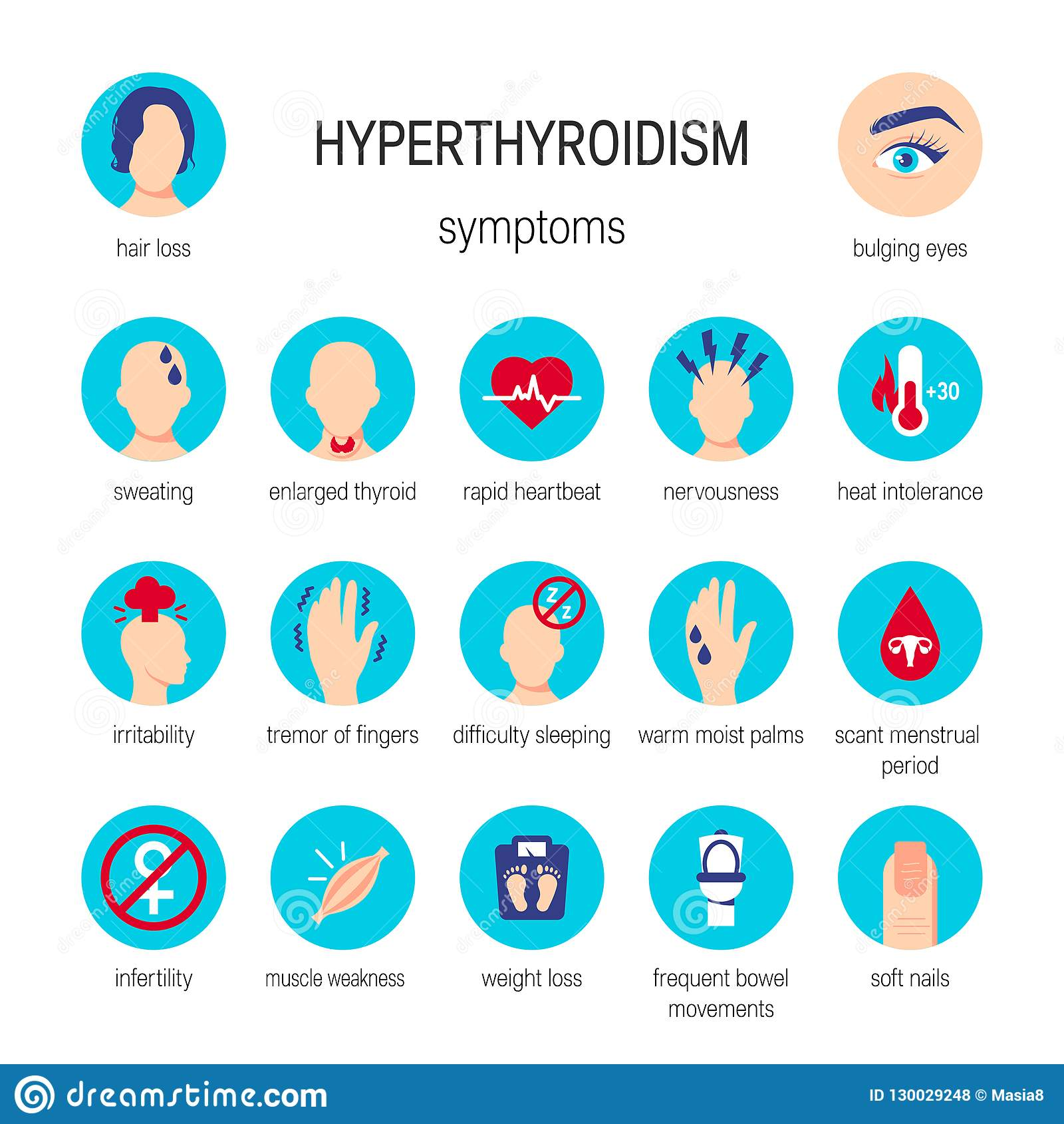
Clinical manifestations continued…
- Cardiovascular
- Respiratory
- GI
- Integumentary
- Musculoskeletal
- Nervous
- Reproductive
- “hot and high” s/s
Clinical manifestations continued…
- Intolerance to heat
- Elevated basal temperature
- Lid lag, stare
- Eyelid retraction
- Rapid speech
Acute Thyrotoxicosis-extreme
- Thyrotoxic crisis or thyroid storm
- Excessive amounts of hormones released
- Life-threatening emergency
- Death rare when treatment initiated
- Results from stressors
- Thyroidectomy patients at risk
- Manifestations: Severe tachycardia, heart failure, shock, hyperthermia, agitation, seizures, abdominal pain, vomiting, diarrhea, delirium, coma
Diagnostic studies- Hyperthyroidism
- Decreased or undetectable TSH
- Increased free thyroxine (Free T4)
- Total T3 and T4- not as definitive as TSH and Free T4
- Radioactive iodine uptake (RAIU)-increased uptake
- Differentiates Graves’ disease from other forms of thyroiditis
The two primary laboratory findings used to confirm the diagnosis of hyperthyroidism are low or undetectable TSH levels (< 0.4 mIU/L) and elevated free thyroxine (free T4) levels.
Total T3 and T4 levels may also be assessed, but they are not as definitive.
Total T3 and T4 determine both free and bound (to protein) hormone levels. The free hormone is the only biologically active form of these hormones.
The RAIU test is used to differentiate Graves’ disease from other forms of thyroiditis.
The patient with Graves’ disease will show a diffuse, homogeneous uptake of 35% to 95%, whereas the patient with thyroiditis will show an uptake of less than 2%.
The person with a nodular goiter will have an uptake in the high normal range.
Collaborative Management-hyperthyroidism
- Goals:
- Block adverse effects of thyroid hormones
- Suppress hormone oversecretion
- Prevent complications
- Three primary treatment options:
- Antithyroid medications: Antithyroid drugs, Iodine, beta-Adrenergic blockers
- Radioactive iodine therapy (RAI)
- Surgery
Medications treat the thyrotoxic states, but they are not curative
Antithyroid Drugs
- Propylthiouracil (PTU) and methimazole (Tapazole)
- MOA: Inhibit synthesis of thyroid hormone
- Improvement in 1-2 weeks
- Good results in 4 to 8 weeks
- Therapy for 6 to 15 months
- antithyroid medications may take several months for full affect
- Do not stop drug abruptly
The first-line antithyroid drugs are propylthiouracil and methimazole (Tapazole).
These drugs inhibit the synthesis of thyroid hormones.
Indications for use include Graves’ disease in young patients, hyperthyroidism during pregnancy, and the need to achieve a euthyroid state before surgery or radiation therapy.
PTU is generally given to patients who are in the first trimester of pregnancy, who have had an adverse reaction to methimazole, or for whom a rapid reduction in symptoms is required.
PTU is also considered first line in thyrotoxic crisis as it also blocks the peripheral conversion of T4 to T3.
The advantage of PTU is that it achieves the therapeutic goal of a euthyroid state more quickly, but it must be taken three times per day.
In contrast, methimazole is given in a single daily dose.
Improvement usually begins 1 to 2 weeks after the start of drug therapy.
Good results are usually seen within 4 to 8 weeks.
Therapy is usually continued for 6 to 15 months to allow for spontaneous remission, which occurs in 20% to 40% of patients.
Emphasize to the patient the importance of adhering to the drug regimen.
Abruptly discontinuing drug therapy can result in a return of hyperthyroidism.
Iodine
- Potassium iodine (SSKI) and Lugol’s solution
- MOA: Inhibit synthesis of T3 and T4 and block their release into circulation
- Decreases vascularity of thyroid gland-safer surgery if needed
- Maximal effect within 1 to 2 weeks
- Used before surgery and used in conjunction with other antithyroid medications to treat crisis
- Nursing considerations- mix with water/juice, drink through straw, give after meals,
Iodine is available as saturated solution of potassium iodine (SSKI) and Lugol's solution.
Iodine is used with other antithyroid drugs to prepare the patient for thyroidectomy or for treatment of thyrotoxicosis.
Rapidly giving large doses of iodine inhibits synthesis of T3 and T4 and blocks the release of these hormones into circulation.
It also decreases the vascularity of the thyroid gland, making surgery safer and easier.
The maximal effect is usually seen within 1 to 2 weeks.
Because of a reduction in the therapeutic effect, long-term iodine therapy is not effective in controlling hyperthyroidism.
Iodine is mixed with water or juice, sipped through a straw, and given after meals.
Assess the patient for signs of iodine toxicity such as swelling of the buccal mucosa and other mucous membranes, excessive salivation, nausea and vomiting, and skin reactions. If toxicity occurs, discontinue iodine administration and notify the HCP.
Beta-Adrenergic Blockers
- Symptomatic relief of thyrotoxicosis
- MOA: Block effects of sympathetic nervous stimulation: decrease tachycardia, nervousness, irritability, and tremors
- Propranolol
- Atenolol
Radioactive Iodine Therapy (RAI)
- Treatment of choice in nonpregnant adults
- Damages or destroys thyroid tissue
- Delayed response of up to 3 months
- Treated with antithyroid drugs and beta-blocker before and during first 3 months of RAI
- Given on outpatient basis
- Patient teaching
- Dryness of mouth and throat
- radiation protocols
Radioactive iodine (RAI) therapy is the treatment of choice for most nonpregnant adults.
RAI damages or destroys thyroid tissue, thus limiting thyroid hormone secretion.
RAI has a delayed response. The maximum effect may not be seen for up to 3 months.
For this reason, the patient is usually treated with antithyroid drugs and propranolol before and during the first 3 months after the initiation of RAI until the effects of irradiation become apparent.
While RAI is usually effective, 80% of patients have posttreatment hypothyroidism; thus the need for thyroid hormone therapy may be lifelong.
RAI therapy is usually given on an outpatient basis.
A pregnancy test is done on all women who experience menstrual cycles before starting therapy.
Tell the patient that radiation thyroiditis and parotiditis are possible and may cause dryness and irritation of the mouth and throat.
Relief may be obtained with frequent sips of water, ice chips, or the use of a salt-and-soda gargle three or four times per day.
This gargle is made by dissolving 1 teaspoon of salt and 1 teaspoon of baking soda in 2 cups of warm water.
The discomfort should subside in 3 to 4 days.
A mixture of antacid (Mylanta or Maalox), diphenhydramine (Benadryl), and viscous lidocaine can be used to swish and spit, allowing for better patient comfort during eating.
Patients are asked to follow some radiation precautions after treatment in order to limit radiation exposure to others.
Teach the patient receiving RAI on the importance of home precautions, including the following:
Use private toilet facilities, if possible, and flush two to three times after each use.
Separately launder towels, bed linens, and clothes daily at home.
