Cancer Care Notes
Care for Clients with Cancer
Types of Cancer
Hepatobiliary cancers: These include malignancies of the pancreas, liver, and biliary system, which can significantly affect digestion and metabolism, often requiring specialized treatments.
Gastrointestinal Cancers: Encompasses colon, rectal, anal, stomach, intestinal, and esophageal cancers, often presenting with gastrointestinal disturbances.
Endocrine Cancers: These include cancers of glands such as the thyroid and adrenal glands, which can disrupt hormonal balance and bodily functions.
Breast Cancer: One of the most common cancers among women, with risk factors including family history, age, and lifestyle choices.
Blood Cancers: Such as leukemia, lymphoma (both Hodgkin's and non-Hodgkin), and multiple myeloma, requiring profound systemic therapies.
Genitourinary Cancers: Involves cancers of the bladder, kidney, prostate, and testicles, often with implications for sexual health and urination.
Skin Cancer: Primarily melanoma, often associated with UV exposure, requiring vigilant monitoring and preventative strategies.
Gynecologic Cancers: Include cancers of the uterus, cervix, ovaries, vagina, and vulva, affecting women's reproductive health.
Screening Guidelines
Breast Cancer Screening:
Women aged 45-54: Annual mammograms recommended.
Women aged 55 and older: Mammograms every two years or continue annual screening based on risk factors.
Clinical Breast Exam: Recommended every three years for women aged 20-39, and annually for women older than 40.
Colonoscopy: Starting at age 45 for average-risk individuals, with a repeat every 10 years to detect precancerous lesions or early-stage cancer.
Fecal Testing:
Hemoccult stool test (FOBT): Annually for early detection.
Stool DNA test: Recommended every 3 years for its higher sensitivity.
Prostate Exam (DRE): Recommended at age 40 for high-risk men and generally at age 50 for average risk.
Gene Mutation Testing: Advisable for individuals with a strong family history of breast or colon cancer to assess genetic predisposition.
Impact of Cancer on Physical Function
Cancer can have several debilitating effects on the physical functions of the body, such as:
Immunity and Clotting: decreased production of healthy bone marrow can occur when cancer starts or invades the bone marrow.
causes a decrease in WBCs needed for normal immunity
cancer treatment like chemotherapy, reduces neutrophil WBC numbers, making the pt more prone to infection
Bone marrow dysfunction causes anemia and thrombocytopenia
pt with anemia can have fatigue, SOB, and tachycardia
Pt with thrombocytopenia will have impaired clotting and an increased risk for bleeding.
Gastrointestinal Function: Tumors of GI tract or advanced cancers increase the metabolic rate and need for nutrients
Cachexia (extreme body wasting and malnutrition) may occur during treatment or with advanced cancer.
Peripheral Nerve Sensory Perception: Neurotoxic chemotherapy agents injure peripheral nerves, leading to peripheral neuropathy with reduced sensory perception
pt with chemotherapy-induced peripheral neuropathy (CIPN) reports loss of sensation, especially in the lower extremities
Symptoms include numbness, tingling, neuropathic pain, changes in gait and balance
Central Motor and Sensory Deficits: occurs when cancer invades the bone or the brain or compresses nerves
bones become thinner, with an increased risk for fractures that can occur with minimal trauma
causes bone pain, fractures, spinal cord compression (SCC) and hypercalcemia.
Respiratory and Cardiac Function: Tumors may exert pressure on these vital organs or be a side effect of treatments, creating additional health risks.
Comfort and Quality of Life: Physical limitations often lead to reduced overall well-being and emotional distress.
Cancer Management Strategies
Surgery
Prophylactic surgery: removes potentially cancerous tissue as a means of preventing cancer development. (removing opposite breast in pt who has genetic mutation BRCA1, BRCA2 to prevent cancer in the unaffected breast.
Diagnostic surgery: (excisional biopsy) is the removal of all parts of a suspected lesion for examination and testing to confirm or rule out a cancer diagnosis.
Palliative surgery focuses on providing symptom relief and improving the quality of life, but is not curative
ex: removal of tumor tissue that is causing pain, obstruction, or difficulty swallowing
Radiation
uses high-energy radiation to kill cancer cells, with the intent to cure or relieve symptoms (palliative). The goal of radiation is to kill the cancer cells while having minimal damaging effects on the surrounding normal tissues
Radiation is considered a local treatment.