Do not prepare food for others that requires prolonged handling with bare hands.
Avoid being close to pregnant women and children for 7 days after therapy.
Because of the high frequency of hypothyroidism after RAI therapy, teach the patient and family about the symptoms of hypothyroidism and to seek medical help if these symptoms occur.
Surgical Therapy
- Indications
- Large goiter causing tracheal compression
- Unresponsive to antithyroid therapy
- Thyroid cancer
- Not a candidate for RAI
- Rapid reduction in T3 and T4 levels
- Subtotal thyroidectomy: Remove 90% of thyroid
- Preferred surgical procedure
- Minimally invasive procedures:
- Endoscopic thyroidectomy
- Robotic surgery
Nutritional Therapy
- Potential for nutritional deficit r/t hypermetabolism
- High-calorie diet (4000-5000 cal/day)
- 6 full meals/day with snacks in between
- Protein: 1-2g/kg ideal body weight
- Increased carbohydrate intake
- Avoid caffeine
- Dietician referral
Hypothyroidism
“Low and slow”
Defined
- general slowing of the metabolic rate
- More common in American women than in men
- Subclinical hypothyroidism
- TSH is >4.5 mIU/L
- T4 levels normal
- Affects up to 10% of women over 60
- Nonthyroidal illness syndrome (NTIS)
- Critically ill patients
- Low T3, T4, and TSH levels
Etiology and Pathophysiology
- Primary hypothyroidism
- Caused by destruction of thyroid tissue or defective hormone synthesis
- Secondary hypothyroidism
- Caused by pituitary or hypothalamic dysfunction (↓ TSH or TRH)
- Iodine deficiency
- Atrophy of the gland
- Treatment for hyperthyroidism
- Drugs
- Severe cognitive deficits if occurs in infancy and remains untreated
Hypothyroidism can be classified as primary or secondary.
Primary hypothyroidism is caused by destruction of thyroid tissue or defective hormone synthesis.
Secondary hypothyroidism is caused by pituitary disease with decreased TSH secretion or hypothalamic dysfunction with decreased thyrotropin-releasing hormone (TRH) secretion.
Hypothyroidism can be transient and related to thyroiditis or discontinuing thyroid hormone therapy.
Iodine deficiency is the most common cause of hypothyroidism worldwide.
In the United States, the most common cause of primary hypothyroidism is atrophy of the thyroid gland. This atrophy is the end result of Hashimoto’s thyroiditis or Graves’ disease. These autoimmune diseases destroy the thyroid gland.
Hypothyroidism also may develop after treatment for hyperthyroidism, specifically thyroidectomy or RAI therapy.
Drugs such as amiodarone (Cordarone) (which contains iodine) and lithium (which blocks hormone production) can cause hypothyroidism.
Hypothyroidism that develops in infancy (cretinism) is caused by thyroid hormone deficiencies during fetal or early neonatal life. All infants in the United States are screened for decreased thyroid function at birth.
Clinical Manifestations
- Systemic effects characterized by slowing of body processes
- Manifestations variable, slow onset
- Symptoms may be attributed to normal aging in older adult
- Cardiovascular system
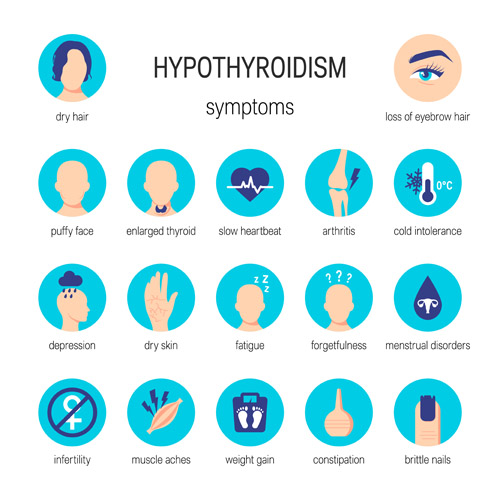 Respiratory system
Respiratory system- Integumentary
- Neurologic system
- Gastrointestinal system
- Musculoskeletal system
- Reproductive system
The patient is often fatigued, lethargic, and experiences personality and mental changes, including impaired memory, slowed speech, decreased initiative, and somnolence. Many appear depressed. Weight gain is most likely a result of a decreased metabolic rate.
In the older adult the typical manifestations of hypothyroidism (fatigue, cold and dry skin, hoarseness, hair loss, constipation, and cold intolerance) may be attributed to normal aging.
For this reason, the patient's symptoms may not raise suspicion of an underlying condition.
Older adults who have confusion, lethargy, and depression should be evaluated for thyroid disease.
Hypothyroidism Extreme: Common Features of Myxedema
- A manifestation of severe, long-standing hypothyroidism
- Skin and subcutaneous tissue develop hydrophilic mucopolysaccharides-leads to edema
- Puffiness
- Facial and periorbital edema
- Masklike affect
Complications-Myxedema
- Myxedema coma-medical emergency
- Precipitated by infection, drugs, cold, trauma
- Characterized by:
- Impaired consciousness
- Subnormal temperature, hypotension, hypoventilation
- Cardiovascular collapse
- Treated with IV thyroid hormone
The mental sluggishness, drowsiness, and lethargy of hypothyroidism may progress gradually or suddenly to a notable impairment of consciousness or coma. This situation, termed myxedema coma, is a medical emergency.
Myxedema coma can be precipitated by infection, drugs (especially opioids, tranquilizers, and barbiturates), exposure to cold, and trauma.
It is characterized by subnormal temperature, hypotension, and hypoventilation.
Cardiovascular collapse can result from hypoventilation, hyponatremia, hypoglycemia, and lactic acidosis.
For the patient to survive a myxedema coma, vital functions must be supported, and IV thyroid hormone replacement must be administered.
Diagnostic Studies- Hypothyroidism
- History and physical examination
- TSH and free T4
- TSH ↑ with primary hypothyroidism
- TSH ↓ with secondary hypothyroidism
- Thyroid antibodies- if positive suggestive of autoimmune origin
- ↑ Cholesterol
- ↑ Triglycerides
- ↑ Creatine kinase
- ↓ RBCs (anemia)
The most reliable laboratory tests for thyroid function are TSH and free T4. These values, correlated with symptoms gathered from the history and physical examination, confirm the diagnosis of hypothyroidism.
Serum TSH levels help determine the cause of hypothyroidism. Serum TSH is high when the defect is in the thyroid and low when it is in the pituitary or hypothalamus.
The presence of thyroid antibodies suggests an autoimmune origin.
Pharmacology-hypothyroidism
- Restoration of euthyroid state as safely and rapidly as possible
- Levothyroxine (Synthroid)
- Start with low dose
- Monitor for: cardiovascular side effects (increased heart rate, chest pain, dysrhythmias), weight loss, nervousness, tremors, insomnia
- monitor apical pulse rate, rhythm, sleep pattern, and weight
- Increase dose in 4- to 6-week intervals as needed-can take time to get right dose; repeat labs
- Lifelong therapy
- Nursing considerations
- take before meals
- take at same time each day
- monitor apical pulse
Other endocrine disorders: Cushing syndrome: Etiology & Pathophysiology
- Iatrogenic administration of corticosteroids
- ACTH-secreting pituitary adenoma (Cushing disease)
- Adrenal tumors, ectopic ACTH production by tumors (lung or pancreas)
- High circulating levels of corticosteroids lead to:
- Immunosuppression
- Weight gain due to accumulation of adipose tissue (centripetal obesity with
- broad purple striae, “moon face,” and “buffalo hump”)
- Hyperglycemia (glucose intolerance and increased gluconeogenesis in liver)
- Muscle wasting and weakness
- Osteoporosis, back pain
- Weak, thin, easily bruised skin
- Delayed wound healing
- Mineralocorticoid excess: hypokalemia, hypertension
- Adrenal androgen excess: severe acne, virilization in women, feminization in men
- Most physical changes resolve after surgery or treatment and hormone levels return to normal
Cortisol increases the breakdown of muscle into amino acids so that it can be turned into glucose during gluconeogenesis. Excess cortisol leads to protein breakdown throughout the body causing muscle wasting, osteoporosis, and thin skin.
Most of the physical changes caused by Cushing syndrome may resolve after surgery once hormone levels return to normal
Cushing syndrome: Diagnostics
- Midnight or late-night salivary cortisol
- Low-dose dexamethasone suppression test (blood test)
- 24-hour urine cortisol
- CT scan or MRI of pituitary and adrenal glands
- ACTH levels (may be up or down depending on etiology)
Nursing considerations:
altered body image
Most of the physical changes caused by Cushing syndrome may resolve after surgery once hormone levels return to normal
Addison’s Disease: Etiology and Pathophysiology
- Primary
- Secondary
- 80% of cases caused by an autoimmune response
- Other causes:
- TB (not a common cause in United States)
- Amyloidosis
- Fungal infections
- AIDS
- Metastatic cancer
- Iatrogenic Addison’s disease
- Common symptoms:
- fatigue
- muscle pain and weakness
- weight loss
- low blood pressure
- joint pain
Adrenocortical insufficiency (hypofunction of the adrenal cortex) may be from a primary cause (Addison’s disease) or a secondary cause (lack of pituitary ACTH secretion).
In Addison’s disease, amounts of all three classes of adrenal corticosteroids (glucocorticoids, mineralocorticoids, and androgens) are reduced.
In secondary adrenocortical insufficiency, corticosteroid and androgen levels are deficient, but mineralocorticoid levels rarely are.
ACTH deficiency may be caused by pituitary disease or suppression of the hypothalamic-pituitary axis because of the administration of exogenous corticosteroids.
Up to 80% of Addison's disease cases in the United States are caused by an autoimmune response.
Autoimmune adrenalitis causes the adrenal cortex to be destroyed by antibodies. This results in loss of glucocorticoid, mineralocorticoid, and adrenal androgen hormones.
Addison’s disease can be present along with other endocrine conditions. This is known as autoimmune polyglandular syndrome.
It is most common in white females.
Those with autoimmune adrenalitis often have other autoimmune disorders such as type 1 diabetes, autoimmune thyroid disease, pernicious anemia, and celiac disease.
Iatrogenic Addison's disease may be due to adrenal hemorrhage, often related to anticoagulant therapy, chemotherapy, ketoconazole therapy for AIDS, or bilateral adrenalectomy.
Adrenal insufficiency most often occurs in adults younger than 60 years of age and affects both genders equally.
Corticosteroid Therapy
- Effective but complicated
- Side effects with long-term use
- Benefits v. Risks
- Expected effects
- Anti Inflammatory action
- Immunosuppression
- Maintenance of normal BP
- Side effects:
- ↓ Potassium and calcium
- ↑ Glucose and BP
- Delayed healing
- Susceptibility to infection
- Suppressed immune response
- Peptic ulcer disease
- Muscle atrophy/weakness
- Mood and behavior changes
- Moon face, truncal obesity
- Protein depletion
- Risk for acute adrenal crisis if therapy is stopped abruptly
Patient teaching: Corticosteroid Therapy
- Dietary needs
- Rest and exercise needs
- Sodium restriction if edema occurs
- Need to monitor for hyperglycemia
- Notify health care provider if epigastric pain develops
- Need to prevent injury/infection
- Inform all health care providers
- Should be taken in morning with food to reduce gastric irritation
- Must not be stopped abruptly
- Needs to increase in times of stress
- Measures to reduce occurrence of osteoporosis
SIADH – syndrome of inappropriate antidiuretic hormone
a posterior pituitary problem
- Overproduction of ADH
- Results in reabsorption of water
- Fluid retention
- serum hypoosmolality
- dilutional hyponatremia
- hypochloremia
- concentrated urine/lower urinary output
Diabetes Insipidus – a posterior pituitary problem
- Deficient ADH production or secretion
- Or Decreased renal response to ADH
- Results in:
- Increased urine output (several times normal)
- Increased plasma osmolality
- Electrolyte imbalance
Signs & Symptoms of DI
- Polydipsia
- Polyuria (2-20 L/day)
- Urine specific gravity very low
- Serum osmolality high
- Hypernatremia
- Some who drink water excessively will maintain normal serum osmolality
- Fatigue, generalized weakness
Central (neurogenic) DI phases
- Caused by damage to the pituitary gland
- Acute phase: abrupt onset polyuria
- Interphase: urine volume normalizes
- Third phase: permanent DI
- End result: Severe dehydration, hypotension, tachycardia, hypovolemic shock, coma
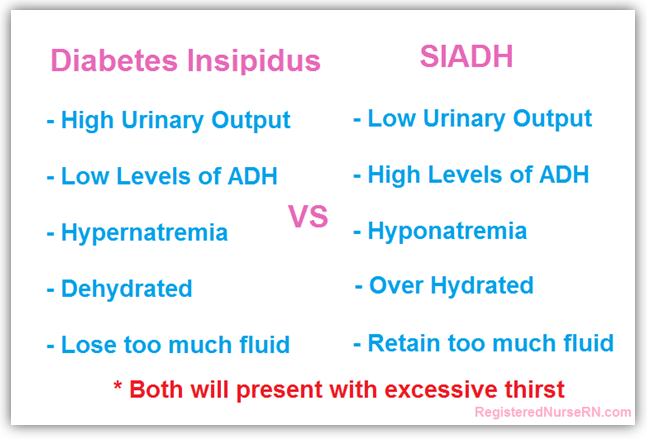
Pulmonary
Pulmonary, Upper Respiratory
Learning objectives
- Identify structures and functions of the upper respiratory system
- Name gerontologic considerations and the effects of aging on the respiratory system
- Describe tests and associated values for diagnosing respiratory issues
- Explain treatments and medications for managing upper respiratory issues including allergic rhinitis, cough, and the common cold
Structures and Functions of
Respiratory System
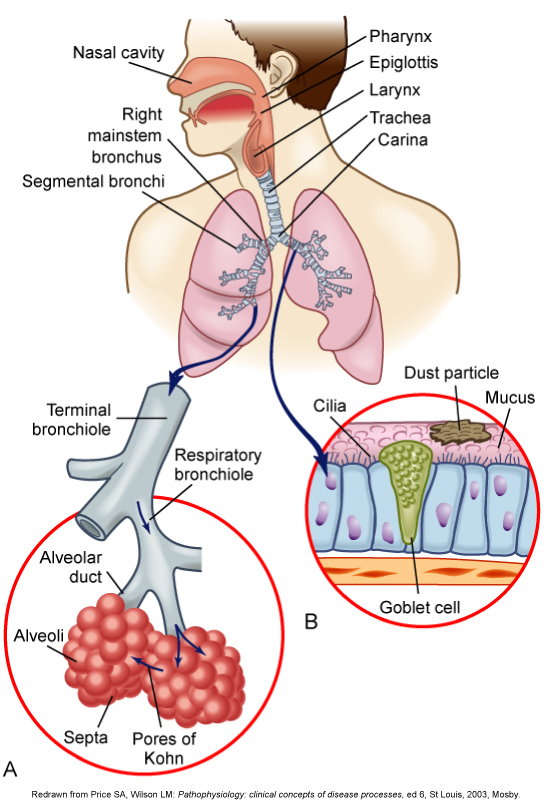
Structures and Functions of Respiratory System
- Primary purpose: Gas exchange
- Two parts
- Upper respiratory tract
- Lower respiratory tract
The primary purpose of the respiratory system is gas exchange.
This involves the transfer of oxygen and carbon dioxide between the atmosphere and blood.
The respiratory system is divided into two parts: upper respiratory tract and the lower respiratory tract.
- Upper Respiratory Tract
- Nose
- Mouth
- Pharynx
- Epiglottis
- Larynx
- Trachea
Air enters into the respiratory tract through the nose.
The nasal cavity connects with the pharynx, a tubular passageway that is subdivided into three parts: the nasopharynx, the oropharynx, and the laryngopharynx.
The nose functions to protect the lower airway by warming and humidifying air and filtering small particles before air enters the lungs. Olfactory nerve endings, located in the roof of the nose, are responsible for the sense of smell.
Air moves through the oropharynx to the laryngopharynx. It then travels through the epiglottis to the larynx before moving into the trachea.
The epiglottis is a small flap located behind the tongue that closes over the larynx during swallowing. This prevents solids and liquids from entering the lungs.
The vocal cords are located in the larynx. Air passes through the glottis (the opening between the vocal cords) and into the trachea.
The trachea is a cylindrical tube about 5 inches (10 to 12 cm) long and 1 inch (1.5 to 2.5 cm) in diameter. U-shaped cartilages keep the trachea open but allow the adjacent esophagus to expand for swallowing.
The trachea bifurcates into the right and left mainstem bronchi at a point called the carina. The carina is located at the level of the manubriosternal junction, also called the angle of Louis. The carina is highly sensitive, and stimulation of this area during suctioning causes vigorous coughing.
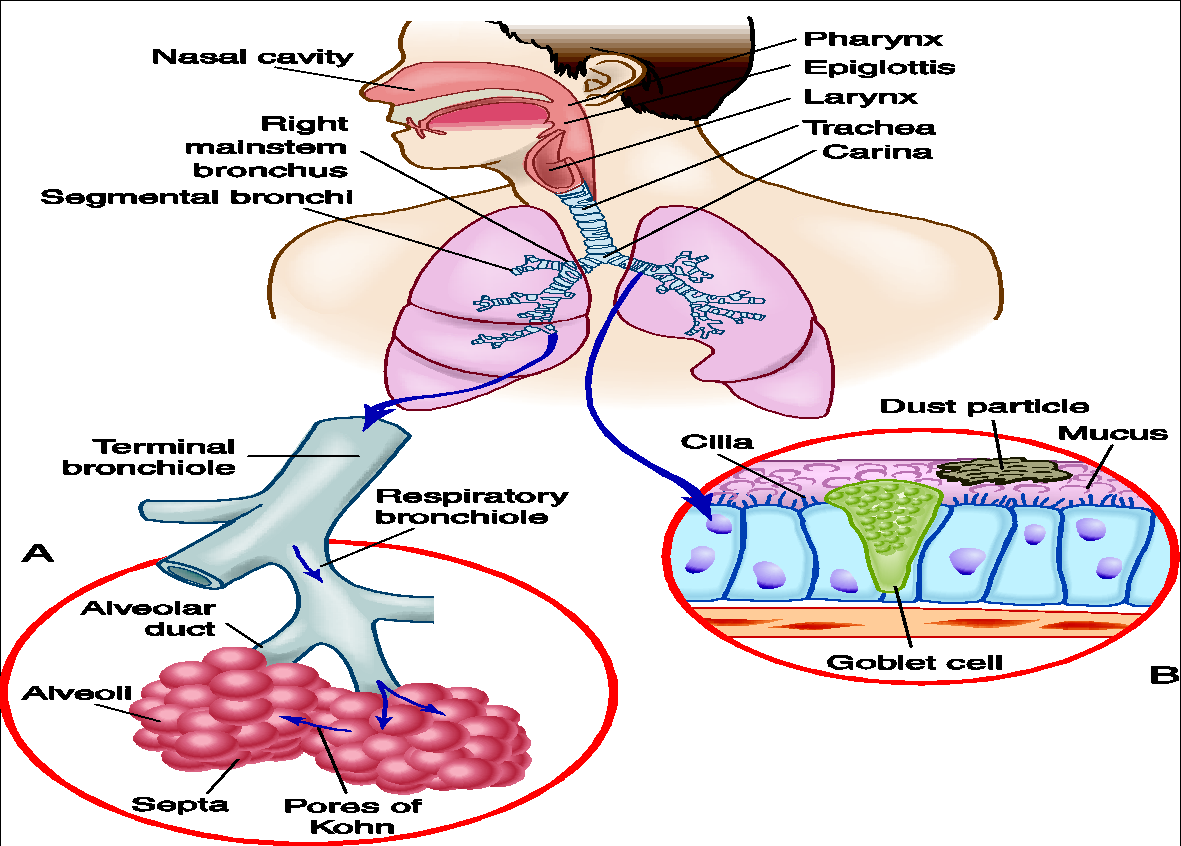
- Lower Respiratory Tract
- Bronchi
- Bronchioles
- Alveolar ducts
- Alveoli
- Lung lobes
The lower respiratory tract consists of the bronchi, bronchioles, alveolar ducts, and alveoli. With the exception of the right and left mainstem bronchi, all lower airway structures are located inside the lungs.
The right mainstem bronchus is shorter, wider, and straighter than the left mainstem bronchus. For this reason, aspiration is more likely to occur in the right lung than in the left lung.
The right lung is divided into three lobes (upper, middle, and lower) and the left lung into two lobes (upper and lower).
Physiology of Respiration
- Oxygenation
- Partial pressure of oxygen in arterial blood (PaO2)
- Oxygen dissolved in plasma
- Millimeters of mercury (mm Hg).
- Arterial oxygen saturation (SaO2)
- Amount of oxygen bound to hemoglobin
- Expressed as a percentage (%)
Oxygenation refers to the process of obtaining oxygen from the atmospheric air and making it available to the organs and tissues of the body. The lungs' ability to oxygenate arterial blood adequately is assessed by clinical assessment of the patient (Table 25-2), partial pressure of oxygen in arterial blood (PaO2), and arterial oxygen saturation (SaO2).