Usually given as a series of divided doses (fractionation) over a set time
time is the length of exposure to the radiation field. The limit time directly at the radiation source
distance is how far from the radiation source you remain. The farther away from the radiation source, the less the exposure
shielding is using a material (such as a leaf apron) to avoid exposure.
Chemotheraphy
powerful med that stops cancer cells from dividing
Immunotheraphy
use of the body’s own defense system to attack the foreign cells
Hormonal (endocrine) therapy
slows or stops the growth of certain cancers that use hormones to grow
Radiation Therapy Details
Goal: The primary objective is to eliminate cancer cells while minimizing damage to the surrounding healthy tissues, enhancing patient safety and treatment efficacy.
Administration Protocol: Standard practice involves dividing total radiation doses over specified intervals to allow recovery of normal tissue.
Delivery Methods:
External beam radiation (teletherapy): Targets tumors from outside the body
since the radioactive source is external, the pt is not radioactive, and there is no hazard to others around the pt once treatment is complete
Internal radiation (brachytherapy): Involves placing radioactive sources inside or near the tumor.
The radiation source comes into direct, continuous contact with the tumor for a specific time period. This method provides a higher dose of radiation in the tumor over a specified time period, while limiting the dose in surrounding normal tissues
Precautions:
handle according to the guidelines. During hospitalization for radiation, pregnant women and children are not allowed to visit the pt
assign pt to a private room with a private bath
place a “caution: radioactive material” sign on the door of the pt’s room
wear a dosimeter film badge at all times while caring for pt with radioactive implants. the badge offers no protection,
limit each visitor to 1 half hour per day. be sure visitors stay at least 6 ft from the source.
keep the lead container in pt room
don’t remove temporary ink or dye markings
Skin protection during radiation therapy
wash the irradiated area gently each day with water or mild soap (use hands instead of a washcloth to avoid friction)
Avoid wearing belts, buckles, straps, or any type of clothing that binds or rubs the skin at the radiation site.
protect the area by wearing clothing over it
Advise against direct skin exposure to the sun during treatment and for at least 1 yr after completion of traditional therapy
Teach pt about skin care because skin becomes dry and itchy and may break down
avoid deodorant and lotion on the day of treatment
Side Effects of Radiation Therapy
Radiation therapy can lead to both acute and long-term side effects.
Common Side Effects:
Radiation dermatitis: Skin irritation and changes near the treated area are most common and can range from redness and rash to skin desquamation
Fatigue: A frequent complaint during and after treatment,
Altered taste: Common among patients, impacting dietary intake.
head and neck radiation may damage the salivary glands and cause dry mouth (xerostomia), which may impact speaking, chewing, and swallowing, and increase the pt’s lifelong risk for tooth decay
Bone marrow suppression: This can cause significant reductions in immunity and increase susceptibility to infections.
Cytotoxic Systemic Therapy
Cytotoxic therapy employs chemotherapeutic drugs to kill cancer cells and disrupt their cell regulation.
Unlike surgery or radiation, cytotoxic chemotherapy kills cancer cells (and normal cells) throughout the body
can be used alone, before or after treatment, or in combination
Types:
Neoadjuvant: Administered prior to surgery/radiation to shrink tumors for better surgical outcomes.
Adjuvant: used to kill remaining cancer cells following surgery or radiation
Risks: Increased vulnerability to infections and potential for complications due to myelosuppression from treatment.
The time when bone marrow activity and WBC counts are at their lowest levels after cytotoxic therapy is the nadir.
Administration of Chemotherapy Drugs
Chemotherapy is useful in treating cancer because its effects are systemic, providing the opportunity to kill cancer cells, and it may provide protection from cells that have started to metastasize.
These drugs target cancer cells through various mechanisms, such as:
Chemotherapy drugs can prevent cellular division
break DNA strands to halt replication
Disrupt cell reactions
prevent mitosis
Combination Therapy
using more than 1 drug for treatment
Different mechanisms of action work together to impact cell division
treatment issues
dosage are calculated according to the pt’s size, based on(mg/m2) of body surface area (BSA)
scheduling
administration
Administration Methods:
Routes can include intrathecal (spinal), intraperitoneal (abdominal), intravesicular (bladder), topical, and intra-arterial delivery.