Oxygen is carried in the blood in two forms: dissolved oxygen and hemoglobin-bound oxygen. The PaO2 represents the amount of oxygen dissolved in the plasma and is expressed in millimeters of mercury (mm Hg). The SaO2 is the amount of oxygen bound to hemoglobin in comparison with the amount of oxygen the hemoglobin can carry and is expressed as a percentage.
Oxygen and carbon dioxide move back and forth across the alveolar-capillary membrane by diffusion. The overall direction of movement is from the area of higher concentration to the area of lower concentration. Thus oxygen moves from alveolar gas (atmospheric air) into the arterial blood and carbon dioxide from the arterial blood into the alveolar gas. Diffusion continues until equilibrium is reached.
Control of Respiration
- Chemoreceptors respond to changes in PaCO2 and pH
- Central chemoreceptors-change in PaCO2 and pH
- Peripheral chemoreceptors-change in PaO2 and pH
- Mechanical receptors respond to a variety of physiologic factors- respond to irritants, stretching of tissue
A chemoreceptor is a receptor that responds to a change in the chemical composition (PaCO2 and pH) of the fluid around it. Central chemoreceptors are located in the medulla and respond to changes in the hydrogen ion (H+) concentration.
An increase in the H+ concentration (acidosis) causes the medulla to increase the respiratory rate and tidal volume (Vt).
A decrease in H+ concentration (alkalosis) has the opposite effect.
Peripheral chemoreceptors are located in the carotid bodies at the bifurcation of the common carotid arteries and in the aortic bodies above and below the aortic arch.
The peripheral chemoreceptors respond to decreases in PaO2 and pH and to increases in PaCO2. These changes also cause stimulation of the respiratory center.
Mechanical receptors (juxtacapillary and irritant) are located in the lungs, upper airways, chest wall, and diaphragm.
They are stimulated by a variety of physiologic factors, such as irritants, muscle stretching, and alveolar wall distortion.
Signals from the stretch receptors aid in the control of respiration. As the lungs inflate, pulmonary stretch receptors activate the inspiratory center to inhibit further lung expansion. This is termed the Hering-Breuer reflex, and it prevents overdistention of the lungs.
The stimulation of juxtacapillary receptors cause the rapid respiration (tachypnea) seen in pulmonary edema. These receptors are stimulated by fluid entering the pulmonary interstitial space.
Respiratory Defense Mechanisms
- Filtration of air
- Mucociliary clearance system- mucus and cillia work together to protect
- Cough reflex-clears airway
- Reflex bronchoconstriction
- Alveolar macrophages
Respiratory defense mechanisms are efficient in protecting the lungs from inhaled particles, microorganisms, and toxic gases.
Nasal hairs filter inspired air. Most large particles (greater than 5 μm in size) are removed in the nasopharynx or bronchi and do not reach the alveoli.
Below the larynx, the movement of mucus is accomplished by the mucociliary clearance system, commonly referred to as the mucociliary escalator. This term is used to indicate the interrelationship between the secretion of mucus and the ciliary activity. Mucus is continually secreted at a rate of about 100 mL/day by the goblet cells and submucosal glands. It forms a mucous blanket that contains the impacted particles and debris from distal lung areas. Cilia beat rhythmically about 1000 times per minute in the large airways, moving mucus toward the mouth. The ciliary beat is slower further down the tracheobronchial tree. As a consequence, particles that penetrate more deeply into the airways are removed less rapidly.
The cough is a protective reflex action that clears the airway by a high-pressure, high-velocity flow of air. It is a backup for mucociliary clearance, especially when this clearance mechanism is overwhelmed or ineffective. Coughing is only effective in removing secretions above the subsegmental level (large or main airways).
Reflex bronchoconstriction is another defense mechanism. In response to the inhalation of large amounts of irritating substances (e.g., dusts, aerosols), the bronchi constrict in an effort to prevent entry of the irritants. A person with hyperreactive airways, such as a person with asthma, may experience bronchoconstriction after inhalation of triggers such as cold air, perfume, or other strong odors.
Because ciliated cells are not found below the level of the respiratory bronchioles, the primary defense mechanism at the alveolar level is alveolar macrophages. Alveolar macrophages rapidly phagocytize inhaled foreign particles such as bacteria. The debris is moved to the level of the bronchioles for removal by the cilia or removed from the lungs by the lymphatic system.
Gerontologic Considerations:Effects of Aging on Respiratory System
- Structural changes
- Defense mechanisms
- Respiratory control
Age-related changes in the respiratory system can be divided into alterations in structure, defense mechanisms, and respiratory control.
Structural changes include calcification of the costal cartilages, which can interfere with chest expansion.
The outward curvature of the spine is marked, especially with osteoporosis, and the lumbar curve flattens and he chest may appear barrel-shaped, and the elderly may need to use accessory muscles to breathe. Respiratory muscle strength progressively declines after age 50. Overall, the lungs in the older adult are harder to inflate.
Within the lung, the number of functional alveoli decreases, and they become less elastic. Decrease in PaO2 results in less tolerance for exertion, and dyspnea can occur if activity exceeds normal exercise.
Respiratory defense mechanisms are less effective because of a decline in both cell-mediated and humoral immunity (ability to produce antibodies). The alveolar macrophages are less effective at phagocytosis. An older patient has a less forceful cough and fewer and less functional cilia. Mucous membranes tend to be drier. Retained mucus predisposes the older adult to respiratory infections.
Respiratory control is altered, resulting in a more gradual response to changes in blood oxygen or carbon dioxide level. The PaO2 may drop to a slightly lower level, and the PaCO2 may rise to a slightly higher level before the respiratory rate changes.
There is much variability in the extent of these changes in persons of the same age. The older adult who has a significant smoking history, is obese, and has a chronic illness is at greatest risk of adverse outcomes.
Clubbing
Causes of cyanosis include hypoxemia or decreased cardiac output. Inspect the fingers for evidence of long-standing hypoxemia known as clubbing (an increase in the angle between the base of the nail and the fingernail to 180 degrees or more, usually accompanied by an increase in the depth, bulk, and sponginess of the end of the finger).
Allergic Rhinitis
- Inflammatory disorder of the upper airway, lower airway, and eyes
- Symptoms
- Sneezing
- Rhinorrhea
- Pruritus
- Nasal congestion
- For some people: Conjunctivitis, sinusitis, and asthma
- Seasonal and perennial
- Triggered by airborne allergens
- Allergens bind to immunoglobulin E (IgE) on mast cells
- Triggers release of inflammatory mediators
- Histamine, leukotrienes, prostaglandins
Classes of Drugs Used for Allergic Rhinitis
- Glucocorticoids (intranasal)
- Antihistamines (oral and intranasal)
- Sympathomimetics (oral and intranasal)
Intranasal Glucocorticoids
- First choice—most effective for treatment and prevention of rhinitis
- Mild adverse effects
- Drying of nasal mucosa or sore throat
- Epistaxis
- Headache
- Rarely, systemic effects (adrenal suppression and slowing of linear pediatric growth)
Oral Antihistamines
- For allergic rhinitis
- Do not reduce nasal congestion, treat histamine response
- Most effective if taken prophylactically
- Should be taken regularly throughout the allergy season, even when symptoms are absent, to prevent an initial histamine receptor activation
- Mild adverse effects: Sedation with first generation (much less with second generation)
Intranasal Antihistamines: Azelastine and Olopatadine
- Indicated for allergic rhinitis in adults and in children over 12 years old
- Systemic absorption can be sufficient to cause somnolence
- Nosebleeds
- Anticholinergic effects
- Unpleasant taste
Sympathomimetics
- Reduce nasal congestion (do not reduce rhinorrhea, sneezing, or itching)
- Activate alpha1-adrenergic receptors on nasal blood vessels
- Adverse effects
- Rebound congestion
- CNS stimulation
- Cardiovascular effects and stroke
- Abuse
- Factors in topical administration
- Should not use longer than 5 consecutive days
- Drops or sprays
- Comparison: Topical versus oral
- Topical agents act more quickly than oral agents and are usually more effective
- Oral agents act longer than topical preparations
- Systemic effects occur primarily with oral agents; topical agents usually elicit these responses only when dosage is higher than recommended
- Rebound congestion is common with prolonged use of topical agents but rare with oral agents
ex: Afrin
Cough-Drugs for Cough
- Antitussives
- Drugs that suppress cough
- Opioid antitussives
- Codeine and hydrocodone
- Nonopioid antitussives
- Dextromethorphan
- Diphenhydramine
- Benzonatate
Cough- Expectorants
- Guaifenesin [Mucinex, Humibid]
- Renders cough more productive by stimulating flow of respiratory tract secretions
- Nursing considerations
- drink plenty of fluids
- avoid combining with other OTC products
- check OTC products for similar medications so not taking more than recommended
Cough- Mucolytics
- Hypertonic saline - nebulized
- Acetylcysteine - inhaled
- Mucolytics react directly with mucus to make it more watery
- High sulfur content, “rotten egg” smell
- Can trigger bronchospasm
- Nursing considerations
- drink plenty of fluids
- avoid using with combination medications
Pharyngitis
- Acute pharyngitis
- viral, bacterial (strep throat), fungal
- Fungal pharyngitis
- increased risk for patients who are immunocompromised (HIV), who use long term ABX or inhaled corticosteroids
- Treatment
- antibiotics only warranted for confirmed bacterial infection, viral infection aimed toward symptom management and secondary infection prevention
- encourage fluids but avoid irritating drinks such as citrus juices, tylenol/ibuprofen for pain management, gargle salt water for sore throat
- Fungal pharyngitis
- treated with antifungal drugs
- proper patient medication education
- rinse mouth thoroughly with water after use of inhaled corticosteroids
Common Cold
- Acute upper respiratory viral infection
- Rhinorrhea, nasal congestion, cough, sneezing, sore throat, headache, hoarseness, malaise, myalgia
- Fever common in kids, rare in adults
- Self-limited, usually benign
- No cure; just treatment of symptoms
Over-the-Counter (OTC) Cold Remedies
- Combination cold remedies usually contain two or more of the following:
- Nasal decongestant
- Antitussive
- Analgesic
- Antihistamine (for anti-cholinergic actions)
- Nursing considerations
- avoid using multiple combination medications
Pediatric OTC Cold Remedies
- Use with caution in young children
- Avoid OTC cold remedies in children younger than 4 to 6 years
- Use only products labeled for pediatric use
- Consult a healthcare professional before giving these drugs to a child
- Read all product safety information before dosing
- Use the measuring device provided with the product
- Discontinue the medicine and seek professional care if the child’s condition worsens or fails to improve
- Avoid using antihistamine-containing products to sedate children
A patient asks what medication would be most effective in the treatment of seasonal hay fever. The nurse will teach the patient about the use of which drug?
- Azelastine [Astelin]
- Chlorpheniramine [Chlor-Trimeton]
- Fluticasone [Flonase]
- Pseudoephedrine [Sudafed]
Answer: C
Rationale: Glucocorticoids (fluticasone [Flonase]) are the most effective agents used to treat allergic rhinitis.
Lower Respiratory Issues
Learning Objectives
- Identify structures and functions of the lower respiratory system
- Describe the pathophysiology of pneumonia
- Differentiate between the different etiologies and types of pneumonia
- Explain treatments and medications for managing lower respiratory issues including bronchitis and pneumonia
Bronchitis
- Most often caused by a viral illness
- Can be acute
- Can become chronic- COPD
Pneumonia
- Acute infection of lung parenchyma
- Associated with significant morbidity and mortality rates
- Pneumonia and influenza are 8th leading cause of death in the U.S.
Pneumonia is an acute infection of the lung parenchyma (gas exchange)
Until 1936, pneumonia was the leading cause of death in the United States. The discovery of sulfa drugs and penicillin was pivotal in the treatment of pneumonia. Since that time, there has been remarkable progress in the development of antibiotics to treat pneumonia.
However, despite newer antimicrobial agents, pneumonia is still associated with significant morbidity and mortality rates.
Etiology
- Likely to result when defense mechanisms become incompetent or overwhelmed
- ↓ Cough and epiglottal reflexes may allow aspiration
Normally, the airway distal to the larynx is protected from infection by various defense mechanisms. Mechanisms that create a mechanical barrier to microorganisms entering the tracheobronchial tree include air filtration, epiglottis closure over the trachea, cough reflex, mucociliary escalator mechanism, and reflex bronchoconstriction. Immune defense mechanisms include secretion of immunoglobulins A and G and alveolar macrophages.
Pneumonia is more likely to occur when defense mechanisms become incompetent or are overwhelmed by the virulence or quantity of infectious agents.
Decreased consciousness weakens the cough and epiglottal reflexes, which may allow aspiration of oropharyngeal contents into the lungs.
Etiology
- Mucociliary mechanism impaired- damage
- Pollution
- Cigarette smoking
- Upper respiratory infections (URI)
- Tracheal intubation
- Aging
- Chronic diseases suppress immune system
Air pollution, cigarette smoking, viral upper respiratory infections (URIs), tracheal intubation, and normal changes that occur with aging can impair the mucociliary escalator mechanism.
Chronic diseases can suppress the immune system’s ability to inhibit bacterial growth. The risk factors for pneumonia are listed in Table 27-1.
Etiology
- Three ways organisms reach lungs:
- Aspiration from nasopharynx or oropharynx
- Inhalation of microbes present in air
- Hematogenous spread from primary infection elsewhere in body (rare)
Organisms that cause pneumonia reach the lung by three methods:
Aspiration of normal flora from the nasopharynx or oropharynx. Many organisms that cause pneumonia are normal inhabitants of the pharynx in healthy adults.
Inhalation of microbes present in the air. Examples include Mycoplasma pneumoniae and fungal pneumonias.
Hematogenous spread from a primary infection elsewhere in the body. An example is Streptococci and Staphylococcus aureus from infective endocarditis.
Types of Pneumonia
- Can be classified according to causative organism
- Clinical classification:
- Community-acquired (CAP)
- Hospital-acquired (HAP)
- Ventilator-associated (VAP)
Bacteria, viruses, Mycoplasma, fungi, parasites, and chemicals are all potential causes of pneumonia.
Although pneumonia can be classified many different ways (e.g., according to the causative organism), a clinically effective way is to classify pneumonia as community-acquired or hospital-acquired pneumonia.
Classifying pneumonia is important because of the differences in the likely causative organisms and the selection of appropriate antimicrobial therapy.
See Table 27-2 for further information.
Types of Pneumonia
- Community-Acquired Pneumonia (CAP)
- Occurs in patients who have not been hospitalized or resided in a long-term care facility within 14 days of the onset of symptoms
- Can be treated at home or hospitalized dependent on patient condition
- Empiric antibiotic therapy started ASAP
The decision to treat the patient at home or admit them to the hospital is based on several factors such as patient’s age, vital signs, mental status, presence of comorbid conditions, and current physiologic condition.
Clinicians can use tools such as the CURB-65 scale to supplement clinical judgment. (See Table 27-3.)
Empiric antibiotic therapy, the initiation of treatment before a definitive diagnosis or causative agent is confirmed, should be started as soon as possible when CAP is suspected. Empiric antibiotic administration is based on experience and knowledge of drugs known to be effective for the most likely causative agent.
Types of Pneumonia
- Hospital-Acquired Pneumonia (HAP)
- HAP: Occurs 48 hours or longer after hospitalization and not present at time of admission
- (Ventilator-associated )VAP: Occurs more than 48 hours after endotracheal intubation
- Associated with longer hospital stays, increased costs, sicker patients, and increased risk of morbidity and mortality
HAP, previously known as nosocomial pneumonia, is a pneumonia in a nonintubated patient that begins 48 hours or longer after admission to hospital and was not present at the time of admission.
Ventilator-associated pneumonia (VAP), also a type of HAP, refers to pneumonia that occurs more than 48 hours after endotracheal intubation. (VAP is discussed in Chapter 65.)
Once the diagnosis of HAP or VAP is made, treatment of pneumonia is initiated based on known risk factors, early versus late onset, and probable organism. Antibiotic therapy can be adjusted once the results of sputum cultures identify the exact pathogen.
Types of Pneumonia
- Multidrug-resistant (MDR) organisms are major problem in treatment
- Staphylococcus aureus
- Gram-negative bacilli
- Risk factors for MDR pneumonia
- Advanced age
- Immunosuppression
- History of antibiotic use
- Prolonged mechanical ventilation
A major problem in treating pneumonia today is the development of multidrug-resistant (MDR) organisms.
Primary culprits include methicillin-resistant Staphylococcus aureus and gram- negative bacilli.
Antibiotic susceptibility tests can identify MDR organisms.
The virulence of these organisms can severely limit the available and appropriate antimicrobial therapy.
MDR organisms can also increase the morbidity and mortality risks associated with pneumonia. (Chapter 14 discusses MDR organisms.)
Types of Pneumonia
- Aspiration Pneumonia
- Results from abnormal entry of secretions into lower airway
- Major risk factors:
- Decreased level of consciousness
- Difficulty swallowing
- Insertion of nasogastric tubes with or without tube feeding
Decreased level of consciousness might be from seizures, anesthesia, head injury, stroke, alcohol intake, or others.
With loss of consciousness, the gag and cough reflexes are depressed, and aspiration is more likely to occur.
Types of Pneumonia
- Aspiration Pneumonia
- Aspirated material triggers inflammatory response
- Primary bacterial infection most common
- Empiric therapy based on severity of illness, where infection acquired, and probable causative organism
- Aspiration of acid gastric contents initially causes chemical (noninfectious) pneumonitis; no ABX initially, secondary bacterial infection can occur
The aspirated material (food, water, vomitus, or oropharyngeal secretions) triggers an inflammatory response.
The most common form of aspiration pneumonia is a primary bacterial infection. Typically, more than one organism is identified on sputum culture, including both aerobes and anaerobes as they both comprise the flora of the oropharynx.
Until the cultures are completed and results obtained, initial antibiotic therapy is based on an assessment of probable causative organism, severity of illness, patient factors (e.g., malnutrition, current use of antibiotic therapy), and ability to treat common community-acquired organisms.
For patients who aspirate in hospitals, appropriate antibiotics should include coverage for both gram-negative organisms and MRSA.
In contrast, aspiration of acidic gastric contents causes chemical (noninfectious) pneumonitis, which may not require antibiotic therapy. However, secondary bacterial infection can occur 48 to 72 hours later.
Types of Pneumonia
- Necrotizing Pneumonia
- Rare complication of bacterial lung infection
- Often results from CAP
- Signs and symptoms
- Immediate respiratory insufficiency and/or failure
- Leukopenia
- Bleeding into airways
Necrotizing pneumonia is characterized by liquefaction and, in some situations, cavitation of lung tissue.
Although the exact pathophysiological mechanisms involved are controversial, causative organisms include Staphylococcus, Klebsiella, and Streptococcus.
Lung abscesses commonly occur.
Treatment often includes long- term antibiotic therapy and possible surgery.
Types of Pneumonia
- Opportunistic Pneumonia
- Patients at risk
- Severe protein-calorie malnutrition
- Immunodeficiencies
- Chemotherapy/radiation recipients
- Long-term corticosteroid therapy
- Caused by microorganisms that do not normally cause disease
Opportunistic pneumonia is inflammation and infection of the lower respiratory tract in immunocompromised patients.
In addition to the risk of bacterial and viral pneumonia, the immunocompromised person may develop an infection from microorganisms that do not normally cause disease.
Types of Pneumonia
- Chest x-ray findings
Pathophysiology of Pneumonia
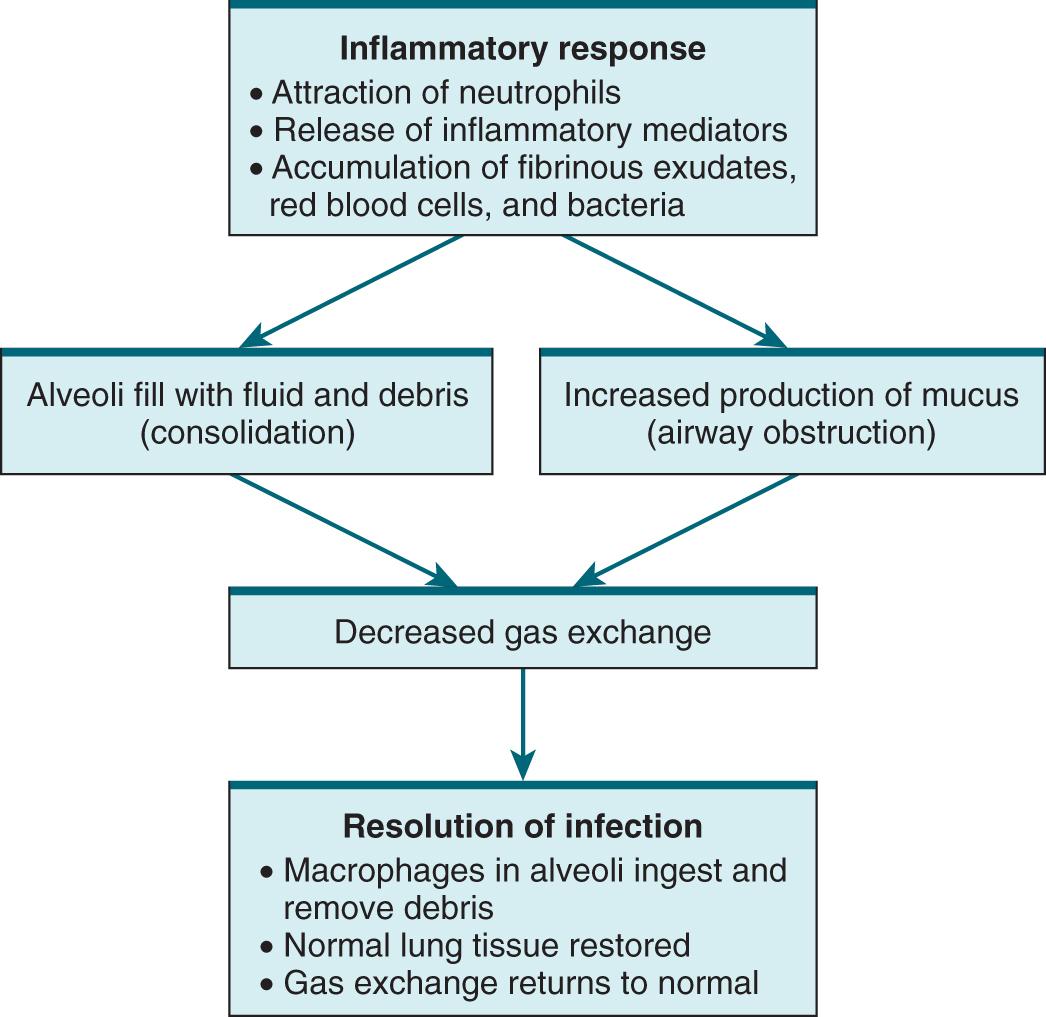
Specific pathophysiologic changes related to pneumonia vary according to the offending organism, but the majority of organisms trigger an inflammatory response in the lungs.