Extravasation: monitor blood return at the access site during infusion at regular intervals
Oral anticancer drugs are just as toxic to the pt taking the drug and to the person handling the drug as are IV chemotherapy agents
Common Side Effects of Chemotherapy
Chemotherapy can lead to a range of side effects, some of which may resolve and others that can be permanent:
Increased susceptibility to infections (neutropenia)
Thrombocytopenia (decreased number of platelets) leading to bleeding and impaired clotting
Mucositis causes inflammation and ulceration of the lining of the gastrointestinal tract
Alopecia or hair loss affects psychological well-being
pt wear cooling caps on the head while receiving chemotherapy to help decrease rates of alopecia.
Skin changes such as rashes or hyperpigmentation
Anxiety and emotional distress due to treatment side effects
Chemotherapy-induced peripheral neuropathy (CIPN) leads to sensory changes.
Bone Marrow Suppression
Important educational points for managing patients include:
Preventing infections through improved hygiene, vaccinations, and careful monitoring of symptoms.
importance of reporting fever, signs and symptoms of infection, any changes in health status ( when temp elevates above 100.4 F or 38 C, respond by reporting to HCP)
report a cough, burning on urination, pain around the venous access site, or new drainage from a wound or any area of the body.
Avoiding injuries in patients with thrombocytopenia to minimize bleeding risk.
Implementing precautions for those experiencing myelosuppression and neutropenia, including avoidance of crowded places and careful monitoring of temperatures.
monitor VS every 4hrs, including temp
ensure that the pt’s room and bathroom are cleaned at least once each day
Nausea & Vomiting Associated with Chemotherapy
Nausea and vomiting can be categorized as follows:
Anticipatory: Occurs before chemotherapy due to past experiences.
Acute: Develops within the first 24 hours after treatment.
Delayed: Occurs more than 24 hours post-treatment.
Breakthrough: Occurs despite prophylactic medications for nausea.
Many cancer drugs are highly emetogenic, warranting preventative management strategies to enhance quality of life.
Ondansetron, can prolong QT interval within the cardiac cycle. ECG monitoring is recommended in pt with electrolyte abnormalities (hypokalemia or hypomagnesemia), HF, or bradyarrhythmias or pt taking other meds that can cause QT prolongation
ensure antiemetics are given before chemotherapy and are repeated based on the response and duration of CINV.
Cognitive Function Changes
Known colloquially as "chemo-brain," this condition may involve memory lapses and difficulty concentrating.
Support Strategies:
Cognitive training exercises to sharpen and enhance mental functions.
Advising against alcohol consumption and illicit drugs that could worsen cognitive impairments.
Endocrine (Hormone) Therapy
may include use of
Aromatase inhibitors
Gonadotropin-releasing hormone analogues (leuprolide)
anti-androgens
antiestrogens
Side Effects: Varying effects based on therapy choice, common ones include
fatigue, arthralgia, joint stiffness and/or bone pain, hot flashes, and sexual dysfunction
Long-term side effects include osteoporosis, increased cardiovascular risk, and risk for thrombotic events
Bisphosphonates are prescribed to help improve skeletal health and decrease risk for osteoporosis and pathologic bone fractures
Supportive Therapies
Colony-Stimulating Factors: Enhance bone marrow recovery and overall blood counts during chemotherapy, significantly decreasing the risk of complications.