Inflammation, characterized by an increase in blood flow and vascular permeability, activates neutrophils to engulf and kill the offending organisms.
As a result, the inflammatory process attracts more neutrophils, edema of the airways occurs, and fluid leaks from the capillaries and tissues into alveoli.
Normal oxygen transport is affected, leading to clinical manifestations of hypoxia (e.g., tachypnea, dyspnea, tachycardia).
Consolidation, a feature typical of bacterial pneumonia, occurs when the normally air-filled alveoli become filled with fluid and debris. Mucous production also increases, which can potentially obstruct airflow and impair gas exchange even further.
Over time and with appropriate antibiotic therapy, macrophages lyse and process the debris, lung tissue is allowed to recover, and gas exchange returns to normal. Resolution and healing occur if there are no complications.
Case Study
D.T. is an 88-year-old woman who lives alone.
She has been feeling weaker over past 2 days.
Last night became confused and disoriented.
Copyright © 2017, Elsevier Inc. All Rights Reserved.
19
Case Study
Her housekeeper notified her daughter, who brought D.T. to the clinic.
She complains of coughing over the past 3 days.
(©iStockphoto/Thinkstock)
Copyright © 2017, Elsevier Inc. All Rights Reserved.
20
Case Study
She has a history of mild heart failure that is treated medically but has no other significant health disorders.
She last saw her health care provider 4 months ago.
(©iStockphoto/Thinkstock)
Copyright © 2017, Elsevier Inc. All Rights Reserved.
21
Case Study
What are D.T.’s risk factors for pneumonia?
What type of pneumonia is D.T. likely exhibiting?
(©iStockphoto/Thinkstock)
Copyright © 2017, Elsevier Inc. All Rights Reserved.
Age, limited mobility, chronic heart failure
CAP because there is no mention of hospitalization or long-term care facility residency within the last 2 weeks; she last saw her HCP 4 months ago.
22
Case Study
What clinical manifestations of pneumonia is D.T. displaying?
For what other clinical manifestations would you assess D.T. ?
What diagnostic tests would you expect the nurse practitioner in the clinic to order?
- Chest x-ray, sputum for gram stain and culture and sensitivity, CBC with differential, electrolytes, brain natriuretic peptide (BNP)
- Copyright © 2017, Elsevier Inc. All Rights Reserved.
Cough, weakness, confusion
Shaking chills; dyspnea; tachypnea; pleuritic chest pain; green, yellow, or rust-colored sputum; rhonchi and rales; bronchial breath sounds; egophony; ↑ fremitus; dullness to percussion if pleural effusion present; nonspecific manifestations including diaphoresis, anorexia, myalgias, headache, and abdominal pain
Chest x-ray, sputum for gram stain and culture and sensitivity, CBC with differential, electrolytes, brain natriuretic peptide (BNP)
Clinical Manifestations
- Most common
- Cough
- Fever, chills
- Dyspnea, tachypnea
- Pleuritic chest pain
- Green, yellow, or rust-colored sputum
- Change in mentation for older or debilitated patients
- Nonspecific manifestations
The most common presenting symptoms of pneumonia are cough, fever, shaking chills, dyspnea, tachypnea, and pleuritic chest pain. The cough may or may not be productive. Sputum may appear green, yellow, or even rust-colored (bloody).
Viral pneumonia may initially present as influenza, with respiratory symptoms appearing and/or worsening 12 to 36 hours after onset.
The older or debilitated patient may not have classic symptoms of pneumonia. Confusion or stupor (possibly related to hypoxia) may be the only finding. Hypothermia, rather than fever, may also be noted with the older patient.
Nonspecific clinical manifestations include diaphoresis, anorexia, fatigue, myalgias, and headache.
Clinical Manifestations
- Physical examination findings
- Fine or coarse crackles
- Bronchial breath sounds
- Egophony
- ↑ Fremitus
- Dullness to percussion if pleural effusion present
On physical examination, fine or coarse crackles may be auscultated over the affected region.
If consolidation is present, bronchial breath sounds, egophony (a change in the sound of the voice of the patient) and increased fremitus (vibration of the chest wall produced by vocalization) may be noted.
Patients with pleural effusion may exhibit dullness to percussion over the affected area.
Complications
- Atelectasis
- Pleurisy
- Pleural effusion
- Bacteremia
- Pneumothorax
- Acute respiratory failure
- Sepsis/septic shock
Complications develop more frequently in older individuals and those with underlying chronic diseases. Potential complications include the following:
• Atelectasis (collapsed, airless alveoli) of one or part of one lobe may occur. These areas may clear with effective deep breathing and coughing.
• Pleurisy (inflammation of the pleura) may occur.
• Pleural effusion (fluid in the pleural space) can occur. In most cases, the effusion is sterile and is reabsorbed in 1 to 2 weeks. Occasionally, effusions require aspiration by thoracentesis.
• Bacteremia (bacterial infection in the blood) is more likely to occur in infections with Streptococcus pneumoniae and Haemophilus influenzae.
• Pneumothorax can occur when air collects in the pleura space, causing the lungs to collapse.
What tests do anticipate being ordered?
Case Study
D.T.’s chest x-ray reveals consolidation in her left lower lobe, consistent with pneumonia.
Her WBC is 17,000/μL (17 × 109/L) (nl 4.5-11)
(©iStockphoto/Thinkstock)
Copyright © 2017, Elsevier Inc. All Rights Reserved.
28
Case Study
Her electrolytes and B-type natriuretic peptide (BNP) are within normal limits.
Sputum Gram stain shows gram-positive diplococci and many WBCs.
Would you anticipate she would be admitted to the hospital for care?
(©iStockphoto/Thinkstock)
Copyright © 2017, Elsevier Inc. All Rights Reserved.
29
Case Study
Because of her age and altered mentation, the health care provider admits her to the hospital for treatment.
What treatment do you anticipate?
(©iStockphoto/Thinkstock)
Copyright © 2017, Elsevier Inc. All Rights Reserved.
30
Interprofessional Care
- Supportive care
- Oxygen for hypoxemia
- Patient positioning
- Analgesics for chest pain
- Antipyretics
- Individualize rest and activity
- No definitive treatment for majority of viral pneumonias
- Antivirals for influenza pneumonia
In addition to antibiotic therapy, supportive measures are individualized to the patient’s needs.
These may include oxygen therapy to treat hypoxemia, analgesics to relieve the chest pain, and antipyretics such as aspirin or acetaminophen for elevated temperature.
Although cough suppressants, mucolytics, bronchodilators, and corticosteroids are often prescribed as adjunctive therapy, the use of these drugs is controversial. However, they may be prescribed for patients with underlying chronic conditions.
Individualize rest and activity to each patient’s tolerance. Benefits of mobility include improved diaphragm movement and chest expansion, mobilization of secretions, and prevention of venous stasis.
Currently, there is no definitive treatment for the majority of viral pneumonias. As identified earlier, care is generally supportive. In most circumstances, viral pneumonia is self-limiting and will often resolve in 3-4 days. Antiviral therapy may be used to treat pneumonia caused by influenza (e.g., oseltamivir or zanamivir) and a few other viruses (e.g., acyclovir [Zovirax] for herpes simplex virus).
Interprofessional Care
- Pneumococcal vaccine
- To prevent Streptococcus pneumoniae
- Prompt treatment with antibiotics is essential for bacterial pneumonia
- Response generally occurs within 48-72 hr
- ↓ Temperature
- Improved breathing
- ↓ Chest discomfort
- Response generally occurs within 48-72 hr
- Repeat chest x-ray in 6-8 weeks
Prompt treatment with the appropriate antibiotic is essential. Antibiotics are highly effective for both bacterial and mycoplasma pneumonia.
In uncomplicated cases, the patient responds to drug therapy within 48 to 72 hours.
Abnormal physical findings can last more than 7 days.
A repeat chest x-ray may be obtained in 6 to 8 weeks to assess for resolution.
Drug Therapy
- Start with empiric therapy
- Based on likely infecting organism and risk factors for MDR organisms
- Varies with local patterns of antibiotic resistance
- Should see improvement in 3-5 days
- Start with IV and then switch to oral therapy as soon as patient stable
Once the pneumonia is classified, the HCP selects empiric therapy on the likely infecting organism (see Table 27-2).
For all types of pneumonia, empiric antibiotic therapy is based on whether the patient has risk factors for MDR organisms.
The prevalence and resistance patterns of MDR pathogens vary among localities and institutions. Therefore the antibiotic regimen needs to be adapted to local patterns of antibiotic resistance.
Multiple regimens exist, but all should initially include antibiotics that are effective against both resistant gram-negative and gram-positive organisms.
Clinical improvement usually occurs between 3 and 5 days. Patients who deteriorate or fail to respond to therapy will require aggressive reevaluation to assess for noninfectious etiologies, complications, other coexisting infectious processes, or pneumonia caused by a drug-resistant pathogen.
IV antibiotic therapy should be switched to oral therapy as soon as the patient is hemodynamically stable, improving clinically, able to ingest oral medication, and has a functioning GI tract. Stable patients do not need to be observed in the hospital and can be discharged to home on oral antibiotics.
Total treatment time for patients with CAP should be a minimum of 5 days, and the patient should be afebrile for 48 to 72 hours. However, you need to emphasize the importance of completing the full course of antibiotic treatment. Longer treatment time may be needed if initial therapy was not active against the identified pathogen or complications occur.
Nutritional Therapy
- Adequate hydration
- Prevent dehydration
- Thin and loosen secretions
- Adjust for older adults, patients with heart failure, those with preexisting respiratory conditions
- High calorie, small, frequent meals
- Monitor for weight loss
Hydration is important in the supportive treatment of pneumonia to prevent dehydration and to thin and loosen secretions.
Individualize and carefully monitor fluid intake. If the patient is an older adult, has heart failure, or has known preexisting respiratory condition.
IV administration of fluids and electrolytes may be necessary.
Weight loss may occur in patients with pneumonia because of increased metabolic needs and difficulty eating due to non-specific abdominal complaints or shortness of breath. Small, frequent meals are easier for dyspneic patients to tolerate. Offer foods high in calories and nutrients.
Case Study
It has been 4 days since D.T. was admitted for pneumonia.
She is hemodynamically stable and neurologically intact. What does this mean?
(©iStockphoto/Thinkstock)
Copyright © 2017, Elsevier Inc. All Rights Reserved.
Teach the importance of rest and fluids while recovering, the importance of finishing the antibiotics, and food or drug interactions with the prescribed antibiotic, avoidance of alcohol and smoking, importance of follow-up chest x-ray, information about yearly influenza vaccinations, and signs and symptoms to watch for in the future.
35
Case Study
She has been switched from IV antibiotics to oral antibiotics and is ready for discharge.
What important teaching should you provide to the patient and family?
(©iStockphoto/Thinkstock)
Copyright © 2017, Elsevier Inc. All Rights Reserved.
Teach the importance of rest and fluids while recovering, the importance of finishing the antibiotics, and food or drug interactions with the prescribed antibiotic, avoidance of alcohol and smoking, importance of follow-up chest x-ray, information about yearly influenza vaccinations, and signs and symptoms to watch for in the future.
36
Ambulatory Care
- Patient teaching for home care
- Emphasize need to take full course of medication(s)
- Drug-drug and drug-food interactions
- Adequate rest
- Adequate hydration
- Avoid alcohol and smoking
- Cool mist humidifier
- Chest x-ray, vaccinations
Teach the patient about the importance of taking every dose of the prescribed antibiotic, any drug-drug and food-drug interactions for the prescribed antibiotic, and the need for adequate rest to facilitate recovery.
Instruct the patient to drink plenty of liquids (at least 6-10 glasses/day unless contraindicated) and to avoid alcohol and smoking.
A cool mist humidifier or warm bath may help the patient breathe easier.
Tell patients that it may be several weeks before their usual vigor and sense of well-being return.
Explain that a follow-up chest x-ray may be done in 6-8 weeks to evaluate resolution of pneumonia. A prolonged period of convalescence may be necessary for the older adult or chronically ill patient.
Teaching should also include information about available influenza and pneumococcal vaccines. Patients can receive the pneumococcal vaccine and influenza vaccine at the same time but not in the exact same location and the vaccines cannot be mixed into one shot.
The nurse is caring for a patient with pneumonia. If a pleural effusion is developing, the nurse would expect which finding?
Barrel-shaped chest
Paradoxical respirations
Hyperresonance on percussion
Localized decreased breath sounds
Audience Response Question
Copyright © 2017, Elsevier Inc. All Rights Reserved.
38
Answer: D
Rationale: Clinical manifestations of pleural effusion include diminished breath sounds over the affected area, decreased movement of the chest on the affected side, dullness to percussion, dyspnea, cough, and occasional sharp and nonradiating chest pain that is worse on inhalation.
Audience Response Question
The nurse is caring for a patient with acute bronchitis. What would indicate an objective sign of increased work of breathing? (select all that apply)
Barrel-shaped chest
Retractions
Nasal flaring
Cough
Accessory muscle use
Patient verbalizes feeling SOB
B, C, E
39
Drugs for Asthma and Chronic Obstructive Pulmonary Disease
Learning objectives
- Describe the pathophysiology of asthma and COPD
- Explain treatments and medications for managing asthma and COPD
- Differentiate between the different classes of medications used to manage asthma and COPD
- Provide education for anti inflammatory drugs used to manage asthma and COPD including bronchodilators, glucocorticoids, immunomodulators, and anticholinergics
Asthma
- Chronic inflammatory disorder of the airway
- Characteristic signs and symptoms
- Sense of breathlessness
- Tightening of the chest
- Wheezing
- Dyspnea
- Cough
- Cause: Immune-mediated airway inflammation
Pathophysiology
- Symptoms of asthma result from a combination of inflammation and bronchoconstriction, so treatment must address both components
Chronic Obstructive Pulmonary Disease (COPD)
- Chronic, progressive, largely irreversible disorder characterized by airflow restrictions and inflammation
- Characteristic signs and symptoms
- Chronic cough
- Excessive sputum production
- Wheezing
- Dyspnea
- Poor exercise tolerance
- Cause: Smoking cigarettes
- Main cause of COPD is cigarette smoking
- Symptoms of COPD result largely from two pathologic processes: Chronic bronchitis and emphysema
- Both processes are caused by an exaggerated inflammatory reaction to cigarette smoke
- Chronic bronchitis, which is defined by a chronic cough and excessive sputum production, results from hypertrophy of mucus-secreting glands in the epithelium of the larger airways
- Emphysema is enlargement of the air space within the bronchioles and alveoli, brought on by deterioration of the walls of these air spaces
- Among individuals with COPD, the relative contribution of these two processes can vary
Overview of Drugs for Asthma and COPD
- Two main pharmacologic classes
- Anti-inflammatory agents
- Glucocorticoids (steroids)
- Anti-inflammatory agents
- Bronchodilators
- Beta2 agonists
Inhalation Drugs
- Three obvious advantages
- Therapeutic effects are enhanced
- Systemic effects are minimized
- Relief of acute attacks is rapid
- Four types
- Metered-dose inhalers (MDIs)
- Respimats
- Dry-powder inhalers (DPIs)
- Nebulizers
*Review the Pulmonary Video/Study Resources document in Moodle to see how each type works*
10
- MDI - use a spacer, long controlled inhale
- Respimat - is a soft mist - no spacer needed, long controlled inhale
- Nebulizer - makes a mist, takes several minutes, breath regularly from mouthpiece
- DPI - no spacer, it is a powder, requires a sharp intake of breath
Anti-inflammatory Drugs
- Foundation of asthma therapy
- Taken daily for long-term control
- Principal anti-inflammatory drugs are the glucocorticoids (eg, budesonide, fluticasone)
- Mechanism of action
- Considered the most effective antiasthma drugs available
- Decrease synthesis and release of inflammatory mediators
- Reduce infiltration and activity of inflammatory cells
- Decrease edema of the airway mucosa
- Usually administered by inhalation, but IV and oral routes are also options
Anti-inflammatory Drugs: Glucocorticoids
- Mechanism of action = suppress inflammation
- Reduce bronchial hyperreactivity and decrease airway mucus production
Anti-inflammatory Drugs: Glucocorticoids (Cont.)
- Use
- Prophylaxis of chronic asthma
- Dosing must be on a fixed schedule, not as needed (PRN)
- Not used to abort an ongoing attack because beneficial effects develop slowly; not “rescue” inhaler
- Inhaled use
- First-line therapy for management of inflammatory component of asthma
- Most patients with persistent asthma should use these drugs daily
- Inhaled glucocorticoids are very effective and much safer than systemic glucocorticoids
- Oral use
- For patients with moderate to severe persistent asthma or for management of acute exacerbations of asthma or COPD
- Potential for toxicity; should be used only when symptoms cannot be controlled with safer medications (inhaled glucocorticoids, inhaled beta2 agonists)
- Treatment should be as brief as possible!!
- Recall side effects of oral steroids
Anti-inflammatory Drugs: Glucocorticoids (Cont.)
- Adverse effects of inhaled forms
- Flovent (fluticasone), Pulmicort (budesonide)
- Adrenal suppression, but way less likely than oral or IV
- Oropharyngeal candidiasis
- Dysphonia
- Adverse effects of oral forms (chronic or long-term use)\
- Prednisone
- Adrenal suppression
- Osteoporosis
- Hyperglycemia
- Peptic ulcer disease
- In young patients: Growth suppression
Anti-inflammatory Drugs: Glucocorticoids (Cont.)
- Adrenal suppression
- Prolonged glucocorticoid use can decrease the ability of the adrenal cortex to produce glucocorticoids of its own (HPA axis suppression)
- Life-threatening at times of severe physiologic stress (eg, surgery, trauma, or systemic infection)
- Administration of high levels of glucocorticoids are required to survive severe stress
- Adrenal suppression prevents production of endogenous glucocorticoids
- Patients must be given increased doses of oral or IV glucocorticoids at times of stress
- Failure to do so can prove fatal
- Anti-inflammatory Drugs: Glucocorticoids (Cont.)
- Discontinuing treatment
- Must be done slowly
- Recovery of adrenocortical function takes several months
- Dosage of exogenous sources must be reduced gradually
- During this time, patients—including those switched to inhaled glucocorticoids—may need to be given supplemental oral or IV glucocorticoids at times of severe stress
Anti-inflammatory Drugs
- Suppress effects of leukotrienes
- Leukotrienes: Promote smooth muscle constriction, blood vessel permeability, and inflammatory responses through direct action and recruitment of eosinophils and other inflammatory cells
- In patients with asthma, leukotriene modifiers can reduce bronchoconstriction and inflammatory responses such as edema and mucous secretion
- Second-line agent
- Generally well tolerated but can cause adverse neuropsychiatric effects, including depression, suicidal thinking, and suicidal behavior (Black Box Warning)
- Montelukast [Singulair]
Bronchodilators
- Provide symptomatic relief but do not alter the underlying disease process (inflammation)
- In almost all cases, patients taking a bronchodilator should also be taking a glucocorticoid for long-term suppression of inflammation
- Principal bronchodilators are the beta2-adrenergic agonists
Bronchodilators: Beta2-Adrenergic Agonists (Cont.)
- Use in asthma and COPD
- Inhaled short-acting beta2 agonists (SABAs)
- Albuterol (ProAir, Proventil)
- Taken PRN to abort an ongoing attack
- EIB: Taken before exercise to prevent an attack
- Hospitalized patients undergoing a severe acute attack: Nebulized SABA is the traditional treatment of choice
- Delivery with an MDI in the outpatient setting may be equally effective
Bronchodilators: Beta2-Adrenergic Agonists (Cont.)