bone pain is a common side effect in pt receiving colony-stimulating factors (acetaminophen or ibuprofen)
Oncologic Emergencies
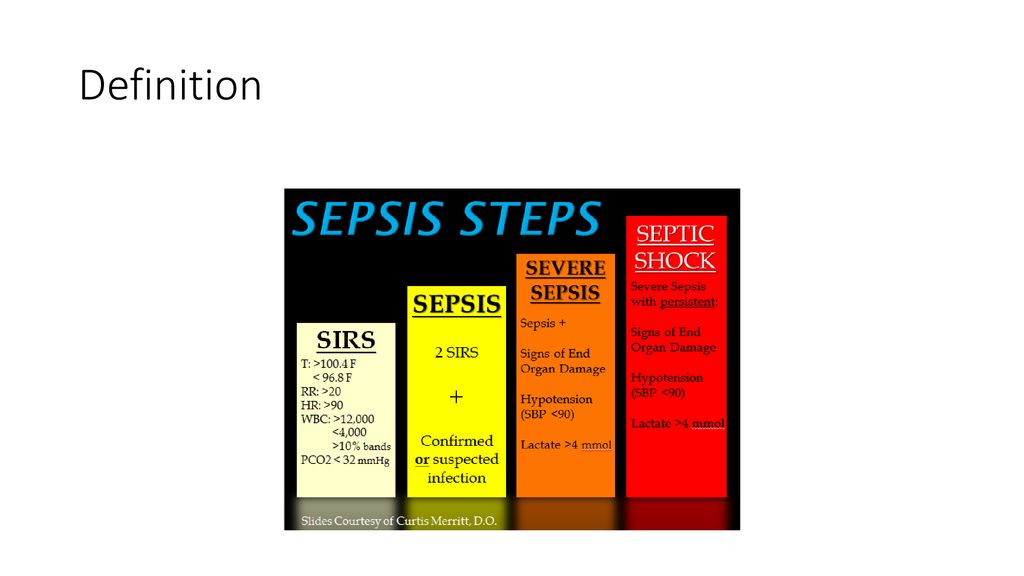
Sepsis: is a condition in which organisms enter the bloodstream through any site of skin, severe sepsis can result in septic shock which is life-threatening
often a low-grade fever (100.4 F or 38C) is the only sign of infection. infection and sepsis have a high mortality rate in adults with neutropenia

DIC (Disseminated Intravascular Coagulation): is a problem with the blood clotting process. DIC is triggered by many severe illnesses, including cancer
Bleeding from many sites is the most common problem and ranges from oozing to fatal hemorrhage
treatment: anticoagulants (heparin) are given to limit clotting and prevent the rapid consumption of circulating clotting factors
SIADH (Syndrome of Inappropriate Antidiuretic Hormone secretion): Leads to abnormal water retention and low sodium levels that can cause neurological symptoms.
cancer is a common cause of SIAH, especially small-cell lung cancer
mild symptoms include:
weakness
muscle cramps, loss of appetite
with greater fluid retention and decreased sodium levels, weight gain, nervous system changes, personality changes, confusion, and extreme muscle weakness occur
sodium levels drop towards 110, seizures, coma, and death may follow
Spinal Cord Compression: Requires immediate treatment to alleviate nerve compression and prevent paralysis; could be caused by tumor growth.
Back pain is a common 1st symptom
DX: MRI
treatment: high-dose Radiation and high-dose corticosteroids, surgery to remove the tumor
Hypercalcemia: Characterized by elevated calcium levels in the blood, bone metastasis can stimulate bone breakdown (osteoclast activity) and bone resorption, which releases more calcium from bone and leads to hypercalcemia
common s/s: fatigue, loss of appetite, N/V, constipation,and increased urine output
Treatment: IV hydration NS
Loop diuretics
avoid thiazide diuractics
Dialysis, if life-threatening
Superior Vena Cava Syndrome: Compression by tumors leads to compromised blood flow, and leads to congestion of blood returning to the body.
early s/s: edema of the face, especially around the eyes (periorbital edema) on arising in the morning, and reports of head fullness
as the compression worsens, pt develops engorged blood vessels and erythema of the upper body, edema in the arms and hands, and dyspnea
stridor. Symptoms are more apparent when the pt is in the supine position
Treatment: radiation/chemotherapy. surgery last result
Tumor Lysis Syndrome: Occurs after aggressive treatment leading to rapid cell breakdown, causing significant electrolyte imbalances requiring urgent medical management.
Severe or untreated TLS can cause acute kidney injury and death
serum k+ levels increase, causing Hyperkalemia, which can lead to cardiac dysfunction
The large amount of cellular by-products form uric acid, causing Hyperuricemia
Uric acid crystals precipitate in the kidney, blocking kidney tubules and leading to AKI
early s/s
lethargy, N/V, anorexia, flank pain, muscle weakness, cramps, seizures, and altered mental status
Hydration prevents and manages TLS by increasing the kidney flow rates, preventing uric acid buildup in the kidneys and diluting serum potassium levels.
Survivorship
Addressing unique physical and psychosocial needs of cancer survivors is vital to ensuring quality of life.
Emphasis on routine follow-ups and adherence to care schedules helps in monitoring for recurrence and management of long-term effects of treatment.