- Inhaled long-acting beta2 agonists (LABAs)
- Salmeterol (Advair), formoterol (Symbicort)
- Long-term control in patients who experience frequent attacks
- Dosing is on a fixed schedule, not PRN
- Effective in treating stable COPD
- When used to treat asthma, LABA must always be combined with a glucocorticoid
- Use alone in asthma is contraindicated
- Adverse effects
- Inhaled preparations
- Systemic effects: Tachycardia, angina, tremor
- Inhaled preparations
- Oral preparations
- Excessive dosage: Angina pectoris, tachydysrhythmias
- Tremor
Bronchodilators: Methylxanthines
- Theophylline
- Produces bronchodilation by relaxing smooth muscle of the bronchi
- Narrow therapeutic index
- Plasma level 10 to 20 mcg/mL
- Toxicity is related to theophylline levels
- The drug is usually administered by mouth but may also be administered intravenously
- Toxicity treatment
- Stop theophylline
- Activated charcoal together with a cathartic
- Dysrhythmias respond to lidocaine
- Intravenous diazepam may help control seizures
- Interactions
- Caffeine
- Tobacco and marijuana
- Cimetidine
- Fluoroquinolone antibiotics
Anticholinergic Drugs: Ipratropium
- use in inhaler form or nebulized
- Improves lung function by blocking muscarinic receptors in the bronchi, thereby reducing bronchoconstriction
- Action and use
- Administered by inhalation to relieve bronchospasm
- Therapeutic effects begin within 30 seconds, reach 50% of maximum in 3 minutes, and persist about 6 hours
- Adverse effects
- Dry mouth and irritation of the pharynx
- Glaucoma
- Cardiovascular events
Glucocorticoid/LABA Combinations
- Available combinations
- Fluticasone/salmeterol [Advair]
- Budesonide/formoterol [Symbicort]
- Mometasone/formoterol [Dulera]
- Indicated for long-term maintenance in adults and children with asthma
- Not recommended for initial therapy
Management of Chronic Asthma (Cont.)
- Long-term drug therapy
- Agents for long-term control (eg, inhaled glucocorticoids)
- Agents for quick relief of ongoing attack (eg, inhaled SABAs)
- Stepwise therapy
- Step chosen for initial therapy is based on pretreatment classification of asthma severity
- Moving up or down a step is based on ongoing assessment of asthma control
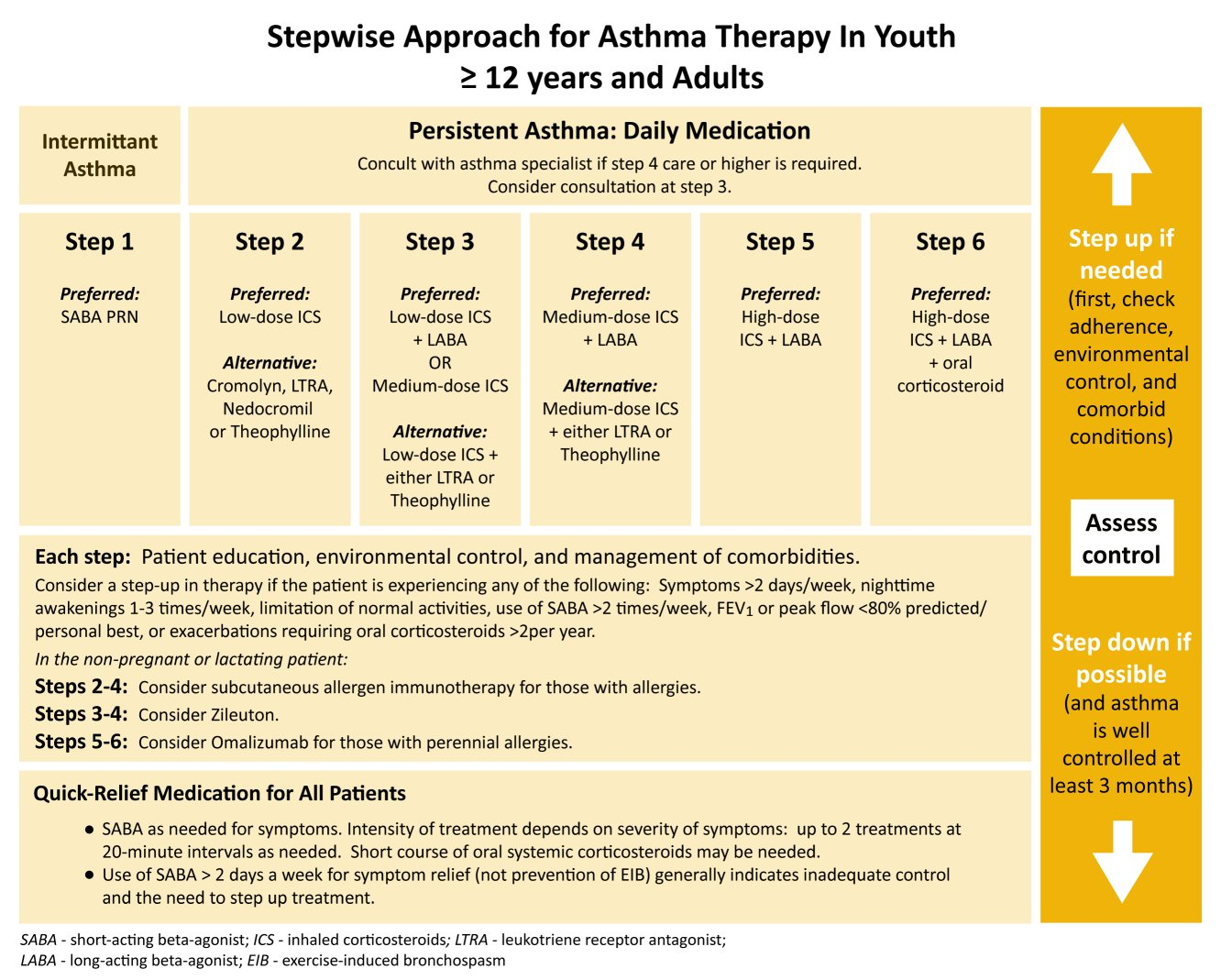
Management of Chronic Asthma (Cont.)
- Important to reduce exposure to allergens and triggers
- Sources of allergens: House dust mites, pets, cockroaches, mold, pollen
- Factors that can exacerbate asthma: Tobacco smoke, wood smoke, household sprays
- Nursing considerations- keep inhaler with you, know triggers, let people know you have asthma, consider medical alert, have plan in place and follow it if symptoms begin
Drugs for Acute Severe Exacerbation of Asthma
- This condition requires immediate attention
- Goals: Relieve airway obstruction and hypoxemia, and normalize lung function as quickly as possible
- Initial therapy consists of administering:
- Oxygen—To relieve hypoxemia
- A systemic glucocorticoid—To reduce airway inflammation
- A nebulized, high-dose SABA—To relieve airflow obstruction
- Nebulized ipratropium—To further reduce airflow obstruction
Drugs for Exercise-Induced Asthma (EIA) or exercised-induced bronchospasm (EIB)
- Cause: Bronchospasm secondary to loss of heat and/or water from the lung
- Starts either during or immediately after exercise, peaks in 5 to 10 minutes, and resolves 20 to 30 minutes later
- SABA or cromolyn administered prophylactically
- Inhaled SABAs generally preferred over cromolyn
- Beta2 agonists should be inhaled immediately before exercise
(cromolyn - a mast cell stabilizer, prevents release of histamine and leukotrienes - inhaled powder often)
Management of COPD Exacerbations
- Pharmacologic management
- SABAs (specifically inhaled, either alone or in combination with inhaled anticholinergics) are preferred for bronchodilation during COPD exacerbations
- Systemic glucocorticoids
- Antibiotics
- Supplemental oxygen to maintain an oxygen saturation of 90-92% (can be as low as 88% depending on the patient)
A patient with asthma is prescribed a long acting beta agonist (LABA), 2 puffs 3 times a day. The nurse should teach the patient to do what?
Rinse the mouth after taking the prescribed dose.
Take an extra dose if breathing is compromised.
Wait 1 minute between puffs from the inhaler.
Take adequate amounts of calcium and vitamin D.
Question 1
Copyright © 2019 by Elsevier, Inc. All rights reserved.
39
39
Answer: C
Rationale: Patients should be taught to wait at least 1 minute between puffs. Extra doses should not be taken unless prescribed by the healthcare provider. Glucocorticoid inhalation requires oral rinses to prevent the development of dysphonia and oropharyngeal candidiasis. Patients should take adequate amounts of calcium and vitamin D with glucocorticoid therapy.
A patient with asthma is prescribed triamcinolone acetonide (glucocorticoid). What should the nurse do?
Take the patient’s pulse before administering the medication.
Teach the patient to use a spacer to prevent a fungal infection.
Instruct the patient to use this drug to treat an acute attack.
Encourage the patient to avoid weight-bearing activity.
Question 2
Copyright © 2019 by Elsevier, Inc. All rights reserved.
40
40
Answer: B
Rationale: Acetonide is an inhaled glucocorticoid. Spacers disperse the medication into the lungs, leaving less in the oropharyngeal mucosa; this reduces the incidence of fungal infection. Beta2-adrenergic agonists may cause tachycardia and are used to abort acute asthma attacks. Patients taking glucocorticoids should engage in weight-bearing activities to prevent osteoporosis. This drug should not be used to treat an acute attack.
Which information should the nurse include when teaching a patient about inhaled glucocorticoids?
Inhaled glucocorticoids have many significant adverse effects.
The principal side effects of inhaled glucocorticoids include hypertension and weight gain.
Patients should rinse the mouth and gargle after administering inhaled glucocorticoids.
Patients should rinse the mouth and gargle before administering inhaled glucocorticoids.
Question 1
Copyright © 2019 by Elsevier, Inc. All rights reserved.
41
41
Answer: C
Rationale: Inhaled glucocorticoids are generally very safe. Their principal side effects are oropharyngeal candidiasis and dysphonia, which can be minimized by using a spacer device during administration and by rinsing the mouth and gargling after use.
Which of the following is NOT a serious adverse effect of long-term oral glucocorticoid therapy?
Adrenal suppression
Osteoporosis
Hypoglycemia
Peptic ulcer disease
Question 2
Copyright © 2019 by Elsevier, Inc. All rights reserved.
42
42
Answer: C
Rationale: Serious adverse effects include adrenal suppression, osteoporosis, hyperglycemia, peptic ulcer disease, and growth suppression.